Abstract
Foetal hypoxia–ischaemia is a key trigger of meconium aspiration syndrome (MAS). However, many neonates develop MAS without evidence of hypoxia–ischaemia, suggesting the presence of covert but important risk variables. We evaluated the association of MAS with clinical variables, placental histopathologic findings, and inflammatory biomarkers at birth. Of 1336 symptomatic and asymptomatic term singleton neonates with meconium-stained amniotic fluid, 88 neonates (6.6%) developed MAS. Univariate analysis showed that MAS development was associated with low 1- and 5-min Apgar scores, low cord blood pH, funisitis, higher α1-acid glycoprotein levels, and higher haptoglobin levels (all p < 0.001 except for p = 0.001 for haptoglobin). Associations of MAS with caesarean delivery (p = 0.004), premature rupture of the membranes (p = 0.006), chorioamnionitis (p = 0.007), and higher C-reactive protein levels (p = 0.008) were lost when adjusted for multiple comparisons. The final multivariate model to explain MAS development comprised lower cord blood pH (odds ratio [OR] 0.58; 95% confidence interval [CI] 0.47–0.73; p < 0.001), funisitis (OR 2.45; 95% Cl 1.41–4.26; p = 0.002), and higher α1-acid glycoprotein levels (OR 1.02; 95% Cl 1.01–1.03; p = 0.001). Our data from a large cohort of neonates suggested that intrauterine inflammation is one of the key independent variables of MAS development, together with foetal hypoxia–ischaemia.
Similar content being viewed by others
Introduction
Meconium-stained amniotic fluid is common during labour and affects 10–15% of neonates. Approximately 5% of these neonates develop meconium aspiration syndrome (MAS)1,2,3. Despite advances in neonatal resuscitation and respiratory care, MAS remains a serious cause of neonatal mortality and morbidity, especially in developing countries and low-resource settings. It is generally accepted that activation of colonic peristalsis triggered by foetal hypoxia–ischaemia leads to the passage of meconium and foetal gasping movements, resulting in meconium aspiration and respiratory distress3,4,5,6. Numerous risk factors for MAS and foetal hypoxia–ischaemia have been identified, including post-term pregnancy, foetal distress, low birth weight, mode of delivery, low Apgar scores, and low cord blood pH7,8,9,10. However, there remain considerable inconsistencies in the relationships among the presence of foetal hypoxia–ischaemia, meconium-stained amniotic fluid, chest radiography findings, and the development of respiratory failure3. For example, no evidence of foetal hypoxia and stress is noted in approximately 50% of neonates with MAS9,11. This suggests the presence of covert but important risk factors for MAS other than acute foetal hypoxia–ischaemia. Intrauterine inflammation has become increasingly recognised as one of the key variables in the development of MAS12. Meconium-stained amniotic fluid is associated with an increased incidence of clinical chorioamnionitis and is accompanied by elevated levels of inflammatory mediators in the amniotic fluid. Interestingly, histopathological chorioamnionitis in term neonates is often observed in the absence of overt bacterial infection13,14. The influence of intrauterine inflammation and the subsequent foetal systemic inflammatory response can be evaluated by the histopathological assessment of the umbilical cord and placenta, and previous studies have demonstrated that the presence of chorioamnionitis and funisitis are risk factors for MAS15. Consistent with this, we have previously developed a model to explain the development of MAS. The model was based on a cohort of 95 neonates hospitalised in a level-II Neonatal Intensive Care Unit (NICU) with meconium-stained amniotic fluid and comprised birth asphyxia, inflammation, and sex16. A study of autopsy cases of MAS highlighted an association between funisitis and villus ischaemic changes, suggesting that the process of lung injury started in utero17. Although the association between meconium-stained amniotic fluid and inflammation is well established, the relationship between foetal inflammation and MAS development remains unclear because most previous studies assessed the umbilical cord and placenta in only a part of the study cohort15,16.
This study aimed to confirm the relationship between foetal hypoxia–ischaemia, intrauterine inflammation, and the development of MAS in a large cohort of term neonates with meconium-stained amniotic fluid.
Results
The final study cohort comprised 1336 neonates with meconium-stained amniotic fluid. The neonates were born at 40.2 ± 1.0 weeks of gestation and weighed 3121 ± 411 g at birth. Of these, 88 neonates (6.6%) developed MAS.
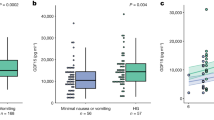
Univariate logistic regression analysis showed that the development of MAS was associated with low 1- and 5-min Apgar scores (both p < 0.001), low cord blood pH (p < 0.001) (Table 1), funisitis (p < 0.001), higher α1-acid glycoprotein (α1-AG) levels (p < 0.001), higher haptoglobin levels (p = 0.001), and higher acute-phase inflammatory reaction (APR) scores (p < 0.001) (Table 2). Associations of MAS development with caesarean delivery (p = 0.004), premature rupture of the membrane (PROM) (p = 0.006), chorioamnionitis (p = 0.007), and higher C-reactive protein (CRP) levels (p = 0.008) were lost when adjusted for multiple comparisons.
The final multivariate model to explain the incidence of MAS comprised lower cord blood pH (odds ratio [OR] 0.58 per 0.10 pH change; 95% confidence interval [Cl] 0.47–0.73; p < 0.001), funisitis (OR 2.45; 95% CI 1.41–4.26; p = 0.002), and higher α1-AG levels (OR 1.02; 95% CI 1.01–1.03; p = 0.001) (adjusted for gestational age, caesarean delivery, and sex) (Table 3).
Alternative multivariate models were developed to assess the potential impact of chorioamnionitis (instead of funisitis) and inflammatory biomarkers other than α1-AG on the development of MAS. Model 2, which replaced funisitis with chorioamnionitis, identified cord blood pH and α1-AG levels (both p < 0.001), but not chorioamnionitis (p = 0.317), as significant independent variables for MAS development (Supplementary Table S1). Model 3, which replaced α1-AG levels with CRP, identified cord blood pH and funisitis (both p < 0.001), but not CRP (p = 0.193), as significant independent variables for MAS development (Supplementary Table S2). Model 4, which replaced α1-AG by the APR score (0, 1, and 2 or 3), confirmed cord blood pH (p = 0.001), funisitis (p < 0.001), and APR scores (p = 0.015 and 0.019 for APR scores of 1 and 2 or 3, respectively, compared with score 0) as significant independent variables for MAS development (Supplementary Table S3).
Discussion
Low cord blood pH, funisitis, and elevated serum α1-AG levels at birth were associated with MAS development in a large population of neonates with meconium-stained amniotic fluid. These findings highlight the importance of considering intrauterine inflammation and foetal hypoxia–ischaemia in the mechanism, prediction, and prevention of MAS development.
The pathological mechanism of MAS has primarily been explained by premature bowel peristalsis triggered by intrauterine hypoxia–ischaemia3,4,5,6. However, studies have identified intrauterine inflammation as an alternative key independent variable for MAS development12. Meconium-stained amniotic fluids are associated with intrauterine inflammation, as evidenced by the presence of bacterial contamination and elevated inflammatory biomarkers, such as interleukin-6, in the amniotic fluid15,18. The amniotic fluid containing bacteria, microproducts, and proinflammatory mediators, when swallowed by the foetuses, may trigger bowel peristalsis and the passage of meconium in utero, potentially explaining the development of MAS even in the absence of intrauterine hypoxia–ischaemia15,18,19. Consistent with these preliminary findings, our study confirmed that the development of MAS is associated with funisitis and serum α1-AG levels at birth and foetal hypoxia–ischaemia in a large cohort of neonates with meconium-stained amniotic fluid. However, it should be noted that hypoxia–ischaemia and inflammation often coincide and trigger each other, further rendering the biological response and clinical manifestation complex20. Future studies that address the mechanism, early diagnosis, and prevention of MAS may need to consider the role of intrauterine inflammation, as well as hypoxia–ischaemia, in disease pathogenesis.
Univariate analysis showed that funisitis and chorioamnionitis were associated with an increased incidence of MAS in this study. However, when adjusted for other independent variables and covariates, only funisitis, but not chorioamnionitis, was an independent variable for MAS development. Both funisitis and chorioamnionitis are accepted as common consequences of intrauterine inflammation21,22. However, there might be subtle but pathologically significant differences between these conditions, such as the stage and extension of intrauterine inflammation and the biological response to the inflammation. Common clinical manifestations of chorioamnionitis include maternal fever, leucocytosis, and foul vaginal discharge, which often proceed to PROM, premature delivery, and intrauterine foetal death. In contrast, clinical symptoms of funisitis appear to represent relatively more foetal conditions, such as leucocytosis, elevated CRP and immunoglobulin M at birth, bronchopulmonary dysplasia, and cerebral palsy23,24. Provided that funisitis reflects the foetal response to intrauterine inflammation relatively more specifically (and that chorioamnionitis predominantly reflects the maternal response to inflammation)25,26,27, it would be reasonable to conclude that funisitis is more closely related to the development of MAS than chorioamnionitis. Future studies should address the exact stage and magnitude of intrauterine inflammation related to funisitis and chorioamnionitis.
We used CRP, α1-AG, and haptoglobin as representative serum inflammatory biomarkers at birth in the current study. Univariate analysis results consistently suggested a relationship between the elevation of these biomarkers and the development of MAS. However, only α1-AG was identified as an independent variable for MAS development in the multivariate model; no significant improvement of the model was observed when α1-AG was replaced by the APR score in Model 4 (Supplementary Table S3). α1-AG is a hepatic glycoprotein, the synthesis of which is regulated by glucocorticoids and inflammatory cytokines, such as IL-1, IL-6, and IL-828. An increase in α1-AG serum level is associated with various conditions, including cancer, trauma, infection, and inflammation29. Simultaneous α1-AG and haptoglobin measurement, in addition to CRP, has been proposed for the early detection of systemic infection in neonates30,31,32. CRP levels tend to rise shortly after birth in neonates with MAS, potentially in response to chemical pneumonitis, mechanical ventilation, bacterial superinfection, and airway obstruction33,34,35. In contrast, serum α1-AG level slightly increases and remains elevated even after CRP returns to the baseline levels36,37. Therefore, α1-AG might be suitable for the assessment of chronic inflammation, including intrauterine inflammation. Indeed, in our current study, α1-AG levels at birth were more closely associated with MAS development than CRP and haptoglobin. Such a property of α1-AG might be relevant as a surrogate marker for intrauterine inflammation associated with histological evidence. Nonetheless, in our study population, there was a trend that an APR score of 2 or 3 was associated with a relatively higher incidence of MAS (Table 2), leaving a possibility that these biomarkers improve the prediction of MAS development in an additive way. Future studies are needed to elucidate whether the combination of CRP, haptoglobin, α1-AG, and other inflammatory biomarkers provide a more reliable prediction of MAS development than α1-AG alone.
We were able to confirm that both foetal hypoxia–ischaemia and intrauterine inflammation are key independent risk factors for MAS development in a large cohort of neonates. Unlike previous studies, which relied on the clinical diagnosis of chorioamnionitis25, our study performed the histopathological assessment of the placenta and umbilical cord and serum biomarker tests in virtually all neonates with meconium-stained amniotic fluid, regardless of subsequent admission to the NICU. This contributed to minimizing selection bias. However, because of the single-centre, retrospective nature of the study, the exact cause-consequence relationships among foetal hypoxia–ischaemia, intrauterine inflammation, and inflammatory response in neonates remain unclear. Because of limited human resources, the placenta and umbilical cord were assessed by a single pathologist using the classifications by Blanc and Redline38,39. An alternative standard classification scale, or the Amsterdam Placental Workshop Group Consensus State, provides relatively more detailed information regarding the severity and extent of intrauterine inflammation, which may allow the assessment of relationships between the spatial pattern and severity of funisitis and MAS development40. In the multivariate model of our study, together with known independent variables for MAS development, such as gestational age, cord blood pH, and mode of delivery7,8,9,10, sex was additionally incorporated as one of the covariates based on our preliminary findings, which suggested the dependence of MAS development on sex16; however, this relationship was not observed in the current analysis. Considering that our multivariate model does not fully explain the development of MAS, exploration for key independent variables of MAS should be continued.
Our data from a large cohort of neonates suggested that intrauterine inflammation and foetal hypoxia–ischaemia are key independent variables for MAS development. Of the variables supporting the presence of intrauterine inflammation and a foetal biochemical response, funisitis and serum α1-AG levels, but not chorioamnionitis or serum CRP and haptoglobin levels, showed robust associations with the development of MAS. These findings may contribute to a more precise understanding of the mechanism underlying MAS development and the prediction, prevention, and treatment of this serious clinical condition. Further studies are needed to elucidate the exact relationship and order between intrauterine inflammation, hypoxia–ischaemia, the elevation of serum biomarkers, and the subsequent development of respiratory failure.
Materials and methods
This single-centre retrospective observational study was conducted under the approval of the Ethics Committee of Nagoya City University West Medical Centre, Nagoya, Japan (reference number: 18-04-381-451). The need for parental informed consent was waived by the ethics committee (the Ethics Committee of Nagoya City University West Medical Centre) because this study was based on anonymised patients’ data. All methods were carried out in accordance with relevant guidelines and regulations.
Study population
Between March 2013 and December 2018, a total of 7772 neonates were born at the birth centre of the Nagoya City University West Medical Centre. In the current study, 1389 term neonates with meconium-stained amniotic fluid were reviewed. In this centre, histopathological examination of the placenta is routinely performed for neonates with meconium-stained amniotic fluid. The following neonates were excluded: 39 neonates whose placentae were unavailable and 10 neonates subsequently diagnosed with major congenital anomalies. Additionally, four multiple gestations were excluded because of potential contamination of the amniotic fluid between the siblings. Consequently, 1336 neonates were available for analysis (Fig. 1).
Clinical variables
The presence of meconium-stained amniotic fluid was visually assessed at the time of the membrane rupture by experienced midwives10,15,18. MAS was defined as respiratory distress in neonates born through meconium-stained amniotic fluid, requiring assisted mechanical ventilation or oxygen at a concentration of ≥ 40% for at least 48 h, based on radiographic findings (assessed by an experienced neonatologist, K.Y.)15,41. Histopathological examination of the placenta and umbilical cord was performed by an experienced pathologist (M.K.) to diagnose chorioamnionitis and funisitis. Chorioamnionitis was defined as infiltration of neutrophils identified in the chorionic plate using Blanc’s classification (Stage II). Funisitis was defined as infiltration of neutrophils within the walls of the umbilical vessels or in Wharton’s jelly38,39.
Patients’ clinical records were reviewed for other clinical variables, including maternal variables (gestational age at delivery, presence of maternal group B streptococcus colonisation, delivery mode, parity, PROM ≥ 24 h, chorioamnionitis, and funisitis). Similarly, neonatal variables, such as birth weight and its z-score, sex, 1- and 5-min Apgar scores, arterial cord blood pH, and other blood tests from the arterial or venous cord or peripheral venous blood at admission, were reviewed.
Laboratory studies
For neonates with meconium-stained amniotic fluid, umbilical cord blood was obtained to assess serum inflammatory biomarkers, including C-reactive protein (CRP; limit of detection, 0.3 mg/dL), α1-acid glycoprotein (α1-AG; limit of detection, 20 mg/dL), and haptoglobin (limit of detection, 13 mg/dL), which were routinely checked using a turbidimetric immunoassay (Quick Turbo, Shino-Test Corporation, Tokyo, Japan)30,31,32. In relatively rare cases, when the volume of the cord blood sample was insufficient for the assay, a venous blood sample was additionally obtained approximately an hour after birth. The raw values of these biomarkers and a composite score, or the APR score, of 0 to 3 were calculated according to the elevation of each biomarker above thresholds (see Supplementary Information S4)32.
Statistical analysis
Values are expressed as the mean ± standard deviation, number (%), median (quartile range) or OR; 95% CI. We employed a fully conditional specification using multiple imputations (5 imputed datasets) by the Markov Chain Monte Carlo algorithm to avoid selection bias from missing data42. The missing cases for the maternal and neonatal variables, including inflammatory biomarkers, were in the range of 0.1–2.1%. To test the hypothesis that the development of MAS is associated with foetal hypoxia–ischaemia and intrauterine inflammation, a logistic regression model was developed using cord blood pH, inflammatory biomarkers, and histopathological findings as independent variables, adjusting for the priori covariates of sex, delivery mode, and gestational age. Additionally, univariate logistic regression analysis was performed to investigate crude effects of the clinical variables on MAS development, where p-values < 0.003 were considered statistically significant for correcting multiple comparisons for 16 variables. All statistical analyses were performed using SPSS Statistics ver. 26 (IBM Corp, Armonk, NY, USA).
References
Yoder, B. A., Kirsch, E. A., Barth, W. H. & Gordon, M. C. Changing obstetric practices associated with decreasing incidence of meconium aspiration syndrome. Obstet. Gynecol. 99, 731–739 (2002).
Dargaville, P. A., Copnell, B. & Australian and New Zealand Neonatal N. The epidemiology of meconium aspiration syndrome: Incidence, risk factors, therapies, and outcome. Pediatrics 117, 1712–1721 (2006).
Swarnam, K., Soraisham, A. S. & Sivanandan, S. Advances in the management of meconium aspiration syndrome. Int. J. Pediatr. 2012, 359571. https://doi.org/10.1155/2012/359571 (2012).
Ahanya, S. N., Lakshmanan, J., Morgan, B. L. & Ross, M. G. Meconium passage in utero: Mechanisms, consequences, and management. Obstet. Gynecol. Surv. 60, 45–74 (2005).
van Ierland, Y. & de Beaufort, A. J. Why does meconium cause meconium aspiration syndrome? Current concepts of MAS pathophysiology. Early Hum. Dev. 85, 617–620 (2009).
Lindenskov, P. H., Castellheim, A., Saugstad, O. D. & Mollnes, T. E. Meconium aspiration syndrome: Possible pathophysiological mechanisms and future potential therapies. Neonatology 107, 225–230 (2015).
Trimmer, K. J. & Gilstrap, L. C. “Meconiumcrit” and birth asphyxia. Am. J. Obstet. Gynecol. 165, 1010–1013 (1991).
Ramin, S. M., Gilstrap, L. C. 3rd., Leveno, K. J., Dax, J. S. & Little, B. B. Acid–base significance of meconium discovered prior to labor. Am. J. Perinatol. 10, 143–145 (1993).
Blackwell, S. C. et al. Meconium aspiration syndrome in term neonates with normal acid–base status at delivery: Is it different?. Am. J. Obstet. Gynecol. 184, 1422–1425 (2001).
Oyelese, Y. et al. Meconium-stained amniotic fluid across gestation and neonatal acid–base status. Obstet. Gynecol. 108, 345–349 (2006).
Yeomans, E. R., Gilstrap, L. C. 3rd., Leveno, K. J. & Burris, J. S. Meconium in the amniotic fluid and fetal acid–base status. Obstet. Gynecol. 73, 175–178 (1989).
Ghidini, A. & Spong, C. Y. Severe meconium aspiration syndrome is not caused by aspiration of meconium. Am. J. Obstet. Gynecol. 185, 931–938 (2001).
Mazouri, A., Fallah, R., Saboute, M., Taherifard, P. & Dehghan, M. The prognostic value of the level of lactate in umbilical cord blood in predicting complications of neonates with meconium aspiration syndrome. J. Matern. Fetal Neonatal Med. 34, 1013–1019 (2021).
Roberts, D. J. et al. Acute histologic chorioamnionitis at term: Nearly always noninfectious. PLoS ONE 7, e31819. https://doi.org/10.1371/journal.pone.0031819 (2012).
Lee, J. et al. Meconium aspiration syndrome: A role for fetal systemic inflammation. Am. J. Obstet. Gynecol. 214(366), e1-366.e3669 (2016).
Yokoi, K., Iwata, O., Kobayashi, S., Muramatsu, K. & Goto, H. Influence of foetal inflammation on the development of meconium aspiration syndrome in term neonates with meconium-stained amniotic fluid. PeerJ 7, e7049. https://doi.org/10.7717/peerj.7049 (2019).
Thureen, P. J., Hall, D. M., Hoffenberg, A. & Tyson, R. W. Fatal meconium aspiration in spite of appropriate perinatal airway management: Pulmonary and placental evidence of prenatal disease. Am. J. Obstet. Gynecol. 176, 967–975 (1997).
Romero, R. et al. Bacteria and endotoxin in meconium-stained amniotic fluid at term: Could intra-amniotic infection cause meconium passage?. J. Matern. Fetal Neonatal Med. 27, 775–788 (2014).
Wolfs, T. G. et al. Chorioamnionitis-induced fetal gut injury is mediated by direct gut exposure of inflammatory mediators or by lung inflammation. Am. J. Physiol. Gastrointest. Liver Physiol. 306, G382–G393 (2014).
Liu, F. & McCullough, L. D. Inflammatory responses in hypoxic ischemic encephalopathy. Acta Pharmacol. Sin. 34, 1121–1130 (2013).
Kim, C. J. et al. Acute chorioamnionitis and funisitis: Definition, pathologic features, and clinical significance. Am. J. Obstet. Gynecol. 213, S29–S52 (2015).
Kim, C. J., Romero, R., Chaemsaithong, P. & Kim, J. S. Chronic inflammation of the placenta: Definition, classification, pathogenesis, and clinical significance. Am. J. Obstet. Gynecol. 213, S53–S69 (2015).
Yoon, B. H. et al. Fetal exposure to an intra-amniotic inflammation and the development of cerebral palsy at the age of three years. Am. J. Obstet. Gynecol. 182, 675–681 (2000).
Nakayama, M. Significance of pathological examination of the placenta, with a focus on intrauterine infection and fetal growth restriction. J. Obstet. Gynaecol. Res. 43, 1522–1535 (2017).
Pacora, P. et al. Funisitis and chorionic vasculitis: The histological counterpart of the fetal inflammatory response syndrome. J. Matern. Fetal Neonatal Med. 11, 18–25 (2002).
Lee, S. M., Lee, K. A., Kim, S. M., Park, C. W. & Yoon, B. H. The risk of intra-amniotic infection, inflammation and histologic chorioamnionitis in term pregnant women with intact membranes and labor. Placenta 32, 516–521 (2011).
Jung, E. et al. The fetal inflammatory response syndrome: The origins of a concept, pathophysiology, diagnosis, and obstetrical implications. Semin. Fetal Neonatal Med. 25, 101146. https://doi.org/10.1016/j.siny.2020.101146 (2020).
Fournier, T., Medjoubi, N. N. & Porquet, D. Alpha-1-acid glycoprotein. Biochim. Biophys. Acta. 1482, 157–171 (2000).
Hashimoto, S. et al. Alpha-1-acid glycoprotein fucosylation as a marker of carcinoma progression and prognosis. Cancer 101, 2825–2836 (2004).
Speer, C., Bruns, A. & Gahr, M. Sequential determination of CRP, alpha 1-antitrypsin and haptoglobin in neonatal septicaemia. Acta Paediatr. Scand. 72, 679–683 (1983).
Ipek, I. O., Saracoglu, M. & Bozaykut, A. Alpha1-acid glycoprotein for the early diagnosis of neonatal sepsis. J. Matern. Fetal Neonatal Med. 23, 617–621 (2010).
Nakamura, T., Hatanaka, D., Yoshioka, T., Yamada, S. & Goto, H. Study on the usefulness of APR scores from the viewpoint of proinflammatory cytokines. Dis. Mark. 2015, 981981. https://doi.org/10.1155/2015/981981 (2015).
Pourcyrous, M., Bada, H. S., Korones, S. B., Baselski, V. & Wong, S. P. Significance of serial C-reactive protein responses in neonatal infection and other disorders. Pediatrics 92, 431–435 (1993).
Hofer, N., Zacharias, E., Müller, W. & Resch, B. An update on the use of C-reactive protein in early-onset neonatal sepsis: Current insights and new tasks. Neonatology 102, 25–36 (2012).
Mahendiran, K., Batra, P., Faridi, M. M. A. & Singh, N. P. Procalcitonin as predictor of bacterial infection in meconium aspiration syndrome. Am. J. Perinatol. 35, 769–773 (2018).
Northrop-Clewes, C. A. Interpreting indicators of iron status during an acute phase response—lessons from malaria and human immunodeficiency virus. Ann. Clin. Biochem. 45, 18–32 (2008).
Suchdev, P. S. et al. Assessment of iron status in settings of inflammation: Challenges and potential approaches. Am. J. Clin. Nutr. 106, 1626S-1633S (2017).
Blanc, W. A. Pathology of the placenta and cord in ascending and in haematogenous infection. Ciba Found. Symp. 77, 17–38 (1979).
Redline, R. W. et al. Amniotic infection syndrome: Nosology and reproducibility of placental reaction patterns. Pediatr. Dev. Pathol. 6, 435–448 (2003).
Khong, T. Y. et al. Sampling and definitions of placental lesions: Amsterdam Placental Workshop Group Consensus Statement. Arch. Pathol. Lab. Med. 140, 698–713 (2016).
Fraser, W. D. et al. Amnioinfusion for the prevention of the meconium aspiration syndrome. N. Engl. J. Med. 353, 909–917 (2005).
White, I. R., Royston, P. & Wood, A. M. Multiple imputation using chained equations: Issues and guidance for practice. Stat. Med. 30, 377–399 (2011).
Acknowledgements
The authors are grateful to all clinical staff in the Department of Obstetrics and Gynecology of Nagoya City University West Medical Centre for sampling placentae.
Funding
This study received no funding.
Author information
Authors and Affiliations
Contributions
K.Y. wrote the manuscript with support from O.I. and S.K. K.Y and O.I. were responsible for data analysis. M.K. contributed to sample preparation. S.S. and H.G. helped supervise the project. All authors discussed the results and commented on the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Yokoi, K., Iwata, O., Kobayashi, S. et al. Evidence of both foetal inflammation and hypoxia–ischaemia is associated with meconium aspiration syndrome. Sci Rep 11, 16799 (2021). https://doi.org/10.1038/s41598-021-96275-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-96275-x
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.