Abstract
There have been marked improvements in oral health in Korea during the past 10 years, including chewing ability. We sought to disentangle age, period, and cohort effects in chewing ability between 2007 and 2018. We analyzed data from the Korea National Health and Nutrition Examination Survey. The main variable was chewing difficulty, which was assessed among participants aged 20 years and older. APC analysis revealed three trends in chewing difficulty: (1) there was an increase in chewing difficulty starting at around 60 years of age (age effect), (2) there was a steady decrease in chewing difficulty during the observation period (period effect), and (3) chewing ability improved with each successive generation born after 1951 (cohort effect). Regarding recent improvements in chewing ability, cohort effects were somewhat more important than period effects.
Similar content being viewed by others
Introduction
Recent studies have suggested that oral health has been improving in many countries1,2,3,4,5,6,7,8,9, with decreased incidence of dental diseases and increased accessibility of dental care. Contributory factors could include improved proximal determinants of oral health (i.e., health behaviors and sugar consumption), as well as improving structural determinants (i.e., socioeconomic context and environmental context) over several decades.
Oral health is affected by exposures throughout the entire life course, beginning in the prenatal period, and is strongly socially patterned10. Studies have tried to identify age, period, and cohort effects to clarify the impact of social and environmental exposure and thereby find compelling evidence of the importance of preventive factors in oral health1,11,12,13,14,15,16,17,18,19. Cohort effects on oral cancer mortality have been revealed in two studies, supporting common risk factors theory12,15. These studies suggested that the influence of smoking and alcohol consumption contributed to marked changes in the cohort-effect curvature15. Secular changes in oral health behaviors (such as regular brushing, use of fluoridated toothpaste) as well as changes in dental practices may result in cohort effects on oral health outcomes over time (i.e., dental care utilization and number of remaining teeth)17. Dental insurance typically has a period effect, i.e., covering it causes changes in access before and after the policy. However, it could influence both period and cohort effects, in terms of a trend changing from problems in visiting patterns to routine and maintenance care1.
In the Korean context, the national dental sealant project launched in 2000 contributed to the prevention of dental caries (a period effect)4. For example, dental sealant use increased (24.8% to 48.9%), while untreated dental caries decreased (49.7% to 19.8%) from 2003 to 2010 among 12-year-olds. Further, the filled teeth for dental decay and the number of teeth increased in the recent birth cohorts (a cohort effect)18. However, evidence has less focused on subjective oral health outcomes which more likely to need-based predict for the population oral health20,21.
Chewing ability is associated with accumulated lifetime impacts on oral health; that is, it is not just an issue for older persons. Chewing ability is associated with the number of teeth affected by dental caries, periodontal disease, and inadequate access to dental care. In turn, aspects of oral health can influence social outcomes (i.e., job opportunity and economic activity)22,23 as well as health outcomes (i.e., life expectancy)24. Recent evidence suggests that improving trends in chewing ability might be attributed to external changes beyond dental treatment interventions25. This is because chewing ability has improved in both older and younger adults, which implies the need to identify age- and period-cohort patterns in these trends.
An age effect on chewing ability implies that there are changes in oral health as a result of accumulated physiological changes over time—for example, the effects of aging on periodontal tissues based on molecular changes in periodontal cells which intensify bone loss in elderly patients with periodontitis26. If improved chewing ability is due to a period effect, then the current trends may persist into the next generation since the same exposure factors would affect all ages simultaneously. If the chewing ability pattern is due to a birth cohort effect, then this will contribute to an improvement in oral health in the future because South Korea is advancing social determinants of oral health.
Thus, we sought to identify age, period, and cohort effects related to trends in improved chewing ability, to reflect overall oral function for persons of all ages.
Methods
Ethics approval and consent to participate
This study used open access data from the Korea National Health and Nutrition Examination Survey (KNHANES) for 2017 and 2016–2018 conducted by the Korea Centers for Disease Control and Prevention (KCDC). All participants of the KNHANES provided written informed consent to participate in the survey. The KNHANES was approved by the Institutional Review Board (IRB) of the KCDC. This is a publicly available, secondary dataset. Our institute determined that the use of the KNHANES dataset does not meet the criteria for human subject research, and was therefore exempt from IRB approval. We confirmed that all methods were performed in accordance with the relevant guidelines and regulations.
Data sources
We used the Korea National Health and Nutrition Examination Survey (KNHANES) data from 2007 to 2016–2018. The KNHANES is a nationally representative cross-sectional survey conducted by the Korea Centers for Disease Control and Prevention (KCDC). The survey includes approximately 10,000 individuals aged 1 year or over during each survey year. Among participants, less than 3% were excluded because of missing values for our variables of interest (i.e., chewing difficulty, age, sex, and study year). Chewing difficulty is defined as difficulty or discomfort during mastication. It was assessed using self-responses to the following in-person questions: ‘Do you have difficulty or discomfort when chewing food due to oral problems, including teeth, dentures, or gums?’ and ‘If you use dentures, please describe your experience of wearing dentures’. Individual responses of experiencing ‘difficulty’ and ‘severe difficulty’ were categorized as ‘chewing difficulties’ and assigned a value of 1; whereas responses of ‘no difficulty’, ‘little difficulty’, and ‘some difficulty’ were categorized as ‘no chewing difficulties’ and assigned a value of 0. Age-adjusted prevalence of chewing difficulty was calculated using the standard population provided by the Korea National Statistical Office’s resident population registry27. In this analysis, age was the self-reported age of the respondents at the time of the survey interview. This ranged from the oldest respondents (80 years or older) to the youngest respondents (aged 20 years). Period represented the years of data collection (2007 to 2016–2018). Birth year was the age subtracted from the survey year. Birth cohort was categorized based on arbitrary 10-year periods from 1900 to 1992.
Statistical analysis
We performed two-stage procedures to estimate age, period, and cohort effects and to confirm robustness of the analysis. First, we constructed age-period-cohort (APC) models (with “acp” parametrization) using the “apcfit” Stata command to apply constraints to overcome the identifiability issue of APC models. Natural splines were used to estimate each of the three effects, which were then combined to obtain estimated rates28. We used yearly interval knots each for age, period, and cohort variable to fit the model appropriately and to ensure sensitivity, which can be dictated by the width of the intervals for the age and period terms. Age, period, and cohort were treated as continuous variables. We also investigated the effect of gender as a covariate. We used a generalized linear model framework with a Poisson family error structure, a log link function, and an offset of log (person risk time).
Second, we used the “grmean” Stata command to plot standardized rates and to plot observed and fitted rates against another variable, with separate lines and symbols used for different groups from the APC models29.
Finally, we confirmed the APC model fit to possible combinations of age, period, and cohort effects using the Akaike information criterion and Bayesian information criterion30. We also conducted a sensitivity test to verify changes in the trends in age-adjusted rates using Joinpoint, which was developed by the Surveillance Research Program of the United States National Cancer Institute31.
We used Stata statistical software (Stata Corp. 2017. Stata Statistical Software: Release 15. College Station, TX: Stata Corp LLC.) for all statistical analyses.
Results
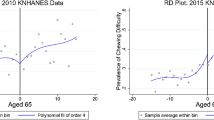
Figure 1 illustrates the results of the age, period, and cohort effects both genders combined, and men and women separately. The APC analysis revealed three trends in chewing difficulty: (1) an increase in chewing difficulty at around 60 years of age (age effect), (2) a steady decrease from 2007 to 2010 and an increase between 2010 and 2014, followed by a decline (period effect), and (3) greater difficulty in the generation born before 1951 compared to the generation born after 1951; chewing difficulty gradually decreased thereafter in each generation (cohort effect).
Age, period, and cohort effects on chewing difficulty. Chewing difficulty prevalence between 2007 and 2018 is shown overall, and for men and women: (a) age-specific difficulty by birth cohort overall, and for men and women, (b) by period overall, and for men and women, (c) birth-cohort-specific rate by age overall, and for men and women.
Although there were apparent differences between men and women in the three results, we confirmed that there was no gender effect on chewing difficulty across the entire dataset after adjusting for other effects in the APC model (Supplementary Table S1).
Table 1 shows the results for each fitted model. The full ACP and APC models, which had the lowest Akaike information criterion and Bayesian information criterion values, were considered the best fit out of the four models32. We confirmed that both the ACP and APC parameterizations represent an adequate fit of our data. Regarding the AIC statistics in Table S2 and Table S3, the only difference between ACP and APC specification is indicated in the 5th decimal place. We also confirmed that the BIC provided comparable results for the ACP and APC specifications.
Figure 2 shows the ratios obtained from the APC analysis with “acp” parametrization which can be interpreted as showing the longitudinal effect of age for the reference cohort and how this differs across cohorts32. It reveals age-specific rates for those born in 1951, after adjustment for the period effect. The left side indicates that among people born in 1951, chewing difficulty increased steadily until around 60 years of age, and then increased markedly thereafter. The right side shows that the cohort effect (including drift) decreased steadily until the 1990s. In the cohort analysis, those born in 1951 are the reference [= 1] and represent the point of acceleration of risk. The graph also shows a lower proportion of participants with chewing difficulty in later cohorts (including Baby Boomers) born between the 1960s and the 1990s. A longitudinal age effect also was confirmed, suggesting that the prevalence of chewing difficulty increases as the cohort ages. (Supplementary Figure S1).
We confirmed the validity of our APC model. In the Joinpoint regression analysis, changes in the linear trends were detected. Chewing difficulty prevalence decreased drastically from 2007 to 2013 (annual percent change: APC: − 5.10, 95% CI − 8.5 to − 1.6) and decreased gradually from 2013 to 2016 (APC: − 2.9, 95% CI − 12.8 to 8.1). In men, the prevalence of chewing difficulty decreased significantly from 2007 to 2013 (APC: − 5.1, 95% CI − 9.5 to − 0.5) and decreased from 2013 to 2016 (APC: − 1.5, 95% CI − 14.4 to 13.3). In women, the prevalence of chewing difficulty decreased significantly from 2007 to 2012 (APC: − 5.4, 95% CI − 8.2 to − 2.5) and decreased from 2012 to 2016 (APC: − 3.8, 95% CI − 7.9 to 0.4; Fig. 3).
Discussion
Our findings show that chewing difficulty trends are largely driven by a birth cohort pattern. The period effects suggest a very slight decline in chewing difficulty up to about 2010, followed by an unexpected (and unexplained) increase in chewing difficulty between 2010 and 2014. The cohort effect curve indicated declining rates of chewing difficulty in birth cohorts born after 1951.
Our findings suggest that social environments affect oral health outcomes, consistent with findings in other countries1,17. These results indicate that cohort succession may be the mechanism by which chewing ability has consistently shown an improvement over time in Korea25. As older cohorts—characterized by higher chewing difficulty—are replaced by younger cohorts, chewing ability improves overall. This suggests that older cohorts with poor oral health outcomes have been replaced by younger cohorts with better outcomes. Moreover, our findings are consistent with a cohort effect previously reported on population trends in the average number of teeth18.
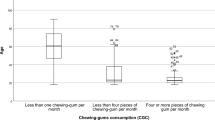
To explain the mechanisms underlying the association between birth cohort and chewing ability, it may be helpful to consider social conditions at multiple levels which affect oral health outcomes33. At the broadest level, social environmental change (e.g., the nutrition transition34,35,36) may have contributed to improved chewing ability among those born after the 1951 cohort. Babies born just after the Korean War experienced a dramatic change in nutritional environment (e.g. exposure to candy, and sweets)34,35, which may have set them up for poor oral health for the rest of their lives. The same nutrition transition has been linked to a shift in disease patterns, away from infectious diseases toward chronic diseases such as diabetes, cardiovascular disease, and cancer34. High caries is associated with the availability of sugar and this often happens when a country is undergoing rapid economic transition34,37,38. For example, in Kenya, the prevalence of dental caries was low (comparable to Ethiopia and Senegal) when the mean daily per capita supply of sugar was 50 g or less37. Dental caries increased in parallel with sugar consumption38. However, for a brief period after a country becomes integrated with the world economy, there is a huge influx of cheap and affordable “junk foods” (i.e., candy and sugary drinks), which leads to deterioration in oral health10,39. The prevalence of dental caries dramatically increased up to 1995, followed by a decline in recent years. For example, the mean number of decayed, missing, filled teeth (DMFT) was 0.6 in 1972, 3.1 in 1995, and down again to 1.4 in 2013–2015 among 12-year-olds3,40. More recent generations may not have the same exposure, i.e., educated parents became more strict about allowing their children to eat sweets4,41.
Fluoride exposure may contribute to oral health later in adulthood8,9,42,43, Contemporaneous and dose–response correlations have been identified42,43. Unfortunately, we could not highlight cohort effects of fluoride exposure due to limited data. In Korea, approximately 13% of the national population has been treated; community water fluoridation was implemented in 1981 and extended until 200344. Individuals could have potentially received exposure for up to 22 years (for those born in 1981). However, if this had a big effect, we would expect to find a dramatic decline in chewing difficulty for generations born after the late-1970s. But we could not find such an effect because the cohorts born after 1970 have not yet reached the age when people begin to develop chewing difficulty. Thus, further observation is warranted into the future.
We could not fully explain the period effect in our data, which appeared to show an unexpected increase in chewing difficulty between 2010 and 2014, before declining again (Fig. 1b). A period effect was identified in the APC model and confirmed using Joinpoint. That is, there was one slope change in the chewing difficulty trend. In addition, we confirmed changes in the linear trends against the alternative of one Joinpoint in the age-adjusted prevalence of chewing difficulty (Fig. 3). During this period, dental insurance coverage was expanded to include dental prosthetics treatment (starting in 2012) and dental scaling (starting in 2013). Older adults (aged 65 and older) are eligible for the former, while the latter is available for those aged 19 and over. However, it seems unlikely that these interventions could be responsible for changing oral health outcomes over the short time period25,45,46. Hence, our anomaly may be a measurement artefact47.
Some limitations should be considered when interpreting our findings. We could not consider the individual level factors that contributed to changes in chewing ability. Our analyses did not define birth cohort based on prior theory (i.e., Generation X) due to lack of evidence of their linkage to oral health. Another potential issue is that our age-effect shows that most people do not develop chewing difficulty until after age 60 because they still have enough teeth left. This means that we could not observe what happened to generations born after 1970, because they are still not old enough yet to develop chewing difficulty. It is possible that when the generation born after 1970 reach older ages, they will begin to show more chewing difficulty.
Conclusions
Our study showed that chewing ability improved over the previous decade. Regarding recent improvements in chewing ability, cohort effects were somewhat more important than period effects.
Data availability
The data from the fourth KNHANES is open to the public, therefore, any researcher can obtain data upon request from https://knhanes.cdc.go.kr. The Korean National Health and Nutrition Examination Survey (KNHANES) data are publicly available through the KNHANES website (https://knhanes.cdc.go.kr/knhanes/eng/sub03/sub03_01.do).
References
Luzzi, L., Chrisopoulos, S. & Brennan, D. S. Decline in usually visiting the dentist for a problem in Australia, 1994 to 2010: an age–period–cohort analysis. Commun. Dent. Oral Epidemiol. 42, 349–357. https://doi.org/10.1111/cdoe.12088 (2014).
Thomson, W. M., Williams, S. M., Broadbent, J. M., Poulton, R. & Locker, D. Long-term dental visiting patterns and adult oral health. J. Dent. Res. 89, 307–311. https://doi.org/10.1177/0022034509356779 (2010).
Kim, H. N., Kong, W. S., Lee, J. H. & Kim, J. B. Reduction of dental caries among children and adolescents from a 15-year community water fluoridation program in a township area, Korea. Int. J. Environ. Res. Public Health 16, 1306. https://doi.org/10.3390/ijerph16071306 (2019).
Lee, H. J. & Han, D. H. Exploring the determinants of secular decreases in dental caries among Korean children. Commun. Dent. Oral Epidemiol. 43, 357–365. https://doi.org/10.1111/cdoe.12160 (2015).
Matsuo, G., Aida, J., Osaka, K. & Rozier, R. G. Effects of community water fluoridation on dental caries disparities in adolescents. Int. J. Environ. Res. Public Health 17, 2020. https://doi.org/10.3390/ijerph17062020 (2020).
Lee, J.-H. et al. Factors related to the number of existing teeth among Korean adults aged 55–79 years. Int. J. Environ. Res. Public Health https://doi.org/10.3390/ijerph16203927 (2019).
Wen, Y. F., Chen, M. X., Wong, H. M. & Qiang, W. J. Trends in the burden of untreated caries of permanent teeth in China, 1993–2017: an age–period–cohort modeling study. Am. J. Prev. Med. 59, 896–903. https://doi.org/10.1016/j.amepre.2020.06.012 (2020).
Carey, C. M. B. A. M. S. P. Focus on fluorides: update on the use of fluoride for the prevention of dental caries. J. Evid. Based Dental Practice 14, 95–102. https://doi.org/10.1016/j.jebdp.2014.02.004 (2014).
Reid, D. J. & Dean, M. C. Variation in modern human enamel formation times. J. Hum. Evol. 50, 329–346. https://doi.org/10.1016/j.jhevol.2005.09.003 (2006).
Peres, M. A. et al. Oral diseases: a global public health challenge. The Lancet (British edition) 394, 249–260. https://doi.org/10.1016/s0140-6736(19)31146-8 (2019).
Raittio, E., Helakorpi, S. & Suominen, A. L. Age–period–cohort analysis of trends in toothache prevalence among 15- to 64-yr-old Finns over a 25-yr period. Eur. J. Oral Sci. 128, 66–73. https://doi.org/10.1111/eos.12677 (2019).
Seoane-Mato, D. et al. Trends in oral cavity, pharyngeal, oesophageal and gastric cancer mortality rates in Spain, 1952–2006: an age-period-cohort analysis. BMC Cancer 14, 254–254. https://doi.org/10.1186/1471-2407-14-254 (2014).
Bernabé, E. & Sheiham, A. Age, period and cohort trends in caries of permanent teeth in four developed countries. Am. J. Public Health 1971(104), e115–e121. https://doi.org/10.2105/ajph.2014.301869 (2014).
Bernabé, E. & Sheiham, A. Tooth loss in the United Kingdom—trends in social inequalities: an age-period-and-cohort analysis. PLoS ONE 9, e104808. https://doi.org/10.1371/journal.pone.0104808 (2014).
Bonifazi, M. et al. Age-period-cohort analysis of oral cancer mortality in Europe: the end of an epidemic?. Oral Oncol. 47, 400–407. https://doi.org/10.1016/j.oraloncology.2010.06.010 (2010).
Bravo, M.-P.-C. Age‐period‐cohort analysis of dentist use in Spain from 1987 to 1997. An analysis based on the Spanish National Health Interview Surveys. Eur. J. Oral Sci. 109, 149–154. https://doi.org/10.1034/j.1600-0722.2001.00010.x (2001).
Ahacic, K. & Thorslund, M. Changes in dental status and dental care utilization in the Swedish population over three decades: age, period, or cohort effects?. Commun. Dent. Oral Epidemiol. 36, 118–127. https://doi.org/10.1111/j.1600-0528.2007.00377.x (2008).
Kim, E.-S., Kim, B.-I. & Jung, H. I. Age, period and cohort trends in oral health status in South Korean adults. Commun. Dent. Oral Epidemiol. https://doi.org/10.1111/cdoe.12585 (2020).
Raittio, E., Helakorpi, S. & Suominen, A. L. Age-period-cohort analysis of toothbrushing frequency in finnish adults: results from annual national cross-sectional surveys from 1978 to 2014. Int. Dent. J. 71, 233–241. https://doi.org/10.1016/j.identj.2020.12.002 (2021).
Ramos, R. Q., Bastos, J. L. & Peres, M. A. Diagnostic validity of self-reported oral health outcomes in population surveys: literature review. Rev. Bras. Epidemiol. 16, 716–728. https://doi.org/10.1590/S1415-790X2013000300015 (2013).
Ueno, M., Shimazu, T., Sawada, N., Tsugane, S. & Kawaguchi, Y. Validity of self-reported tooth counts and masticatory status study of a Japanese adult population. J. Oral Rehabil. 45, 393–398. https://doi.org/10.1111/joor.12615 (2018).
Glied, S. & Neidell, M. The economic value of teeth. J. Hum. Resour. 45, 468–496. https://doi.org/10.3368/jhr.45.2.468 (2010).
Hyde, S., Satariano, W. A. & Weintraub, J. A. Welfare dental intervention improves employment and quality of life. J. Dent. Res. 85, 79–84. https://doi.org/10.1177/154405910608500114 (2006).
Matsuyama, Y., Tsakos, G., Listl, S., Aida, J. & Watt, R. G. Impact of dental diseases on quality-adjusted life expectancy in US adults. J. Dent. Res. 98, 510–516. https://doi.org/10.1177/0022034519833353 (2019).
Kim, N.-H., Chen, J. T. & Kawachi, I. Did expanded dental insurance improve chewing ability in the older Korean population? Results of an interrupted time-series analysis. J. Epidemiol. https://doi.org/10.2188/jea.JE20200417 (2020) (advpub).
Ebersole, J. L. et al. Aging, inflammation, immunity and periodontal disease. Periodontol. 2000(72), 54–75. https://doi.org/10.1111/prd.12135 (2016).
Consonni, D., Coviello, E., Buzzoni, C. & Mensi, C. A command to calculate age-standardized rates with efficient interval estimation. Stand. Genomic Sci. 12, 688–701. https://doi.org/10.1177/1536867X1201200408 (2012).
Rutherford, M. J., Lambert, P. C. & Thompson, J. R. Age-period-cohort modeling. Stand. Genomic Sci. 10, 606–627. https://doi.org/10.1177/1536867X1001000405 (2011).
Sasieni, P. D. Age-period-cohort models in stata. Stand. Genomic Sci. 12, 45–60. https://doi.org/10.1177/1536867X1201200104 (2012).
Wang, Y. & Liu, Q. Comparison of Akaike information criterion (AIC) and Bayesian information criterion (BIC) in selection of stock–recruitment relationships. Fish. Res. 77, 220–225. https://doi.org/10.1016/j.fishres.2005.08.011 (2006).
Institute, C. Cancer Institute, 2020. Joinpoint Regression Program (version 4.8.0.1). Availablefrom: (http://surveillance.cancer.gov/joinpoint). Access to July 10, 2020. version 4.8.0.1, (2012).
Dobson, A., Hockey, R., Chan, H.-W. & Mishra, G. Flexible age-period-cohort modelling illustrated using obesity prevalence data. BMC Med. Res. Methodol. 20, 16–16. https://doi.org/10.1186/s12874-020-0904-8 (2020).
Karonen, E. & Niemelä, M. Life course perspective on economic shocks and income inequality through age-period-cohort analysis: evidence from Finland. Rev. Income Wealth 66, 287–310. https://doi.org/10.1111/roiw.12409 (2020).
Soowon, K. I. M., Soojae, M. & Popkin, B. M. The nutrition transition in South Korea. Am. J. Clin. Nutr. 71, 44–53. https://doi.org/10.1093/ajcn/71.1.44 (2000).
Lee, M. K. The nutrition transition in Korea and Australia: child growth, infant mortality and diabetes. J. Nutr. Intermed. Metab. 1, 39–39. https://doi.org/10.1016/j.jnim.2014.10.140 (2014).
Popkin, B. M. What can public health nutritionists do to curb the epidemic of nutrition-related noncommunicable disease?. Nutr. Rev. 67, S79–S82. https://doi.org/10.1111/j.1753-4887.2009.00165.x (2009).
Sreebny, L. M. Sugar availability, sugar consumption and dental caries. Commun. Dent. Oral Epidemiol. 10, 1–7. https://doi.org/10.1111/j.1600-0528.1982.tb00352.x (1982).
Macigo, F. G., James, R. M., Ogunbodede, E. & Gathece, L. W. Sugar consumption and dental caries experience in Kenya. Int. Dent. J. 66, 158–162. https://doi.org/10.1111/idj.12208 (2016).
Armfield, J. M., Spencer, A. J., Roberts-Thomson, K. F. & Plastow, K. Water fluoridation and the association of sugar-sweetened beverage consumption and dental caries in Australian children. Am. J. Public Health 1971(103), 494–500. https://doi.org/10.2105/ajph.2012.300889 (2013).
Johng-bai, K. What do the public and profession know about dental caries prevention in Korea?. Int. Dent. J. 48, 399–404. https://doi.org/10.1111/j.1875-595x.1998.tb00702.x (1998).
van Loveren, C. Sugar restriction for caries prevention: amount and frequency. Which is more important?. Caries Res. 53, 168–175. https://doi.org/10.1159/000489571 (2019).
Neidell, M., Herzog, K. & Glied, S. The association between community water fluoridation and adult tooth loss. Am. J. Public Health 1971(100), 1980–1985. https://doi.org/10.2105/ajph.2009.189555 (2010).
Slade, G. D., Sanders, A. E., Do, L., Roberts-Thomson, K. & Spencer, A. J. Effects of fluoridated drinking water on dental caries in Australian adults. J. Dent. Res. 92, 376–382. https://doi.org/10.1177/0022034513481190 (2013).
Cho, H. J. et al. Systemic effect of water fluoridation on dental caries prevalence. Commun. Dent. Oral Epidemiol. 42, 341–348. https://doi.org/10.1111/cdoe.12091 (2014).
Kim, N.-H. & Kawachi, I. Did expanded access to denture services improve chewing ability in the Korean older population? Results of a regression discontinuity analysis. Sci. Rep. 10, 1–10. https://doi.org/10.1038/s41598-020-68189-7 (2020).
Kim, N. H. & Kawachi, I. Did the expansion of insurance coverage for oral health reduce self-reported oral health inequalities in Korea? Results of repeated cross-sectional analysis, 2007–2015. J. Epidemiol. 30, 537–541. https://doi.org/10.2188/jea.JE20190119 (2020).
Böhnke, J. R. & Croudace, T. J. Factors of psychological distress: clinical value, measurement substance, and methodological artefacts. Soc. Psychiatry Psychiatr. Epidemiol. 50, 515–524. https://doi.org/10.1007/s00127-015-1022-5 (2015).
Acknowledgements
We acknowledge the KCDC Committee members who provided crucial guidance of the data.
Author information
Authors and Affiliations
Contributions
All authors reviewed the manuscript. N.H.K drafted the original manuscript, acquired and analyzed the data, critically reviewed the manuscript, and conducted all statistical analyses. I.K. provided supervision throughout the drafting of the manuscript and revised the manuscript. I.K. also interpreted the study results and policy implications. All authors gave their final approval and agreed to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kim, NH., Kawachi, I. Age period cohort analysis of chewing ability in Korea from 2007 to 2018. Sci Rep 11, 14660 (2021). https://doi.org/10.1038/s41598-021-94086-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-94086-8
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.