Abstract
This study provides trends in obesity prevalence in adults from 2013 to 2016 in France. 63,582 men and women from independent samples upon inclusion from the Constances cohort were included. Anthropometrics were measured at Health Screening Centers and obesity defined as a Body mass index (BMI) ≥ 30 kg/m2; obesity classes according to BMI are as follows: class 1 [30–34.9]; class 2 [35–39.9]; class 3 [≥ 40 kg/m2]. Linear trends across obesity classes by sex and age groups were examined in regression models and percentage point change from 2013 to 2016 for each age category calculated. All analyses accounted for sample weights for non-response, age and sex-calibrated to the French population. Prevalence of obesity ranged from 14.2 to 15.2% and from 14 to 15.3% in women and men respectively from 2013 to 2016. Class 1 obesity category prevalence was the only one to increase significantly across survey years in both men and women (p for linear trend = 0.04 and 0.01 in women and men respectively). The only significant increase for obesity was observed in the age group 18–29 y in both women and men (+ 2.71% and + 3.26% point increase respectively, equivalent to an approximate rise of 50% in women and 93% in men, p = 0.03 and 0.02 respectively). After adjustment for survey non-response and for age and sex distribution, the results show that class 1 obesity prevalence has significantly increased in both women and men from 2013 to 2016, and only in young adults in a representative sample of the French population aged 18–69 years old.
Similar content being viewed by others
Introduction
The prevalence of obesity has rapidly risen from the beginning of the 1980s, reaching the count of more than 2 billion people affected worldwide in 20151. Obesity is an important risk factor for poor health such as cardiovascular diseases, type 2 diabetes, certain cancers, reduced life expectancy and mortality2, 3. Worldwide data based on 1698 studies has shown that the global prevalence of obesity has increased from 3.2 to 10.8% in men and from 6.4 to 14.9% in women between 1975 and 20141.
The prevalence of severe obesity in the United States (US) was 9.2% among adults in 2017–2018, women having a higher prevalence of severe obesity (11.5%) compared to men (6.9%). Severe obesity prevalence was the highest among adults aged 40–59 (11.5%) compared to adults aged 60 years old and above (5.8%)4.
In France, few studies have documented the prevalence of obesity with estimates ranging from 15 to 17.2% among adults5,6,7. The Obepi study was conducted every three years from 1997 to 2012 and was based on self-reported weight and height. The estimated prevalence in 2012 was 15%, reflecting an increase of 76.4% from the period of 1997–2009, a figure that has tapered off thereafter.
The Esteban study conducted by Public Health France has estimated that the prevalence of obesity was 17.2% in adults aged 18–74 years of age (n = 3,000). This study has also highlighted that the prevalence of obesity increased with age in both sexes (21.5% and 20.6% in men and women aged 55–74 years of age versus 10.1% and 11.3% in men and women aged 18–39 years old, respectively)6, 8. Cross sectional data from the Constances cohort conducted in 2013 on participants aged 30–69 has found a prevalence of obesity of 15.8% in men and 15.6% in women. The cross-sectional estimates of obesity prevalence in the aforementioned studies are somehow coherent but less is known about trends in obesity and severe obesity (i.e., grades of obesity) in France while analyzing independent samples with the same methodology and selection criteria, as well as throughout different age groups and socio-economic backgrounds. Moreover, representative data adjusting for survey non-response and for age and sex distribution of the French population is lacking. The main objective of this paper is to present the most recent trends in obesity prevalence using standardised operational protocols for weight and height measurements for survey years 2013–2016 among adults in France from the Constances cohort9. The second objective is to study the prevalence of obesity by lifestyle factors such as smoking and physical activity as well as its association with income and education.
Methods
Population
Constances is a large, population-based, prospective cohort whose recruitment began in 2012 and ended in 2019; it involves a total of more than 200,000 subjects, including volunteers aged 18–69 years at baseline, and living in 21 selected departments from a total of 26 sub-centers, which were not randomly selected, throughout metropolitan France, in both rural and urban settings10.
Participants were selected among individuals covered by the general insurance scheme or partner health mutual societies (in all, 85% of the French population) using a random sampling scheme stratified on place of residence, age, gender, occupation and socioeconomic status. Eligible individuals were invited to participate in the study by mail. Volunteers completed a self-administered questionnaire on socio-professional status, and attended a Health Screening Center for a comprehensive evaluation including a physical examination and laboratory tests.
The Constances cohort study has received the authorization of the French Data Protection Authority (Commission Nationale de l’Informatique et des Libertés, CNIL) and the institutional review board of the National Institute for Medical Research (Inserm) (Authorization number 910486) and all methods were performed in accordance with the relevant guidelines and regulations. All subjects included in this study gave their informed consent.
The present analyses were restricted to individuals with survey years 2013–2016, with complete baseline data on weight, height, age and sex, and were all affiliated to the General Social Security Regime. Pregnant women (N = 334) were excluded from the analyses. Details on participants’ selection by survey year (n = 63,582) are presented in Fig. 1.
Variables
Anthropometrics
Weight and height were measured in Health Screening Centers. Weight was measured using a non-automatic weighing instrument based on the recommendation of the International Organisation of Legal Metrology (OIML R 76-1, Edition 2006). Standing height is measured with a fixed stadiometer with a vertical backboard and a moveable headboard to the nearest 0.1 cm.
To determine obesity status, BMI was calculated using the following formula: weight (kg)/height (m2) and four categories were determined according to the World Health Organization criteria: underweight [BMI < 18.5]; normal weight [18.5–24.9 kg/m2]; overweight BMI [25–29.9 kg/m2]; and individuals with obesity BMI ≥ 30 kg/m2. BMI was modeled as a categorical variable: underweight, normal weight, overweight and obese. Obesity classes were defined as follows: class 1 [30–34.9]; class 2 BMI [35–39.9]; class 3 BMI [≥ 40 kg/m2].
Waist circumference
Waist circumference was measured in cm with a tape measure and abdominal obesity was defined according to two definitions: High Authority of Health [≥ 94 cm in men and ≥ 80 cm in women]; and National Cholesterol Education Program (NCEP) [> 102 cm in men and > 88 cm in women]. All anthropometric measurements were obtained following standardized procedures11, 12.
Socio demographic variables
The following variables were reported on a paper-based version baseline questionnaire.
Demographic
Age and sex were self-reported in the baseline questionnaire and age was further categorized into 5 groups: 18–29; 30–39; 40–49; 50–59; and 60–69 years.
Education
Education was measured using the following question: “What is the highest diploma that you have obtained?” Participants had to select among the following options: (1) no diploma; (2) general study certificate (equivalent to 12 years of school education); (3) certificate of professional aptitude; (4) high school diploma or equivalent; (5) undergraduate degree (2–3 years of study); (6) graduate degree (4 years of study); (7) graduate degree (≥ 5 years of study); or (8) other. Category 8 (other) has been combined with category 1 (no diploma) even though few individuals in category 8 had high diplomas but because of their small number they were not analyzed in a separate category.
Income
Income was measured by the following question: “What is the total amount of the net monthly income of your household? (i.e., the sum of all the incomes of people living in your household or your income if you live alone, regardless of the source of the income)?”. Participants had to select among the following options: (1) less than 450 euros; (2) 450 to less than 1000 euros; (3) 1000 to less than 1500 euros; (4) 1500 to less than 2100 euros; (5) 2100 to less than 2800 euros; (6) 2800–4200 euros; (7) more than or equal to 4200 euros; (8) don’t know how to answer; or (9) does not wish to answer. Categories 1 and 2 were further combined into one category (less than 1000 euros).
Other variables
Physical activity
Physical activity outside work was determined by a calculated score ranging from 0 (i.e., being not active at all) to 6 (being very active). Physical activity was further categorized into low (score of 0–2), medium (score of 3–4), and high (score of 5–6) level.
Smoking status
Smoking use (i.e., non-smoker, former smoker, or current smoker) was self-reported and smoking was modeled as a three category variable.
Statistical analyses
Participants’ characteristics by survey year are presented as percentages and 95% CI. Prevalence and 95% CI of BMI categories and obesity were calculated by survey year and are presented by age group, sex, income, education and smoking status. Further stratification was made by obesity classes (classes 1, 2 and 3).
Linear trends across obesity classes by sex, age group, categories for education and income were examined in regression models with four time points (survey years 2013–2016) modelled as an orthogonal polynomial and p values were reported.
Logistic regression models, further adjusting for age, sex, physical activity and smoking status and analysed separately for education and income were conducted in survey year 2016 to determine if obesity prevalence could be explained by these factors. Since education and income are highly associated we have chosen to separate both outcomes to show their respective strength of their association with obesity.
The choice of survey year 2016 (the most recent available survey year) to conduct the logistic regressions was made because the prevalence of obesity by education and income status was consistent across survey years and trends of difference from 2013 to 2016 were non-significant (results not shown).
Weighting and calibration
First, sample weights for non-response were performed using propensity scores in order to provide results representative of the French general population covered by the general health insurance scheme. A weighting coefficient has been computed for each subject by the CONSTANCES team. This coefficient took into account both the survey weight and the non-participation correction factor based on the follow-up of a control cohort of non-participants10, 13. The weights consider the variables that are associated to the probability of participation to the Constances cohort such as (but not limited to) sociodemographics, socio-professional categories, healthcare use and hospitalisations.
Second, we further calibrate for age and sex using the National Institute of Statistics and Economic Studies (Institut national de la statistique et des études économiques, INSEE) 2016 data which was performed by the ‘raking ratio’ method executed by proc Calmar in SAS. Independent samples upon inclusion to the Constances cohort from 2013 to 2016 were selected.
Age and sex distributions in the Constances study versus those of the French population are presented.
Tabular estimates for the prevalence of BMI categories (i.e., underweight, normal weight, overweight and obese) and obesity classes 1, 2 and 3 are presented by survey years, sex and age groups.
Analyses were conducted using SAS (SAS Institute) version 9.4. A 2-sided p value of 0.05 was used to assess statistical significance.
Results
Baseline characteristics
A total of 65,071 subjects affiliated to the General Social Security Regime from the Constances cohort were selected from survey years 2013–2016 (Fig. 1) and pregnant women (N = 334) were excluded. Among the selected sample, 1155 (1.8%) subjects had missing data on height and weight. Comparison of survey sample in the Constances study with the general French population is presented in Supplementary Table 1. The final sample is based on 63,582 subjects (Table 1) with half of the population being female, mean (SD) age was 44.4 (0.1) and 46.2 (0.1) years in women and men, respectively. About 65% of the population had baccalaureate degree or higher, a quarter was active smokers and a third had a low physical activity level. Abdominal obesity (≥ 88/102 cm, in women and men) ranged from 24 to 26% in women and from 17.2 to 20% of men.
Main findings
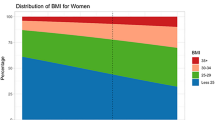
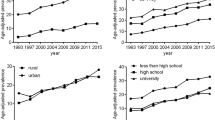
Prevalence of obesity ranged from 14.2% and 14% in women and men respectively in 2013 to 15.2% and 15.3% in 2016 (Fig. 2a,b). The trend for class 1 obesity category prevalence across survey years in both women and men was significant (p value for trend 0.04 and 0.01 respectively. Figure 3a,b show data of BMI categories by age groups and survey years, separately in men and women. In men, age and sex-adjusted estimates indicate that the prevalence of overweight and obesity prevalence in the 18–29 year-old category ranged from 24.4% in 2013 to 28.9% in 2016 and from 51.6 to 74.1% from 2013 to 2016 in participants ≥ 60 years old. In women, overweight and obesity prevalence from 2013 to 2016 ranged from 24.5 to 26.3% in the 18–29 year-olds and from 51.6 to 51.1% in individuals of 60–69 years old (all estimates are presented in Supplementary Table 2).
(a) Trends in obesity classes 1, 2 and 3 prevalence in women. Survey years 2013–2016. *Significant linear trend. P for trend estimated using the coefficients of orthogonal polynomials corresponding to linear contrast. P for linear trend for obesity grade 1 = 0.04 (F = 3.96), for obesity grade 2 = 0.27 (F = 1.20) and obesity grade 3 = 0.41 (F = 0.66). Age and sex-adjusted by the raking ratio method using the Insee data and age groups 18–29, 30–39, 40–49, 50–59, and 60–69 years. Dashed lines are confidence intervals. (b) Trends in obesity classes 1, 2 and 3 prevalence in men. Survey years 2013–2016. *Significant linear trend. P for trend estimated using the coefficients of orthogonal polynomials corresponding to linear contrast. P for linear trend for obesity grade 1 = 0.01 (F = 5.59), for obesity grade 2 = 0.32 (F = 0.97) and obesity grade 3 = 0.15 (F = 0.69). Age and sex-adjusted by the raking ratio method using the Insee data and age groups 18–29, 30–39, 40–49, 50–59, and 60–69 years. Dashed lines are confidence intervals.
(a) BMI categories by age and survey year in men (N = 30,783). Empty bars indicate a prevalence of less than 10 cases and are not represented. Age and sex-adjusted by the raking ratio method using the Insee data and age groups 18–29, 30–39, 40–49, 50–59, and 60–69 years. (b) BMI categories by age and survey year in women (N = 32,799). Age and sex-adjusted by the raking ratio method using the Insee data and age groups 18–29, 30–39, 40–49, 50–59, and 60–69 years.
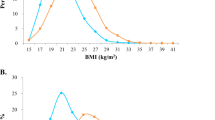
Tables 2 and 3 indicate the prevalence of obesity by sex by and age groups according to survey year. An increasing gradient across age groups was observed at every survey year. From 2013 to 2016, the only significant linear trends was observed in the age group 18–29 in both women and men (p value for trend = 0.01), as well as a significant increase of + 2.71% and 3.26% point, equivalent to a 50% and 93% rise in obesity prevalence in women and men respectively, p for change from 2013 to 2016 = 0.03 and 0.02). The other age categories did not reach statistical significance neither for linear trends across survey years or point change between 2013 and 2016 in both sexes. Prevalence of obesity according to baseline characteristics and survey year is described in Table 4. Smokers had lower obesity prevalence compared to ex-smokers and physically active individuals had the lowest prevalence of obesity. Irrespective of the survey year, a strong decreasing gradient was observed with both education and income levels. As an example, for survey year 2016, the prevalence of obesity for those with no diploma was 29.5%, whilst those with a baccalaureate plus 5 years of education and more exhibited 7.3% prevalence. ORs and 95% CI of obesity in individuals with a monthly income lower than 1000 euros were 2.4 (1.8–3.2) compared to those with an income above 4200 euros and 3.4 (2.4–4.8) in individuals without a diploma compared to those having a graduate degree of more than 5 years of study, these results are presented in Fig. 4a,b.
(a) ORs and 95% of obesity by income categories using multivariate logistic regression with weighted and age and sex-adjusted estimates in survey year 2016. Model adjusted for age, sex, smoking and physical activity level. Interaction of survey year was tested with each characteristic in the model and was not significant. Linear trend across income characteristic is significant (p < 0.0001). Age and sex-adjusted by the raking ratio method using the Insee data and age groups 18–29, 30–39, 40–49, 50–59, and 60–69 years. (b) ORs and 95% of obesity by education categories using multivariate logistic regression with weighted and age and sex-adjusted estimates in survey year 2016. Model adjusted for age, sex, smoking and physical activity level. Interaction of survey year was tested with each characteristic in the model and was not significant. Linear trend across education characteristic is significant (p < 0.0001). Age and sex-adjusted by the raking ratio method using the Insee data and age groups 18–29, 30–39, 40–49, 50–59, and 60–69 years.
Linear trends in abdominal obesity prevalence by age groups and sex are presented in Supplementary Tables 3a and 3b.
Discussion
We took advantage of the Constances cohort to surface linear trends of obesity prevalence in independent samples through survey years 2013–2016.
In the present analyses, class 1 obesity prevalence increased in both men and women (9.1–10.6% in women and 10.7–12.3% in men) from 2013 to 2016, whereas the other obesity classes (2 and 3) remain relatively stable across this time span in both sexes.
In addition, we have determined linear trends of obesity by sex across age groups; in these subgroup analyses, linear trends have only significantly increased in the youngest adults (i.e., 18–29 years of age) in both women and men. We have not observed any significant changes across the other age groups. The rising trends in obesity found in Constances from 2013 to 2016, even though only significant for obesity class 1 and for young adults; do not show a massive rise in global obesity similar to that seen from 1997 to 2009 in Obepi (which had shown an increase of 76.4%)5, 14. It should be noted however that weight and height data have been declared in the French Obepi study compared to Constances, this may have led to underestimation in obesity prevalence in Obepi which varies with age, sex and period. Our results are more comparable to the Esteban study in France, which is based on measured anthropometrics and shows that from 2006 to 2015, obesity prevalence has been relatively stable at around 17% in adults’ men and women. In fact, data from several countries show a decline or stabilization of obesity levels, albeit with a mixed evidence, data from 2015 to 2016 prevalence indicating no evidence of a decline in obesity at any age15.
Recent data from the United States has shown that although from 1999–2000 through 2017–2018, the prevalence of global obesity and also severe obesity have increased, the most recent period of interests between 2015–2016 and 2017–2018 did not show a significant increase (5). It remains that we have observed a significant increase in individuals with obesity class 1, but not in individuals with obesity classes 2 and 3.
We have also found a 50% increase in women and 93% increase in men young adults. This finding is not consistent with data from the United States that shows no evidence for an increase in obesity in 2015–2016 versus 2017–2018 among individuals aged 20–39 years old, the prevalence being much higher than that in France (40%) which might suggest a slight tapering off at increased levels of obesity in this age group in the United States4. In the Constances cohort, even if the latest prevalence in this subgroup is not very high (7.7%), such an increase over a four year period is worrying. Our findings indicate that young adults should not be overlooked in health-policy making with regard to obesity. Since obesity is higher in low income statuses and the increase in poverty across years in the young groups may explain our finding, we have looked at the prevalence of different income categories across survey years, but have not found an increase in the prevalence of low income groups (results not shown).
We have further analyzed linear trends of obesity in young individuals among employees and students, and found out that obesity increased significantly in young employees (p for trend < 0.0001) but not students. This additionally highlights the social inequalities with regard to obesity as students who have access to education are less likely to be affected by this increase. This is also in line with our finding on the higher prevalence of obesity among individuals with lower education and income. Although the reason behind such an increase among young individuals and no other remains to be determined, the result of such an increase in Constances could be attributed to peer social transmission and non-social mechanisms. Researchers studying dynamic simulation models to understand how underlying population age structure and different mechanisms influence trends of obesity, have shown that obesity prevalence was most sensitive to adult parameters (such as social interactions, interplay of individual behaviors and norms)15. Our results show a somehow lower prevalence of obesity in the four study points compared to the Esteban study which was also based on measured anthropometrics and has found a prevalence of obesity of 17% in adults aged 18–74 years. Our study is consistent with Esteban in that it shows a higher prevalence of obesity in the 40–69 age groups compared to younger adults (18–39).In addition, we have observed a significant higher prevalence of obesity among individuals with lower education or income, even after adjustment for age, sex, physical activity and smoking status in multivariate models. It should be noted however that income was not measured per unit of consumption but rather as net monthly revenue for the household. Income in our analyses was measured through a range of pre-specified categories and we were able to find a linear trend of increase in the prevalence of obesity going from high to lower income categories. This is consistent with our previous finding in the Constances cohort among 30–69 year-old participants (15). To further test whether obesity prevalence has increased among different income or education categories, we have tested linear trends from 2013 to 2016 and have observed that results are not significant (results not shown herein); in other words obesity prevalence has not changed significantly in the same category of income or education across survey years; thus obesity remains high in the most financially deprived individuals and lower in the more privileged participants.
Our finding of higher obesity prevalence among lower education and income groups is consistent with other studies. Results from the French Abena study have shown that adult women relying on food aid programs had two times more obesity prevalence compared to the general population (35% vs. 15%)16. In the United States during 2011–2014, the age-adjusted prevalence of obesity among adults was lower in the highest income group (31.2%) than the other groups and the age-adjusted prevalence of obesity among college graduates was lower (27.9%) than among those with some college (40.6%)17.
One reason for the association between low education and income and obesity may be psychosocial stress and this exposure may mediate the relationship between poverty and increased obesity risk18. Additionally, low income may be associated with an increased risk of obesity by the limited access to healthy food and the toxic environment leading to low physical activity levels18. This highlights the relevance of public health programs to focus on healthier environments for the reduction of obesity prevalence among the most deprived individuals.
Interestingly, we have found a significant linear trend in older adults men (60–69 years) for abdominal obesity in men (waist circumference ≥ 94 cm) but not in women. Although, obesity rates have not increased significantly in this subgroup, adults aged 60–69 years old are at risk of developing abdominal obesity.
Strengths and limitations
The strengths of our study include the large sample and the design of the Constances cohort that have allowed us to study trends in obesity prevalence by selecting independent samples of participants upon inclusion. All anthropometric data have been collected at Health Screening Centers (HSC) in France and routine protocols and checkups have been conducted by specialized teams12. Moreover, the calculated weightings for non-response that are taken into consideration with such complex survey design, have allowed us to render the analyzed sample representative of the Constances’ population and all estimates were age and sex-adjusted according to the INSEE data. Moreover, to our knowledge, this study provides recent trends with several time points of obesity prevalence in France.
Limitations include the low number of survey years included in our analyses (4 years). These four time points were able to provide a statistical estimation of a linear trend, however we are cognizant that more time points are needed to provide a better estimation of this linear variation. Additionally, the results are representative of the population affiliated to the General Social Security Regime and aged between 18–69 years old and cannot be representative of the French population. We have used the INSEE data to adjust for the age and sex distribution of the French population but are cognizant that this may differ from the Constances’ cohort population”, particularly because certain socio professional categories (with a low prevalence in our sample) are not represented in Constances, such as independent workers, farmers and craftsmen.
Our findings of an increase in the obesity class 1 category, and among the 18–29 age group, need to be interpreted with caution, as it is important to note that analysis of time trends depends on the initial point of examination (16). We have selected the first year of inclusion of participants in Constances as a starting point (2013); however a comparison between different starting time points may lead to different interpretations.
Conclusion
Overall, there have been significant changes in obesity prevalence in the obesity class 1 category in both men and women. Obesity classes 2 and 3 remained stable across survey years. An increase of 50% and 93% (women and men) in obesity prevalence was found in young adults aged 18–29 years between 2013–2016, whereas it did not reach significance in the other age subgroups. Obesity prevalence remained high in the most socially deprived or less educated individuals. More survey points are needed to draw conclusions about the rising trends of obesity in France, whilst it remains important to monitor its prevalence.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Swinburn, B. A. et al. The global syndemic of obesity, undernutrition, and climate change: The Lancet Commission report. The Lancet 393(10173), 791–846 (2019).
Panel, O. E. Managing overweight and obesity in adults: Systematic evidence review. Bethesda, MD: National Heart, Lung and Blood Institute, NIH, US DHHS. 2013.
Bhaskaran, K., dos-Santos-Silva, I., Leon, D. A., Douglas, I. J. & Smeeth, L. Association of BMI with overall and cause-specific mortality: A population-based cohort study of 3· 6 million adults in the UK. Lancet Diabetes Endocrinol. 6(12), 944–953 (2018).
Hales, C. M., Carroll, M. D., Fryar, C. D. & Ogden, C. L. Prevalence of obesity and severe obesity among adults: United States, 2017–2018. 2020.
Diouf, I. et al. Evolution of obesity prevalence in France: An age-period-cohort analysis. Epidemiology 21(3), 360 (2010).
Castetbon, K. et al. Dietary intake, physical activity and nutritional status in adults: The French nutrition and health survey (ENNS, 2006–2007). Br. J. Nutr. 102(5), 733–743 (2009).
Matta, J. et al. Prévalence du surpoids, de l’obésité et des facteurs de risque cardio-métaboliques dans la cohorte Constances. Bull. Epidemiol. Hebd. 35, 640–646 (2016).
Etude ESTEBAN 2014–2016—Chapitre corpulence : stabilisation du surpoids et de l’obésité chez l’enfant et l’adulte. Santé publique France-Volet Nutrition 2014–2016; Chapitre Corpulence 7.
Zins, M. et al. The CONSTANCES cohort: An open epidemiological laboratory. BMC Public Health 10(1), 1–9 (2010).
Zins, M. & Goldberg, M. The French CONSTANCES population-based cohort: Design, inclusion and follow-up. Eur. J. Epidemiol. 30(12), 1317–1328 (2015).
Ruiz, F. et al. High quality standards for a large-scale prospective population-based observational cohort: Constances. BMC Public Health 16(1), 877 (2016).
Santin, G. et al. Estimation de prévalences dans Constances: Premières explorations. Bull. Epidémiol. Hebd. 35(36), 622–629 (2016).
Charles, M.-A., Eschwege, E. & Basdevant, A. Épidémiologie de l’obésité de l’adulte en France Les études Obépi 1997–2006. Obésité 3(4), 258–263 (2008).
Frerichs, L., Araz, O. M., Calancie, L., Huang, T. T. K. & Hassmiller, L. K. Dynamic empirically based model for understanding future trends in US obesity prevalence in the context of social influences. Obesity 27(10), 1671–1681 (2019).
Vernay, M. et al. Facteurs socioéconomiques associés à l’obésité parmi les femmes ayant recours à l’aide alimentaire en France. Étude Abena 2011–2012. Bull. Epidémiol. Hebd. BEH 18–19, 317–325 (2014).
Ogden, C. L. et al. Prevalence of obesity among adults, by household income and education—United States, 2011–2014. MMWR Morb. Mortal. Wkly. Rep. 66(50), 1369 (2017).
Kwarteng, J. L., Schulz, A. J., Mentz, G. B., Israel, B. A. & Perkins, D. W. Independent effects of neighborhood poverty and psychosocial stress on obesity over time. J. Urban Health 94(6), 791–802 (2017).
Acknowledgements
The authors thank the INSERM-Versailles Saint Quentin en Yvelines University "Population-based Epidemiologic Cohorts Unit” (Cohortes épidémiologiques en population) which designed and manages the Constances Cohort Study. They also thank the National Health Insurance Fund (“Caisse nationale d’assurance maladie des travailleurs salaries”, CNAMTS) and its Health Screening Centres (“Centres d’examens de santé"), which are collecting a large part of the data, as well as the National Old-Age Insurance Fund (Caisse nationale d’assurance vieillesse) for its contribution to the constitution of the cohort, ClinSearch, Asqualab and Eurocell, which are conducting the data quality control.
Funding
The Constances cohort is supported by the National Health Insurance Fund (“Caisse nationale d’assurance maladie des travailleurs salaries”, CNAMTS), the ministry of health, the ministry of research and the National Institute for Health and Medical Research. The Constances Cohort benefits from a grant from ANR (ANR-11-INBS0002). Constances is also partly funded by MSD, AstraZeneca, Lundbeck and l’Oréal handled by INSERM.
Author information
Authors and Affiliations
Contributions
S.C. and J.M. take responsibility for all aspects of the reliability and freedom from bias of the data presented and their discussed interpretation. S.C. and J.M. designed the study; M.G. and M.Z. acquired the data; J.M. and A.R. performed statistical analysis. AR calculated weightings for non-response in the Constances cohort. All authors contributed to the interpretation of data. SC and JM drafted the article; A.R., C.R.L., C.C., G.A., E.W., A.O., S.K., M.G. and M.Z. revised it critically for important intellectual content. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
Sébastien Czernichow has received honoraria from Novo Nordisk, Sanofi, Lilly, Janssen, Servier, Novartis, fitforme, BMS and Fresenius outside the present work. He owns shares of Mygoodlife and serves as a member of the scientific advisory board of Bariatek. Claire Carette has received honoraria from Astra Zeneca, Lilly, Novo Nordisk, Novartis Pharma, MSD France, IPSEN Pharma, Pfizer, Publicis Health outside the presented work. Guillaume Airagnes has received speaker and/or consulting fees from Pierre Fabre, Lundbeck, Pfizer and MasterClass Santé. Claire Rives Lange reports personal fees from Nestlé Health Sciences and Fitforme. The other authors have nothing to declare.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Czernichow, S., Renuy, A., Rives-Lange, C. et al. Evolution of the prevalence of obesity in the adult population in France, 2013–2016: the Constances study. Sci Rep 11, 14152 (2021). https://doi.org/10.1038/s41598-021-93432-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-93432-0
This article is cited by
-
Impact of obesity on morbidity and oncologic outcomes after total mesorectal excision for mid and low rectal cancer
Techniques in Coloproctology (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.