Abstract
The study aims to determine the prevalence of strabismus and its risk factors among school children in Hong Kong. This is a cross-sectional study involving 6–8 year old children from different districts in Hong Kong. 4273 children received comprehensive ophthalmological examination, cycloplegic auto-refraction, best corrected visual acuity (BCVA), anterior segment examination, cover/uncover test, ocular motility, and fundus examination. Demographic information, pre- and post- natal background, parental smoking status, and family history of strabismus were obtained through questionnaires. Strabismus was found among 133 children (3.11%, 95% CI 2.59–3.63%), including 117 (2.74%) exotropia and 12 (0.28%) esotropia cases (exotropia-esotropia ratio: 9.75:1). There was no significant difference in prevalence across age (6–8 years) and gender. Multivariate analysis revealed associations of strabismus with myopia (≤ − 1.00D; OR 1.61; 95% CI 1.03–2.52; P = 0.037) hyperopia (≥ + 2.00D; OR 2.49; 95% CI 1.42–4.39; P = 0.002), astigmatism (≥ + 2.00D; OR 2.32; 95% CI 1.36–3.94; P = 0.002), and anisometropia (≥ 2.00D; OR 3.21; 95% CI 1.36–7.55; P = 0.008). Other risk factors for strabismus included maternal smoking during pregnancy (OR 4.21; 95% CI 1.80–9.81; P = 0.001), family history of strabismus (OR 6.36; 95% CI 2.78–14.50, P < 0.0001) and advanced maternal age at childbirth (> 35 years; OR 1.65; CI 1.09–2.49, P = 0.018). The prevalence of strabismus among children aged 6—8 years in Hong Kong is 3.11%. Refractive errors, family history of strabismus and maternal smoking history during pregnancy are risk factors. Early correction of refractive errors and avoidance of maternal smoking during pregnancy are potentially helpful in preventing strabismus.
Similar content being viewed by others
Introduction
Strabismus is an important cause of amblyopia and other visual impairments among school children1. It is associated with reduced visual function and eye-related quality of life in children and also affects quality of life of their parents2. Early detection and appropriate intervention can improve binocularity and prevent occurrence of permanent visual deficits3.
Epidemiologic studies on strabismus and its risk factors among preschool and school-aged children have been conducted in different populations of different living environments. The Multi-Ethnic Pediatric Eye Disease Study (MEPEDS) included children of Asian and Caucasian descent in the United States1,4. Similar strabismus prevalence was reported among Hispanic/Latino (2.4%) and African-American children (2.5%)1. The Baltimore Pediatric Eye Disease Study (BPEDS) was on white and African American children3. The prevalence of strabismus was found to be 3.3% and 2.1% among White and African Americans respectively. The Strabismus, Amblyopia, and Refractive Error in Singaporean Children Study (STARS) was conducted in Singapore among children of dominant Chinese ethnicity5. According to their study, the prevalence of strabismus among children (6 to 72 months) was found to be 0.84%. Notably, their exotropia to esotropia (7:1) was similar to that our data (9.75:1). Similar study conducted in Asia, the Korea National Health and Nutrition Examination Survey detected a strabismic prevalence of 1.6% among children and adolescents aged from 5 to 186. In Hong Kong, epidemiological data on strabismus is not known although it is needed for health care policies. It is expected to be different from other populations due to differences in ethnicity and environmental factors1,4. In this study, we aim to determine the prevalence and risk factors of strabismus in Chinese children aged 6–8 years in Hong Kong.
Methods
Study design and population
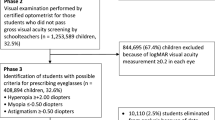
The study subjects were recruited from the Hong Kong Children Eye Study (HKCES)7,8,9,10, which is a population-based cohort study of eye conditions among children aged 6–8 years old in Hong Kong. The HKCES was designed to determine the occurrence and development of eye disorders, including refractive errors, strabismus, amblyopia, and allergic disease, and to identify their environmental and genetic determinants11,12,13. According to previous studies, the prevalence of strabismus ranged from 1.9314 to 5.65%15 across various regions in China. Assuming a design effect of 2.0, type 1 error of 0.05, and 20% loss to follow-up; a sample size of 4355 children is required to provide over 80% of statistical power to reject the null hypothesis. A total sample of 5000 children were invited.
The sample selection was completed based on a stratified and clustered randomized sampling frame. We stratified all Education Bureau registered primary schools (n = 571) into the 7 cluster regions used by the Hospital Authority Services in Hong Kong. This division into seven clusters is determined by Hong Kong Government according to even distribution of population density in each cluster. Therefore, 714 children should be recruited from each cluster region. The schools in each cluster region were randomly assigned an invitation priority according to the ranking numbers generated by computer. Details of sample size considerations and protocols are described in the previous report8. Children attending the territory-wide Hong Kong Children Eye Study from all regions over Hong Kong were invited to this study. All the participating children were ethnic Chinese. Children aged 6 to 8 years old in the sampling frame were included in the study. The exclusion criteria was that children older/ younger than the aforementioned age group were not in the sampling frame. The study adhered to the Declaration of Helsinki. The study protocol was approved by the Ethics Committee Board of the Chinese University of Hong Kong. All children and their parents signed a written informed consent upon their participation in the study.
Ocular examinations
Distance visual acuity (VA) was measured using a logarithm of the minimum angle of resolution (LogMAR) chart (Nidek, Gamagori, Japan). In the case of uncorrected VA in either eye being > 0.1, best-corrected visual acuity (BCVA) was subsequently measured in a monocular fashion using a trial frame. Refractive status was measured both before and after cycloplegia using an auto-refractor (Nidek ARK-510A, Gamagori, Japan). Two cycles of 1% cyclopentolate (Cyclogyl, Alcon-Convreur, Rijksweg, Belgium) and 1% tropicamide (Santen, Osaka, Japan) were given ten minutes apart. An additional third cycle of cyclopentolate and tropicamide drops was administered thirty minutes after the last drop if either a pupillary light reflex was still present, or pupil size was less than 6.0 mm. Detailed ocular examinations for the anterior segment and the retina were conducted by an ophthalmologist using a slit-lamp (Haag-Streit, Koeniz, Switzerland) and binocular ophthalmoscope with a 20D lens (Volk, Houston, TX) respectively.
Definition and assessment of ocular alignment
Ocular alignment was taken before cycloplegia with habitual optical correction, if worn. It was evaluated by an ophthalmologist using both the unilateral cover (cover / uncover) test and an alternate cover and prism test. Both tests were administered at near (30 cm) and distance (6 m) fixations, as well as both with and without optical correction if the study subject used any corrective methods. A prism cover test was performed to detect the degree of eye misalignment. A transient misalignment found during alternate cover testing was not defined as strabismus unless confirmed by a repeat unilateral cover test.
Strabismus cases were classified according to the direction of the tropia as esotropic, exotropic, or vertical. A case was considered as a constant tropia if it was constant at both near and distance fixations. Otherwise it was considered as an intermittent tropia. Spherical equivalent (SE) was calculated as the sum of the spherical power plus half of the cylindrical power using cycloplegic refraction. The worse eye was delineated as the eye with the higher absolute value of the SE refractive error.
Questionnaires
Parents or child carers were asked to complete background information questionnaires, assisted by a trained staff member either in person or over the telephone8,10. The information collected included the family demographics and parental data regarding smoking history, alcohol use, the gestational week at delivery, and family histories of eye diseases. Smoking history data was further classified into two types: “maternal smoking during pregnancy” and “maternal smoking,” Each Habitual smoker was asked by the question:” did you quit smoke or continue smoke during pregnancy?” Maternal smoking during pregnancy is defined by whether the mother has ever smoked during pregnancy. Habitual smokers who quit smoke during pregnancy were not defined as “maternal smoking during pregnancy” Regarding gestational data, a low birth weight was defined as being < 2.5 kg, while gestational age was classified for babies born at < 32, 32–36, 37–42, and > 42 weeks respectively16. All this information was collected to aid the study in terms of identifying possible risk factors of the development of strabismus among the children in Hong Kong.
Statistical analysis
Stata (version 14.0, StataCorp LP, College Station, TX) was used for all statistical analyses. Confidence intervals (CIs) and P values (significant at levels < 0.05) for prevalence estimates and regression models were calculated with adjustments for cluster effects associated with the sampling design. A multivariate logistic regression was used to investigate the associations of age, gender, and refractive error with strabismus. Risk factors were first explored using a univariate analysis; those which showed at least a marginally significant association (P < 0.1) were then considered as candidates for a subsequent forward stepwise multivariate logistic regression. Odds ratios (ORs) and 95% confidence intervals (95% CIs) were calculated to determine significant independent risk factors, which were hence included in the final model.
Results
Study population
A total of 4273 children (2236 boys and 2037 girls) responded to the invitation and completed ophthalmological examinations. The response rate was 85.46%. Participating children were 6–8 years old, with a mean (± SD) age 7.61 ± 0.98 years.
Prevalence and types of strabismus
A total of 133 children (3.11%) were identified as strabismic, with the prevalence being similar across age and gender (P = 0.429 and P = 0.417 respectively; Table 1). Among them, 117 exhibited concomitant exotropia (63 intermittent, 54 constant-type); 12 exhibited concomitant esotropia; and 4 exhibited purely vertical strabismus. Exotropes outnumbered esotropes by a ratio of 9.75:1. (Table 2) Incomitant deviations were excluded in the analysis. Three children had history of incomitant strabismus. They received treatment due to severe diplopia (1 case) and compensatory head posture (2 cases) and recovered before they attended in the study.
Associations of strabismus with different types of refractive errors
Strabismus was associated with myopia (≤ − 1.00D; OR 1.72; P = 0.012), hyperopia (≥ + 2.00D; OR 2.56; P = 0.001), moderate astigmatism (≥ 2.00D; OR 2.33; P = 0.048) and severe anisometropia (≥ 2.00 D; OR 2.47; P < 0.0001). (Table 3).
Associations of strabismus with parental factors
Among the children in this study, 3959 (92.6%) had a parent or child carer who completed the associated questionnaire. There were no significant differences between the children who had a completed questionnaire and those who did not, in age, gender, SE refractive errors, and prevalence of strabismus. (Supplementary Table S1).
In the univariate analysis, maternal smoking was associated with strabismus. Children whose mothers were habitual smokers were prone to developing strabismus, with prevalence as high as 6.88% (P = 0.006). For those children whose mothers smoked during pregnancy, the risk was almost doubled to 11.86% (P = 0.002). Other risk factors identified in this analysis included premature birth (P = 0.025), advanced maternal age (P = 0.015), and family history of strabismus (P = 0.001). (Table 4) In the multivariate analysis, strabismus was associated with maternal smoking during pregnancy (OR 4.21; 95% CI 1.80–9.81; P = 0.001), family history of strabismus (OR 6.35; 95% CI 2.78–14.50; P < 0.0001) and advanced maternal age (OR 1.65, 95% CI 1.09–2.49; P = 0.018), and refractive errors (Table 5).
Discussion
In this population-based study of ethnic Chinese school children in the highly urbanized and densely populated city of Hong Kong, we report a prevalence rate of 3.11% for strabismus, which was similar across gender and ages from 6 to 8 years old (Table 1). It is higher than results reported from other populations Japan (6–12 years old, 0.99%)17,18, Singapore (0.5–6 years old, 0.84%)5, Mexico (2.3%)19, and Sydney, Australia (2.8%)20 (Supplementary Table S2). MEPEDS previously found that among Asian children with strabismus, exotropia (prevalence, 2.10%; 95% CI 1.44–2.96) was more common than esotropia (prevalence, 1.38%; 95% CI 0.18–2.10)1. The exotropia:esotropia ratio was much lower, at 1.5:11. In contrast, most of the strabismic children in the current study had exotropia, 117, while 12 children had esotropia. The prevalence of exotropia was 2.64% (113/4273) and esotropia 0.28% (12/4273), with an exotropia:esotropia ratio of 9.4:1. In STARS conducted in Singapore, where the majority population of Chinese descent is similar to Hong Kong, has shown significantly similar ratio of 7:15. This evidence demonstrates a higher prevalence of exotropia in Chinese population among Asians. Our high prevalence of strabismus could be owing to the high prevalence of myopia in this locality. According to a meta-analysis study conducted in 2016 involving 23,541 subjects, it was found that myopia was an independent risk factor for exotropia with odd ratio 5.23. The study had postulated that the fusional control at distant sight among myopes was weakened; whereas for near vision, owing to the large accommodation lag, less accommodative effort was needed. As the result, less accommodative convergence was stimulated. It was believed that the prolonged suboptimal convergence would cause breakdown of the fusional control and subsequently predispose to the development of exotropia21.
Most of the strabismic children in the current study had exotropia, 117 out of 133 (84.96%). The next common was esotropia, 12 out of 133 (9.02%). In this study prevalence of exotropia was 2.64% (113/4273) and esotropia 0.28% (12/4273), with an exotropia:esotropia ratio of 9.4:1. MEPEDS previously found that among Asian children with strabismus, exotropia (prevalence, 2.10%; 95% CI 1.44–2.96) was more common than esotropia (prevalence, 1.38%; 95% CI 0.18–2.10)1. The exotropia:esotropia ratio was much lower, at 1.5:1. In STARS, it was concluded that exotropia represented 83.3% of strabismus cases among Singaporean5, similar to the 84.96% in Hong Kong Chinese children in this study.
We discovered a significant risk for children with a family history of strabismus, as represented by an OR of 6.35 (95% CI 2.78–14.50, P < 0.001). This is consistent with another study conducted in Korea22, which quantified the association of family history with strabismus as an OR of 4.91 (95% CI 1.71–14.08; P = 0.003). In addition, both MEPEDS1 and BPEDS3 have also reported a two-fold increase in the risk of developing exotropia among subjects with a family history of strabismus.
Our univariate analysis discovered that maternal smoking, low birth weight, premature birth with a gestational age lower than 32 weeks, and advanced maternal age over 35 years old were all associated with childhood strabismus. In particular, low birth weight, and early gestational age are partly attributed to maternal smoking history, since maternal smoking can give rise to unfavourable pregnancy outcomes23,6 including low birth weight23 and premature birth6. Furthermore, excluding other factors in the stepwise multivariate logistic regression model, maternal smoking during pregnancy was independently highly associated with strabismus with an OR of 4.21. At present, the exact causative mechanism of how prenatal exposure to tobacco would lead to strabismus or poor pregnancy outcomes has not been established. Nevertheless, since the developing foetus is directly exposed to maternal placenta, it is believed that tobacco may induce neurotoxic effects on the foetal nervous system16. Greater emphasis should therefore be given to examining how maternal smoking can cause detrimental effects on a child’s vision during pregnancy, including strabismus. Moreover, maternal smoking is a modifiable risk factor, education should be promoted to raise public awareness. On the other hand, future studies should investigate the exact dosage relationship between tobacco smoking and the development of strabismus. Regarding other non-ocular risk factors, advanced maternal age (> 35 years old) carried a P-value of 0.018 upon multivariate regression analysis. Although children whose mothers gave birth at an advanced age are generally prone to higher risks of adverse effects, the exact causative mechanism of how advanced age is associated with strabismus is yet to be found.
The associations we found for refractive errors of myopia, hyperopia, astigmatism, and anisometropia with strabismus are generally consistent with other publications21,24. A meta-analysis involving 23,541 children showed that myopia resulted in an increased risk of developing concomitant strabismus, and that there was a strong association between hyperopia and concomitant strabismus8. In this study, multivariable analysis showed that myopia (P = 0.037) and hyperopia (P = 0.002) were both associated with strabismus. In addition, astigmatism (≥ 2.00D, p = 0.002) and anisometropia (≥ 2.00D, P = 0.008) were independently associated with strabismus.
The strengths of our study include its population-based design, relatively large sample size, and standardized methods for sampling and examination. Our study is a territory-wide study and study subjects were from all 18 districts of HK. In addition, all participants were invited to our clinic to receive comprehensive ophthalmological examinations. We maintained proper examination techniques and examination room settings throughout the entire study to achieve high sensitivity and specificity for diagnosing strabismus. These facilities enabled detection of mild cases of strabismus, such as microstrabismus, heterotropia, and heterophoria. In particular, refractive status was measured for all participants both before and after cycloplegia to obtain an accurate assessment of the association between amblyopia and refractive errors.
Findings of our study need to be interpreted with the following caveats. First, this is a cross-sectional study and a causal relationship cannot be concluded. Second, among the 4273 participants who underwent comprehensive ophthalmological examinations, only 3959 had a parent or child carer who accepted the background information questionnaire, reducing the total number of subjects that participated in the risk factor analysis. Third, information on children and families were collected based on the parent-reported questionnaire, which carried a risk of recall bias. Fourth, children who may have been received ophthalmic care from other practicing ophthalmologists, along with those whose strabismus had been completely treated, might have been absent from the study. This may have lowered the prevalence rate. Fifth, we did not include ocular co-morbitidies (except refractive error) or past medical history since the prevalence is relatively low among the healthy subjects of our population based sample group. Instead, we measured other health parameters, including BMI, blood pressure to maximize the yield of comparison. Last but not least, the risk factors of esotropia and exotropia could not be analyzed separately due to insufficient power related to the limited number of cases for each type.
In conclusion, the prevalence of strabismus among ethnic Chinese children age 6–8 years old was found to be 3.11%. Refractive errors are a strong risk factor to strabismus. Among the strabismus cases, exotropia is the predominant type and outnumbers esotropia by a ratio of 9.75:1. Furthermore, family history of strabismus and maternal smoking during pregnancy were significant independent risk factors for strabismus. The adverse effects of maternal smoking on child vision should be emphasized with proper education to parents and public for promotion of child health. In the meantime, efforts should be made through public health service to detect childhood strabismus among the high-risk children whose parents have strabismus or a history of smoking. Early correction of refractive errors and avoidance of maternal smoking during pregnancy are potentially helpful in preventing strabismus.
References
McKean-Cowdin, R. et al. Prevalence of amblyopia or strabismus in Asian and non-Hispanic white preschool children: Multi-ethnic pediatric eye disease study. Ophthalmology 120(10), 2117–2124 (2013).
Hatt, S. R. et al. Association of strabismus with functional vision and eye-related quality of life in children. JAMA Ophthalmol. 138(5), 528–535 (2020).
Friedman, D. S. et al. Prevalence of amblyopia and strabismus in white and African American children aged 6 through 71 months the Baltimore Pediatric Eye Disease Study. Ophthalmology 116(11), 2128–2134 (2009).
Multi-ethnic Pediatric Eye Disease Study G. Prevalence of amblyopia and strabismus in African American and Hispanic children ages 6 to 72 months the multi-ethnic pediatric eye disease study. Ophthalmology 115(7), 1229–1236 (2008).
Chia, A. et al. Prevalence of amblyopia and strabismus in young singaporean chinese children. Invest. Ophthalmol. Vis. Sci. 51(7), 3411–3417 (2010).
Dahlin, S. et al. Maternal tobacco use and extremely premature birth: A population-based cohort study. BJOG 123(12), 1938–1946 (2016).
Cheung, C. Y. et al. Quantitative retinal microvasculature in children using swept-source optical coherence tomography: The Hong Kong Children Eye Study. Br. J. Ophthalmol. 103, 672–679 (2018).
Yam, J. C. et al. High prevalence of myopia in children and their parents in Hong Kong Chinese Population: The Hong Kong Children eye study. Acta Ophthalmol. 98, e639–e648 (2020).
Wong, E. S. et al. Association of optical coherence tomography angiography metrics with detection of impaired macular microvasculature and decreased vision in amblyopic eyes: The Hong Kong children eye study. JAMA Ophthalmol. 138, 858–865 (2020).
Yuan, N. et al. Association of secondhand smoking exposure with choroidal thinning in children aged 6 to 8 years: The Hong Kong Children eye study. JAMA Ophthalmol. 137, 1406–1414 (2019).
Lu, S. Y. et al. Association of WNT7B and RSPO1 with axial length in school children. Invest. Ophthalmol. Vis. Sci. 61(10), 11 (2020).
Li, F. F. et al. Genetic associations of myopia severities and endophenotypes in children. Br. J. Ophthalmol. https://doi.org/10.1136/bjophthalmol-2020-316728 (2020).
Tang, S. M. et al. Association of the ZC3H11B, ZFHX1B and SNTB1 genes with myopia of different severities. Br. J. Ophthalmol. 104(10), 1472–1476 (2020).
Zhu, H. et al. Prevalence of amblyopia and strabismus in Hani school children in rural southwest China: A cross-sectional study. BMJ Open 9(2), e025441 (2019).
Chen, X. et al. Prevalence of amblyopia and strabismus in Eastern China: Results from screening of preschool children aged 36–72 months. Br. J. Ophthalmol. 100(4), 515–519 (2016).
Cotter, S. A. et al. Risk factors associated with childhood strabismus: The multi-ethnic pediatric eye disease and Baltimore pediatric eye disease studies. Ophthalmology 118(11), 2251–2261 (2011).
Matsuo, T. & Matsuo, C. Comparison of prevalence rates of strabismus and amblyopia in Japanese elementary school children between the years 2003 and 2005. Acta Med. Okayama 61(6), 329–334 (2007).
Matsuo, T. & Matsuo, C. The prevalence of strabismus and amblyopia in Japanese elementary school children. Ophthalmic Epidemiol. 12(1), 31–36 (2005).
Ohlsson, J. et al. Visual acuity, amblyopia, and ocular pathology in 12- to 13-year-old children in Northern Mexico. J AAPOS 7(1), 47–53 (2003).
Robaei, D., Kifley, A. & Mitchell, P. Factors associated with a previous diagnosis of strabismus in a population-based sample of 12-year-old Australian children. Am. J. Ophthalmol. 142(6), 1085–1088 (2006).
Tang, S. M. et al. Refractive errors and concomitant strabismus: A systematic review and meta-analysis. Sci. Rep. 6, 35177 (2016).
Han, K. E. et al. Prevalence and risk factors of strabismus in children and adolescents in South Korea: Korea National Health and Nutrition Examination Survey, 2008–2011. PLoS ONE 13(2), e0191857 (2018).
Kataoka, M. C. et al. Smoking during pregnancy and harm reduction in birth weight: A cross-sectional study. BMC Pregnancy Childbirth 18(1), 67 (2018).
Fiess, A. et al. Prevalence and associated factors of strabismus in former preterm and full-term infants between 4 and 10 Years of age. BMC Ophthalmol. 17(1), 228 (2017).
Acknowledgements
We thank all the children and their families for their participation in the Hong Kong Children Eye Study. We also thank our colleagues and volunteers for all their hard work and dedication in data collection for this study. We are very grateful to Ms Mandy P.H. Ng from the Department of Ophthalmology and Visual Sciences, the Chinese University of Hong Kong, for her overall coordination and logistic arrangements on the study.
Funding
This study was supported in part by the CUHK Jockey Club Children Eye Care Programme; the General Research Fund (GRF), Research Grants Council, Hong Kong (14111515 and 14103419 [JCY]); the Health and Medical Research Fund (HMRF), Hong Kong (5160836 [LJC] and 07180826 [XJZ]); the Direct Grants of the Chinese University of Hong Kong (4054193 [LJC] and 4054121 & 4054199 [JCY]); the UBS Optimus Foundation Grant 8984 [JCY]; and the Centaline Myopia Fund [JCY].
Author information
Authors and Affiliations
Contributions
Conception or design of the work: J.C.Y.; Data collection: X.J.Z, Y.H.L, K.W.K; Data analysis and interpretation: X.J.Z, Y.M.W.; Drafting the article: X.J.Z., Y.H.L.; Critical revision of the article: J.C.Y, C.P.P, L.J.C., P.I, W.W.Y., S.T.K., A.L.Y., C.C.T.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zhang, X.J., Lau, Y.H., Wang, Y.M. et al. Prevalence of strabismus and its risk factors among school aged children: The Hong Kong Children Eye Study. Sci Rep 11, 13820 (2021). https://doi.org/10.1038/s41598-021-93131-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-93131-w
This article is cited by
-
Factors associated with progressive anisometropia after bilateral intraocular lens implantation in patients with pediatric cataract
Eye (2024)
-
Interocular Symmetry in Retinal Nerve Fiber Layer Thickness in Children: The Hong Kong Children Eye Study
Ophthalmology and Therapy (2023)
-
Medical expenditure for strabismus: a hospital-based retrospective survey
Cost Effectiveness and Resource Allocation (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.