Abstract
We investigated longitudinal associations of moderate-to-vigorous physical activity (MVPA) and light-intensity physical activity (LPA) with plasma concentrations of 138 metabolites after colorectal cancer (CRC) treatment. Self-reported physical activity data and blood samples were obtained at 6 weeks, and 6, 12 and 24 months post-treatment in stage I-III CRC survivors (n = 252). Metabolite concentrations were measured by tandem mass spectrometry (BIOCRATES AbsoluteIDQp180 kit). Linear mixed models were used to evaluate confounder-adjusted longitudinal associations. Inter-individual (between-participant differences) and intra-individual associations (within-participant changes over time) were assessed as percentage difference in metabolite concentration per 5 h/week of MVPA or LPA. At 6 weeks post-treatment, participants reported a median of 6.5 h/week of MVPA (interquartile range:2.3,13.5) and 7.5 h/week of LPA (2.0,15.8). Inter-individual associations were observed with more MVPA being related (FDR-adjusted q-value < 0.05) to higher concentrations of arginine, citrulline and histidine, eight lysophosphatidylcholines, nine diacylphosphatidylcholines, 13 acyl-alkylphosphatidylcholines, two sphingomyelins, and acylcarnitine C10:1. No intra-individual associations were found. LPA was not associated with any metabolite. More MVPA was associated with higher concentrations of several lipids and three amino acids, which have been linked to anti-inflammatory processes and improved metabolic health. Mechanistic studies are needed to investigate whether these metabolites may affect prognosis.
Similar content being viewed by others
Introduction
In 2018, there were almost five million colorectal cancer (CRC) survivors who were diagnosed in the past five years, making CRC the second most prevalent cancer worldwide1. The number of CRC survivors is expected to continue to rise in coming years due to a higher incidence and better survival2. There is strong evidence that engaging in leisure-time physical activity after a diagnosis of CRC is associated with lower overall3,4,5 and CRC-specific mortality3,4, and better quality of life6,7,8. Cancer survivors are currently advised to engage in ≥ 150 min/week of moderate-to-vigorous physical activity (MVPA)9,10, including activities expending ≥ 3 metabolic equivalents (METs) such as brisk walking or cycling11. Emerging evidence from our research group suggests that light-intensity physical activity (LPA: < 3 METs), e.g. light household work, is also beneficially associated with quality of life among CRC survivors12.
The biological mechanisms through which physical activity may influence health and well-being after CRC are not well understood4,6. Previous research suggests that obesity, hormones, growth factors, the immune system and inflammatory processes may be involved, but evidence is still preliminary and mostly based on studies in breast cancer survivors13. A better understanding of the metabolic pathways that are influenced by physical activity in CRC survivors will contribute to the development of tailored physical activity interventions14. Metabolomics is a powerful approach to investigate how health-related exposures and outcomes are associated with human metabolism by allowing a simultaneous assessment of hundreds of metabolites from key metabolic pathways, such as amino acids, phospholipids, sugars and other metabolites15,16. To the best of our knowledge, no study to date has applied a metabolomics approach to investigate associations of physical activity with circulating metabolites in CRC survivors. In the general population, cross-sectional associations have been found between physical activity and blood concentrations of phosphatidylcholines (PCs)17,18, amino acids18,19,20,21,22,23,24 and glucose19,21. In one of these studies, LPA was associated with several amino acids and glucose, whereas weaker associations were observed for MVPA19.
Further research is necessary to determine whether these cross-sectional observations in the general population can be replicated in CRC survivors. Furthermore, a longitudinal analysis is needed to study whether changes in physical activity may affect metabolite concentrations over time, which is important to develop future interventions. Therefore, we investigated longitudinal associations of self-reported time spent in MVPA and LPA with plasma concentrations of 138 targeted metabolites in CRC survivors up to two years post-treatment.
Methods
Study design and participants
The Energy for life after ColoRectal cancer (EnCoRe) study is an ongoing prospective cohort study initiated in 2012 (Netherlands Trial Register no. NL6904)25. Stage I–III CRC patients are recruited at diagnosis (response ~ 45%) in three participating hospitals in the southeastern part of The Netherlands (Maastricht University Medical Center + , VieCuri Medical Center, and Zuyderland Medical Centre). Men and women aged minimum 18 years old are eligible, while individuals with stage IV CRC and comorbidities obstructing successful study participation (e.g. Alzheimer’s disease) are excluded. Repeated measurements of, among others, self-reported physical activity and blood samples are obtained at diagnosis (before cancer treatment, i.e. surgery, chemotherapy and/or radiotherapy), and at 6 weeks, 6 months, and 1, 2 and 5 years after the end of treatment, by trained research dieticians during home visits. The EnCoRe study has been approved by the Medical Ethics Committee of the Academic Hospital Maastricht and Maastricht University, The Netherlands. The study was conducted in accordance with the Declaration of Helsinki and all participants gave written informed consent.
For the current study, data collected up until November 1st 2016 were used. Since the study is focused on associations of physical activity and metabolites after CRC treatment, we included individuals with at least one post-treatment measurement of self-reported physical activity, targeted metabolomics and covariates. In total, n = 252 CRC survivors were included in the analyses, with data at 6 weeks (n = 241), 6 months (n = 192), 12 months (n = 152) and 24 months (n = 67) post-treatment (Fig. 1; n = 57 participants had data at all post-treatment time points). The statistical technique being used for longitudinal analysis, i.e. linear mixed modelling, employs all data including data of participants with missing data at some time points26. Response rates at post-treatment measurements were > 90% and mortality during follow-up was limited (n = 17). The declining numbers of participants at subsequent time points and the lack of 5 year post-treatment measurements are (predominantly) due to the fact that not all participants included at diagnosis from April 2012 onwards had reached yet these time points in November 2016.
Flow diagram of participants and measurements within the EnCoRe study and the number of post-treatment measurements included in the analyses presented in this paper. Data collected up until November 1st 2016 were included in the analyses. 1 Totals do not add up because some individuals reported multiple reasons for non-participation. 2 Response rate = (persons with home visits)/(persons with home visits + persons lost to follow-up – persons died). The declining numbers of participants at subsequent time points are predominantly due to the fact that not all participants had reached yet these time points on November 1st 2016. 3 Since the current analysis was focused on physical activity and metabolites after colorectal cancer treatment, only post-treatment measurements with available data on self-reported physical activity, metabolites and covariates were included. A total of n = 252 participants with at least one post-treatment measurement including these data were included in the analysis. The number of participants with available physical activity and metabolites data were respectively n = 268 and n = 249 at 6 weeks, n = 215 and n = 203 at 6 months, n = 169 and n = 162 at 1 year, and n = 72 and n = 73 at 2 years post-treatment. 4 Other person who also missed 6 weeks visit did not have follow-up visit before November 1st 2016.
Physical activity
The Short QUestionnaire to ASsess Health-enhancing physical activity (SQUASH) was used to assess self-reported time spent in MVPA and LPA (hours/week)27. Participants reported the frequency (days/week), duration (time/day) and intensity (light, moderate or vigorous) of commuting (walking and cycling), household, work and leisure-time activities (walking, cycling, gardening, odd jobs, and up to four sports) in the previous week. Based on Ainsworth’s Compendium of Physical Activities, all activities were assigned MET-values and categorized as either MVPA (≥ 3 MET; e.g. vigorous household work, walking and sports), or LPA (< 3 MET; e.g. light household or light work activities)28. At each time point, the most commonly reported sport was going to the gym. By summing time spent on activities in each category, total hours/week spent in MVPA and LPA were calculated. In addition, it was determined whether participants adhered to the physical activity guidelines (≥ 150 min/week of MVPA)9,10. The SQUASH is fairly reliable (test–retest: Spearman’s ρ 0.57–0.58)27,29. Its relative validity in assessing time spent in physical activity compared to accelerometer data is comparable to other physical activity questionnaires (Spearman’s ρ 0.56 for total physical activity, 0.35 for vigorous-intensity activities, 0.40 for moderate-intensity activities, and 0.20 for LPA)29.
Blood sampling and laboratory analyses
Blood samples were drawn from fasting participants according to standardized protocols. Samples were collected in 6 mL EDTA plasma tubes, and then centrifuged, aliquoted and stored at − 80 °C within 4 h after blood draw.
Targeted metabolomics analysis were performed at the International Agency for Research on Cancer (IARC), Lyon, France, using the AbsoluteIDQ p180 kit (BIOCRATES Life Sciences AG, Austria) measuring a panel of up to 188 metabolites, including acylcarnitines, amino acids, biogenic amines, a sum of hexoses, PCs including lysoPCs, diacylPCs, and acyl-alkylPCs, and sphingomyelins (SMs). A good to excellent reliability for the majority of metabolites measured using this kit has been observed when comparing samples collected in the same individuals over a period of 4 months30 and 2 years31 (intra-class correlation coefficients > 0.50 for most metabolites). The procedures and metabolite nomenclature have been described in detail previously32,33,34. Briefly, samples were analyzed by ultra-high performance liquid chromatography (LC; 1290 Series HPLC, Agilent, France) coupled to a tandem mass spectrometer (MS/MS; Triple Quad 4500, AB Sciex, USA). Samples were analyzed in ten analytical batches with participants randomized over batches, and post-treatment samples of each participant placed subsequently in the same batch in a random order. Each batch included human plasma-based quality control (QC) samples from the manufacturer (three spiked samples), from the IARC laboratory (two samples in duplicate), and from a previous cross-sectional study conducted in 2–10 year post-treatment CRC survivors 3 samples in duplicate25. Samples collected at diagnosis had been previously analyzed using the same protocol33.
Metabolites with inter-batch or intra-batch coefficients of variation (CVs) > 20% for IARC replicates were excluded from the analysis, leading to a total of 149 metabolites. Of these, metabolites with > 20% of missing values and/or measurements outside the measurable range (i.e. below the limit of detection/quantification or above highest calibration standards) were excluded34, resulting in a total of 138 metabolites included in the current analysis, including 13 acylcarnitines, 21 amino acids, nine biogenic amines, 80 PCs (11 lysoPCs, 34 diacylPCs, and 35 acyl-alkylPCs), 14 SMs, and a sum of hexoses. Supplementary Table 1 lists measurement information on all metabolites in the kit. Mean (intrabatch) CVs of QC samples from CRC survivors in the previous cross-sectional study were < 20% for all included metabolites. Measurements below the limit of detection or quantification (where applicable) were set to half the batch-specific limit of detection or quantification, respectively34. In addition, all measurements above the highest calibration standards were set to the highest standard concentration. Metabolite concentrations (µM) were log-transformed (natural logarithm) to reduce right skewness of distributions.
Covariates
Highest attained education level was self-reported by participants at diagnosis, as low, medium, or high. At each post-treatment time point, smoking status (never, former or current) was assessed through self-report, weight and height of participants was measured by trained dieticians and used to calculate body mass index (BMI; kg/m2), alcohol intake (g/day) was assessed through 7-day dietary records35, and the number of comorbidities was measured using the 13-item Self-Administered Comorbidity Questionnaire36. Clinical characteristics including tumor site (colon/rectum), cancer stage and treatment were collected from clinical records.
Statistical analysis
Descriptive analyses were performed for sociodemographic, lifestyle, and clinical variables. Correlation coefficients between physical activity variables and metabolites were visualized in heatmaps. The development of metabolite concentrations during post-treatment measurements was assessed using linear mixed models with batch and sex-adjusted residuals (calculated as described below) as dependent variable, and time since end of treatment included as independent variable (continuous, per 6 months).
To be able to adjust for sex and analytical batch in the main analysis, residuals of each of the ln-transformed metabolite concentrations were computed from linear mixed models with sex as independent variable and random intercepts for individuals nested within analytical batches. The residuals were summed with individual random effects (to retain individual variation in metabolites over time, while excluding batch effects) to be used as dependent variables in further analyses.
Linear mixed regression with random intercepts for individuals was applied to analyze longitudinal associations of self-reported MVPA and LPA (continuously, per 5 h/week) and adherence to the physical activity guideline (yes/no) with circulating concentrations of each of the metabolites (batch and sex-adjusted residuals), between 6 weeks up to 2 years post-treatment. Obtained regression coefficients of the overall longitudinal relationship can be interpreted as a weighted average of a between-subject component (i.e. how differences in physical activity variables between participants are related to metabolite concentrations over time: inter-individual associations) and a within-subject component (i.e. how changes in physical activity variables within participants over time are related to metabolite concentrations over time: intra-individual associations). We also applied a hybrid modelling method, where the between-subject component was modelled as the mean value of the physical activity variable for each participant across time points, while the within-subject component was modelled as the difference between the physical activity level at each time point and the mean level across time points37,38.
Models were adjusted for age (continuous), sex, hospital, time since end of treatment (continuous), smoking status, BMI (continuous), alcohol intake (continuous), and number of comorbidities (0/1/ ≥ 2 comorbidities) at post-treatment measurements. Models were also adjusted for post-treatment levels of MVPA for the analysis of LPA, and vice versa. Potential confounders were identified a priori based on theoretical considerations and literature; other covariates were considered in sensitivity analyses as described below. To adjust for multiple testing, false discovery rate (FDR) adjustment of P-values using the Benjamini–Hochberg method was applied (q-values < 0.05 were considered significant)39.
Heterogeneity analyses
To explore potential heterogeneity by sex, chemotherapy (yes/no), radiotherapy (yes/no), tumor site, number of comorbidities (≥ 2 versus < 2) and time since end of treatment, interaction product terms (e.g. product of MVPA and sex) were tested with FDR-adjustment.
Sensitivity analyses
To assess potential confounding by tumor-related variables, additional analyses were performed including chemotherapy and radiotherapy (yes/no, including neo-adjuvant and/or adjuvant treatment) as covariates. In addition, models were run with additional adjustment for metabolite concentrations at diagnosis, using batch-adjusted residuals that were calculated similarly as for post-treatment data. Based on an a priori defined directed acyclic graph (Supplementary Fig. 1), we hypothesized that adjustment for metabolite concentrations at diagnosis may lead to collider bias, similar to what has been reported previously40. Therefore, a difference in results compared to the main analysis could be due to confounding and/or collider bias. Models with additional adjustment for self-reported time spent on LPA and MVPA at diagnosis showed signs of collinearity with increasing standard errors and variance inflation factors of physical activity variables > 2.5041, likely due to strong correlations between physical activity variables at diagnosis and at post-treatment measurements (Spearman’s ρ; range: 0.59, 0.80). These models were therefore not reported.
All analyses were conducted using R (version 3.6.2).
Disclaimer
Where authors are identified as personnel of the International Agency for Research on Cancer / World Health Organization, the authors alone are responsible for the views expressed in this article and they do not necessarily represent the decisions, policy or views of the International Agency for Research on Cancer / World Health Organization.
Results
Participant characteristics
Characteristics of included study participants (n = 252) at 6 weeks post-treatment, by adherence to the physical activity guideline, are shown in Table 1. About two-third of the participants were men (68.7%) and the mean age at 6 weeks post-treatment was 66.7 years (SD: 9.2). Mean BMI was 27.8 kg/m2 (SD: 4.4). Just over half of participants reported ≥ 2 comorbidities (53.6%) and 25.4% had one comorbidity. Most participants were colon cancer survivors (60.7%), while 39.3% were rectum cancer survivors. The majority of participants received surgery (89.7%), and 38.1% and 27.8% received (neo-)adjuvant chemotherapy and radiotherapy, respectively. Participants who reported adherence to the physical activity guideline at 6 weeks post-treatment (75.8%) were more often men, and reported more often current or former smoking and a higher alcohol intake compared to non-adhering participants; other characteristics were similar.
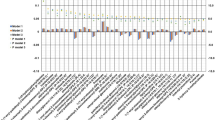
At each time point, median MVPA was lower among women than men, while the opposite was observed for LPA (Fig. 2). At 6 weeks post-treatment, women reported a median of 4 h/week of MVPA (IQR: 2, 7) and 14 h/week7,24 of LPA, while men reported 9 h/week4,16 of MVPA and 6 h/week1,12 of LPA. Most participants decreased physical activity levels between diagnosis and 6 weeks post-treatment (median change in MVPA in women: − 4, men: − 3 h/week; LPA in women: − 3, men: − 1 h/week), and increased at later post-treatment time points particularly between 6 weeks and 6 months post-treatment (median change in MVPA: + 2 h/week in both sexes; LPA in women: + 2, men: + 0.1 h/week). Both MVPA and LPA showed moderate to strong correlations across repeated measurements (range in Spearman’s ρ for MVPA: 0.58, 0.76; LPA: 0.57, 0.80), while mostly negative and weak correlations were observed between MVPA and LPA at each time point (-0.29, 0.03) (heatmap in Supplementary Fig. 2).
Sex-stratified medians and interquartile ranges of self-reported (a) hours/week of moderate-to-vigorous physical activity (MVPA), (b) percentage self-reported adherence to physical activity guideline (≥ 150 min/week of MVPA), and (c) hours/week of light-intensity physical activity (LPA) at diagnosis and at post-treatment (PT) time points among colorectal cancer survivors included in the current analysis (n = 252).
Metabolome characteristics
Descriptives of included metabolites at each time point are reported in Supplementary Table 2, and heatmaps of correlations between metabolites are depicted in Supplementary Fig. 3. Within classes of metabolites at 6 weeks post-treatment, median Spearman’s ρ was generally higher for lysoPCs (0.50; IQR: 0.29, 0.68), diacylPCs (0.48; 0.36, 0.60), acyl-alkylPCs (0.59; 0.50, 0.68) and SMs (0.60; 0.50, 0.69), compared to acylcarnitines (0.32; 0.14, 0.53), amino acids (0.23; 0.13, 0.35) and biogenic amines (0.14; 0.01, 0.26), and similar patterns were observed at other time points. Correlations between repeated metabolite measurements across post-treatment time points were moderate to strong (range in median Spearman’s ρ: 0.62, 0.70; Supplementary Table 3). During the post-treatment period, 23 metabolites significantly changed over time (FDR q-value < 0.05), with mostly increasing concentrations at later time points (median percentage change in metabolite concentrations per 6 months: 1.3, IQR: 0.4, 1.9; Supplementary Table 4).
Associations of physical activity with metabolites
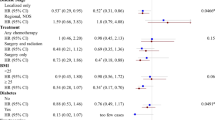
In confounder-adjusted analyses assessing overall longitudinal associations over time, higher levels of MVPA were related to higher concentrations of 12 out of 138 metabolites after FDR-adjustment (Fig. 3a; full results in Supplementary Table 5). In the hybrid model, inter-individual associations were observed with higher levels of MVPA being related to higher plasma concentrations of 36 metabolites, including acylcarnitine C10:1, three amino acids (arginine, histidine and citrulline), eight lysoPCs, nine diacylPCs, 13 acyl-alkylPCs, and two SMs. No statistically significant intra-individual associations were observed and effect estimates were generally smaller than for inter-individual associations. Adherence to the physical activity guideline was associated with higher concentrations of 13 metabolites in the overall longitudinal analysis (Fig. 3b; Supplementary Table 5). In the inter-individual analysis, adherence was associated with higher concentrations of 12 metabolites, including SM C26:0 and SM(OH) C24:1 which had not been identified in the analysis of continuous MVPA. Adherence was also associated with lower concentrations of acylcarnitine C12:1 and symmetric dimethylarginine (SDMA). LPA was not longitudinally associated with any of the metabolites (Supplementary Table 5). Figure 4 shows a heatmap of the correlations at 6 weeks post-treatment across metabolites that were longitudinally related to continuous MVPA and/or adherence to the guideline. Generally, moderate to strong positive correlations were observed within and across classes of PCs and SMs, except for lysoPCs being weakly correlated with SMs and other PCs, and similar patterns were observed at other post-treatment time points.
Forest plots showing effect estimates and 95% confidence intervals of metabolites that were statistically significantly (FDR q-value < 0.05) related to self-reported time spent on moderate-to-vigorous physical activity (MVPA; (a)) and adherence to the physical activity guideline (≥ 150 min/week of MVPA; (b)) among colorectal cancer survivors, between 6 weeks and 2 years post-treatment, including overall, inter-individual and intra-individual longitudinal associations. Asterisk (*) denotes statistical significance after FDR-adjustment (q-values < 0.05 were considered significant). Since light-intensity physical activity (LPA) was not statistically significantly associated with any of the metabolites, these results are not shown. Full results for all physical activity variables and metabolites are included in Supplementary Table 5. AAs amino acids, ACs acylcarnitines, BAs biogenic amines, MVPA moderate-to-vigorous physical activity, PCs phosphatidylcholines. Analyzed with multivariable linear mixed regression models analyzing associations of the physical activity variables as the main independent variables and as dependent variables the batch-adjusted metabolite residuals (see “Methods” section), with a separate model for each metabolite. Models were adjusted for: sex; age (y; continuous), time since treatment (per 6 months; continuous), centre (Maastricht UMC + ; VieCuri Medical Center; Zuyderland Medical Centre), body mass index (kg/m2; continuous), smoking status (current; former; never), self-reported alcohol consumption (grams/day) and number of comorbidities (no comorbidity; 1 comorbidity; ≥ 2 comorbidities), at post-treatment time points. Models were also adjusted for post-treatment levels of MVPA for the analysis of LPA, and vice versa. The percentage difference in metabolite concentrations was calculated by subtracting the exponent of the obtained regression coefficient from 1 and multiplying the outcome with 100 (since metabolite concentrations were ln-transformed).
Heatmap of Spearman’s correlation coefficients at 6 weeks post-treatment between plasma concentrations of metabolites that were statistically significantly (FDR q-value < 0.05) related to self-reported time spent on moderate-to-vigorous physical activity (MVPA) and/or adherence to the physical activity guideline (≥ 150 min/week of MVPA) among colorectal cancer survivors. Similar patterns of correlations were observed at other post-treatment time points (results not shown). Heatmap of correlations among all analyzed metabolites at each time point is depicted in Supplementary Fig. 4.
Heterogeneity analyses
No statistically significant interactions were observed by sex, chemotherapy, radiotherapy, number of comorbidities (≥ 2 versus < 2) and time since end of treatment (results not shown). One significant interaction was found between tumor site and intra-individual associations of MVPA with PC aa C36:1, where more MVPA was associated with higher concentrations in colon cancer survivors and lower concentrations in rectum cancer survivors.
Sensitivity analyses
Results of the analysis with additional adjustment for chemotherapy and radiotherapy treatment were similar to those obtained in the main analysis (Supplementary Fig. 4). Adjustment for metabolite concentrations at diagnosis resulted in some attenuation of inter-individual associations for continuous MVPA and adherence to the physical activity guideline (Supplementary Fig. 5).
Discussion
To our knowledge, this is the first study to analyze longitudinal associations of physical activity with metabolites in CRC survivors. We found that CRC survivors who engaged in more MVPA had higher plasma concentrations of acylcarnitine C10:1, arginine, histidine and citrulline, and eight lysoPCs, nine diacyl PCs, 13 acyl-alkyl PCs, and two SMs. Adherence to the physical activity guideline was additionally related to higher concentrations of two SMs and histidine, and lower concentrations of acylcarnitine C12:1 and SDMA. Contrary to our hypothesis, intra-individual associations for both MVPA variables were weak and statistically non-significant, and self-reported LPA was not longitudinally associated with any of the metabolites.
Our observations of MVPA being positively associated with several mutually correlated PCs and SMs, are in contrast with findings from a population-based study in Germany where self-reported physical activity was not associated with PCs and SMs, measured using a similar targeted metabolomics approach (BIOCRATES p150)24. Next to the difference in study population compared to our study (general population versus CRC survivors), the differences in study findings may be due to a difference in physical activity assessment, since the German study only included activity during sports24, and in our study we used a more comprehensive assessment including also commuting, household, work and other leisure time activities. However, our results are consistent with those of another German study where a higher cardiorespiratory fitness was associated with higher serum concentrations of a cluster of PCs and some SMs, also measured using the BIOCRATES p15017. Further, in a US study, Ding et al.18 observed that more self-reported MET-hours/week of habitual physical activity was associated with higher plasma concentrations of PCs including lysoPCs, measured using another MS-based platform. Ding et al.18 hypothesized that the increase in phospholipids in plasma may be explained by stimulating effects of physical activity on cholesterol efflux through high-density lipoprotein (HDL). A low HDL concentration is one of the features of metabolic syndrome that is associated with worse prognosis after CRC42. In addition, PCs can have anti-inflammatory effects17 and could therefore mediate the health effects of physical activity after CRC through inflammatory processes13.
The amino acids that we identified to be related to MVPA among CRC survivors have previously been associated with physical activity in the general population, although results have been inconsistent. Consistent with our findings, a higher accelerometer-assessed total physical activity duration has been associated with higher plasma concentrations of arginine in Chinese adults19, and a higher PAEE has been associated with higher serum concentrations of arginine in Canadian women23. Further, positive associations between self-reported physical activity and plasma concentrations of citrulline have been observed in US adults18 and accelerometer-assessed MVPA has been associated with higher serum concentrations of histidine in UK adolescents43. However, a German study reported that more self-reported physical activity was related to lower serum arginine concentrations in men24. In addition, multiple other studies in the general population reported no associations of several physical activity measures with blood concentrations of arginine17,18,20, citrulline17,19,20,24, and histidine17,18,19,20,23,24. To our knowledge, no study to date has reported associations of habitual physical activity with SDMA. Experimental studies suggest that arginine intake may protect against CRC (recurrence) by inhibiting crypt cell hyperproliferation, and promoting immune status through increasing the conversion of arginine to nitric oxide (NO)44. Citrulline can act as a precursor for arginine and thereby contribute to NO synthesis45. SDMA on the other hand has proinflammatory effects and may indirectly inhibit NO production through interfering with arginine transport into cells46. Further, anti-inflammatory effects of histidine in intestinal epithelial cells have been reported47, and a lower histidine has been associated with poor survival after CRC48.
Finally, we observed opposite associations of both MVPA variables with acylcarnitines C10:1 and C12:1. Previous population-based studies reported no significant associations of physical activity with acylcarnitines17,24. Acylcarnitines are used as a substrate for mitochondrial oxidation of fatty acids49, and are markers for incomplete fatty acid oxidation linked to insulin resistance, type 2 diabetes and cardiovascular health50. Experimental studies have found that exercise can induce temporary increases in circulating medium-chain acylcarnitines (including C10:1 and C12:1) as a marker of incomplete fatty acid oxidation51,52, but whether habitual physical activity may also have long-term effects on circulating acylcarnitines was yet unknown. Further research will be necessary to determine whether these acylcarnitines may be related to the health of CRC survivors.
We observed inter-individual associations of MVPA with several metabolites, but intra-individual associations were weak and non-significant. This suggests that post-treatment levels but not changes in MVPA are associated with metabolic health in CRC survivors, which may be relevant in light of potential development of interventions. One explanation of our findings is that the intra-individual changes in MVPA and circulating metabolite concentrations over time may have been insufficient, as correlations between repeated measurements were strong and observed changes in physical activity and metabolites were generally limited. Only seven of the metabolites for which inter-individual associations were observed with the MVPA variables were found to significantly change over time. Our analysis was limited to metabolites included in the kit, of which the majority has been previously observed to be stable over time30,31. Further experimental studies with larger contrasts in physical activity and including also other metabolites (e.g. using untargeted approaches) are necessary to further investigate whether changes in MVPA may influence metabolic pathways in CRC survivors.
Strengths of our study include the prospective design of our study with repeated measurements of physical activity, metabolomics, and potential confounders. Using a hybrid model, we were able to distinguish between intra- and inter-individual associations over time. Finally, all post-treatment samples were drawn under fasting conditions and stored and analyzed according to standardized protocols, ensuring the quality and comparability of metabolomics data. There are also limitations to consider. Firstly, physical activity levels were self-reported through a questionnaire which is prone to recall errors, and a limited validity of the SQUASH has been observed particularly for LPA29. The SQUASH mainly assesses light (household) work as LPA and no other light-intensity activities such as light-walking or standing during leisure time. This may have contributed to the limited intra-individual variation observed over time in LPA, and the lack of longitudinal associations between LPA and metabolites. Further research with accelerometer data will be necessary to confirm our findings. In addition, we were not able to adjust our analysis for physical activity levels at diagnosis, because of collinearity in these models. Therefore, we cannot rule out the possibility that the associations we observed of MVPA with metabolites may reflect effects of lifetime MVPA rather than (only) post-treatment MVPA levels. Further, apart from alcohol consumption and BMI, which are both strongly related to the metabolites included in the BIOCRATES kit34,53, we did not adjust our analysis for other dietary(-related) factors and this could have resulted in residual confounding. In addition, collider bias may have occurred in the analysis with adjustment for metabolite concentrations at diagnosis, which could have caused the attenuation observed. Nevertheless, the attenuation was limited and results were still in the same direction, indicating the robustness of our results.
In conclusion, we observed in this longitudinal study that self-reported time spent on MVPA was associated with plasma concentrations of several PCs, SMs, arginine, citrulline, histidine, SDMA and two acylcarnitines in CRC survivors. Our results indicate that differences in (long-term) MVPA levels between CRC survivors—but not intra-individual changes in MVPA after treatment—are associated with post-treatment metabolite concentrations. These results point towards potential underlying biological mechanisms including inflammation and other metabolic pathways, which may underlie the health-enhancing effects of (lifetime) physical activity in CRC survivors. Further longitudinal accelerometer-based studies are necessary to confirm our results, as well as mechanistic studies to investigate whether these metabolites may affect prognosis after CRC.
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Ferlay J, Ervik M, Lam F, Colombet M, Mery L, Piñeros M, Znaor A, Soerjomataram I, Bray F (2018). Global Cancer Observatory: Cancer Today. Lyon, France: International Agency for Research on Cancer. Available from: https://gco.iarc.fr/today, accessed [17 April 2020].
Arnold, M. et al. Global patterns and trends in colorectal cancer incidence and mortality. Gut 66(4), 683–691 (2017).
Schmid, D. & Leitzmann, M. F. Association between physical activity and mortality among breast cancer and colorectal cancer survivors: A systematic review and meta-analysis. Ann. Oncol. 25(7), 1293–1311 (2014).
Walter, V. et al. Physical activity and survival of colorectal cancer patients: Population-based study from Germany. Int. J. Cancer 140(9), 1985–1997 (2017).
Arem, H. et al. Pre- and postdiagnosis physical activity, television viewing, and mortality among patients with colorectal cancer in the National Institutes of Health-AARP Diet and Health Study. J. Clin. Oncol. 33(2), 180–188 (2015).
Lynch, B. M., van Roekel, E. H. & Vallance, J. K. Physical activity and quality of life after colorectal cancer: Overview of evidence and future directions. Exp. Rev. Qual. Life Cancer Care 1(1), 9–23 (2016).
Eyl, R. E. et al. Physical activity and long-term quality of life among colorectal cancer survivors—a population-based prospective study. Cancer Prev Res. 2, 2 (2020).
van Veen, M. R. et al. Adherence to the world cancer research fund/american institute for cancer research recommendations for cancer prevention is associated with better health-related quality of life among long-term colorectal cancer survivors: results of the PROFILES registry. Support Care Cancer 27(12), 4565–4574 (2019).
Schmitz, K. H. et al. American College of Sports Medicine roundtable on exercise guidelines for cancer survivors. Med. Sci. Sports Exerc. 42(7), 1409–1426 (2010).
World Cancer Research Fund/American Institute for Cancer Research. Diet, Nutrition, Physical Activity, and Cancer: a Global Perspective. Continuous Update Project Expert Report 2018. Available at: dietandcancerreport.org.
Ainsworth, B. E. et al. 2011 Compendium of physical activities: A second update of codes and MET values. Med. Sci. Sports Exerc. 43(8), 1575–1581 (2011).
van Roekel, E. H. et al. Light physical activity is associated with quality of life after colorectal cancer. Med. Sci. Sports Exerc. 47(12), 2493–2503 (2015).
Ballard-Barbash, R. et al. Physical activity, biomarkers, and disease outcomes in cancer survivors: A systematic review. J. Natl. Cancer Inst. 104(11), 815–840 (2012).
Vineis, P. & Perera, F. Molecular epidemiology and biomarkers in etiologic cancer research: The new in light of the old. Cancer Epidemiol. Biomarkers Prev. 16(10), 1954–1965 (2007).
Scalbert, A. et al. Mass-spectrometry-based metabolomics: limitations and recommendations for future progress with particular focus on nutrition research. Metabolomics 5(4), 435–458 (2009).
Dettmer, K., Aronov, P. A. & Hammock, B. D. Mass spectrometry-based metabolomics. Mass Spectrom. Rev. 26(1), 51–78 (2007).
Wientzek, A. et al. Serum metabolites related to cardiorespiratory fitness, physical activity energy expenditure, sedentary time and vigorous activity. Int. J. Sport Nutr. Exerc. Metab. 24(2), 215–226 (2014).
Ding, M. et al. Metabolome-wide association study of the relationship between habitual physical activity and plasma metabolite levels. Am. J. Epidemiol. 188(11), 1932–1943 (2019).
Xiao, Q. et al. Objectively measured physical activity and plasma metabolomics in the Shanghai Physical Activity Study. Int. J. Epidemiol. 45(5), 1433–1444 (2016).
Fukai, K. et al. Metabolic profiling of total physical activity and sedentary behavior in community-dwelling men. PLoS ONE 11(10), e0164877 (2016).
Kujala, U. M. et al. Long-term leisure-time physical activity and serum metabolome. Circulation 127(3), 340–348 (2013).
Gu, Q. et al. Metabolic profiling of adherence to diet, physical activity and body size recommendations for cancer prevention. Sci. Rep. 8(1), 16293 (2018).
Palmnäs, M. S. A. et al. Serum metabolomics of activity energy expenditure and its relation to metabolic syndrome and obesity. Sci. Rep. 8(1), 3308 (2018).
Lacruz, M. E. et al. Cardiovascular risk factors associated with blood metabolite concentrations and their alterations during a 4-year period in a population-based cohort. Circ. Cardiovasc. Genet. 9(6), 487–494 (2016).
van Roekel, E. H. et al. The applicability of the international classification of functioning, disability, and health to study lifestyle and quality of life of colorectal cancer survivors. Cancer Epidemiol. Biomarkers Prev. 23(7), 1394–1405 (2014).
Twisk, J.W.R., Applied Longitudinal Data Analysis for Epidemiology. 2nd revised ed. 2013, Cambridge: Cambridge University Press.
Wendel-Vos, G. C., Schuit, A. J., Saris, W. H. & Kromhout, D. Reproducibility and relative validity of the short questionnaire to assess health-enhancing physical activity. J. Clin. Epidemiol. 56(12), 1163–1169 (2003).
Ainsworth, B. E. et al. Compendium of physical activities: classification of energy costs of human physical activities. Med. Sci. Sports Exerc. 25(1), 71–80 (1993).
Wagenmakers, R. et al. Reliability and validity of the short questionnaire to assess health-enhancing physical activity (SQUASH) in patients after total hip arthroplasty. BMC Musculoskelet. Disord. 9, 141 (2008).
Floegel, A. et al. Reliability of serum metabolite concentrations over a 4-month period using a targeted metabolomic approach. PLoS ONE 6(6), e21103 (2011).
Carayol, M., I. Licaj, D. Achaintre, C. Sacerdote, P. Vineis, T.J. Key, N.C. Onland Moret, A. Scalbert, S. Rinaldi, and P. Ferrari, Reliability of Serum Metabolites over a Two-Year Period: A Targeted Metabolomic Approach in Fasting and Non-Fasting Samples from EPIC. PLoS One, 2015. 10(8): e0135437.
Siskos, A. P. et al. Interlaboratory reproducibility of a targeted metabolomics platform for analysis of human serum and plasma. Anal. Chem. 89(1), 656–665 (2017).
Geijsen, A. et al. Plasma metabolites associated with colorectal cancer stage: Findings from an international consortium. Int. J. Cancer 2, 2 (2019).
van Roekel, E.H., L. Trijsburg, N. Assi, M. Carayol, D. Achaintre, N. Murphy, S. Rinaldi, J.A. Schmidt, M. Stepien, R. Kaaks, T. Kühn, H. Boeing, K. Iqbal, D. Palli, V. Krogh, R. Tumino, F. Ricceri, S. Panico, P.H. Peeters, B. Bueno-de-Mesquita, E. Ardanaz, L. Lujan-Barroso, J.R. Quirós, J.M. Huerta, E. Molina-Portillo, M. Dorronsoro, K.K. Tsilidis, E. Riboli, A.L. Rostgaard-Hansen, A. Tjønneland, K. Overvad, E. Weiderpass, M.C. Boutron-Ruault, G. Severi, A. Trichopoulou, A. Karakatsani, A. Kotanidou, A. Håkansson, J. Malm, M.P. Weijenberg, M.J. Gunter, M. Jenab, M. Johansson, R.C. Travis, A. Scalbert, and P. Ferrari, Circulating Metabolites Associated with Alcohol Intake in the European Prospective Investigation into Cancer and Nutrition Cohort. Nutrients, 2018. 10(5).
Breedveld-Peters, J. J. L. et al. Colorectal cancers survivors’ adherence to lifestyle recommendations and cross-sectional associations with health-related quality of life. Br. J. Nutr. 120(2), 188–197 (2018).
Sangha, O., Stucki, G., Liang, M. H., Fossel, A. H. & Katz, J. N. The Self-Administered Comorbidity Questionnaire: a new method to assess comorbidity for clinical and health services research. Arthritis Rheum. 49(2), 156–163 (2003).
Twisk, J. W. R. & de Vente, W. Hybrid models were found to be very elegant to disentangle longitudinal within- and between-subject relationships. J. Clin. Epidemiol. 107, 66–70 (2019).
Neuhaus, J. M. & Kalbfleisch, J. D. Between- and within-cluster covariate effects in the analysis of clustered data. Biometrics 54(2), 638–645 (1998).
Benjamini, Y. and Y. Hochberg, Controlling the False Discovery Rate: A Practical and Powerful Approach to Multiple Testing. Journal of the Royal Statistical Society. Series B (Methodological), 1995. 57(1):289–300.
Glymour, M. M., Weuve, J., Berkman, L. F., Kawachi, I. & Robins, J. M. When is baseline adjustment useful in analyses of change? An example with education and cognitive change. Am. J. Epidemiol. 162(3), 267–278 (2005).
Johnston, R., Jones, K. & Manley, D. Confounding and collinearity in regression analysis: A cautionary tale and an alternative procedure, illustrated by studies of British voting behaviour. Qual. Quant. 52(4), 1957–1976 (2018).
Peng, F. et al. Preoperative metabolic syndrome and prognosis after radical resection for colorectal cancer: The Fujian prospective investigation of cancer (FIESTA) study. Int. J. Cancer 139(12), 2705–2713 (2016).
Bell, J.A., M. Hamer, R.C. Richmond, N.J. Timpson, D. Carslake, and G. Davey Smith, Associations of device-measured physical activity across adolescence with metabolic traits: Prospective cohort study. PLoS Med, 2018. 15(9): e1002649.
Karimian, J., Hadi, A., Salehi-Sahlabadi, A. & Kafeshani, M. The effect of arginine intake on colorectal cancer: A systematic review of literatures. Clin. Nutr. Res. 8(3), 209–218 (2019).
Bahri, S. et al. Citrulline: From metabolism to therapeutic use. Nutrition 29(3), 479–484 (2013).
Riccioni, G. et al. Physical exercise reduces synthesis of ADMA, SDMA, and L-Arg. Front. Biosci. (Elite Ed) 7, 417–422 (2015).
Son, D. O., Satsu, H. & Shimizu, M. Histidine inhibits oxidative stress- and TNF-alpha-induced interleukin-8 secretion in intestinal epithelial cells. FEBS Lett. 579(21), 4671–4677 (2005).
Sirniö, P. et al. Alterations in serum amino-acid profile in the progression of colorectal cancer: associations with systemic inflammation, tumour stage and patient survival. Br. J. Cancer 120(2), 238–246 (2019).
Indiveri, C. et al. The mitochondrial carnitine/acylcarnitine carrier: Function, structure and physiopathology. Mol. Aspects Med. 32(4), 223–233 (2011).
Sun, L. et al. Early prediction of developing type 2 diabetes by plasma acylcarnitines: A population-based study. Diabetes Care 39(9), 1563–1570 (2016).
Zhang, J. et al. Acylcarnitines as markers of exercise-associated fuel partitioning, xenometabolism, and potential signals to muscle afferent neurons. Exp. Physiol. 102(1), 48–69 (2017).
Hansen, J.S., X. Zhao, M. Irmler, X. Liu, M. Hoene, M. Scheler, Y. Li, J. Beckers, M. Hrabĕ de Angelis, H.-U. Häring, B.K. Pedersen, R. Lehmann, G. Xu, P. Plomgaard, and C. Weigert, Type 2 diabetes alters metabolic and transcriptional signatures of glucose and amino acid metabolism during exercise and recovery. Diabetologia, 2015. 58(8): 1845–1854.
Carayol, M. et al. Blood Metabolic Signatures of Body Mass Index: A Targeted Metabolomics Study in the EPIC Cohort. J Proteome Res 16(9), 3137–3146 (2017).
Acknowledgements
We would like to thank all participants of the EnCoRe study and the health professionals in the three hospitals involved in the recruitment of participants of the study: Maastricht University Medical Centre+, VieCuri Medical Center, and Zuyderland Medical Centre. We would also like to thank the MEMIC center for data and information management for facilitating the logistic processes and data management of our study. Finally, we would like to thank the research dieticians and research assistant who are responsible for patient inclusion and follow-up, performing home visits, as well as data collection and processing. This study was funded by the Wereld Kanker Onderzoek Fonds (WKOF), as part of the World Cancer Research Fund International grant programme (Grant No. 2016/1620). The EnCoRe study is also funded by grants from the Stichting Alpe d'HuZes within the research program 'Leven met kanker' of the Dutch Cancer Society (Grant No. UM-2010-4867 and UM-2012-5653), by grants from Kankeronderzoekfonds Limburg as part of Health Foundation Limburg (Grant No. 00005739) and by a grant of the Wereld Kanker Onderzoek Fonds (WKOF), as part of the World Cancer Research Fund International grant programme (Grant No. 2017/1619). E.H. van Roekel is funded by the Wereld Kanker Onderzoek Fonds (WKOF), as part of the World Cancer Research Fund International grant programme (Grant No. 2016/1620).
Author information
Authors and Affiliations
Contributions
E.H.v.R., M.J.L.B., S.R.,. P.V., I.C.W.A., M.J.G., M.F.L., A.S. and M.P.W. conceived and designed the work; E.H.v.R., M.J.L.B., A.G., A.S. and M.P.W. acquired the data; E.H.v.R., M.J.L.B. and M.P.W. analyzed and interpreted the data; E.H.v.R. drafted the manuscript; all authors contributed to the advanced draft of the manuscript; all authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
van Roekel, E.H., Bours, M.J.L., van Delden, L. et al. Longitudinal associations of physical activity with plasma metabolites among colorectal cancer survivors up to 2 years after treatment. Sci Rep 11, 13738 (2021). https://doi.org/10.1038/s41598-021-92279-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-92279-9
This article is cited by
-
Habitual physical activity modulates cardiometabolic health in long-term testicular cancer survivors
Supportive Care in Cancer (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.