Abstract
Although exposure to particulate matter with aerodynamic diameters ≤ 2.5 µm (PM2.5) influences cardiovascular disease (CVD), its association with CVD-related hospitalizations of super-aged patients in Japan remains uncertain. We investigated the relationship between short-term PM2.5 exposure and CVD-related hospitalizations, lengths of hospital stays, and medical expenses. We analyzed the Japanese national database of patients with CVD (835,405) admitted to acute-care hospitals between 2012 and 2014. Patients with planned hospitalizations and those with missing PM2.5 exposure data were excluded. We classified the included patients into five quintiles based on their PM2.5 exposure: PM-5, -4, -3, -2, and -1 groups, in descending order of concentration. Compared with the PM-1 group, the other groups had higher hospitalization rates. The PM-3, -4, and -5 groups exhibited increased hospitalization durations and medical expenses, compared with the PM-1 group. Interestingly, the hospitalization period was longer for the ≥ 90-year-old group than for the ≤ 64-year-old group, yet the medical expenses were lower for the former group. Short-term PM2.5 exposure is associated with increased CVD-related hospitalizations, hospitalization durations, and medical expenses. The effects of incident CVDs were more marked in elderly than in younger patients. National PM2.5 concentrations should be reduced and the public should be aware of the risks.
Similar content being viewed by others
Introduction
Cardiovascular disease (CVD) is the leading cause of death due to non-communicable disease1. According to NHANES 2013 to 2016 data2, the CVD morbidity increases with age in both sexes, and the prevalence of coronary heart disease which is one of the major CVDs, is 6.7% in US adults. Particulate matter with aerodynamic diameters ≤ 2.5 µm (PM2.5) in the atmosphere increases cardiovascular morbidity and cardiovascular and overall mortality3,4 as well as the risk of developing CVDs, such as myocardial infarction5, heart failure6, arrhythmia7, hypertension8, and ischemic stroke9. According to the American Heart Association, the existing evidence supports a causal relationship between PM2.5 exposure and cardiovascular mortality and morbidity10.
Moreover, few previous studies have focused on the results for individuals > 90 years old. Japan is a super-aged society, with an average life expectancy of 80 years for men and 86 years for women11. Currently, there is a lack of clarity regarding whether CVDs in the super-aged societies of many countries are similarly affected by PM2.5 exposure and whether older people are more susceptible to such pollution than younger people. Most epidemiological studies focus on mortality data; thus, published studies have not examined the association between PM2.5 exposure and CVD-related health care costs, using Japanese nationwide databases. The aging of Japan’s population is not only resulting in a rapid population decline, it is also contributing to longer hospital stays and higher medical costs12,13.
To address these issues, we combined two nationwide databases. The Japanese Registry Of All cardiac and vascular Diseases (JROAD), which contains information on CVD diagnosis, hospitalization duration, and medical costs and the National Institute for Environmental Studies database includes data on environmental pollution. We conducted an observational study to investigate whether the prevalence of all CVDs and the related medical costs are related to short-term PM2.5 exposures.
Results
In the included study population, the median patient age was 76 years, and the male/female distribution was 58%/42%. The percentages of cases with acute myocardial infarction, heart failure, aortic disease, pulmonary embolism, and cardiac arrest were 10.6%, 29.3%, 5.5%, 1.2%, and 9.0%, respectively. A comparison of patient characteristics between the included and excluded patients is shown in Supplementary Table S1.
PM2.5 exposure and the CVD prevalence rate
Multilevel, mixed-effects Poisson regression (Table 1) revealed that the CVD prevalence rate was positively associated with an increase in PM2.5 exposure (prevalence ratio, 1.00071/1-μg/m3 of PM2.5; p < 0.001). Compared with that of the PM-1 group, the CVD-related hospitalization rate was higher for all the other groups (p < 0.001 for PM-5, -4, and -3; p = 0.025 for PM-2).
There was an interaction between PM2.5 exposure and age regarding their effect on the CVD prevalence rate (p < 0.001). Compared with that of the ≤ 64-year group, the effect of PM2.5 exposure on the CVD-related hospitalization rate was greater for all other age groups (all, p < 0.001).
PM2.5 exposure and length of hospital stay
Multilevel, mixed-effects linear regression (Table 2) demonstrated that the lengths of CVD-related hospital stays (log days) were positively associated with an increase in PM2.5 exposure (regression coefficient [95% confidence interval {CI}], 0.006 [0.005–0.008]/1-μg/m3 of PM2.5; p < 0.001) (Fig. 1a). Compared with that of the PM-1 group, the CVD-related hospital stays were longer for all other groups (p < 0.001 for PM-5, -4, and -3; p = 0.048 for PM-2).
Relationship between PM2.5 exposure and length of CVD-related hospital stays and in-hospital medical expenses. The predicted lengths of CVD-related hospital stays and in-hospital medical expenses were calculated using the “marginsplot” command in StataCorp 2015. Stata Statistical Software: Release 14. College Station, TX: StataCorp LP., after the multilevel, mixed-effects, linear regression analyses were performed, as indicated in Tables 2 and 3. Error bars represent predictive margins with 95% confidence intervals. (a) The overall predicted length of hospital stays. (b) The predicted lengths of hospital stays per age group. (c) The overall predicted in-hospital medical expenses. (d) The predicted in-hospital medical expenses per age group. Each age group is indicated by a different colored line (≤ 64 years [blue], 65–74 years [red], 75–89 years [green], and ≧ 90 years [yellow]) in b and d.
There was no evident interaction between PM2.5 exposure and age in terms of lengths of hospital stay (p = 0.871). CVD-related hospital stays were shorter for the ≤ 64-year group than for any other age group (all, p < 0.05) (Fig. 1b). There was a positive relationship between PM2.5 exposure and lengths of CVD-related hospital stays for all age groups, except the ≤ 64-year age group (p for trend, < 0.001).
PM2.5 exposure and in-hospital medical expenses
Multilevel, mixed-effects, linear regression analysis (Table 3) indicated that in-hospital medical expenses (log yen) were positively associated with an increase in PM2.5 exposure (regression coefficient [95% CI], 0.008 [0.007–0.009]/1-μg/m3 of PM2.5; p < 0.001) (Fig. 1c). Compared with those of the PM-1 group, the in-hospital medical expenses were higher in three of the other groups (p < 0.001 for PM-5, -4, and -3).
There was no interaction between PM2.5 exposure and age in terms of in-hospital medical expenses (p = 0.371). In-hospital medical expenses in the ≤ 64-year group were lower than those in the 65–74-y group and higher than those in the 75–89-year and ≥ 90-year groups (all, p < 0.05) (Fig. 1d). PM2.5 exposures and in-hospital medical expenses were positively correlated in all age groups, except the ≥ 90-year group (p for trend, < 0.001).
The specific risk estimates for the CVD prevalence rate on PM2.5 exposure are summarized in Supplementary Fig. S1. There was an interaction between PM2.5 exposure and age in terms of the effect on the CVD prevalence rate (p < 0.001). Compared with that of the ≤ 64-year group, the effect of PM2.5 exposure on the CVD-related hospitalization rate was greater for all other age groups (all, p < 0.001). The effect was greater in males; those with angina, acute myocardial infarction, heart failure, aortic disease, pulmonary embolism, atrial fibrillation or flutter, cardiac arrest; those in east Japan; and on weekdays (all, p < 0.001). The effect was also greater in the summer and winter than in the spring (both, p < 0.001), but contrarily, was less in the autumn (p < 0.001).
Discussion
We conducted an observational study using a Japanese nationwide registry database to investigate the effects of PM2.5 exposure on CVD-related hospitalizations. The outcomes of the study may be summarized as three main findings. (1) Short-term PM2.5 exposure is positively related to the prevalence rate of hospitalizations due to CVDs, particularly among the elderly. (2) Short-term PM2.5 exposure is positively associated with the lengths of CVD-related hospitalizations; hospitalizations tended to be longer for elderly patients than for younger patients. (3) Short-term PM2.5 exposure is positively related to in-hospital medical expenses, and medical expenses tend to be lowest for patients ≥ 90 years old (Fig. 1). These observations suggest that lowering PM2.5 exposures will reduce not only the risk of CVD development but also the lengths of hospital stays and medical expenses in a super-aged society.
The mechanism of the association between PM2.5 exposure and CVDs has been discussed extensively. Pope et al.14 discovered that acute PM2.5 exposure is associated with increased endothelial cell apoptosis and systemic inflammation in healthy young adults. Magari et al.15 observed a negative relationship between PM2.5 exposure and heart rate variability in the working population. Huang et al.16 indicated that seven days of exposure to high concentrations of PM2.5 is associated with substantial blood pressure increases. In addition to these reported mechanisms, the American Heart Association stated that short-term PM2.5 exposure is related to elevations in inflammatory markers, like C-reactive protein, systemic oxidative stress (negative biological impact on cells or tissues), thrombosis (impacts coagulation pathway), and epigenetic changes (subclinical pathophysiological responses)10. Additionally, a recent meta-analysis of PM2.5 exposure and all-cause mortality demonstrated increased risks of all-cause and cause-specific mortality related to short-term PM2.5 exposures, consistent with above-mentioned findings17. Further, Bonzini et al.18 observed that long-term PM2.5 exposure levels were associated with decreased prothrombin times, elevated endogenous thrombin potentials, and elevated C‐reactive protein concentrations in steel production workers. Ljungman et al.19 revealed that a 2-h increase in PM2.5 triggered ventricular arrhythmias in patients with implantable cardioverter-defibrillators. Thus, short-term PM2.5 exposures may cause endothelial dysfunction, increased oxidative stress, and inflammation, all of which may lead to CVDs20.
Of note, our study showed that the effects of PM2.5 exposure were more pronounced in elderly patients than in younger patients. The exact mechanism for this is not clear; however, the long-term effects of PM2.5 exposure include atherosclerosis. In large, population-based cohort studies of adults without pre-existing CVDs, long-term PM2.5 exposure was associated with incident hypertension21, retinal arteriolar narrowing22, coronary calcification23, thoracic aortic calcification24, and intima-media thickening25,26. These risk factors are also known to be associated with age and the development of CVDs, suggesting that short-term PM2.5 exposures may be the triggers associated with the higher risks of CVDs in the elderly, compared with younger people. The relationship between PM2.5 exposures and the development of the specific CVDs shown in the present study (Fig. S1) is compatible with this suggestion.
Non-CVD-related complications, such as organ damage, may explain why PM2.5 exposure prolongs hospital stays and increases medical expenses. For example, PM2.5 exposure is known to be associated with other underlying medical problems, such as pulmonary oxidative stress and disorders of the vasculature, blood flow, liver metabolism, nervous system, etc9,10,13,27.
An analysis of “big data” in a U.S. study of PM2.5 exposures (95,277,269 inpatient hospital claims between 2000 and 2012) demonstrated that each 1-µg/m3 increase in short-term PM2.5 exposure was associated with an annual increase of 20,098 hospitalization days (95% CI, 18,950–21,247 days) and 69 million USD (95% CI, 65–73 million USD) in inpatient and post-acute-care costs28. Our big-data analysis revealed a similar trend. An unexpected finding from our study was that the in-hospital medical costs of patients ≥ 90 years old were not positively related to increasing PM2.5 exposures, despite showing a positive relationship with the lengths of hospital stays. Although we did not investigate the reasons for this finding, Japan’s policy of not performing high-cost procedures on patients ≥ 90 years may contribute to this unexpected relationship.
PM2.5 exposure is not only a problem in Japan, but also in neighboring countries. CVDs are a growing public health concern in all countries with aging populations. Therefore, the findings of the present study may have important implications for CVD risk reduction and related health care costs in similar populations. Further, these results may guide public health interventions that minimize cardiovascular effects due to PM2.5 exposure.
The main strengths of our study are its large sample size and its national scale. Thus, the findings are expected to reflect the actual effects of PM2.5 exposures throughout Japan. Furthermore, we separately analyzed the data for patients ≥ 90 years old. One study limitation is that the data were obtained only from DPC hospitals with cardiovascular care facilities that meet the Japanese Circulation Society requirements (the characteristics of DPC hospitals were previously reported29). However, the JROAD is the largest database of nationwide cardiac health outcomes in Japan. Another limitation was that PM2.5 levels were measured at the local weather station closest to the hospital where the patient was admitted, not at the patient’s home address. Additionally, PM2.5 levels were not measured in the same way at each weather station. For example, the dataset does not include the altitude at which the measurements were made nor the sampling location’s proximity to a road. Therefore, some degree of potential exposure misclassification was unavoidable. Although we obtained the data from publicly available data observed by the National Institute for Environmental Studies, lack of detailed information on PM2.5 measurement may have biased our results towards the null. Further, we did not conduct specific analyses to distinguish between urban and rural areas or account for the socioeconomic status of each area; thus, we were unable to control for these potentially confounding factors. Moreover, the effect size of PM2.5 exposure on CVDs in this study was very small as we divided the number of CVDs admitted to DPC hospitals by the national population size. In addition, we only evaluated the effects of short-term PM2.5 exposures. Therefore, some CVD-related hospitalizations may be attributable to a “harvesting effect,” wherein the impending morbidity of the most vulnerable individuals in the population may merely have moved forward in time after a short-term PM2.5 exposure. This might be similar to one of the ischemic heart disease mortality conclusions from a published time series30 that “excluding short-term changes definitely lead to an increase in the estimated effect of air pollution.” Lastly, we showed the seasonal differences in CVD prevalence rates in Fig. S1; spring and autumn had negative impacts and summer and winter had positive impacts on the CVD prevalence rates associated with PM2.5 exposures. We plan to perform further investigations regarding these associations.
Conclusions
Our big-data analysis of Japan’s super-aged society demonstrated that PM2.5 exposure is associated not only with cardiovascular events but also with the lengths of CVD-related hospital stays and in-hospital medical expenses. Furthermore, the effects were more pronounced in elderly patients than in younger ones. Our findings suggest that reducing the burden of CVD-related diseases and their associated medical costs may require reducing the national PM2.5 concentrations. Increasing the public's awareness of the dangers of PM2.5 exposure is important.
Methods
Data collection
We collected the data for all acute-care hospital admissions due to any type of CVD from the JROAD. The JROAD is a nationwide, prospective registry designed to assess the clinical activity of Japanese hospitals that provide cardiovascular care and provide information for improving each hospital’s patient care31. The Japanese Circulation Society created both the JROAD, which includes each hospital's demographics since 2004, and the JROAD-DPC, which includes data from the Japanese Diagnosis Procedure Combination/Per-Diem Payment System (DPC/PDPS) since 2014.
The DPC database is a case-mix classification system linked with a lump-sum payment system, launched in 2002 by the Ministry of Health, Labour and Welfare of Japan31,32,33,34,35,36; academic, urban, and rural hospitals use the DPC system. All data analyzed in the present study were from patients hospitalized because of clinically apparent CVDs. The DPC database is based on the International Classification of Disease (ICD) code of the illness for which the most medical resources were invested and which represents the cause of hospitalization, including CVDs. Doctors registered the ICD codes of the illness when the patients were discharged. Since ICD codes are divided into acute and chronic diseases, we could differentiate between acute and scheduled admissions in the DPC database.
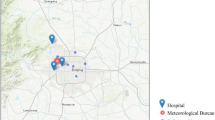
PM2.5 and weather data were obtained from the database of the National Institute for Environmental Studies37. We used hourly temperature and humidity data and calculated the average daily temperature and humidity values. We also noted the PM2.5 concentrations and weather values for the day preceding each patient’s emergency hospitalization due to CVD. The localized weather and air pollution data were obtained by identifying the weather station closest to each hospital. We searched the weather station sites using the municipality code specifically assigned to each municipality by the Ministry of Internal Affairs and Communications; this allowed us to merge the hospital sites with the monitoring stations closest to them. We used the previous day’s data since data from the same day would have included post-admission data because the exact time of each patient’s admission is not available in the database. Thus, the PM2.5 exposure data in this study reflects only the patients’ short-term exposures.
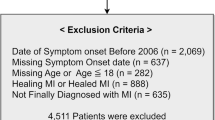
We conducted a cross-sectional study of the relationship between PM2.5 concentrations and CVD prevalence for the period between April 2012 and March 2014. We included 911 hospitals, where 2,369,165 consecutive patients were admitted during the study period. Patients were excluded due to: planned hospitalizations; missing PM2.5, temperature, or humidity data; or missing patient-characteristic data. Finally, 835,405 patients were included in the analysis (Fig. 2). Because the JROAD is not based on the numbers of patients but on DPCs, repeat admissions were considered as separate admissions. We classified the included patients into the following five groups, based on the ambient PM2.5 concentrations at the location where they were admitted: PM-5 (> 20.3 µg/m3), PM-4 (14.8–20.3 µg/m3), PM-3 (11.0–14.8 µg/m3), PM-2 (7.7–11.0 µg/m3), and PM-1 (< 7.7 µg/m3). We included analyses using PM2.5 as a continuous exposure in the supplementary materials (Supplementary Tables S2-4). The multivariable regression spline models (MVRS) command in Stata Statistical Software helped select the RS model that best predicts the outcome variables. MVRS analysis revealed a linear relationship between PM2.5 concentrations and some knots. The Japanese environmental standard for PM2.5 exposure is < 15 µg/m3 per day when averaged over a year, and < 35 µg/m3 as the maximum daily level.
This study design was approved by the Ethics Committee of St. Marianna University School of Medicine (No. 4038); the requirement for individual informed consent was waived because the data were anonymized when provided by the DPC. Further, this study was approved by the institutional review boards of all participating institutions and complies with the Declaration of Helsinki.
Outcomes
The primary outcome was the prevalence of CVDs requiring hospitalization. CVDs were defined to include coronary artery disease, heart failure, arrhythmia, aortic or peripheral artery disease, cardiac arrest, pulmonary embolism, pulmonary hypertension, and endocarditis/pericarditis. The prevalence in this study refers to the number of CVD patients admitted per day. For the 900 CVD patients who were admitted on 15/5/2012, the prevalence was 900. For the 800 CVD patients who were admitted on 16/5/2012, the prevalence was 800. The prevalence (daily admissions) was calculated daily for two years. Other outcomes were per patient hospitalization durations and associated medical expenses.
Statistical analyses
Patient characteristics are presented as medians and interquartile ranges for continuous values; categorical values are shown as frequencies and percentages. Wilcoxon’s rank-sum and chi-square test were used to compare the characteristics between included and excluded patients, in this study. A mixed, random-effects, population-averaged Poisson model was used to analyze the association between the number of CVD-related hospitalizations and PM2.5 exposures. The random effects were specified as the hospitals (institutions), using municipality codes to adjust for regional heterogeneity. Factors, such as hospital, weather, and patient factors were expected to contribute to the development of CVD. We modeled the association of PM2.5 concentrations with hospital data (eastern/western Japan; number of hospital beds; presence of coronary care unit[s], cardiac surgery service, and/or board-certificated cardiologists), weather data (season [Spring, March–May; Summer, June–August; Autumn, September–November; Winter, December–February], average temperature, and humidity), and patient demographics (age, sex, height, weight, Brinkman index38, and Charlson comorbidity index39). The Brinkman index is calculated as the product of the number of cigarettes smoked per day and the number of years of smoking. The Charlson comorbidity index is a score based on the presence or absence of 19 diseases that can influence mortality (congestive heart failure, chronic pulmonary disease, leukemia, metastatic tumor, etc.). These covariates thought to be related to the risk of developing CVD were carefully selected by experienced cardiologists. For the subgroup analysis, we classified the patients’ age into four groups according to the Japan Geriatrics Society guidelines40.
A mixed, random-effects, population-averaged linear model was used to analyze the associations of lengths of hospital stays and in-hospital medical expenses with PM2.5 exposures. The random effects were specified as the lengths of hospital stays and the in-hospital medical expenses. We modeled the association of PM2.5 exposure with hospital data, weather data, patient demographics, and CVD type (angina pectoris, acute myocardial infarction, heart failure, atrial fibrillation/flutter, aortic disease, cardiac arrest, pulmonary embolism, pulmonary hypertension, and tetralogy of Fallot). We included the CVD types in this model because in-hospital medical expenses and lengths of hospital stay may vary according to the CVD type. All analyses were performed in, and all graphs were constructed using, Stata Statistical Software: Release 14. (StataCorp LLC. 2015. College Station, TX, U.S.A.)
Data availability
The data that support the findings of this study are available from the JROAD, but restrictions apply to their availability; the data that were used were approved for use in the current study and are not publicly available. Data are, however, available from the JROAD upon reasonable request. Environmental pollution data are available from National Institute for Environmental Studies, Japan at http://www.nies.go.jp/db/index-e.html.
References
GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 396, 1204–1222 (2019).
National Center for Health Statistics. National Health and Nutrition Examination Survey (NHANES) public use data files. Centers for Disease Control and Prevention website. https://www.cdc.gov/nchs/nhanes (2020).
Cohen, A. J. et al. Estimates and 25-year trends of the global burden of disease attributable to ambient air pollution: an analysis of data from the Global Burden of Diseases Study 2015. Lancet 389, 1907–1918 (2017).
Pope, C. A. 3rd. et al. Lung cancer, cardiopulmonary mortality, and long-term exposure to fine particulate air pollution. JAMA 287, 1132–1141 (2002).
Madrigano, J. et al. Long-term exposure to PM2.5 and incidence of acute myocardial infarction. Environ. Health Perspect. 121, 192–196 (2013).
Shah, A. S. et al. Global association of air pollution and heart failure: a systematic review and meta-analysis. Lancet 382, 1039–1048 (2013).
Song, X. et al. Short-term exposure to air pollution and cardiac arrhythmia: a meta-analysis and systematic review. Int. J. Environ. Res. Public Health 13, 642 (2016).
Liang, R. et al. Effect of exposure to PM2.5 on blood pressure: a systematic review and meta-analysis. J. Hypertens. 32, 2130–2140 (2014).
Wellenius, G. A. et al. Ambient air pollution and the risk of acute ischemic stroke. Arch. Intern. Med. 172, 229–234 (2012).
Brook, R. D. et al. Particulate matter air pollution and cardiovascular disease: an update to the scientific statement from the American Heart Association. Circulation 121, 2331–2378 (2010).
Ministry of Health, Labour and Welfare. Annual Health, Labour and Welfare Report 2017, Overview of the system and the basic statistics, General Welfare and Labour: Trends in life expectancy. https://www.mhlw.go.jp/english/wp/wp-hw11/dl/01epdf (2017).
He, W. Goodkind, W. & Kowal, P. An aging world: 2015. United States Census Bureau. https://www.census.gov/library/publications/2016/demo/P95-16-1.html (2015).
Ministry of Health, Labour and Welfare. Annual Health, Labour and Welfare Report 2017, Overview of the system and the basic statistics, General Welfare and Labour: Changes in the general account expenditure budget classified by expense item allocated for MHLW. https://www.mhlw.go.jp/english/wp/wp-hw11/dl/01epdf (2017).
Pope, C. A. 3rd. et al. Exposure to fine particulate air pollution is associated with endothelial injury and systemic inflammation. Circ. Res. 119, 1204–1214 (2016).
Magari, S. R. et al. Association of heart rate variability with occupational and environmental exposure to particulate air pollution. Circulation 104, 986–991 (2001).
Huang, W. et al. Short-term blood pressure responses to ambient fine particulate matter exposures at the extremes of global air pollution concentrations. Am. J. Hypertens. 31, 590–599 (2018).
Orellano, P., Reynoso, J., Quaranta, N., Bardach, A. & Ciapponi, A. Short-term exposure to particulate matter (PM10 and PM2.5), nitrogen dioxide (NO2), and ozone (O3) and all-cause and cause-specific mortality: systematic review and meta-analysis. Environ. Int. 142, 105876 (2020).
Bonzini, M. et al. Effects of inhalable particulate matter on blood coagulation. J. Thromb. Haemost. 8, 662–668 (2010).
Ljungman, P. L. et al. Rapid effects of air pollution on ventricular arrhythmias. Eur. Heart J. 29, 2894–2901 (2008).
Munzel, T. et al. Effects of gaseous and solid constituents of air pollution on endothelial function. Eur. Heart J. 39, 3543–3550 (2018).
Fuks, K. B. et al. Long-term exposure to ambient air pollution and traffic noise and incident hypertension in seven cohorts of the European study of cohorts for air pollution effects (ESCAPE). Eur. Heart J. 38, 983–990 (2017).
Adar, S. D. et al. Air pollution and the microvasculature: a cross-sectional assessment of in vivo retinal images in the population-based multi-ethnic study of atherosclerosis (MESA). PLoS Med. 7, e1000372 (2010).
Kaufman, J. D. et al. Association between air pollution and coronary artery calcification within six metropolitan areas in the USA (the multi-ethnic study of atherosclerosis and air pollution): a longitudinal cohort study. Lancet 388, 696–704 (2016).
Kalsch, H. et al. Are air pollution and traffic noise independently associated with atherosclerosis: the Heinz Nixdorf Recall Study. Eur. Heart J. 35, 853–860 (2014).
Diez Roux, A. V. et al. Long-term exposure to ambient particulate matter and prevalence of subclinical atherosclerosis in the multi-ethnic study of atherosclerosis. Am. J. Epidemiol. 167, 667–675 (2008).
Bauer, M. et al. Urban particulate matter air pollution is associated with subclinical atherosclerosis: results from the HNR (Heinz Nixdorf Recall) study. J. Am. Coll. Cardiol. 56, 1803–1808 (2010).
Zanobetti, A., Dominici, F., Wang, Y. & Schwartz, J. D. A national case-crossover analysis of the short-term effect of PM2.5 on hospitalizations and mortality in subjects with diabetes and neurological disorders. Environ. Health 13, 38 (2014).
Wei, Y. et al. Short-term exposure to fine particulate matter and hospital admission risks and costs in the Medicare population: time stratified, case crossover study. BMJ 367, l6258 (2019).
Yoneyama, K. et al. Association between the number of board-certified cardiologists and the risk of in-hospital mortality: a nationwide study involving the Japanese registry of all cardiac and vascular diseases. BMJ Open 9, e024657 (2019).
Schwartz, J. Harvesting and long-term exposure effects in the relation between air pollution and mortality. Am. J. Epidemiol. 151, 440–448 (2000).
Yasuda, S. et al. The current status of cardiovascular medicine in Japan—analysis of a large number of health records from a nationwide claim-based database JROAD-DPC. Circ. J. 80, 2327–2335 (2016).
Yasunaga, H., Ide, H., Imamura, T. & Ohe, K. Impact of the Japanese diagnosis procedure combination-based payment system on cardiovascular medicine-related costs. Int. Heart J. 46, 855–866 (2005).
Yasunaga, H., Matsui, H., Horiguchi, H., Fushimi, K. & Matsuda, S. Application of the diagnosis procedure combination (DPC) data to clinical studies. J. UOEH 36, 191–197 (2014).
Nakamura, K. Diagnosis procedure combination database would develop nationwide clinical research in Japan. Circ. J. 80, 2289–2290 (2016).
Yasuda, S., Miyamoto, Y. & Ogawa, H. Current status of cardiovascular medicine in the aging society of Japan. Circulation 138, 965–967 (2018).
Nakao, K. et al. Prescription rates of guideline-directed medications are associated with in-hospital mortality among Japanese patients with acute myocardial infarction: a report from JROAD - DPC Study. J. Am. Heart Assoc. 8, e009692 (2019).
National Institute for Environmental Studies. http://www.nies.go.jp (2020).
Brinkman, G. L. & Coates, E. O. Jr. The effect of bronchitis, smoking, and occupation on ventilation. Am. Rev. Respir. Dis. 87, 684–693 (1963).
Charlson, M. E., Pompei, P., Ales, K. L. & Mackenzie, C. R. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J. Chronic Dis. 40, 373–383 (1987).
Ouchi, Y. et al. Redefining the elderly as aged 75 years and older: Proposal from the Joint Committee of Japan Gerontological Society and the Japan Geriatrics Society. Geriatr. Gerontol. Int. 17, 1045–1047 (2017).
Acknowledgement
We thank the other investigators, staff, and participants of the JROAD study for their valuable contributions. The full list of participating institutions is provided at http://jroadinfo.ncvc.go.jp.
Funding
This work was supported by the Japan Society for the Promotion of Science (KAKENHI Grant Number 18K08119).
Author information
Authors and Affiliations
Contributions
T.K. and K.Y. contributed equally to this work. K.Y., M.N., Y.M., S.Y., and H.O. had full access to all the data in the study and took responsibility for the integrity of the data and accuracy of the data analyses. All authors contributed to the design of the study. T.K., M.W., Y.S., M.I., Y.I., and Y.T. acquired, analyzed, and interpreted the data. T.K., K.Y., M.N., and T.H. drafted the manuscript. All authors critically reviewed the manuscript for important intellectual content. K.Y. and M.N. conducted statistical analyses. Y.M., Y.S., Y.I., T.H., S.Y., and H.O. provided administrative, technical, or material support. T.H., H.O., Y.M., S.Y., and Y.J.A supervised the study.
Corresponding author
Ethics declarations
Competing interests
Dr. Ogawa reports receiving personal fees from Towa Pharmaceutical Co., Ltd, Bristol-Meyers Squibb Co., Ltd, Pfizer Co., Ltd, Toa Eiyo Co., Ltd, Bayer Yakuhin Co., Ltd, and Novartis Pharma Co., Ltd, outside of the context of the submitted work. The other authors have no conflicts of interest to report.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kaihara, T., Yoneyama, K., Nakai, M. et al. Association of PM2.5 exposure with hospitalization for cardiovascular disease in elderly individuals in Japan. Sci Rep 11, 9897 (2021). https://doi.org/10.1038/s41598-021-89290-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-89290-5
This article is cited by
-
Association of ambient particulate matter with hospital admissions, length of hospital stay, and hospital costs due to cardiovascular disease: time-series analysis based on data from the Shanghai Medical Insurance System from 2016 to 2019
Environmental Sciences Europe (2023)
-
Association between satellite-based estimates of long-term PM2.5 exposure and cardiovascular disease: evidence from the Indonesian Family Life Survey
Environmental Science and Pollution Research (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.