Abstract
The article presents a comparative analysis of SARS-CoV-2 viral load (VL), T lymphocyte count and respiratory index PaO2:FiO2 ratio as prospective markers of COVID-19 course severity and prognosis. 8806 patients and asymptomatic carriers were investigated in time interval 15 March–19 December 2020. T cell count demonstrated better applicability as a marker of aggravating COVID-19 clinical course and unfavourable disease prognosis than SARS-CoV-2 VL or PaO2:FiO2 ratio taken alone. Using T cell count in clinical practice may provide an opportunity of early prediction of deteriorating a patient’s state.
Similar content being viewed by others
Introduction
There is a definite need in laboratory markers of COVID-19 clinical course severity and prediction of the disease outcome. Several COVID-19 prognosis predicting models have been proposed lately1,2,3,4,5,6,7. Most of them are one-factor, but there are complex multifactor models too. Skevaki et al.8 and Galloway et al.9 used data on severe COVID-19 patients, trying to identify the major laboratory markers of very serious cases and mortality. In these studies, the data obtained on laboratory markers were rather contradictory. Most importantly, the size of sample sets was restricted (several dozen or several hundred patients at the utmost). Limited volume of experimental data may have been the main reason of many models’ low accuracy observed hitherto.
Currently SARS-CoV-2 viral load (VL) is almost universally regarded as a factor directly related to COVID-19 severity and prognosis and, therefore, one of the major indicators of the disease progression10,11,12,13,14. However, recently it has been demonstrated by a number of research groups that it may be an oversimplified, if not incorrect approach15,16,17,18,19,20. According to the recent findings, VL may indicate some COVID-19 severe cases such as “cytokine storm” or serious disease progression in immunosuppressed patients but is problematic to apply as a marker of COVID-19 severity universally21,22,23,24. For VL to become a reliable marker of COVID-19 severity, in most cases it must be supplemented with other markers, as merely one parameter can be hardly used for a satisfactory description of such complex system as a full set of COVID-19 clinical manifestation25,26,27. We think that T-cell immune response may be a good choice.
We report our findings in studying interdependence of
-
1.
SARS-CoV-2 VL,
-
2.
Leukocyte, B and T lymphocyte count,
-
3.
Respiratory marker PaO2:FiO2 ratio
in COVID-19 patients/carriers to find the most demonstrative laboratory markers of COVID-19 clinical course severity and prognosis.
Methods
Patients and clinical data
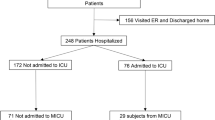
8806 patients/carriers were investigated since 15 March to 19 December 2020, whose SARS-CoV-2 positive status was initially proven by molecular biology. Objective and subjective information about COVID-19 clinical manifestations was recorded in hospitals and clinics in twelve Russian regions (Moscow, Moscow region, St Petersburg, Nizhny Novgorod, Murmansk, Dagestan, Komi, Krasnoyarsk, Tyumen, Krasnodar, Khabarovsk, and Vladivostok).
Twenty-six hospitals, thirty-four outpatients’ clinics and ambulance centres, and sixteen non-commercial test labs and medical centres were involved in the research. Symptomatic patients and asymptomatic carriers were included in the group. The patient sample set composition gives an opportunity to regard the set as random. Age, gender, results of general clinical blood tests, X-ray CT results, clinical symptomatic picture (or the fact of symptoms absence for asymptomatic carriers), time of symptom onset, clinical procedures including admission to general wards and ICU as well as outcome were known. No patient identifying information was known or disclosed.
Measurements
RT-qPCR technique was applied to make SARS-CoV-2 VL measurements (Bio-Rad CFX Automation System II, Hercules, CA, USA+ Vector Multiplex RT-qPCR SARS-CoV-2 Test Kit, Novosibirsk, Russia). The nasopharyngeal or oropharyngeal swabs were taken in clinics/hospitals or at home in case of asymptomatic or mild symptomatic carriers and COVID-19 out-patients. Flow immunofluorocytometry (MACSQuant Analyzer 16 Flow Cytometer, Miltenyi Biotec, Bergisch Gladbach, Germany) with necessary Miltenyi Biotec and Vector reagents and kits was used for performing immunological cell blood analyses. For isolation of T killer cells, MACSxpress CD8 T Cell Isolation Kit was used + specific marker presence/absence check during flow cytometry CD27– CD28– CD45RA+ Perforin+; for Th1 helpers MACSxpress CD4 T Cell Isolation Kit + IFN-γ Secretion Assay—Cell Enrichment and Detection Kit; for isolation of γδT cells Anti-TCRγ/δ MicroBead Kit; for NKT cells Anti-iNKT MicroBeads; for CD8αα+ cells Vector CD8 homodimer Isolation Kit; for B1 cells Miltenyi Biotec StraightFrom Whole Blood CD19 MicroBead Kit, StraightFrom Whole Blood CD45 MicroBead Kit + CD20 and CD43 markers presence on cytometry; for plasma cells Miltenyi Biotec StraightFrom Whole Blood CD138 MicroBeads.
For symptomatic patients, VL was measured in nasopharyngeal/oropharyngeal swabs taken on Days 1–4 since symptomatic onset. The day of onset was taken as Day Zero. According to the literature28,29,30,31,32,33, VL is maximal approximately at this time, for COVID-19 symptomatic clinical course. For asymptomatic carriers, if a test for SARS-CoV-2 RNA was positive and the person in question expressed his/her wish to participate in the research, the day of test was conventionally counted as Day Zero and subsequent days received corresponding numbers. Total leukocyte count and B1 cell counts were measured in blood samples taken on Days 2–4. Plasma cell and T cell counts were measured on Days 8–12 in serum and pharyngeal mucosa-associated lymphoid tissue (MALT). As we found in another study of a relatively small group of HIV/SARS-CoV-2 co-infected people, the maximum of T cell response to SARS-CoV-2 acute infection is usually observed since Day 6 to 1634. As well, PaO2/FiO2 ratio was measured on Days 8–12 (1) to correspond roughly with T cell measurements; and (2) since it was demonstrated by different groups of researchers that severe COVID-19-associated ARDS is generally detected after the first week of the COVID-19 disease35,36,37,38. Two separate intakes and two separate measurements with calculating the average value were made in every analysis, to reduce the contribution of experimental errors.
Subjective symptomatic score
We introduced a so-called “subjective symptomatic score” whose invention was partly inspired by methodology described in works of Calza et al.39 and Galloway et al.9. However, we used our own modification of this factor. The presence of every symptom has a score of + 1 – + 5 depending on the pronouncedness, its absence 0. Medical personnel was consulted to apply such a system of evaluation and we received the numerical data in the majority of cases. Where numerical data were missing, we transformed qualitative description of symptomatic course into the score discussed, by ourselves. While the symptomatic picture is definitely subjective as it is based on personal perception of COVID-19 symptoms or observations of medical staff and therefore qualitative, the score may give a semi-quantitative indication of COVID-19 course severity. The list of symptoms taken into account are summarized in Table 1.
As one can conclude, asymptomatic carriers had the total score of 0. The maximal possible value is 5 × 20 = 100. When calculating subjective symptomatic score for symptomatic cohort, we did not count asymptomatic values lest the score should be greatly skewed to low values.
Acute respiratory distress syndrome (ARDS) score
We suggest using ARDS score AS to assess COVID-19 respiratory complications. We may define it as
where RR is respiratory rate [min–1]. The detailed description of this indicator is provided in our another work34. An advantage of using AS over any of PaO2/FiO2 ratio, SpO2 or RR can be explained by the complex nature of AS. AS encompasses more border states of ARDS than any of these three indicators. Therefore, in some cases using AS may be more reliable as it usually highlights suspicious cases of ARDS that some of the three separate indicators may miss.
The formula for AS contains reversed PaO2/FiO2 ratio as the first item (with multiplier 1000 taken for convenience). It explains why we used reversed PaO2/FiO2 ratio in the current study instead of PaO2/FiO2 ratio that is generally used as an indicator of respiratory state of a patient. Indeed, we searched for direct proportionality between VL and COVID-19 respiratory complications. One can expect that high VLs may potentially indicate severe respiratory failure, as it was shown in numerous research papers, e.g. in the works40,41,42. Low PaO2/FiO2 ratio values which stand for respiratory failure do not correlate with high VLs as direct proportionality, but high reversed PaO2/FiO2 ratios do. However, using reversed PaO2/FiO2 ratio was a mere convention dictated by the simplicity of formulas in the current study. It can be easily substituted by PaO2/FiO2 ratio.
Statistical analysis and visualisation
OriginPro ver. 9.2.196 (OriginLab Corporation, Northampton, Mass., USA, https://www.originlab.com) was used for statistical calculations and visualisation.
Type of study
The study does not represent a randomised controlled clinical trial. All relevant measurements and data processing were performed retrospectively. Reporting of the study conforms to broad EQUATOR guidelines.
Informed consent for participation and publication
An informed consent has been given by the patients for using their anonymised clinical data for scientific investigations and publication. It was duly signed and kept in the respective medical institutions. For minor human participants under the age of 18 years, informed consent has been obtained from their parent and/or legal guardian.
Ethics guidelines
The Ethical Committee of Koltzov Institute of Developmental Biology of Russian Academy of Sciences regarded the current study ethically appropriate and exempt from human subjects review, as (1) no private identifying information was known and, consequently, disclosed by the authors; (2) all experiments were performed in accordance with relevant guidelines and regulations; and (3) all the methods used were approved as conforming to the relevant guidelines and regulations (permission no. 39100920).
Ethics approval
Granted by Ethical Committee of Koltzov Institute of Developmental Biology of Russian Academy of Sciences (no. 39100920).
Results and discussion
Main clinical parameters
Demographics and main clinical parameters of the patients are summarised in Table 2.
SARS-CoV-2 viral load as prospective marker of COVID-19 course severity
Figure 1 demonstrates relationship between SARS-CoV-2 VL and reversed PaO2/FiO2 ratio (the first item in the formula for ARDS score AS, see “Methods” section).
Correlation between reversed PaO2/FiO2 ratio as an indicator of COVID-19 respiratory complications severity (the first item in ARDS score formula) and SARS-CoV-2 VL. In this and subsequent figures Confidence interval (CI) is 95%. Standard error of mean is showed as whiskers. Green dash-dotted line stands for the conditional border between asymptomatic carriers and symptomatic patients. Red dash-dotted line stands for the conditional border between extremely severe clinical cases and the rest of the patients. Percentage numbers in parentheses (green) correspond to the proportion of asymptomatic carriers whose manifestations fit into the conditional range to the left of the green line. Created in OriginPro ver. 9.2.196, https://www.originlab.com.
We can observe that there is no clear correlation between reversed PaO2/FiO2 ratio and VL for the whole range of VLs. None the less, the almost linear piecewise dependence of reversed PaO2/FiO2 ratio on SARS-CoV-2 VL (several linear fragments) helps to isolate asymptomatic carriers (the leftmost points in Fig. 1) and severest cases (the rightmost points), whereas the majority of VLs corresponds to approximately the same reversed PaO2/FiO2 ratio = 3.6 ± 1.3 mmHg–1 (horizontal plateau in the middle of Fig. 1). That corresponds to direct PaO2/FiO2 ratio range = [204…434 mmHg].
Statistical analysis gave the following results. For reversed PaO2/FiO2 ratio dependence on VL (Fig. 1), approximation function was logistic function of accumulation (sigmoidal):
with coefficients: A1 = 2.1200, A1 (SE—henceforward Standard Error of Mean) = 0.1188 [mmHg–1]; A2 = 3.5585, A2 (SE) = 0.0718 [mmHg–1]; VL0 = 24,532, VL0 (SE) = 14,032 [RNA copies per reaction]; p = 2.8127, p (SE) = 1.9974. The statistical analysis parameters: χred.2 = 0.0646; Radj.2 = 0.8688, Fisher coefficient F = 787.77.
In Fig. 1 we see that only very high VL led to the distortion of plateau PaO2/FiO2 = 281 mmHg (to the right of the red vertical line, i.e. further diminishing PaO2/FiO2), whereas the majority of VLs were statistically undistinguishable in terms of PaO2/FiO2 ratio.
Leukocyte and B lymphocyte counts in serum as prospective markers of COVID-19 course severity
In Fig. 2 one can see the dependence of total leukocyte count in serum on logarithm of SARS-CoV-2 VL and in Fig. 3 the dependence of B lymphocyte subpopulation counts on logarithm of SARS-CoV-2 VL. Leukocyte count (more exactly, granulocyte count) may be understood as a common indicator of the front line of innate immune system response to SARS-CoV-2 and B cell counts as parts of both innate and adaptive immune response. However, again we do not observe any direct proportionality between VL and overall white blood cell counts, nor B lymphocyte counts, as the correlations are non-linear or there are no correlation at all (for B1 cells, Fig. 3).
Correlation between leukocyte count in serum on logarithm of SARS-CoV-2 VL. Created in OriginPro ver. 9.2.196, https://www.originlab.com.
Correlation between B1 cell (light green line) and plasma cell (dark green line) counts in serum on logarithm of SARS-CoV-2 VL. Created in OriginPro ver. 9.2.196, https://www.originlab.com.
Both leukocyte and plasma cell count correlations with SARS-CoV-2 VL have an asymmetric wave shape with maximums around VLs of 105–108 RNA equivalents per reaction. These maximums correspond with the majority of symptomatic patients. In asymptomatic carriers, immune response is not pronounced and almost all severest cases were cases of patients with chronic immune problems. This may indicate that the strongest immune response (innate and adaptive) to SARS-CoV-2 is present in COVID-19 symptomatic or at least paucisymptomatic patients without serious immune disorders.
Therefore, we may suggest that neither overall white blood cell count, nor B cell count can serve as an evident marker of COVID-19 clinical course severity.
Viral load and severe clinical cases
In the works24,43,44 it was assumed that SARS-CoV-2 VL may be an indicator of COVID-19 course severity in specific disease cases, e.g. in the severest cases or complications. We suggested that VL might correlate with the most serious cases. In Fig. 4, we plot the distribution of VLs in the severest COVID-19 patients.
Distribution of SARS-CoV-2 VLs in severe clinical cases: (1) serious viral interstitial pneumonia with X-ray computer tomography opaqueness not less than 15% (469 cases, 5.33%); (2) severe respiratory failure of type 1 [either of PaO2/FiO2 ratio < 280 mmHg OR respiratory rate > 30 min–1 OR SpO2 < 90% (ARDS score AS > 10–12)] (103 cases, 1.17%); (3) pulmonary embolism (48 cases, 0.55%); (4) immune response dysregulation known as “cytokine storm” (37 cases, 0.42%); (5) internal organ malfunction (11 cases, 0.12%); (6) transfer from general ward to ICU (202 cases, 2.29%); (7) lethal outcome (71 cases, 0.81%). Individual cases and statistical boxes are visualised along each other. Boxes: 25/50/75%. Whiskers: 5/95%. Horizontal lines are maximums/minimums, crosses stand for 1/99%. Created in OriginPro ver. 9.2.196, https://www.originlab.com.
A careful look at Fig. 4 proves that SARS-CoV-2 VL cannot be used as an unequivocal marker of COVID-19 complications, excepting internal organ malfunction (orange box). Very broad ranges of VLs correspond with COVID-19 serious complications (pronounced interstitial pneumonia, respiratory failure, acute respiratory distress syndrome (ARDS), pulmonary embolism, “cytokine storm,” etc.).
T lymphocyte count as prospective marker of COVID-19 course severity
To find such markers, we studied correlation between (1) VL and T lymphocyte counts (Fig. 5); and (2) reversed PaO2/FiO2 ratio and T lymphocyte counts (Fig. 6).
T cell count dependence on logarithm of SARS-CoV-2 VL. Piecewise and smooth approximations are shown. Green dash-dotted line stands for the conditional border between asymptomatic carriers and symptomatic patients. Red dash-dotted line stands for the conditional border between extremely severe clinical cases and the rest of the patients. Percentage numbers in parentheses (green) correspond to the proportion of asymptomatic carriers whose manifestations fit into the conditional range to the left of the green line. (A) T killer (CD8+ cytotoxic lymphocyte) count (in serum) dependency on log10VL. (B) Th1 helper (CD4+ CD94 + lymphocyte) count (in serum) dependency on log10VL. (C) γδT and NKT lymphocyte counts (in serum) dependency on log10VL. (D) CD8αα+ lymphocyte count (in pharynx MALT analysed in nasopharyngeal or oropharyngeal swabs) dependency on log10VL. Created in OriginPro ver. 9.2.196, https://www.originlab.com.
T cell count dependence on respiratory factor reversed PaO2/FiO2 ratio. Linear piecewise approximation is shown. (A) T killer and NKT cell counts dependency on PaO2/FiO2 ratio. (B) γδT and CD8αα+ cell counts dependency on PaO2/FiO2 ratio. Created in OriginPro ver. 9.2.196, https://www.originlab.com.
Dependence of T killer (cytotoxic CD8+ T lymphocyte) [membrane phenotype CD3+ CD8+ CD45RA+ CD27– CD28– CCR7– CD178(FasL)+ CD107a(LAMP-1)+ IFNγ+ Granzyme B+ Perforin-1+] count (Fig. 5A) and Th1 helper [membrane phenotype CD3+ CD4+ CD94 + CD183(CXCR3)+ CD195(CCR5)+ CCR3– CCR4– CXCR4–] count/10 (one tenth part) (Fig. 5B) in serum on logarithm of SARS-CoV-2 VL provides a promising instrument for marking very serious and aggravating COVID-19 clinical cases. Correlation between T killer and Th1 helper counts was very strong (Pearson correlation coefficient C = 0.91371, p = 0.01258).
Dependence of γδT [membrane phenotype CD3+ TCRγ/δ+ IFNγ+] and NKT [membrane phenotype CD3+ CD161(NK1.1/NKR-P1)+ CD16+ CD56+ CD57+ CD44+ CD69+] lymphocyte count on logarithm of SARS-CoV-2 VL (Fig. 5C) demonstrates the absence of statistically significant dependence of cell count on VLs for asymptomatic/symptomatic patients/carriers distinguishing. For extremely severe (critical) cases, a strict diminishment was observed. It may be an indication that SARS-CoV-2 influence on immunity is related to mainly adaptive immunity, as NKT cell selection and homeostasis are connected with adaptive immunity regulation, whereas γδT cells are a part of innate immunity.
Distribution of CD8αα+ cells on VL is presented in Fig. 5D. Homodimeric CD8αα+ cells are a “non-classical” subpopulation of γδT-lymphocytes whose membrane phenotype may be described as CD3+ CD8αα+ CD2– CD5– CD28– CD4+/–45,46. Instead of dimer ζ2, in their TCR they contain homodimer FcεRIγ/FcεRIγ or heterodimer ζ/FcεRIγ. Homodimer CD8αα does not act as a co-receptor—otherwise CD8αα+ cells could recognise an antigen presented within MHC-I, and CD8αα+ response to antigen is likely to proceed with “non-classical” MHC-I molecules, probably along Qa or TL pathways.
In Fig. 6, dependence of T lymphocyte population size on reversed PaO2/FiO2 ratio is presented.
Here the dependence is much stronger than the dependence on VL. Statistically significant difference in T killer, NKT cell (Fig. 6A), γδT and CD8αα+ cell population size (Fig. 6B) gives an opportunity to use this functional relation as a more unequivocal marker of COVID-19 course severity than T cell count—VL dependency. We did not detect any connection of CD8αα+ cell count on SARS-CoV-2 VL (Fig. 5D), but observed strong diminishment of CD8αα+ lymphocyte population size in pharynx MALT with the growth of respiratory distress severity (Fig. 6B).
Markers of clinical course outcome, mortality and prognosis
To find a convincing marker of COVID-19 clinical course outcome, including mortality, may be regarded a separate important task in suggesting markers for COVID-19 clinical course predictions.
COVID-19-related mortality was closely connected with T cell population suppression in severest cases. T cell population size diminishment (especially of T killers, Th1 helpers, and CD8αα+ lymphocytes) was more closely connected with COVID-19-related mortality (Pearson correlation coefficient C = 0.7411 at p = 0.1217) than PaO2/FiO2 ratio with COVID-19-related mortality (C = 0.6238 at p = 0.2150). But even more importantly, as we detected, strong diminution of T cell populations often (in 58.22% cases) shows deterioration of a patient’s conditions 2–5 days before worsening his/her respiratory status measured by PaO2/FiO2 ratio.
The mortality distribution on VLs (Fig. 4, rightmost dark-grey box) did not demonstrate direct proportionality relationship between VL (or its reversed logarithm \(\frac{1}{{\log_{10} {\text{VL}}}}\)) and lethal outcome. While mortality net number was distributed in an asymmetric peak-like mode, not Gaussian mode, the distribution of mortality percentage did not show any clear dependence on VL (Fig. 7A). The approximation dependence
Dependence of in-group mortality percentage on VL (A) and CF1 (B), experimental data and approximation. For detailed description please see the text. Created in OriginPro ver. 9.2.196, https://www.originlab.com.
is very weak and even unreliable, that can be observed from the poor approximation parameters values: a = 26.82, a (SE) = 1.53; b = 2.39, b (SE) = 3.08; Fisher coefficient F = 0.6030; Pearson’s r coefficient = 0.1566; Radj.2 = –0.0161. The prediction force is low and, for severest COVID-19 cases, mortality percentage prediction deviates enormously from 8 to 40%.
However, the mortality percentage distribution on the product of several factors (“complex factor” CF1)
did demonstrate a stronger dependence (Fig. 7B). The best fit can be achieved through approximating by biphasic dose–response function:
A1 = 3.58, A1 (SE) = 2.38; A2 = 3906.18, A2 (SE) = 1380.15; log10 x1 = 482.38, log10 x1 (SE) = 55.14; log10 x2 = –19,014.35, log10 x2 (SE) = 4639.34; h1 = –0.0040; h1 (SE) = 0.0027; h2 = –0.000121; h2 (SE) = 0.000397; p = 0.00729; p (SE) = 0.00925.
By comparing results of the statistical analyses, we see that the complex factor CF1 is more promising for using as an input variable for predicting lethal outcome than VL. In the defining formula for CF1, we did not include Th1 helper count, as Th1 count was shown to be very strongly correlated with T killer count (Fig. 5A,B). Therefore, of the two variables T killer and Th1 helper counts, a truly independent variable is merely one.
The approximation by biphasic dose–response function is still imperfect and 95% confidence interval boundaries are very wide (Fig. 7B). E.g., for COVID-19 severest clinical course (CF1 < 300) μl–3, prediction range for mortality percentage spans from 34 to 66%. However, this approximation provides one of the most precise predictive ranges for mortality.
Limitations of the study
The research has serious limitations that cannot be ignored, despite considerable size of the set studied.
-
1.
The range of patients’ demographics is extremely broad. Such breadth is a result of initial randomising approach of the study, which was aimed at collecting data from a most representative population set. However, such an approach has as well drawback as advantages. Patients with quite different comorbidities entered the set, as there was no filtration of patients/carriers. In the study, the influence of comorbidities on COVID-19 clinical course was not studied quantitatively and thoroughly, as it may be a task for a separate investigation. Different comorbidities may lead to quite dissimilar COVID-19 clinical course and blur the VL/ARDS score/T cell count relationships. It was not paid due attention in the current work.
-
2.
The main conclusion of the study is T cells counts’ being the best predictive markers for COVID-19 clinical course and mortality. Therefore, it may be implied that effective adaptive immune system response plays a major role in positive prognosis and immune impairments deteriorate the prognosis. However, we did not specifically and assiduously investigate patients with immunity disorders (we merely took into consideration the fact of clinically documented immunity diseases), nor immunity deterioration with age. As the set was very broad, many aged persons and people with impaired immunity were included in it, but their immunity functioning (e.g., median levels of T cell serum concentrations in the presence and absence of an acute infectious disease) before COVID-19 was not taken into account. This oversimplifying might distort the results to considerable degree.
-
3.
After the extensive research, it is still unclear whether SARS-CoV-2 causes lymphopenia or, on the contrary, “cytokine storm” (hyperinflammation) as its most probable effect on immunity of a conditionally healthy adult. There are plenty of works supporting either assumption. The data obtained in our research cannot support a suggestion that SARS-CoV-2 causes any significant CD8+ and CD4+ lymphopenia itself, even less so suppression of other T lymphocyte populations. It is highly possible that SARS-CoV-2 may be an exacerbating factor of immune dysfunctions or diseases already present in people with serious disease- or age-related lymphocyte population decrease. E.g. HIV, HBV, HCV, immunosuppressed status after anti-cancer chemotherapy, organ/tissue transplantation/grafting etc. may cause substantial lymphopenia that SARS-CoV-2 may exaggerate further.
We ground our assumption on the following observation. Of all deaths registered for patients with more than twofold T cell count diminution (either of T killer, Th1 helper, NKT cells, γδT cells or CD8αα+ cells), 87.4% were also associated with immune dysregulation/diseases not related to SARS-CoV-2 and clinically documented before the pandemic. Therefore, we suggest that the assumption about SARS-CoV-2’s resulting in immune dysregulation of a healthy person, should be re-evaluated on a more clinically checked set of SARS-CoV-2 carriers/patients, ideally in randomised controlled clinical trials.
Primary targeting T killer and NKT cell populations instead of CD4+ lymphocyte population hints that SARS-CoV-2 influence on cell immunity is completely dissimilar with HIV-1. Indeed, it is possible that SARS-CoV-2 can act as an inductor or “amplifier” of immune disorders/dysfunction. If this is true, in most patients SARS-CoV-2 does not cause lymphopenia itself, rather only augments it, possibly like influenza or some other respiratory viruse (e.g. parainfluenza viruses)47,48,49,50,51,52,53.
However, the role of SARS-CoV-2 in lymphopenia, whether it is primary or secondary, was not studied. Suppression of lymphocyte population size (lymphopenia) needs a further detailed research. We do not know biochemical mechanisms of such lymphopenia, i.e. whether they are related to membrane protein degradation or another distortion of T cell differentiation or activation.
-
4.
SARS-CoV-2 was found to cause a wave-form correlation of leukocyte and plasma cell serum concentrations with VL in the majority of symptomatic patients and typical VLs of 105–108 RNA copies per reaction were determined to correspond with the maximum of the wave. This fact was not possible to interpret in the current study within any theory of immune response.
-
5.
It is clear that SARS-CoV-2 targets adaptive immunity much more than innate immunity, and T and NKT cells more than γδT cells. However, homodimeric CD8αα+ lymphocyte population (a part of innate immunity) in pharyngeal MALT (and hence very likely in all parts of the upper respiratory tract MALT) is very seriously affected in severe COVID-19 cases and may be the best marker of a patient’s respiratory state deterioration. The finding has not yet been fully interpreted and comprehended in this research, partly because insufficiency of our data and partly because the role of CD8αα+ cells in human immune system is still not completely clear.
-
6.
We had a rather arbitrary choice of measurement time of VL, PaO2/FiO2 ratio and leukocyte/lymphocyte counts, as specified in Methods section. No longitudinal studies were made in this work. The time of measurement was approximately the same for all carriers/patients that allowed to reduce the dispersion of results. However, we have to remember that dynamics of the parameters studied is very important, as these parameters change with COVID-19 clinical course and, according to the remark of our Reviewer, their alteration may indicate improvement or progression of COVID-19.
-
7.
For the majority of patients, no immune tests have been ever made before the onset of COVID-19 disease (or detecting the asymptomatic course). We may only assume that their immune indicators (B and T cell counts) were within normal range of a conventionally healthy adult before COVID-19.
Conclusions
-
1.
T lymphocyte count may be a perspective marker of COVID-19 course severity and prognosis, more unambiguous than SARS-CoV-2 VL in the upper respiratory tract or respiratory index PaO2/FiO2. Using T cell count in clinical practice may provide an opportunity of early prediction of deteriorating a patient’s state.
-
2.
A very broad range of SARS-CoV-2 VL (50–1013 RNA copies per reaction) may correspond to similar complications of COVID-19. That makes VL a poor indicator of COVID-19 clinical course severity.
-
3.
Asymptomatic SARS-CoV-2 carriers, whose percentage in SARS-CoV-2-affected population was found to be large (more than two thirds of all infected persons), do not demonstrate any significant changes in the levels of B and T lymphocytes, while VLs in these carriers remain low.
-
4.
The best marker of mortality was found to be a “complex factor” that can be calculated as a product of reversed logarithm of VL, T killer count, plasma cell count and NKT cell count in serum. The lowest values of this factor highlight extremely severe cases of COVID-19 disease with negative prognosis.
-
5.
The best predictive marker of COVID-19-related severe ARDS was detected to be CD8αα+ lymphocyte count in pharyngeal MALT. Its sharp reduction may be used in clinical practice as an unambiguous indicator of necessity to admit a patient to ICU wards.
Data availability
Available upon a reasonable request.
References
Luo, Y. et al. Prediction model based on the combination of cytokines and lymphocyte subsets for prognosis of SARS-CoV-2 infection. J. Clin. Immunol. https://doi.org/10.1007/s10875-020-00821-7 (2020).
Merckx, J., Labrecque, J. A. & Kaufman, J. S. Transmission of SARS-CoV-2 by Children. Dtsch. Arztebl. Int. 117(33–34), 553–560. https://doi.org/10.3238/arztebl.2020.0553 (2020).
Parrill, A., Tsao, T., Dong, V. & Huy, N. T. SARS-CoV-2-induced immunodysregulation and the need for higher clinical suspicion for co-infection and secondary infection in COVID-19 patients. J. Microbiol. Immunol. Infect. https://doi.org/10.1016/j.jmii.2020.08.016 (2020).
Wellinghausen, N. et al. SARS-CoV-2-IgG response is different in COVID-19 outpatients and asymptomatic contact persons. J. Clin. Virol. 130, 104542. https://doi.org/10.1016/j.jcv.2020.104542 (2020).
Valba, O. V., Avetisov, V. A., Gorsky, A. S. & Nechaev, S. K. Evaluating ideologies of coronacrisis-related self-isolation and frontiers closing by SIR compartmental epidemiological model. Beacon J. Stud. Ideol. Ment. Dimens. 3(2), 020210318 (2020).
Wang, S. et al. Modeling the viral dynamics of SARS-CoV-2 infection. Math. Biosci. 328, 108438. https://doi.org/10.1016/j.mbs.2020.108438 (2020).
Malkov, E. Simulation of coronavirus disease 2019 (COVID-19) scenarios with possibility of reinfection. Chaos Solitons Fract. 139, 110296. https://doi.org/10.1016/j.chaos.2020.110296 (2020).
Skevaki, C. et al. Laboratory characteristics of patients infected with the novel SARS-CoV-2 virus. J. Infect. 81(2), 205–212. https://doi.org/10.1016/j.jinf.2020.06.039 (2020).
Galloway, J. B. et al. A clinical risk score to identify patients with COVID-19 at high risk of critical care admission or death: An observational cohort study. J. Infect. 81(2), 282–288. https://doi.org/10.1016/j.jinf.2020.05.064 (2020).
Yu, F. et al. Quantitative detection and viral load analysis of SARS-CoV-2 in infected patients. Clin. Infect. Dis. 71(15), 793–798. https://doi.org/10.1093/cid/ciaa345 (2020).
Zheng, S. et al. Viral load dynamics and disease severity in patients infected with SARS-CoV-2 in Zhejiang province, China, January–March 2020: Retrospective cohort study. BMJ 21(369), m1443. https://doi.org/10.1136/bmj.m1443 (2020).
La Scola, B. et al. Viral RNA load as determined by cell culture as a management tool for discharge of SARS-CoV-2 patients from infectious disease wards. Eur. J. Clin. Microbiol. Infect. Dis. 39(6), 1059–1061. https://doi.org/10.1007/s10096-020-03913-9 (2020).
Huang, Y. et al. SARS-CoV-2 viral load in clinical samples from critically ill patients. Am. J. Respir. Crit. Care Med. 201(11), 1435–1438. https://doi.org/10.1164/rccm.202003-0572LE (2020).
Yu, X. et al. SARS-CoV-2 viral load in sputum correlates with risk of COVID-19 progression. Crit. Care 24(1), 170. https://doi.org/10.1186/s13054-020-02893-8 (2020).
Gerilovych, A. P. et al. Coronavirus infections of animals and humans: Ideological use in media vs evidence-based scientific approach. Beacon J. Stud. Ideol. Ment. Dimens. 3(1), 020130318 (2020).
Widders, A., Broom, A. & Broom, J. SARS-CoV-2: The viral shedding vs infectivity dilemma. Infect. Dis. Health 25(3), 210–215. https://doi.org/10.1016/j.idh.2020.05.002 (2020).
Lai, C. C. et al. Asymptomatic carrier state, acute respiratory disease, and pneumonia due to severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2): Facts and myths. J. Microbiol. Immunol. Infect. 53(3), 404–412. https://doi.org/10.1016/j.jmii.2020.02.012 (2020).
Lai, C. C., Wang, C. Y. & Hsueh, P. R. Co-infections among patients with COVID-19: The need for combination therapy with non-anti-SARS-CoV-2 agents?. J. Microbiol. Immunol. Infect. 53(4), 505–512. https://doi.org/10.1016/j.jmii.2020.05.013 (2020).
Sassin, W. Deja Vue?. Beacon J. Stud. Ideol. Ment. Dimens. 2(2), 020210216 (2019).
Raoult, D., Hsueh, P. R., Stefani, S. & Rolain, J. M. COVID-19 therapeutic and prevention. Int. J. Antimicrob. Agents 55(4), 105937. https://doi.org/10.1016/j.ijantimicag.2020.105937 (2020).
Sassin, W. Die Grenzen der Ökonomie: Globalisierung - Vom Füllhorn zum Giftbecher?. Eur. Crossrd. 1(1), 010410216 (2020).
Sassin, W. Globalisierung und Digitalisierung - Die exponentielle Ausbreitung ansteckender Information und deren mögliche Eindämmung. Beacon J. Stud. Ideol. Ment. Dimens. 3(1), 010510201 (2020).
Weiskopf, D. et al. Phenotype and kinetics of SARS-CoV-2-specific T cells in COVID-19 patients with acute respiratory distress syndrome. Sci. Immunol. 5(48), eabd2071. https://doi.org/10.1126/sciimmunol.abd2071 (2020).
Walsh, K. A. et al. SARS-CoV-2 detection, viral load and infectivity over the course of an infection. J. Infect. 81(3), 357–371. https://doi.org/10.1016/j.jinf.2020.06.067 (2020).
Chen, X. et al. Detectable serum severe acute respiratory syndrome coronavirus 2 viral load (RNAemia) is closely correlated with drastically elevated interleukin 6 level in critically ill patients with coronavirus disease 2019. Clin. Infect. Dis. 71(8), 1937–1942. https://doi.org/10.1093/cid/ciaa449 (2020).
Andreakos, E. & Tsiodras, S. COVID-19: Lambda interferon against viral load and hyperinflammation. EMBO Mol. Med. 12(6), e12465. https://doi.org/10.15252/emmm.202012465 (2020).
Gao, Y. D. et al. Risk factors for severe and critically ill COVID-19 patients: A review. Allergy 76(2), 428–455. https://doi.org/10.1111/all.14657 (2021).
Mathers, A. J. The practical challenges of making clinical use of the quantitative value for SARS-CoV-2 viral load across several dynamics. Clin. Infect. Dis. 10, ciaa958. https://doi.org/10.1093/cid/ciaa958 (2020).
Kam, K. Q. et al. SARS-CoV-2 viral RNA load dynamics in the nasopharynx of infected children. Epidemiol. Infect. 149, e18. https://doi.org/10.1017/S095026882100008X (2021).
Song, K. H. et al. Dynamics of viral load and anti-SARS-CoV-2 antibodies in patients with positive RT-PCR results after recovery from COVID-19. Korean J. Intern. Med. 36(1), 11–14. https://doi.org/10.3904/kjim.2020.325 (2021).
Xu, T. et al. Clinical features and dynamics of viral load in imported and non-imported patients with COVID-19. Int. J. Infect. Dis. 94, 68–71. https://doi.org/10.1016/j.ijid.2020.03.022 (2020).
Tirupathi, R. et al. Viral dynamics in the Upper Respiratory Tract (URT) of SARS-CoV-2. Infez. Med. 28(4), 486–499 (2020).
Zhou, R. et al. Viral dynamics in asymptomatic patients with COVID-19. Int. J. Infect. Dis. 96, 288–290. https://doi.org/10.1016/j.ijid.2020.05.030 (2020).
Sharov, K. S. HIV/SARS-CoV-2 co-infection: T cell profile, cytokine dynamics and role of exhausted lymphocytes. Int. J. Infect. Dis. 102, 163–169. https://doi.org/10.1016/j.ijid.2020.10.049 (2021).
Malagón-Rojas, J. et al. SARS-CoV-2 and RT-PCR in asymptomatic patients: Results of a cohort of workers at El Dorado International Airport in Bogota, 2020. Biomedica 40(Suppl. 2), 166–172. https://doi.org/10.7705/biomedica.5802 (2020).
Haaksma, M. E. et al. Lung ultrasound findings in patients with novel SARS-CoV-2. ERJ Open Res. 6(4), 00238–02020. https://doi.org/10.1183/23120541.00238-2020 (2020).
Wazny, V., Siau, A., Wu, K. X. & Cheung, C. Vascular underpinning of COVID-19. Open Biol. 10(8), 200208. https://doi.org/10.1098/rsob.200208 (2020).
Salvamani, S. et al. Understanding the dynamics of COVID-19; implications for therapeutic intervention, vaccine development and movement control. Br. J. Biomed. Sci. 77(4), 168–184. https://doi.org/10.1080/09674845.2020.1826136 (2020).
Calza, L. et al. COVID-19 in patients with HIV-1 infection: A single-centre experience in northern Italy. Infection 49, 333–337. https://doi.org/10.1007/s15010-020-01492-7 (2020).
De la Calle, C. et al. Impact of viral load at admission on the development of respiratory failure in hospitalized patients with SARS-CoV-2 infection. Eur. J. Clin. Microbiol. Infect. Dis. https://doi.org/10.1007/s10096-020-04150-w (2021).
Chugh, H. et al. A comprehensive review on potential therapeutics interventions for COVID-19. Eur. J. Pharmacol. 5(890), 173741. https://doi.org/10.1016/j.ejphar.2020.173741 (2021).
Xu, D. et al. Relationship between serum SARS-CoV-2 nucleic acid(RNAemia) and organ damage in COVID-19 Patients: A Cohort Study. Clin. Infect. Dis. https://doi.org/10.1093/cid/ciaa1085 (2020).
Sassin, W. Ursprung und Grenzen von Gemeinschaft: Eine eurasische Perspektive. Eur. Crossrd. 2(1), 010210217 (2021).
Yoon, J. G. et al. Clinical significance of a high SARS-CoV-2 viral load in the Saliva. J. Korean Med. Sci. 35(20), e195. https://doi.org/10.3346/jkms.2020.35.e195 (2020).
Rich, R. R. et al. Clinical Immunology (Elsevier, 2019).
Yarilin, A. A. Immunology (GEOTAR Media, 2010).
Wang, L. et al. Hong Kong influenzas: Ideological implications. Beacon J. Stud. Ideol. Ment. Dimens. 1(2), 020510415 (2018).
Russell, E., Yang, A., Tardrew, S. & Ison, M. G. Parainfluenza virus in hospitalized adults: A 7-year retrospective study. Clin. Infect. Dis. 68(2), 298–305. https://doi.org/10.1093/cid/ciy451 (2019).
Russell, C. D., Unger, S. A., Walton, M. & Schwarze, J. The human immune response to respiratory syncytial virus infection. Clin. Microbiol. Rev. 30(2), 481–502. https://doi.org/10.1128/CMR.00090-16 (2017).
Sharov, K. S. Adaptation of a Russian population to SARS-CoV-2: Asymptomatic course, comorbidities, mortality, and other respiratory viruses—A reply to Fear versus Data. Int. J. Antimicrob. Agents 56, 106093. https://doi.org/10.1016/j.ijantimicag.2020.106093 (2020).
Sharov, K. S. SARS-CoV-2-related pneumonia cases in pneumonia picture in Russia in March-May 2020: Secondary bacterial pneumonia and viral co-infections. J. Glob. Health 10(2), 020504. https://doi.org/10.7189/jogh.10.020504 (2020).
Le Hingrat, Q. et al. Viral epidemiology and SARS-CoV-2 co-infections with other respiratory viruses during the first COVID-19 wave in Paris, France. . Influenza Other Respir. Viruses https://doi.org/10.1111/irv.12853 (2021).
Lalueza, A. et al. Severe lymphopenia in hospitalized patients with influenza virus infection as a marker of a poor outcome. Infect. Dis. (Lond) 51(7), 543–546. https://doi.org/10.1080/23744235.2019.1598572 (2019).
Acknowledgements
We would like to thank Nikolay Belousov, Polina Chernova, Maria Dolgova, Leonid Gerasimov, Anna Gorenintseva, Elizaveta Ilyina, Pavel Ivanov, Tatiana Kartseva, Ekaterina Koshkina, Mikhail Marushkevich, Sofia Petrova, Alexandra Sheveleva, Alexander Sokolov, Anastasia Sonina, Alexei Volodin, Vadim Zhuravlyov (Russia) for their technical and informational support in working with samplings and data sets, for providing the clinical data vital for the analysis.
Funding
This work has been funded by Government programme of basic research in Koltzov Institute of Developmental Biology, Russian Academy of Sciences, in 2021, No. 0088-2021-0008.
Author information
Authors and Affiliations
Contributions
K.S.S. is the sole author.
Corresponding author
Ethics declarations
Competing interests
The author declares no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sharov, K.S. 8806 Russian patients demonstrate T cell count as better marker of COVID-19 clinical course severity than SARS-CoV-2 viral load. Sci Rep 11, 9440 (2021). https://doi.org/10.1038/s41598-021-88714-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-88714-6
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.