Abstract
This study examines if overweight/obesity are related to higher impulsivity, food addiction and depressive symptoms, and if these variables could be modified after 1 year of a multimodal intervention (diet, physical activity, psychosocial support). 342 adults (55–75 years) with overweight/obesity and metabolic syndrome (MetS) from the PREDIMED-Plus Cognition study were randomized to the intervention or to the control group (lifestyle recommendations). Cognitive and psychopathological assessments were performed at baseline and after 1-year follow-up. At baseline, higher impulsivity was linked to higher food addiction and depressive symptoms, but not to body mass index (BMI). Food addiction not only predicted higher BMI and depressive symptoms, but also achieved a mediational role between impulsivity and BMI/depressive symptoms. After 1 year, patients in both groups reported significant decreases in BMI, food addiction and impulsivity. BMI reduction and impulsivity improvements were higher in the intervention group. Higher BMI decrease was achieved in individuals with lower impulsivity. Higher scores in food addiction were also related to greater post-treatment impulsivity. To conclude, overweight/obesity are related to higher impulsivity, food addiction and depressive symptoms in mid/old age individuals with MetS. Our results also highlight the modifiable nature of the studied variables and the interest of promoting multimodal interventions within this population.
Similar content being viewed by others
Introduction
Overweight and obesity are among the greatest health challenges of this century. They significantly increase the risk of death and chronic diseases such as metabolic syndrome (MetS), which is a cluster of cardiovascular risk factors that includes abdominal obesity, insulin resistance/diabetes, hypertension, and atherogenic dyslipidemia1. This subject is of big concern for the population aged 60 or over, as in this age range the prevalence of obesity is as high as 84%2. Overweight/obesity have been associated with different psychological factors, such as impulsivity3, food addiction4,5 and psychological wellbeing6.
Impulsivity is a pattern of undercontrolled behaviour or a tendency to act out in response to impulses7 and it can be conceptualized along three different domains8,9,10: impulsive personality traits, deficits in inhibitory control and impulsive choice or decision-making. Higher body mass index (BMI) and obesity have been linked to poorer inhibitory control11,12, impaired decision-making13,14,15,16,17 and certain impulsive traits5,18. In the older age population, there is still little evidence on the association between impulsivity and body weight. The few current studies in inhibitory control have shown unconclusive results, with some pointing to reduced inhibitory control in older adults with higher BMI19,20,21, but others indicating normal parameters in this population22. Regarding impulsive choice, there is even less evidence23, with only a recent study showing that increased reward sensitivity may characterize higher BMI throughout aging22.
Food addiction (FA) is a developing construct, which refers to an overconsumption of highly palatable food sustained by addictive processes24. It is highly prevalent (25–30%) in individuals with overweight/obesity25 and it is associated with high levels of impulsivity3,26,27,28. Besides, FA has been described as a mediator of the association between impulsivity and obesity5 and postulated to share similar neural mechanisms with other addictions (e.g.: greater activation of striatal regions to food/drug cues)29,30,31. Nevertheless, there is still a lack of studies examining these associations in elderly population with MetS.
Psychological health appears to worsen with the increasing severity of obesity32,33 and individuals with overweight/obesity carry a high prevalence of different psychological comorbidities (e.g.: mood and anxiety disorders)34,35,36,37. Some studies highlight the link between obesity and depression in adulthood, placing depression as a risk factor for developing obesity38,39 especially among females40. Besides, this population often suffers from prejudice and feelings of dislike about their bodies and appearance, which commonly lead to greater levels of depressive symptoms41. For this reason, some researchers uphold that the link between these two factors is bidirectional38 yet this is not conclusive and some contrary findings have also been reported42.
Finally, different studies have explored how changes in lifestyle, such as increased physical activity and healthier eating habits, may reduce body weight and the risk of cardiovascular diseases, type 2 diabetes and MetS43,44,45,46,47,48,49,50. In fact, these positive effects can be observed not only on BMI but also on impulsivity, FA and psychological health51,52,53,54,55,56,57,58. Nevertheless, longitudinal studies that consider all previously mentioned variables while controlling for relevant confounders are needed to increase the validity of current knowledge.
The first aim of this study was to examine if overweight and obesity in mid-old age individuals with MetS are related to higher impulsivity, food addiction and depressive symptoms. We hypothesized that impulsivity features would predict higher BMI, FA and depressive symptoms. The second aim was to longitudinally explore through a randomized clinical trial if these variables could be modified after 1 year of a multimodal psychosocial intervention (based on an energy-restricted diet, physical activity promotion and behavioural-motivational support). By doing so, we aim to not only better describe the psychological factors related to overweight/obesity but also to test the effectivity of the treatment when dealing with them. We hypothesize that the multimodal intervention, compared to the control intervention, would higher reduce BMI, FA, depressive symptoms as well as impulsivity. Our last hypothesis is that the severity of impulsivity and FA at baseline would predict the extent of BMI pre-post change.
Methods
Design
This is a cross-sectional and longitudinal data analysis from baseline and 1-year follow-up within the frame of the PREDIMED-Plus study (Cognition Subprogram), a multicentre, randomized, parallel-group, primary prevention clinical trial conducted in Spain to assess the effect of an intensive weight loss intervention program based on an energy-restricted traditional Mediterranean diet, physical activity promotion and behavioural support59,60. The design and methods have been published59,60 and the study protocol is available at http://www.predimedplus.com/. This study was registered at the International Standard Randomized Controlled Trial (ISRCT; http://www.isrctn.com/ISRCTN89898870, Date applied 28/05/2014, Date assigned 24/07/2014). Cognitive function, quality of life, and psychological and neuropsychological scores are secondary outcomes of the study.
Participants
The study was comprised of 489 participants who were randomly assigned to control group (n = 247) or intervention group (n = 242). 147 participants were excluded from analysis given that their assessments had no complete data in relation to the outcome variables studied. Final analyses were conducted with 342 participants (167 females). Control and intervention group consisted of 179 and 163 participants respectively (see the Supplementary Figure S1 for the Consort flow diagram). Participants were recruited September 2014 to October 2016 from Primary Health Care facilities belonging to the National Health System associated to four centres from different universities, teaching hospitals and research institutes in Spain participating in the PREDIMED-Plus cognition subprogram: Universitat Rovira i Virgili (Tarragona), Universidad de Valencia (Valencia), Institut Hospital del Mar d’Investigacions Mèdiques-IMIM (Barcelona), and Bellvitge University Hospital-IDIBELL (Barcelona). The eligible participants were community-dwelling adults (aged between 55 and 75 years in case of men; and between 60 and 75 years in women), free of cardiovascular disease (CVD) at enrolment, with a BMI of 27–40 kg/m2, and harbouring the MetS61. Further details of the inclusion and exclusion criteria can be found elsewhere59,60. Participants included in the current analysis were part of the PREDIMED-Plus and were explored with an extended cognitive protocol. Data collected assessed cognitive domains related with impulsivity and food addiction. Depressive symptoms, as well as detailed specification of BMI, physical conditions and sociodemographic data were collected in the frame of the PREDIMED-Plus study. All participants provided written informed consent, and the study protocol and procedures were approved according to the ethical standards of the Declaration of Helsinki by the Research Ethics Committees from all the participating institutions: CEIC Hospital Universitari Sant Joan de Reus (13-7-25/7proj2), CEIm-PSMAR (2019/8612/I), CEIC Hospital Universitari de Bellvitge (PR240/13), Institutional Review Board of Valencia University (H1373255532771).
Measures
All participants were assessed at baseline and reassessed at 1-year follow-up. During these two assessments, the participants completed several self-reported questionnaires and a set of neuropsychological tests for evaluating impulsivity domains and decision making (namely Stroop Colour and Word Test—SCWT, Conner’s Continuous Performance Test—CPT and Iowa Gambling Task—IGT) and psychopathological factors (namely depression symptomatology and food addiction). At each visit, sociodemographic-clinical information, including age, weight, height, and other relevant indexes were also collected by means of a self-reported questionnaire and a hetero-administered clinical interview assessing medical conditions.
Clinical and psychometrical assessment:
The Beck Depression Inventory–II62 is a 21-item self-report measure for assessing the severity of depressive symptoms in adults and adolescents (ages from 13 to 80 years). The BDI-II reflects the diagnostic criteria for Major Depressive Disorder listed in the DSM-563. Scores for each item range from 0 to 3; the total score is the sum of all responses. The Cronbach’s alpha in our sample shows a good internal consistency (α = 0.874).
The Yale Food Addiction Scale version 2.064,65 is a 35 item self-report questionnaire scored on an eight-level Likert scale (from 0 = never to 7 = every day) to measure addictive food behaviours based on DSM-5 substance-related and addictive disorders criteria63. The YFAS 2.0 has been validated in a Spanish-speaking population, presenting excellent accuracy in discriminating between healthy control and eating-disorder subsamples (α = 0.75) and excellent internal reliability coefficient (α = 0.94). Two scores can be derived from the YAFS: (a) a continuous symptom count score that reflects the number of fulfilled diagnostic criteria (ranging from 0 to 11) and (b) a diagnosis of food addiction based on the number of symptoms and clinically significant impairment or distress. The Cronbach’s α value for the present study was 0.883.
The UPPS-P Impulsivity Scale66 is a 59-item questionnaire to assess five different features of impulsive behaviour: negative urgency, lack of perseverance, lack of premeditation, sensation seeking and positive urgency. The UPPS-P has satisfactory psychometric properties in terms of both convergent and discriminatory validity67,68. The Spanish adaptation of the scale has adequate psychometric properties69. The α values for the different UPPS-P scales in our sample are as follows: lack of premeditation (0.818), lack of perseverance (0.759), sensation seeking (0.846), positive urgency (0.897) and negative urgency (0.812).
Neuropsychological assessment
The Stroop Colour and Word Test70,71 is a widely employed task which assesses inhibitory control, that is, the cognitive ability to control dominant behavioural responses to stimuli. It involves three different lists: a word list with names of colours printed in black ink, a colour list including letter Xs printed in colour, and a colour-word list composed of names of colours in a colour ink that does not match the written name. Three final scores are obtained calculating the number of items read in 45 s. An interference score is also computed based on the three aforementioned lists, this score enables the assessment of individual’s cognitive flexibility and the ability to inhibit cognitive interference. Higher scores in this index mean better inhibitory control.
The Conner’s Continuous Performance Test, second edition72 is a computerized task in which participants have to press the space bar in response to visual stimuli (i.e., letters on the computer screen). This task has a duration of 14 min. The CPT-II provides information about the participants' errors (i.e. omissions and commissions), reaction time and response variability. All these measures are used to assess sustained attention and inhibitory control. Higher scores on the CPT-II indicate worse performance. High levels of impulsivity involve a fast Hit Reaction time (HRT) together with a high rate of Commissions72.
The Iowa Gambling Task73,74 is a computer-based task which enables to assess decision-making, which is proposed to be a measure of choice of impulsivity75. It comprises a total of 100 trials in which the participant has to select among four decks of cards (A, B, C, and D), a specified amount of play money is awarded afterward. The interspersed rewards amongst these decks are probabilistic punishments (monetary losses). The final aim of the task is to win as much money as possible trying to lose as less money as possible. In addition, they might choose cards from any deck, and switch decks at any time. The final score is obtained by subtracting the number of cards selected from decks A and B from the number of cards selected from decks C and D. These two last decks are advantageous as the punishments are smaller, while decks A and B are disadvantageous since the final loss is higher than the final gain. Higher scores implicate better performance on the task.
Anthropometric and biochemical measurements
Calibrated weighting scales were used to measure weight, while a wall-mounted stadiometer provided information about participants’ height. BMI was calculated though the following equation: BMI = kilograms/meters2.
Clinical interventions
Participants randomized to the control group received usual lifestyle recommendations for the management of the MetS. They were recommended to follow a Mediterranean diet based on materials and results developed in the framework of the PREDIMED study59,60. The participants of the control group were offered sessions every 6 months, which consisted of an individual visit, a telephone call and a group session, all of them led by the team of dieticians of the PREDIMED-Plus study. No specific motivational advice for increasing physical activity or losing weight was provided.
Participants randomized to the intervention group (intensive lifestyle with a psychosocial approach) received an energy restricted traditional Mediterranean diet. Dietary intervention was associated with physical activity promotion and psychosocial (behavioural-motivational) support, with specific goals of weight loss, including self-monitoring and frequent monitoring throughout the study. These subjects participated in individual interviews (15–30 min) and motivational group sessions (30–45 min; maximum 20 participants) three times per month during the first year of the intervention. The level of compliance with the intervention was periodically monitored in order to adapt it if deemed necessary.Participants in both groups were provided with an allotment of extra-virgin olive oil (1 L/mo) and raw nuts (125 g/mo) for free. However, we recommended that all participants consume a total of 500 g/mo of mixed nuts.
Further information on the intervention procedures and goals were previously described elsewhere59,76.
Statistical analysis
Statistical analysis was carried out with SPSS24 and Stata16 for Windows using the available database January 15th, 2019 PREDIMED-Plus Cognition subprogram database. Comparisons on the descriptive variables of the two intervention groups were implemented via chi-square (categorical variables) and t test tests (quantitative variables). Multiple regression analysis was used to test if the impulsivity measures predicted FA (YFAS-total score), BMI (kg/m2) and depressive symptoms (BDI total score) at baseline. These models were obtained in two blocks (each block representing one step): a) the first block entered and fixed the covariates sex, age, and education; and b) the second block used a stepwise procedure to automatically select the impulsivity measures which were significantly predicting each outcome. The incremental predictive capacity of impulsivity was estimated with the R2 change/increase.
Pre-post changes were tested with a mixed analysis of variance (ANOVA), defining time (pre-post) as the intra-subjects’ factor and intervention group (control-intervention) as the between-subjects factor. These analyses were adjusted by sex, age and education.
Multiple regression analysis was used to test the incremental predictive capacity of FA and impulsivity at baseline as well as group of treatment (control-intervention) on pre-post changes in BMI (kg/m2). These models were obtained in four blocks (each block representing one step): a) the first block entered and fixed the covariates sex, age, education, and BMI at baseline; b) the second block entered and fixed the covariate FA; and c) the third block used a stepwise procedure for automatically selecting the best predictors (from the set of impulsivity measures—UPPS-P, STROOP word/colours and interference, CPT commissions-omissions—hit reaction time) of the outcome; and d) the fourth block entered and fixed the treatment group. Incremental predictive capacity of each block was estimated with the increase/change in the R2 coefficient.
Path analysis (a special case of structural equation modelling: SEM) was implemented to analyse the underlying mechanisms explaining the mediational links (direct and indirect effects) among the variables of the study77. In this study, the maximum-likelihood estimation (MLE) method of parameter estimation was used and a latent variable was defined for the impulsivity trait considering the scores in the UPPS-P scales. Goodness-of-fit was considered for78: measuring root mean square error of approximation RMSEA < 0.08, Bentler’s Comparative Fit Index CFI > 0.90, Tucker-Lewis Index TLI > 0.90, and standardized root mean square residual SRMR < 0.10.
In this study, the increase of Type-I error due to multiple comparisons was controlled with the Finner-method (a familywise error rate stepwise procedure which has demonstrated higher power than the classical Bonferroni-method79).
Results
Characteristics of the participants
No statistical differences were found in sociodemographic data when compared participants included and those excluded due to missing values in the outcome variables (age: F = 0.52, df = 1/487, p = 0.472; sex: χ2 = 1.29, df = 1, p = 0.257; origin European vs other: χ2 = 1.19, df = 1, p = 0.275; civil status: χ2 = 0.34, df = 1, p = 0.559; education level: χ2 = 7.55, df = 4, p = 0.109; and employment status: χ2 = 0.72, df = 1, p = 0.395), BMI at baseline (F = 0.02, df = 1/487, p = 0.880) and psychometrical measures at baseline (UPPS-premeditation: F = 1.14, df = 1/487, p = 0.287; UPPS-perseverance: F = 0.55, df = 1/487, p = 0.458; UPPS-sensation seeking: F = 1.66, df = 1/487, p = 0.199; UPPS-positive urgency: F = 0.91, df = 1/487, p = 0.341; UPPS-negative urgency; F = 2.50, df = 1/487, p = 0.115; YFAS-total: F = 2.53, df = 1/487, p = 0.112; BDI-total: F = 1.31, df = 1/487, p = 0.254).
Table 1 includes the distribution of the sociodemographic features and the BMI at the baseline for the participants in this study. No baseline significant differences were observed between the two groups on age, education or BMI. Similarly, no statistical differences were found for the final sample of the two treatment arms on the sociodemographic or main general variables of the study (see Figure S1 for excluded participants due to missing data) (sex: χ2 = 1.29, p = 0.257; origin: χ2 = 1.19, p = 0.275; civil status: χ2 = 0.34, p = 0.559; school level: χ2 = 7.55, p = 0.109; employment status: χ2 = 0.72, p = 0.395; age: F = 0.52, p = 0.472; and BMI: F = 0.02, p = 0.880).
Cross-sectional analysis
Table 2 contains the three multiple regressions estimating the predictive capacity of the impulsivity measures on FA scores (YFAS total), BMI and depressive symptoms (BDI total) at baseline. After adjusting by the participants’ sex, age and education, higher FA and depressive symptoms were observed on individuals with higher scores in the UPPS-P lack of perseverance and negative urgency impulsivity components. No significant predictors of BMI were found for the set of impulsivity measures. For these analyses, participants from both intervention and control groups were pooled.
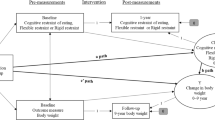
Figure 1 includes the path-diagram with the standardized coefficients obtained in the SEM with the measures at baseline (adequate fitting was achieved). The latent variable measuring trait impulsivity was significantly and positively defined by the set of the UPPS-P (the highest coefficient-weight was achieved for the negative urgency scale and the lowest for the sensation seeking). FA severity was positively associated with impulsivity. Higher BMI was only predicted by higher FA scores, whereas higher depressive symptoms were predicted by both higher FA scores and higher impulsivity. FA achieved a mediational role between the impulsivity levels and the BMI and BDI scores. Women significantly displayed increased impulsivity and the BDI scores, but there were no significant predictors of the YFAS or the BMI.
Longitudinal analysis after 1 year of intervention
Table 3 contains pre-post changes in each treatment group for the variables of the study (i.e.: impulsivity measures, FA and BMI) adjusted by sex, age and education. Patients from both groups presented a significant decrease in BMI and FA scores; although the decrease in BMI was significantly higher for the patients in the intervention group.
Regarding trait impulsivity, significant interaction parameters were found for the UPPS-P positive and negative urgency traits, indicating that changes in pre-post measures were different depending on the group of treatment (control-intervention). More specifically, patients of the intervention group presented significantly lower positive and negative urgency at post treatment than patients in the control group and, patients in the intervention group presented a significant decrease on negative urgency (pre-post) whereas the patients in the control group did not. Finally, patients in the control group presented higher scores in lack of perseverance both in the pre and post treatment.
Additionally, a tendency to decrease inhibitory control was observed through the STROOP and CPT in both groups but the intervention group reached a significant improved performance on the pre-post STROOP words/colours whereas the control group on the CPT commissions. No significant changes were found concerning trait impulsivity or choice impulsivity (decision making).
Table 4 comprises the final multiple regression results depicting the incremental capacity of FA and impulsivity measures as well as treatment group on BMI pre-post change. These results show that after adjusting by the participants’ sex, age, education and BMI at baseline, a higher decrease in the BMI was achieved for individuals with a lower score in the UPPS-P negative urgency and for those included into the intervention group.
Figure 2 displays the SEM path-diagram with the standardized coefficients (adjusted by the education level) of the variables measured during the follow-up (goodness-of-fit was achieved). The results of this model are similar to those obtained in the SEM for the cross-sectional analysis. Regarding the post-treatment results, FA scores were higher for participants who reported higher scores in the latent variable defined as trait impulsivity (UPPS-P).
Additionally, participants in the intervention group reported lower levels of trait impulsivity and lower BMI. Post treatment FA scores mediated the association between trait impulsivity and the BMI, that is, higher trait impulsivity is related to higher FA, and higher FA increases the BMI. The treatment group also achieved indirect effects on the FA and the BMI through the impulsivity trait: being in the intervention group decreases the impulsivity levels and lower impulsivity levels related to both lower FA and lower BMI.
Discussion
This study examined if overweight and obesity in mid/old age individuals with MetS were related to specific impulsivity domains, food addiction and depressive symptoms, and if these factors can be modified by 1 year of a multimodal lifestyle intervention. Results showed the mediating role of FA between trait impulsivity and BMI or depressive symptoms at baseline and revealed that, after 1 year of treatment, BMI and some impulsivity features can be further decreased in the patients of the intervention group.
At a cross-sectional level, our results showed higher negative urgency and lack of perseverance values in individuals with higher FA and higher depressive symptoms, but no direct associations were found between impulsivity and higher BMI. Still, SEM analysis revealed that FA not only predicted higher BMI and depressive symptoms, but also achieved a mediational role between impulsivity levels and the BMI and depressive symptoms. Interestingly, negative urgency (the propensity to act rashly when facing negative emotion) has long been described as one of the main impulsivity traits linked to the development and maintenance of FA3,26,80 and other addictions, such as substance abuse, gambling disorder and compulsive buying81,82,83,84. Likewise, lack of perseverance (the inability to remain focused on a task) has been linked to higher disorder severity and poorer treatment response of addictive behaviours such as gambling or Internet addiction85,86. In the current sample of the study, these two impulsivity traits seem to be linked to obesity/overweight through the presence of FA. Recent studies have pointed out that FA may partly explain obesity87. However, it would not be the only responsible factor of obesity, which would be the result of different metabolic, behavioural or psychological factors42,88,89. Therefore, in our sample, only the individuals presenting higher scores in FA would also present impulsive traits long associated with addictive patterns. Finally, depressive symptoms were found to be greater for individuals with higher FA, impulsivity and BMI which suggest that the mood state of the individuals could be affected by the struggles deriving from these variables. This has previously been reported in different samples where obesity, high impulsivity and FA can hamper the individuals’ daily life and be related to a perceived worse quality of life and lower mood state6,90.
At a longitudinal level, after 1 year of treatment (either in the intervention group or the control group), patients reported a significant decrease in BMI and FA, together with a significant tendency to decrease different impulsivity features (i.e. trait impulsivity and inhibitory control). However, the decrease of BMI and the improvement of some impulsivity features (negative urgency and inhibitory control) were higher for the patients in the intervention group. As previously stated, it has to be noted that negative urgency is an impulsivity trait highly linked to addictive behaviours, such as FA27. Thus, the changes found within these variables reinforce the usefulness of an intensive multimodal psychosocial intervention (promoting a healthy dietary pattern such as the Mediterranean diet, physical activity and behavioural-motivational support) not only on reducing obesity as a risk factor for MetS and cardiovascular diseases48,91, but also on decreasing impulsivity and FA (source of distress and highly linked to obesity3,43). As previously stated, its success is higher than the one observed in the control group and seems to be largely associated with aspects of the individual's impulsivity that we can modulate through group support sessions. With this in mind, it strikes as interesting for future studies to explore the role of treatment compliance within the studied variables. For instance, to explore if a lower impulsivity is related to a better compliance and thus to better treatment outcomes.
Results also stressed that, despite the treatment arm, the higher decrease in the BMI was achieved for individuals with lower negative urgency and better inhibitory control. We hypothesise that those individuals presenting stronger psychological features related not only to FA but also to addictions in general (such as negative urgency) present a greater resistance to reduce BMI and could better benefit from a more psychologically driven intervention. In fact, previous studies have highlighted that this trait may hamper attempts to treat patients with different addictive behaviours92,93. Consequently, in line with this hypothesis, the SEM analysis showed that after 1 year of treatment and despite the improvement of the patients (measured by a lower BMI and FA scores), the associations between trait impulsivity and FA/BMI were still present.
The current study should be considered under some limitations. Firstly, given that our study participants are senior adults with MetS, the present findings cannot be extrapolated to other population groups. However, it is one of the strengths of this study that it is conducted with a large sample of mid/old age men and women with overweight or obesity and at high cardiovascular risk. Future studies should further explore the associations reported regarding the presence of FA, impulsivity and BMI in different populations of advanced age. Also, some of the measures are self-reported thus subject to recall biases and to complement issues. For instance, 147 participants had to be excluded due to missing data (e.g.: items not answered within one questionnaire) and the sample was reduced.
To conclude, overweight and obesity in mid/old age individuals with MetS are related to higher impulsivity, food addiction and depressive symptoms. Our results provide evidence towards the role of FA on BMI and depressive symptoms as well as its link with trait impulsivity. Finally, an intensive multimodal intervention is better than the treatment following the usual recommendations and the success is largely associated with aspects of the individual's impulsivity that we can modulate through group support sessions within the intervention. The results also highlight the modifiable nature of FA and BMI partially through improving impulsivity features and, second the need of promoting interventions within this population.
References
Cornier, M.-A. et al. The metabolic syndrome. Endocr. Rev. 29, 777–822 (2008).
Albers, U. et al. Prevalence of overweight and obesity in non-institutionalized people aged 65 or over from Spain: the elderly EXERNET multi-centre study. Obes. Rev. 12, 583–592 (2011).
VanderBroek-Stice, L., Stojek, M. K., Beach, S. R. H., vanDellen, M. R. & MacKillop, J. Multidimensional assessment of impulsivity in relation to obesity and food addiction. Appetite 112, 59–68 (2017).
Steward, T. et al. Food addiction and impaired executive functions in women with obesity. Eur. Eat. Disord. Rev. https://doi.org/10.1002/erv.2636 (2018).
Murphy, C. M., Stojek, M. K. & MacKillop, J. Interrelationships among impulsive personality traits, food addiction, and body mass index. Appetite 73, 45–50 (2014).
Romain, A. J., Marleau, J. & Baillot, A. Impact of obesity and mood disorders on physical comorbidities, psychological well-being, health behaviours and use of health services. J. Affect. Disord. 225, 381–388 (2018).
Evenden, J. L. Varieties of impulsivity. Psychopharmacology 146, 348–361 (1999).
MacKillop, J. et al. The latent structure of impulsivity: impulsive choice, impulsive action, and impulsive personality traits. Psychopharmacology 233, 3361–3370 (2016).
Meda, S. A. et al. Investigating the behavioral and self-report constructs of impulsivity domains using principal component analysis. Behav. Pharmacol. 20, 390–399 (2009).
Bari, A. & Robbins, T. W. Inhibition and impulsivity: Behavioral and neural basis of response control. Prog. Neurobiol. 108, 44–79 (2013).
Stinson, E. J., Krakoff, J. & Gluck, M. E. Depressive symptoms and poorer performance on the Stroop Task are associated with weight gain. Physiol. Behav. 186, 25–30 (2018).
Mole, T. B. et al. Impulsivity in disorders of food and drug misuse. Psychol. Med. 45, 771–782 (2015).
Pignatti, R. et al. Decision-making in obesity: a study using the Gambling Task. Eat. Weight Disord. 11, 126–132 (2006).
Brogan, A., Hevey, D., O’Callaghan, G., Yoder, R. & O’Shea, D. Impaired decision making among morbidly obese adults. J. Psychosom. Res. 70, 189–196 (2011).
Mallorquí-Bagué, N. et al. Decision making impairment: a shared vulnerability in obesity, gambling disorder and substance use disorders?. PLoS ONE 11, e0163901 (2016).
Steward, T. et al. Delay discounting of reward and impulsivity in eating disorders: from anorexia nervosa to binge eating disorder. Eur. Eat. Disord. Rev. 25, 601–606 (2017).
Amlung, M., Petker, T., Jackson, J., Balodis, I. & MacKillop, J. Steep discounting of delayed monetary and food rewards in obesity: a meta-analysis. Psychol. Med. 46, 2423–2434 (2016).
Mobbs, O., Crépin, C., Thiéry, C., Golay, A. & Van der Linden, M. Obesity and the four facets of impulsivity. Patient Educ. Couns. 79, 372–377 (2010).
Waldstein, S. R. & Katzel, L. I. Interactive relations of central versus total obesity and blood pressure to cognitive function. Int. J. Obes. https://doi.org/10.1038/sj.ijo.0803114 (2006).
Walther, K., Birdsill, A. C., Glisky, E. L. & Ryan, L. Structural brain differences and cognitive functioning related to body mass index in older females. Hum. Brain Mapp. https://doi.org/10.1002/hbm.20916 (2010).
Gunstad, J., Paul, R. H., Cohen, R. A., Tate, D. F. & Gordon, E. Obesity is associated with memory deficits in young and middle-aged adults. Eat. Weight Disord. https://doi.org/10.1007/BF03327747 (2006).
Aiello, M. et al. Body weight and its association with impulsivity in middle and old age individuals. Brain Cogn. 123, 103–109 (2018).
van Meer, F., Charbonnier, L. & Smeets, P. A. M. Food decision-making: effects of weight status and age. Curr. DiabetesRep. https://doi.org/10.1007/s11892-016-0773-z (2016).
Gearhardt, A. N., Corbin, W. R. & Brownell, K. D. Preliminary validation of the Yale Food Addiction Scale. Appetite 52, 430–436 (2009).
Pursey, K., Stanwell, P., Gearhardt, A., Collins, C. & Burrows, T. The prevalence of food addiction as assessed by the Yale Food Addiction Scale: a systematic review. Obes. Res. Clin. Pract. 8, 80–81 (2014).
Wolz, I. et al. ‘Food Addiction’ in patients with eating disorders is associated with negative urgency and difficulties to focuson long-term goals. Front. Psychol. 7, 61 (2016).
Wolz, I., Granero, R. & Fernández-Aranda, F. A comprehensive model of food addiction in patients with binge-eating symptomatology: The essential role of negative urgency. Compr. Psychiatry 74, 118–124 (2017).
Rose, M. H., Nadler, E. P. & Mackey, E. R. Impulse control in negative mood states, emotional eating, and food addiction are associated with lower quality of life in adolescents with severe obesity. J. Pediatr. Psychol. 43, 443–451 (2018).
Stice, E., Yokum, S., Burger, K. S., Epstein, L. H. & Small, D. M. Youth at risk for obesity show greater activation of striatal and somatosensory regions to food. J. Neurosci. 31, 4360–4366 (2011).
Stice, E. & Yokum, S. Gain in body fat is associated with increased striatal response to palatable food cues, whereas body fat stability is associated with decreased striatal response. J. Neurosci. 36, 6949–6956 (2016).
Holsen, L. M. et al. Neural mechanisms underlying food motivation in children and adolescents. Neuroimage 27, 669–676 (2005).
Lin, K. P., Liang, T. L., Liao, I. C. & Tsay, S. L. Associations among depression, obesity, and metabolic syndrome in young adult females. Biol. Res. Nurs. 16, 327–334 (2014).
Marazziti, D., Rutigliano, G., Baroni, S., Landi, P. & Dell’Osso, L. Metabolic syndrome and major depression. CNS Spectr. 19, 293–304 (2014).
Friedman, M. A. & Brownell, K. D. Psychological correlates of obesity: moving to the next research generation. Psychol. Bull. 117, 3–20 (1995).
Gariepy, G., Nitka, D. & Schmitz, N. The association between obesity and anxiety disorders in the population: a systematic review and meta-analysis. Int. J. Obes. 34, 407–419 (2010).
Kubik, J. F., Gill, R. S., Laffin, M. & Karmali, S. The impact of bariatric surgery on psychological health. J. Obes. 2013, 837989 (2013).
Lykouras, L. Psychological profile of obese patients. Dig. Dis. 26, 36–39 (2008).
Luppino, F. S. et al. Overweight, obesity, and depression. Arch. Gen. Psychiatry 67, 220 (2010).
Blaine, B. Does depression cause obesity?. J. Health Psychol. 13, 1190–1197 (2008).
de Wit, L. et al. Depression and obesity: A meta-analysis of community-based studies. Psychiatry Res. 178, 230–235 (2010).
Kaminsky, J. & Gadaleta, D. A study of discrimination within the medical community as viewed by obese patients. Obes. Surg. 12, 14–18 (2002).
Atlantis, E. & Baker, M. Obesity effects on depression: systematic review of epidemiological studies. Int. J. Obes. 32, 881–891 (2008).
Lakka, T. A. & Laaksonen, D. E. Physical activity in prevention and treatment of the metabolic syndrome. Appl. Physiol. Nutr. Metab. 32, 76–88 (2007).
Li, T. Y. et al. Obesity as compared with physical activity in predicting risk of coronary heart disease in women. Circulation 113, 499–506 (2006).
Jeon, C. Y., Lokken, R. P., Hu, F. B. & Van Dam, R. M. Physical activity of moderate intensity and risk of type 2 diabetes: a systematic review. Diabetes Care 30, 744–752 (2007).
Hu, G. et al. Physical activity, body mass index, and risk of type 2 diabetes in patients with normal or impaired glucose regulation. Arch. Intern. Med. 164, 892–896 (2004).
Becker, W. et al. Nordic nutrition recommendations 2004—integrating nutrition and physical activity. Food Nutr. Res. 48, 178–187 (2004).
Barnard, N. D. et al. A low-fat vegan diet and a conventional diabetes diet in the treatment of type 2 diabetes: a randomized, controlled, 74-wk clinical trial. Am. J. Clin. Nutr. 89, 1588S-1596S (2009).
Webster, C. C., Murphy, T. E., Larmuth, K. M., Noakes, T. D. & Smith, J. A. Diet, diabetes status, and personal experiences of individuals with type 2 diabetes who self-selected and followed a low carbohydrate high fat diet. Diabetes Metab. Syndr. Obes. Targets Ther. 12, 2567–2582 (2019).
Abellán Alemán, J. et al. Adherence to the ‘Mediterranean Diet’ in Spain and its relationship with cardiovascular risk (DIMERICA Study). Nutrients 8, 680 (2016).
Kulendran, M. et al. Neuropsychological assessment as a predictor of weight loss in obese adolescents. Int. J. Obes. 38, 507–512 (2014).
Zang, Y. Impact of physical exercise on children with attention deficit hyperactivity disorders: evidence through a meta-analysis. Medicine (Baltimore) 98, e17980 (2019).
Del-Ponte, B., Quinte, G. C., Cruz, S., Grellert, M. & Santos, I. S. Dietary patterns and attention deficit/hyperactivity disorder (ADHD): a systematic review and meta-analysis. J. Affect. Disord. 252, 160–173 (2019).
Delgado-Rico, E. et al. Effects of a multicomponent behavioral intervention on impulsivity and cognitive deficits in adolescents with excess weight. Behav. Pharmacol. 23, 609–615 (2012).
Molendijk, M., Molero, P., Ortuño Sánchez-Pedreño, F., Van der Does, W. & Angel Martínez-González, M. Diet quality and depression risk: a systematic review and dose-response meta-analysis of prospective studies. J. Affect. Disord. 226, 346–354 (2018).
Daneshzad, E., Keshavarz, S., Qorbani, M., Larijani, B. & Azadbakht, L. The association between low carbohydrate diet, sleep status, depression, anxiety and stress score. J. Sci. Food Agric. https://doi.org/10.1002/jsfa.10322 (2020).
Carmen, M. et al. Treating binge eating and food addiction symptoms with low-carbohydrate Ketogenic diets: a case series. J. Eat. Disord. 8, 2 (2020).
Guzzardi, M. A. et al. Food addiction distinguishes an overweight phenotype that can be reversed by low calorie diet. Eur. Eat. Disord. Rev. 26, 657–670 (2018).
Martínez-González, M. A. et al. Cohort profile: design and methods of the PREDIMED-plus randomized trial. Int. J. Epidemiol. 48, 387–388o (2019).
Salas-Salvadó, J. et al. Effect of a lifestyle intervention program with energy-restricted Mediterranean diet and exercise on weight loss and cardiovascular risk factors: one-year results of the PREDIMED-Plus trial. Diabetes Care 42, 777–788 (2019).
Alberti, K. G. M. M. et al. Harmonizing the metabolic syndrome: a joint interim statement of the international diabetes federation task force on epidemiology and prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; And International Association for the Study of Obesity. Circulation 120, 1640–1645 (2009).
Beck, A., Brown, G. & Steer, R. Beck depression inventory-ii manual. J. Health Psychol. https://doi.org/10.1177/1359105311424470 (1996).
American Psychiatric Association. Diagnostic and statistical manual of mental disorders : DSM-5 (American Psychiatric Association, 2013).
Gearhardt, A. N., Corbin, W. R. & Brownell, K. D. Development of the Yale Food Addiction Scale version 2.0. Psychol. Addict. Behav. 30, 113–121 (2016).
Granero, R. et al. Validation of the Spanish version of the Yale Food Addiction Scale 2.0 (YFAS 2.0) and clinical correlates in a sample of eating disorder, gambling disorder, and healthy control participants. Front. Psychiatry 9, 208 (2018).
Whiteside, S. P., Lynam, D. R., Miller, J. D. & Reynolds, S. K. Validation of the UPPS impulsive behaviour scale: a four-factor model of impulsivity. Eur. J. Pers. 19, 559–574 (2005).
Cyders, M. A. & Smith, G. T. Emotion-based dispositions to rash action: Positive and negative urgency. Psychol. Bull. 134, 807–828 (2008).
Smith, E., Hay, P., Campbell, L. & Trollor, J. N. A review of the association between obesity and cognitive function across the lifespan: implications for novel approaches to prevention and treatment. Obes. Rev. 12, 740–755 (2011).
Verdejo-García, A., Lozano, Ó., Moya, M., Alcázar, M. Á. & Pérez-García, M. Psychometric properties of a Spanish version of the UPPS–P Impulsive Behavior Scale: reliability, validity and association with trait and cognitive impulsivity. J. Pers. Assess. 92, 70–77 (2010).
Golden, C. J. Stroop colour and word test. Age (Omaha). 15, 90 (1978).
Golden, C. J. Stroop: test de colores y palabras: manual (TEA ediciones, 2001).
Conners, C. Conners’ Continuous Performance Test (CPT II) Version 5 for Windows: Technical Guide and Software Manual (2004).
Bechara, A., Damasio, H., Tranel, D. & Damasio, A. R. Deciding advantageously before knowing the advantageous strategy. Science 275, 1293–1295 (1997).
Bechara, A., Tranel, D. & Damasio, H. Characterization of the decision-making deficit of patients with ventromedial prefrontal cortex lesions. Brain 123, 2189–2202 (2000).
Eisinger, A. et al. Iowa gambling task: illustration of a behavioral measurement. Neuropsychopharmacol. Hung. 18, 45–55 (2016).
Sayón-Orea, C. et al. Effect of a nutritional and behavioral intervention on energy-reduced mediterranean diet adherence among patients with metabolic syndrome: interim analysis of the PREDIMED-plus randomized clinical trial. JAMA - J. Am. Med. Assoc. 322, 1486–1499 (2019).
Kline, R. B. Principles and Practice of Structural Equation Modeling 2nd edn. (The Guilford Press, 2005).
Barrett, P. Structural equation modelling: adjudging model fit. Pers. Individ. Differ. 42, 815–824 (2007).
Finner, H. On a monotonicity problem in step-down multiple test procedures. J. Am. Stat. Assoc. 88, 920–923 (1993).
Pivarunas, B. & Conner, B. T. Impulsivity and emotion dysregulation as predictors of food addiction. Eat. Behav. 19, 9–14 (2015).
Zorrilla, E. P. & Koob, G. F. Impulsivity derived from the dark side: neurocircuits that contribute to negative urgency. Front. Behav. Neurosci. 13, 136 (2019).
Quintero, M. J., Navas, J. F. & Perales, J. C. The associative underpinnings of negative urgency and its role in problematic gambling behavior. Addict. Behav. https://doi.org/10.1016/j.addbeh.2020.106533 (2020).
Rose, P. & Segrist, D. J. Negative and positive urgency may both be risk factors for compulsive buying. J. Behav. Addict. 3, 128–132 (2014).
Oh, H., Jang, S. K., Lee, H. S., Lee, E. B. & Choi, K. H. Personality traits in individuals with the dual diagnosis of psychosis and substance use disorders: a comprehensive review and meta-analysis. J. Dual Diagn. https://doi.org/10.1080/15504263.2020.1839827 (2021).
Burnay, J., Billieux, J., Blairy, S. & Larøi, F. Which psychological factors influence Internet addiction? Evidence through an integrative model. Comput. Human Behav. 43, 28–34 (2015).
Mallorquí-Bagué, N. et al. Impulsivity and cognitive distortions in different clinical phenotypes of gambling disorder: profiles and longitudinal prediction of treatment outcomes. Eur. Psychiatry 61, 9–16 (2019).
Davis, C. et al. Evidence that ‘food addiction’ is a valid phenotype of obesity. Appetite 57, 711–717 (2011).
Özcan, U. et al. Endoplasmic reticulum stress links obesity, insulin action, and type 2 diabetes. Science 306, 457–461 (2004).
Saunders, T. J. et al. Associations of sedentary behavior, sedentary bouts and breaks in sedentary time with cardiometabolic risk in children with a family history of obesity. PLoS ONE 8, e79143 (2013).
Avila, C. et al. An overview of links between obesity and mental health. Curr. Obes. Rep. 4, 303–310 (2015).
Kiehm, T. G., Anderson, J. W. & Ward, K. Beneficial effects of a high carbohydrate, high fiber diet on hyperglycemic diabetic men. Am. J. Clin. Nutr. 29, 895–899 (1976).
Coskunpinar, A., Dir, A. L. & Cyders, M. A. Multidimensionality in impulsivity and alcohol use: a meta-analysis using the UPPS model of impulsivity. Alcohol. Clin. Exp. Res. 37, 1441–1450 (2013).
Hershberger, A., Connors, M., Um, M. & Cyders, M. A. The theory of planned behavior and e-cig use: impulsive personality, e-cig attitudes, and e-cig use. Int. J. Ment. Health Addict. 16, 366–376 (2018).
Acknowledgements
We thank all the volunteers for the participation and personnel for the contribution in the PREDIMED-Plus trial. We also thank all the investigators of the PREDIMED-Plus study. CIBERobn (Centros de Investigación Biomédica en Red: Obesidad y Nutrición), is an initiative of ISCIII, Madrid, Spain. The authors also thank the PREDIMED-Plus Biobank Network, as a part of the National Biobank Platform of the Carlos III Health Institute (ISCIII) for storing and managing the PREDIMED-Plus biological samples. Food companies Hojiblanca (Lucena, Spain) and Patrimonio Comunal Olivarero (Madrid, Spain) donated extra virgin olive oil, and the Almond Board of California (Modesto, CA), American Pistachio Growers (Fresno, CA), and Paramount Farms (Wonderful Company, LLC, Los Angeles, CA) donated nuts.
Funding
Study resulting from the following grants: SLT006/17/00246 and SLT002/16/00045, funded by the Department of Health of the Generalitat de Catalunya by the calls “Acció instrumental de programes de recerca orientats en l'àmbit de la recerca i la innovació en salut” and "Pla estratègic de recerca i innovació en salut (PERIS)". We thank CERCA Programme/Generalitat de Catalunya for institutional support. This project was funded by Instituto de Salud Carlos III (ISCIII), the Spanish Government Official Agency for funding biomedical research—with competitive grants leaded by Jordi Salas-Salvadó and Josep Vidal for the periods 2014–2016, 2015–2017, 2017–2019 and 2018–2020, through the Fondo de Investigación para la Salud (FIS), which is co-funded by the European Regional Development Fund [grants: PI13/00233, PI13/00728, PI13/01123, PI13/00462, PI16/00533, PI16/00366, PI16/01094, PI16/00501, PI19/00017, PI19/00781, PI19/01032, PI19/00576]; the Especial Action Project entitled: Implementación y evaluación de una intervención intensiva sobre la actividad física Cohorte PREDIMED-Plus grant to Jordi Salas-Salvadó; the European Research Council [Advanced Research Grant 2014–2019; agreement #340918] granted to Miguel Ángel Martínez-González; the Recercaixa (number 2013ACUP00194) grant to Jordi Salas-Salvadó. This research was also partially funded by EU-H2020 Grants (Eat2beNICE/H2020-SFS-2016-2; Ref 728018; and PRIME/H2020-SC1-BHC-2018-2020; Ref: 847879) and Instituto Salud Carlos III (Fondo Investigación Sanitario, FIS: PI17/01167), Grant PROMETEO/2017/017 (Generalitat Valenciana) and Grant FEA/SEA 2017 for Primary Care Research. This work is also partially supported by ICREA under the ICREA Academia programme. None of these funding sources plays any role in the design, collection, analysis, or interpretation of the data or in the decision to submit manuscripts for publication. MLM and CVA are supported by a predoctoral Grant of the Ministerio de Educación, Cultura y Deporte (FPU15/02911 and FPU16/01453). This work was supported by grants from DIUE de la Generalitat de Catalunya 2017 SGR 138 (RTF) from the Departament d’Economia i Coneixement de la Generalitat de Catalunya (Spain). The funders of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report.
Author information
Authors and Affiliations
Contributions
The authors’ responsibilities were as follows: F.F.-A., Rd.T. and N.M.-B., designed the current study; N.M.-B., M.L.-M., C.V-.A., L.F., A.C., and A.D.-L. conducted the study and collected the data; N.M.-B., M.L.-M., C.V.-A., L.F., A.D.-L., R.F.-C., S.J.-M., D.C., X.P., A.C., M.B., J.S.-S., Rd.T., F.F.-A. provided essential materials; R.G. analysed the data; N.M.-B., M.L.-M., R.G., F.F.-A. and Rd.T.: wrote the manuscript; N.M.-B., M.L.-M., C.V.-A., R.G., J.S.-S., S.J.-M., F.F.-A. and Rd.T. had primary responsibility for the final content; and all authors participated in data interpretation, provided critical review and commentary on the draft of the manuscript, and read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mallorquí-Bagué, N., Lozano-Madrid, M., Vintró-Alcaraz, C. et al. Effects of a psychosocial intervention at one-year follow-up in a PREDIMED-plus sample with obesity and metabolic syndrome. Sci Rep 11, 9144 (2021). https://doi.org/10.1038/s41598-021-88298-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-88298-1
This article is cited by
-
Applying psycho-behavioural phenotyping in obesity characterization
Reviews in Endocrine and Metabolic Disorders (2023)
-
Food Addiction and Impulsivity in Clinical Populations by Gender: a Systematic Review
Current Addiction Reports (2023)
-
Impact of Food Addiction in Therapy Response in Obesity and Eating Disorders
Current Addiction Reports (2022)
-
Impulsivity is longitudinally associated with healthy and unhealthy dietary patterns in individuals with overweight or obesity and metabolic syndrome within the framework of the PREDIMED-Plus trial
International Journal of Behavioral Nutrition and Physical Activity (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.