Abstract
This study evaluated the association of contact point locations with the knee medial and lateral contact force (Fmed, Flat) alterations in OA and healthy subjects. A musculoskeletal model of the lower limb with subject-specific tibiofemoral contact point trajectories was used to estimate the Fmed and Flat in ten healthy and twelve OA subjects during treadmill gait. Regression analyses were performed to evaluate the correlation of the contact point locations, knee adduction moment (KAM), knee flexion moment (KFM), frontal plane alignment, and gait speed with the Fmed and Flat. Medial contact point locations in the medial–lateral direction showed a poor correlation with the Fmed in OA (R2 = 0.13, p = 0.01) and healthy (R2 = 0.24, p = 0.001) subjects. Anterior–posterior location of the contact points also showed a poor correlation with the Fmed of OA subjects (R2 = 0.32, p < 0.001). Across all subjects, KAM and KFM remained the best predictors of the Fmed and Flat, respectively (R2 between 0.62 and 0.69). Results suggest different mechanisms of contact force distribution in OA joints. The variations in the location of the contact points participate partially to explains the Fmed variations in OA subjects together with the KFM and KAM.
Similar content being viewed by others
Introduction
Excessive or less frequent loading, misplaced contact regions, and altered muscle loading are among the biomechanical factors associated with the pathogenesis of knee osteoarthritis (OA)1. Knee OA is mostly developed on the medial compartment through which a major percentage of the total contact force (Ftot) is transferred1,2,3. Reducing the knee medial contact force (Fmed) has been the focus of many studies using osteotomy surgery4, or noninvasive techniques such as cane or shoe soles, gait modifications, and valgus braces5,6,7,8 which could eventually change the frontal plane alignment or knee adduction moment (KAM). Therefore, characterizing the biomechanical parameters that contribute to the Fmed can help to get insight the mechanism of OA initiation and help to find more effective therapeutic interventions to potentially slow down the OA progression.
Due to the complexity and the limited feasibility of estimating the contact forces using either musculoskeletal models or instrumented implants, the KAM has been widely used as a surrogate for the Fmed or the medial-to-total contact force ratio (MR)9,10,11,12,13,14,15,16. Despite the considerable evidence on the relationship between the KAM with the Fmed17, and with the medial compartment OA progression1,18,19, the level of KAM correlation with the Fmed is still debated20. In fact, the coefficient of determination (R2) between KAM and Fmed from the linear regression models in previous studies falls in a wide range from 19 to 76%14,15,16,21,22,23. The values of R2 were also considerably variable across the subjects suggesting that the KAM is much less able to explain the variability in the Fmed and/or MR in some individuals14. Several other parameters were suggested to increase the Fmed. Among those, the knee flexion moment (KFM)23,24, frontal plane alignment20,25, and gait speed14 were found to have substantial correlation with the Fmed. Moreover, sensitivity analysis studies showed that the anterior–posterior and medial–lateral locations of the tibiofemoral contact points had also a high impact on the contact forces and the force distribution between the medial and lateral compartments26,27,28,29. For instance, in a simulation study, Lerner et al. (2015) reported a 6% increase in the MR per each millimeter of the contact point medial shift (R2 = 0.99). Since there has been no means to straightforwardly incorporate the subject-specific contact point trajectories into the contact force estimations, no study could have tested the association of contact point locations with the knee medial and lateral contact force. Recently, Zeighami et al.(2018)28 incorporated the subject-specific contact point trajectories obtained from 3D/2D registration techniques into the medial and lateral knee contact force estimations. This technique currently allows evaluating the correlation of the contact point locations with the Fmed and Flat alongside the other parameters.
In addition, most of the studies on the Fmed are performed in knee arthroplasty subjects, and the data on the intact healthy and OA knees are scarce. The few available OA-control studies which estimated the Fmed and Flat used a classical linear model of the contact point trajectories or a generic deformable model of the knee24,30,31,32,33,34, and therefore, did not take into account the inter-subject variations and the distinct patterns of the anterior–posterior and medial–lateral contact point locations in healthy and OA subjects35,36.
Therefore the objectives of this study are (1) to estimate the Fmed and Flat in both healthy and OA subjects using the subject-specific contact point trajectories obtained from 3D/2D registration techniques, and (2) to analyze the impact of the medial–lateral and anterior–posterior contact point locations along with KAM, KFM, gait speed, and frontal plane alignment on the Fmed and Flat.
Materials and methods
Experimental protocol
Ten healthy (6 men, 4 women, 55 yrs., 1.68 m, 71 kg) and 12 severe OA (2 men, 10 women, 59 yrs.1.61 m, 85.53 kg, K–L grade 4) subjects were asked to walk at their comfortable speed on an instrumented split-belt treadmill for 45 s (Table 1). Data from force platforms and reflective markers mounted on the kneeKG™ system37 were filtered using a zero-lag 2nd order Butterworth filter with cut-off frequencies automatically calculated using a power spectrum analysis (PSA) algorithm38.
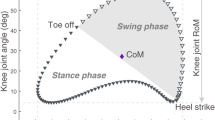
The subject-specific contact point trajectories were approximated using a weighted center of bone-to-bone proximity algorithm during a quasi-static squat task36. The 3D models of the tibia and femur were reconstructed and registered from EOS™ low-dose biplane X-ray images of the subjects recorded at 0°, 15°, 30°, 45°, and 70° of knee flexion (Fig. 1). The subject-specific tibiofemoral contact point trajectories were built as a function of the knee flexion angle as described earlier28. The frontal plane alignment was measured from the reconstructed tibia and femur of the subjects at the standing posture (~ 0°).
All subjects signed an informed consent form and the experimental protocol was approved by the ethics committees of the Centre de Recherche, Centre Hospitalier de l’Université de Montréal (CRCHUM) and École de Technologie Supérieure de Montréal (ÉTS). All the research and methods in this study were performed in accordance with the CRCHUM and ÉTS ethics committee guidelines as well as with the Helsinki Declaration of 1975, as revised in 2000.
Musculoskeletal model with subject-specific contact point trajectories
The medial and lateral knee contact forces were estimated using a musculoskeletal model of the lower limb with the integration of the subject-specific contact point trajectories28 (Fig. 1). The model consists of 5 segments and 5 joint degrees of freedom (DOF), with the hip joint modeled as a ball and socket joint (3 DOF) and the ankle modeled as a ball and socket joint plus two isometric ligaments (1 DOF). The tibiofemoral joint (1 DOF) is defined by 5 kinematic constraints derived from the subject-specific tibiofemoral contact point trajectories: at each flexion angle, the femoral and tibial contact points are superimposed in the 3 spatial directions on the medial compartment, and in both anterior–posterior and proximal–distal directions on the lateral compartment. The proximal–distal constraints on each compartment allow for a straightforward computation of medial and lateral contact forces28. The musculo-tendon origin and insertion points were adopted from Delp et al. (1990)39.
A full description of the musculoskeletal model of the lower limb (except for the tibiofemoral joint) is detailed in40. The model medial and lateral contact force estimations, without subject-specific contact point trajectories, were previously validated40,41,42 against instrumented implants data. For a semi-quantitative validation of the model with the subject-specific tibiofemoral contact points, the active/inactive state of 8 muscles was compared (i.e. concordance coefficients43) to the EMG signals to check if the model predictions are realistic for 10 healthy subjects28. The EMG concordance coefficients for the OA and healthy subjects of the current study are provided in the supplementary material (1).
The contact forces were calculated in a one-step procedure simultaneously minimizing the contact and musculo-tendon forces. Internal joint moments are computed by inverse dynamics (they equal the inter-segmental action of muscles, ligaments, and contacts forces in the model) and represent the action of the proximal onto the distal segment expressed in the joint coordinate system44,45,46. The external knee adduction (KAM) and knee flexion moments (KFM) were obtained by reversing the corresponding internal moment signs.
The knee contact forces were normalized to body weight (BW) and the KAM and KFM were normalized to BW*height.
Statistical analysis
Linear regression tests were performed to evaluate the extent to which the independent variables were predictive of the Fmed and Flat in OA and healthy subjects. Given the limited number of subjects, the analyses were limited to simple linear regressions only. The dependent variables were Fmed and Flat at 4 peak instances being the 1st and 2nd medial and lateral peaks. The independent variables were the KAM, KFM, frontal plane alignment, gait speed, and positions of the medial and lateral contact points in the anterior–posterior (CPxmed, CPxlat), and medial–lateral (CPzmed, CPzlat) directions at the corresponding timing. The rationale for considering 4 peaks was because the peaks occurs at different timings of the medial and lateral contact. A non-parametric Mann–Whitney U-test was performed to compare all independent and dependent variables between the OA and healthy subjects (p < 0.05). The coefficients of determination (R2) were compared to identify the parameters that explains the greatest proportion of the variance of the dependent variables. The correlation was considered poor, moderate, or good if R2 ≤ 0.50, 0.50 < R2 < 0.75, and R2 > 0.75, respectively. The regression model was rated as significant for p < 0.05. The correlation with each variable was independently tested.
Results
OA and healthy group comparison
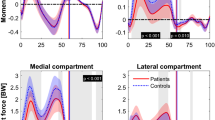
The differences at 1st and 2nd peak Fmed, Flat, and Ftot were not significant between the OA and healthy groups (p > 0.05) (Fig. 2). The contact forces in healthy and OA subjects averaged slightly higher than the OA subjects at the 2nd peak Fmed (OA = 1.7 BW, healthy = 1.9 BW), 1st peak Flat (OA = 1.1 BW, healthy = 1.2 BW), 2nd peak Flat (OA = 0.5 BW, healthy = 0.6 BW), 1st peak Ftot (OA = 2.5 BW, healthy = 2.7 BW), and 2nd peak Ftot (OA = 2.1 BW, healthy = 2.4 BW), and were similar at the 1st peak Fmed (OA = healthy = 1.6 BW). The Fmed, Flat, and Ftot over the stance phase are presented in the supplementary material (2).
Box and whisker plot of contact forces of the healthy (blue) and OA (red) groups at the 1st and 2nd peaks of medial contact force (pk1 Med, pk2 Med), 1st and 2nd peaks of the lateral contact force (pk1 Lat, pk2 Lat), 1st and 2nd peaks of the total contact force (pk1 Tot, pk2 Tot), the average medial (mean Med) and lateral (mean Lat) contact forces during the stance phase, and the medial-to-total contact force ratio (MR) during the stance phase. The plot represents the minimum, maximum, lower and higher quartiles, and the median as well as the mean value (X mark), and the outliers (o mark).
The average KAM in OA subjects at the timing of the 1st and 2nd peaks of Fmed and Flat were significantly greater than that of the healthy subjects (p < 0.05). Contra wise, the average KFM was not significantly different between OA and healthy subjects (p > 0.05). The KAM and KFM plots are provided in the supplementary material (3).
The CPzmed and CPzlat at the timing of the 1st and 2nd peaks of Fmed and Flat represented significant differences (p < 0.001) between the two groups while the CPxmed and CPxlat were not significantly different (p > 0.05). The individual contact point trajectories are provided in the supplementary material (4) and were extensively described in Zeighami et al. (2017)36.
The frontal plane alignment in OA subjects (6.26°) was significantly greater than in the healthy subjects (0.57°, p < 0.01). The groups were not matched for height, BMI (p < 0.05), and gender (Table 1). Gait speed did not significantly differ between the two groups (p = 0.11).
Medial and lateral contact force (Fmed, Flat) regression
The linear regression tests revealed that the KAM was the best predictor of Fmed both for OA (R2 = 0.62) and healthy (R2 = 0.62) subjects. No other variable accounted for more than 50% of the variance in Fmed in either group (Table 2). CPxmed was the second-best predictor of Fmed in OA subjects (R2 = 0.32) followed by the KFM (R2 = 0.16), gait speed (R2 = 0.15), and CPzmed (R2 = 0.13). In healthy subjects, the gait speed (R2 = 0.27) and CPzmed (R2 = 0.24) had the strongest correlation with the Fmed after the KAM.
The KAM, CPzmed, and gait speed were significantly correlated to the Fmed both in OA and healthy subjects. However, the Fmed in healthy subjects increases faster due to a unit increase in the KAM and CPzmed as the slopes of the regressions in healthy subjects (KAM:c2 = 0.62, CPzmed:c2 = 0.13) are higher than those in OA subjects (KAM:c2 = 0.48, CPzmed:c2 = 0.07) (Table 2). The gait speed slopes were similar in OA and healthy subjects (Table 2).
The KFM was the dominant predictor of the Flat in OA (R2 = 0.69) and healthy subjects (R2 = 0.68). Other significant parameters associated with the Flat consists of KAM (R2 = 0.19) and CPxlat (R2 = 0.10) in OA subjects, and gait speed (R2 = 0.16) in healthy subjects.
The KAM slopes are positive in the Fmed regressions both in OA and healthy subjects (OA KAM:c2 = 0.48, Healthy KAM:c2 = 0.62) while they are negative in the Flat regressions (OA KAM:c2 = − 0.22, Healthy KAM:c2 = − 0.13). Therefore, an increase in the KAM is associated to increase in the Fmed and a decrease in the Flat in both groups.
Discussion
The objective of this study was to estimate the knee contact forces in both healthy and OA subjects and to analyze the association of contact point locations with the knee medial and lateral contact force, alongside other parameters (KAM, KFM, frontal plane alignment, and gait speed). For that, we used a musculoskeletal model with subject-specific tibiofemoral joint contact point trajectories to investigate if the subject-specific contact point trajectories are correlated to the knee contact forces in OA and healthy subjects.
A large body of the literature reported the contact forces using prosthetic measurements or musculoskeletal model estimations. Our contact force estimations (Table 3) falls within the literature range for the peaks of Fmed (2.1 ± 0.5 BW), Flat (0.9 ± 0.4 BW), and Ftot (3.1 ± 0.8 BW)6,7,8,11,27,30,40,47,48,49,50,51,52,53. More recently, there has been an increased interest towards comparing the Fmed and Flat in OA and healthy subjects24,30,31,32,34. Sritharan et al. (2017)30 and Kumar et al. (2013)24 used musculoskeletal models with classical linear contact point trajectories to estimate the contact forces. They reported that despite the differences between the absolute values of the contact forces in the two groups (Table 3), the differences were not significant which is in accordance with our results. The peaks of Fmed in both studies were greater than the peaks of Flat. Other studies reported similar values with slightly different contact forces between OA and healthy groups (Table 3). While we found no significant differences in the knee contact forces between OA and healthy subjects, the external moments, the contact point locations, and the corresponding regression coefficients and slopes were different, suggesting altered mechanisms of contact force distribution in the OA joint.
The external moments on the knee joint are thought to be counterbalanced by the musculotendon and the tibiofemoral contact forces. The static equilibrium of the knee joint in the frontal plane requires that the contact point locations be related to the Fmed and Flat54. Therefore, it is conceivable that the load taken by each compartment is proportional to the contact point distance from the joint center as postulated by previous sensitivity analyses27,29. Nevertheless, a multifactorial study, considering the 3D joint equilibrium, suggested that there are other factors which confound a strong correlation between the contact point location and the Fmed28. However, the contributing parameters and their association with the Fmed and Flat modification were not previously investigated.
Overall, the Fmed was better predicted by the contact point locations than the Flat both in OA and healthy subjects. The contact point locations in the two directions (R2 = 0.13 and R2 = 0.32) and the contact point location in medial–lateral direction (R2 = 0.24) were among the significant, yet low, predictors of the Fmed in OA and healthy subjects. A weak correlation between the peaks of Fmed and the CPzmed was similarly reported in a previous study on healthy subjects28. The lateral contact point location in anterior–posterior (CPxlat) direction was the only component of the contact point slightly correlated with the Flat in OA subjects (R2 = 0.10, p = 0.032). To our knowledge, our study is the first one to analyze the correlations between subject-specific contact point locations and contact forces. In the literature, sensitivity analyses have previously studied the impact of the contact point locations in both the anterior–posterior and medial–lateral directions and have established they are sensitive model parameters26,27,28,29. The reported sensitivity of 0.04 and 0.03 BW/mm on the first and second peaks of Fmed are close to the slopes of regression found in our study29.
Before our study, it was not clear, especially in OA patients, how these correlations between the contact point location and the contact force compare with respect to other correlations. The KFM and KAM accounted for a high proportion of the variance in Fmed and Flat compared to the components of the contact point location. The KAM was the most powerful predictor of the Fmed in both OA and healthy groups (R2 = 0.62), whereas it had a smaller effect on the Flat only in the OA group (R2 = 0.19). The most powerful predictor of the Flat was the KFM in both groups reflecting the contrasting influence of the sagittal and frontal plane knee moments on the medial and lateral contact forces.
The importance of the KFM in estimating the magnitude or variation of Fmed was also highlighted in previous studies both in OA and healthy subjects24,55. Meireles et al. (2016)56 performed regression tests with KFM and KAM inputted independently. They found that in early OA subjects, the correlation of KFM and KAM with the 1st peak of medial contact force were similar (R2 = 0.62, 0.67 accordingly). They also reported that, in healthy controls, the correlation with the KAM (R2 = 0.65) was much higher than with the KFM (R2 = 0.21). This implies the knee load sharing can be affected by the knee pathology with KFM having a more important impact on the Fmed in OA group with respect to the healthy group. This is similar to the higher correlation of KFM with the Fmed in OA subjects in our study. Manal et al. (2013)57 reported that the KFM adds an additional 22% to the 63% of the variance in the Fmed peak which is explained by the KAM. Both moments together accounted for ~ 85% of the Fmed variation. In the current study, we found a similar correlation of KAM (R2 ~ 0.62) with the Fmed. In an instrumented implant study, Trepczynski et al. (2014)17 observed that the KAM alone accounted for 87% of the Fmed variation. The higher contribution of KAM in their study could be attributed to the prosthetic knee which has a different joint configuration and congruence compared to the native knees.
We did not find a significant correlation between the frontal plane alignment and the Fmed, or Flat (p > 0.05). In an FE simulation study with one subject, the frontal plane alignment was reported a much more effective factor in reducing Fmed compared to the KAM20. Nevertheless, Kumar et al. (2013)24 failed to find a significant correlation between frontal plane alignment and the Fmed peak in neither healthy (n = 12) or OA (n = 16) groups. In our study, we did not find a significant correlation between the frontal plane alignments (at the standing posture) and Fmed (p > 0.05).
Gait speed was correlated to the Fmed and Flat in healthy, and to the Fmed in OA subjects. The Fmed was similarily increases by a similar rate in OA and healthy subjects due to an increase in the gait speed as its slope of regression in both groups is similar.
The current study has several limitations. The subject-specific contact point trajectories were measured during a quasi-static squat and may vary in different weight-bearing tasks. Even though, Gasparutto et al. (2015)58 showed that the impact of the dynamic activity on the couplings between the joint degrees of freedom was limited. Similarly, a recent systematic review59 showed that CPxmed and CPxlat were in the range of other contact point trajectories measured by fluoroscopy on both OA and healthy subjects during various weight-bearing tasks (gait, step-up, kneeling, squat…). The estimation of the contact point trajectories is based on a weighted center of bone-to-bone proximity28 and is subject to inaccuracies in approximating the center of pressure. This is primarily due to the absence of cartilage layer and menisci in the X-ray images and the errors in the reconstruction and registration process36,60,61. Moreover, the contact point trajectories were interpolated from a limited number of contact point locations. Finally, the number of subjects is not enough to generalize the conclusions made in this study.
As a conclusion, in the current work, we assessed the association of the contact point locations with the alterations of the knee contact forces and their distribution. Fmed was influenced more than the Flat by the contact point locations in both directions especially in OA subjects. Overall, the contact point locations had lower correlation with respect to the KFM and KAM and the two moments remained the best predictors of the Fmed and Flat. KAM and KFM can be easily estimated from classical inverse dynamics while obtaining subject-specific contact points require more complex procedures. However, the correlation between the contact points and the contact forces helps to understand the proportion of the variation in the contact forces which is not explained by the KAM and KFM. Even though the contact force variables (Fmed, Flat, and Ftot) did not present significant differences between the OA and healthy groups, the correlations were different (typically the slopes of regression), suggesting altered mechanisms of contact force distribution in the OA joint. Knowledge of the association of various parameters with the knee contact forces distribution could eventually lead to better understand the OA progression mechanism and help better planning the most effective interventions to slow the disease process. In a review of the biomechanical characteristics that have possible influence over articular tissue loading in OA, altered KAM and KFM, as well as slower gait speed (together with more flexed knees, reduced range of motion, muscle atrophy and other characteristics that were not analyzed in our study) were associated to lower contact forces, altered distribution of Fmed and Flat and different region of articular surface loaded62. The altered contact point trajectories were not directly listed in this review and our study demonstrate that this characteristics is also associated to altered distribution of Fmed and Flat. Typically, a more posterior and medial contact point location in the medial compartment is associated to a lower Fmed in OA patients.
Data availability
All data generated or analyzed during this study are included in this published article (and its Supplementary Information files).
Abbreviations
- OA:
-
Knee osteoarthritis
- Ftot :
-
Knee total contact force
- Fmed :
-
Knee medial contact force
- Flat :
-
Knee lateral contact force
- MR:
-
Medial-to-total contact force ratio
- KAM:
-
Knee adduction moment
- KFM:
-
Knee flexion moment
- R2 :
-
Coefficient of determination
- DOF:
-
Degrees of freedom
- BW:
-
Body weight
- CPzmed:
-
Medial contact point in the anterior–posterior direction
- CPzlat:
-
Lateral contact point in the anterior–posterior direction
- CPxmed:
-
Medial contact point in the medial–lateral direction
- CPxlat:
-
Lateral contact point in the medial–lateral direction
References
Miyazaki, T. et al. Dynamic load at baseline can predict radiographic disease progression in medial compartment knee osteoarthritis. Ann. Rheum. Dis. 61, 617–622 (2002).
Johnson, F., Scarrow, P. & Waugh, W. Assessments of loads in the knee joint. Med. Biol. Eng. Comput. 19, 237–243 (1981).
Prodromos, C. C., Andriacchi, T. & Galante, J. A relationship between gait and clinical changes following high tibial osteotomy. J. Bone Jt. Surg. Am. Vol. 67, 1188–1194 (1985).
Briem, K., Ramsey, D. K., Newcomb, W., Rudolph, K. S. & Snyder-Mackler, L. Effects of the amount of valgus correction for medial compartment knee osteoarthritis on clinical outcome, knee kinetics and muscle co-contraction after opening wedge high tibial osteotomy. J. Orthop. Res. 25, 311–318 (2007).
Kemp, G., Crossley, K. M., Wrigley, T. V., Metcalf, B. R. & Hinman, R. S. Reducing joint loading in medial knee osteoarthritis: Shoes and canes. Arthritis Care Res. 59, 609–614 (2008).
Fregly, B. J., D’Lima, D. D. & Colwell, C. W. Effective gait patterns for offloading the medial compartment of the knee. J. Orthop. Res. 27, 1016–1021 (2009).
Erhart, J. C., Dyrby, C. O., D’Lima, D. D., Colwell, C. W. & Andriacchi, T. P. Changes in in vivo knee loading with a variable-stiffness intervention shoe correlate with changes in the knee adduction moment. J. Orthop. Res. 28, 1548–1553 (2010).
Kutzner, I. et al. The effect of valgus braces on medial compartment load of the knee joint–in vivo load measurements in three subjects. J. Biomech. 44, 1354–1360 (2011).
Butler, R. J., Marchesi, S., Royer, T. & Davis, I. S. The effect of a subject-specific amount of lateral wedge on knee mechanics in patients with medial knee osteoarthritis. J. Orthop. Res. 25, 1121–1127 (2007).
Kinney, A. L. et al. Changes in in vivo knee contact forces through gait modification. J. Orthop. Res. 31, 434–440 (2013).
Zhao, D. et al. Correlation between the knee adduction torque and medial contact force for a variety of gait patterns. J. Orthop. Res. 25, 789–797 (2007).
Schipplein, O. & Andriacchi, T. Interaction between active and passive knee stabilizers during level walking. J. Orthop. Res. 9, 113–119 (1991).
Astephen, J. & Deluzio, K. Changes in frontal plane dynamics and the loading response phase of the gait cycle are characteristic of severe knee osteoarthritis application of a multidimensional analysis technique. Clin. Biomech. 20, 209–217 (2005).
Kutzner, I., Trepczynski, A., Heller, M. O. & Bergmann, G. Knee adduction moment and medial contact force–facts about their correlation during gait. PLoS ONE 8, e81036 (2013).
Meyer, A. J. et al. Are external knee load and EMG measures accurate indicators of internal knee contact forces during gait?. J. Orthop. Res. 31, 921–929 (2013).
Richards, R., Andersen, M. S., Harlaar, J. & van den Noort, J. Relationship between knee joint contact forces and external knee joint moments in patients with medial knee osteoarthritis: Effects of gait modifications. Osteoarthritis Cartilage 26, 1203–1214 (2018).
Trepczynski, A., Kutzner, I., Bergmann, G., Taylor, W. R. & Heller, M. O. Modulation of the relationship between external knee adduction moments and medial joint contact forces across subjects and activities. Arthritis Rheumatol. 66, 1218–1227 (2014).
Bennell, K. L. et al. Higher dynamic medial knee load predicts greater cartilage loss over 12 months in medial knee osteoarthritis. Ann. Rheum. Dis. 70, 1770–1774 (2011).
Thorp, L. E. et al. Knee joint loading differs in individuals with mild compared with moderate medial knee osteoarthritis. Arthritis Rheumatol. 54, 3842–3849 (2006).
Adouni, M. & Shirazi-Adl, A. Partitioning of knee joint internal forces in gait is dictated by the knee adduction angle and not by the knee adduction moment. J. Biomech. 47, 1696–1703 (2014).
Walter, J. P., D’Lima, D. D., Colwell, C. W. & Fregly, B. J. Decreased knee adduction moment does not guarantee decreased medial contact force during gait. J. Orthop. Res. 28, 1348–1354 (2010).
Walter, J. P., Korkmaz, N., Fregly, B. J. & Pandy, M. G. Contribution of tibiofemoral joint contact to net loads at the knee in gait. J. Orthop. Res. 33, 1054–1060 (2015).
Esculier, J.-F., Willy, R. W., Baggaley, M. W., Meardon, S. A. & Willson, J. D. Sex-specific kinetic and kinematic indicators of medial tibiofemoral force during walking and running. Knee 24, 1317–1325 (2017).
Kumar, D., Manal, K. T. & Rudolph, K. S. Knee joint loading during gait in healthy controls and individuals with knee osteoarthritis. Osteoarthritis Cartilage 21, 298–305 (2013).
Marouane, H. & Shirazi-Adl, A. Sensitivity of medial-lateral load sharing to changes in adduction moments or angles in an asymptomatic knee joint model during gait. Gait Posture 70, 39–47 (2019).
Nissan, M. Review of some basic assumptions in knee biomechanics. J. Biomech. 13, 375–381 (1980).
Lerner, Z. F., DeMers, M. S., Delp, S. L. & Browning, R. C. How tibiofemoral alignment and contact locations affect predictions of medial and lateral tibiofemoral contact forces. J. Biomech. 48, 644–650 (2015).
Zeighami, A., Aissaoui, R. & Dumas, R. Knee medial and lateral contact forces in a musculoskeletal model with subject-specific contact point trajectories. J. Biomech. 69, 138–145 (2018).
Saliba, C. M., Brandon, S. C. & Deluzio, K. J. Sensitivity of medial and lateral knee contact force predictions to frontal plane alignment and contact locations. J. Biomech. 57, 125–130 (2017).
Sritharan, P. et al. Musculoskeletal loading in the symptomatic and asymptomatic knees of middle-aged osteoarthritis patients. J. Orthop. Res. 35, 321–330 (2017).
Dell’Isola, A., Smith, S., Andersen, M. S. & Steultjens, M. Knee internal contact force in a varus malaligned phenotype in knee osteoarthritis (KOA). Osteoarthritis Cartilage 25, 2007–2013 (2017).
Meireles, S. et al. Medial knee loading is altered in subjects with early osteoarthritis during gait but not during step-up-and-over task. PLoS ONE 12, e0187583 (2017).
Van Rossom, S. et al. Knee joint loading in healthy adults during functional exercises: Implications for rehabilitation guidelines. J. Orthop. Sports Phys. Ther. 48, 162–173 (2018).
Van Rossom, S., Khatib, N., Holt, C., Van Assche, D. & Jonkers, I. Subjects with medial and lateral tibiofemoral articular cartilage defects do not alter compartmental loading during walking. Clin. Biomech. 60, 149–156 (2018).
Farrokhi, S., Voycheck, C. A., Gustafson, J. A., Fitzgerald, G. K. & Tashman, S. Knee joint contact mechanics during downhill gait and its relationship with varus/valgus motion and muscle strength in patients with knee osteoarthritis. Knee 23, 49–56 (2016).
Zeighami, A. et al. Tibio-femoral joint contact in healthy and osteoarthritic knees during quasi-static squat: A bi-planar X-ray analysis. J. Biomech. 53, 178–184 (2017).
Hagemeister, N. et al. A reproducible method for studying three-dimensional knee kinematics. J. Biomech. 38, 1926–1931 (2005).
Aissaoui, R., Husse, S., Mecheri, H., Parent, G. & De Guise, J. in 2006 IEEE International Symposium on Industrial Electronics 614–619 (IEEE).
Delp, S. L. et al. An interactive graphics-based model of the lower extremity to study orthopaedic surgical procedures. IEEE Trans. Biomed. Eng. 37, 757–767 (1990).
Moissenet, F., Chèze, L. & Dumas, R. A 3D lower limb musculoskeletal model for simultaneous estimation of musculo-tendon, joint contact, ligament and bone forces during gait. J. Biomech. 47, 50–58 (2014).
Moissenet, F., Chèze, L. & Dumas, R. Influence of the level of muscular redundancy on the validity of a musculoskeletal model. J. Biomech. Eng. 138, 021019 (2016).
Moissenet, F., Giroux, M., Chèze, L. & Dumas, R. Validity of a musculoskeletal model using two different geometries for estimating hip contact forces during normal walking. Comput. Methods Biomech. Biomed. Engin. 18, 2000–2001 (2015).
Giroux, M., Moissenet, F. & Dumas, R. EMG-based validation of musculo-skeletal models for gait analysis. Comput. Methods Biomech. Biomed. Eng. 16, 152–154 (2013).
Wu, G. & Cavanagh, P. R. ISB recommendations for standardization in the reporting of kinematic data. J. Biomech. 28, 1257–1261 (1995).
Grood, E. S. & Suntay, W. J. A joint coordinate system for the clinical description of three-dimensional motions: Application to the knee (1983).
Wu, G. et al. ISB recommendation on definitions of joint coordinate system of various joints for the reporting of human joint motion—Part I: Ankle, hip, and spine. J. Biomech. 35, 543–548 (2002).
Manal, K. & Buchanan, T. S. An electromyogram-driven musculoskeletal model of the knee to predict in vivo joint contact forces during normal and novel gait patterns. J. Biomech. Eng. 135, 021014 (2013).
Lin, Y.-C., Walter, J. P., Banks, S. A., Pandy, M. G. & Fregly, B. J. Simultaneous prediction of muscle and contact forces in the knee during gait. J. Biomech. 43, 945–952 (2010).
Winby, C. R., Lloyd, D. G., Besier, T. F. & Kirk, T. B. Muscle and external load contribution to knee joint contact loads during normal gait. J. Biomech. 42, 2294–2300 (2009).
Lundberg, H. J., Foucher, K. C. & Wimmer, M. A. A parametric approach to numerical modeling of TKR contact forces. J. Biomech. 42, 541–545 (2009).
Kim, H. J. et al. Evaluation of predicted knee-joint muscle forces during gait using an instrumented knee implant. J. Orthop. Res. 27, 1326–1331 (2009).
Shelburne, K. B., Torry, M. R. & Pandy, M. G. Muscle, ligament, and joint-contact forces at the knee during walking. Med. Sci. Sports Exerc. 37, 1948–1956 (2005).
Shelburne, K. B., Torry, M. R. & Pandy, M. G. Contributions of muscles, ligaments, and the ground-reaction force to tibiofemoral joint loading during normal gait. J. Orthop. Res. 24, 1983–1990 (2006).
Stensgaard Stoltze, J., Rasmussen, J. & Skipper Andersen, M. On the biomechanical relationship between applied hip, knee and ankle joint moments and the internal knee compressive forces. Int. Biomech. 5, 63–74 (2018).
Creaby, M. It’s not all about the knee adduction moment: The role of the knee flexion moment in medial knee joint loading. Osteoarthritis Cartilage 23, 1038–1040 (2015).
Meireles, S. et al. Knee contact forces are not altered in early knee osteoarthritis. Gait Posture 45, 115–120 (2016).
Manal, K., Gardinier, E., Buchanan, T. S. & Snyder-Mackler, L. A more informed evaluation of medial compartment loading: The combined use of the knee adduction and flexor moments. Osteoarthritis Cartilage 23, 1107–1111 (2015).
Gasparutto, X., Moissenet, F., Lafon, Y., Cheze, L. & Dumas, R. Kinematics of the normal knee during dynamic activities: A synthesis of data from intracortical pins and biplane imaging. Appl. Bionics Biomech. 2017, 1908618 (2017).
Scarvell, J. M., Galvin, C. R., Perriman, D. M., Lynch, J. T. & van Deursen, R. W. Kinematics of knees with osteoarthritis show reduced lateral femoral roll-back and maintain an adducted position. A systematic review of research using medical imaging. J. Biomech. 75, 108–122 (2018).
Marouane, H., Shirazi-Adl, A. & Adouni, M. Alterations in knee contact forces and centers in stance phase of gait: A detailed lower extremity musculoskeletal model. J. Biomech. 49, 185–192 (2016).
DeFrate, L. E., Sun, H., Gill, T. J., Rubash, H. E. & Li, G. In vivo tibiofemoral contact analysis using 3D MRI-based knee models. J. Biomech. 37, 1499–1504 (2004).
Saxby, D. & Lloyd, D. Osteoarthritis year in review 2016: Mechanics. Osteoarthritis Cartilage 25, 190–198 (2017).
Acknowledgements
This work was supported by the Fonds de Recherche du Québec en Santé (FRQ-S), the Fonds de Recherche du Québec en Nature et Technologie (FRQ-NT), as well as by the Natural Science and Research Council of Canada (NSERC). This work was performed within the framework of the LABEX PRIMES (ANR-11-LABX-0063) of Université de Lyon, within the program "Investissements d'Avenir" (ANR-11-IDEX-0007) operated by the French National Research Agency (ANR). The funding sources were not involved in any part of the study design, collection, analysis, and interpretation of data, in the writing of the manuscript, nor in the decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Contributions
A.Z., R.D., and R.A. designed the study. Analysis was undertaken by A.Z. verified and approved by R.D. and R.A. A.Z. drafted the manuscript, revised by R.D., and R.A. All authors interpreted data, reviewed the article critically, and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zeighami, A., Dumas, R. & Aissaoui, R. Knee loading in OA subjects is correlated to flexion and adduction moments and to contact point locations. Sci Rep 11, 8594 (2021). https://doi.org/10.1038/s41598-021-87978-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-87978-2
This article is cited by
-
The effectiveness of a 6-week biofeedback gait retraining programme in people with knee osteoarthritis: protocol for a randomised controlled trial
BMC Musculoskeletal Disorders (2023)
-
Peak knee joint moments accurately predict medial and lateral knee contact forces in patients with valgus malalignment
Scientific Reports (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.