Abstract
To elucidate the disease-flare process in rheumatoid arthritis (RA) after discontinuing biological disease-modifying antirheumatic drugs (bDMARDs), we first focused on RA-flare prediction after achieving stringent remission criteria. Patients with RA who maintained a simplified disease activity index ≤ 3.3 for ≥ 3 months during November 2014–January 2018 in our medical centre in Tokyo, Japan, were eligible. The primary endpoint was flare (disease activity score 28—erythrocyte sedimentation rate ≥ 3.2 with increase from baseline > 0.6) within 2 years after bDMARD discontinuation. Comprehensive clinical assessments, ultrasonographic evaluation of 40 joints, and blood sampling for 12 biomarkers were performed every 2–3 months for 2 years unless patients experienced flare. Flare-positive and flare-negative patients were compared using univariate and Kaplan–Meier analyses. Thirty-six patients (80.6% female, median disease duration, 5.2 years; median treatment period with discontinued bDMARD, 2 years; median remission duration, 18 months) were enrolled. Twenty patients (55.6%) experienced RA flare 43–651 (median, 115) days after the first skipped date of bDMARDs. Two patients who withdrew without disease flare were excluded from the comparison. Clinical and ultrasonographic evaluations did not show significant between-group differences; Kaplan–Meier analysis showed that higher baseline soluble tumour necrosis factor receptor 1 (sTNFR1) concentration impacted subsequent disease flare (p = 0.0041); higher baseline interleukin (IL)-2 concentration was exclusively beneficial to patients with lower sTNFR1 (p = 0.0058), resulting in remission maintenance in 83.3% of patients with lower sTNFR1 and higher IL-2. We demonstrated the usefulness of combined biomarker evaluation for predicting sustained remission after bDMARD discontinuation in RA.
Similar content being viewed by others
Introduction
Sustained remission has become a realistic treatment target for patients with rheumatoid arthritis (RA)1. Clinical remission defined by the stringent criteria of the American College of Rheumatology (ACR)/the European League Against Rheumatism (EULAR)2, namely the Boolean remission criteria in which patients must achieve a tender joint count (TJC) of all 28 joints (TJC28) ≤ 1, swollen joint count (SJC) of 28 joints (SJC28) ≤ 1, patient global assessment of disease activity (PtGA) ≤ 1 (0–10 cm = 0–100 mm visual analogue scale [VAS]) and serum C-reactive protein (CRP) ≤ 1 mg/dL, or simplified disease activity index3 (SDAI; the sum of TJC28, SJC28, PtGA [cm], physician or other evaluators’ global assessment of disease activity [PhGA; cm] and CRP [mg/dL]) ≤ 3.3, has been actually achieved by a considerable portion of patients in recent clinical trials examining biological disease-modifying antirheumatic drugs (bDMARDs)4,5, as well as in observational studies6,7.
The pathogenesis of RA has not been fully elucidated partly because of difficulty in the evaluation and follow-up of the population before RA development8. Instead, the process of RA flare, which may mimic that of RA development, can be closely monitored. The economic burden of bDMARDs may justify their discontinuation when patients achieve clinical remission or low disease activity1, and evidence of bDMARD discontinuation in such patients has accumulated9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26. Importantly, many patients successfully regained remission or low disease activity by re-treatment with the same bDMARD when they experienced disease flare after bDMARD discontinuation in the above studies.
Therefore, this prospective study was conceived to elucidate the process of RA flare by sequential assessment of clinical, imaging, and biomarker parameters. In this first report, we focused on the prediction of RA flare after bDMARD discontinuation by assessing the above-mentioned parameters starting at the point of achieving ACR/EULAR-defined clinical remission.
Results
Demographic and clinical characteristics of enrolled patients
Demographic and clinical characteristics of the 36 patients are summarised in Table 1. Two patients did not complete the 2-year study, one due to sudden relocation on day 43 and the other because of death due to comorbidity (cardiomyopathy) on day 175; neither had experienced disease flare at the time of drop out. Thus, these patients were excluded from the comparative study between flare-positive and flare-negative patients. Twenty-nine (80.6%) patients were female, and the median (interquartile range [IQR]) age at enrolment was 69 (53–75) years. The median (IQR) disease duration was 5.2 years, treatment with the discontinued bDMARD had lasted for 2.1 (1.4–3.5) years, and the median (IQR) remission duration was 20 (9–31) months (< 6 months in only two patients). Most (72.2%) patients had been under treatment with first bDMARD and 76.5% and 77.8% of the patients were respectively positive for anti-cyclic citrullinated peptide antibody (anti-CCP) and rheumatoid factor.
In line with the fact that all enrolled patients fulfilled the SDAI ≤ 3.3 criterion, the medians (IQRs) of TJC28 and SJC were both 0 (0–0) as were those of Health Assessment Questionnaire-disability index (HAQ-DI). The median PtGA (mm VAS) was 3, and the median PhGA (mm VAS) was 0. The median CRP value was 0.04 mg/dL, and the median disease activity score 28—erythrocyte sedimentation rate (DAS28-ESR)27 and SDAI were 2.0 and 0.4, respectively. Importantly, 31 (86.1%) of 36 patients had achieved the ACR/EULAR Boolean remission criteria, which have been shown to be the most stringent criteria of clinical RA remission4. The ultrasonographic (US) examination of the 40 joints showed that the total power Doppler (PD) score was ‘0’ in 26 patients and ‘1’ in 5 patients. Therefore, imaging remission was confirmed in at least 72.2% of the enrolled patients.
Twenty-six (72.2%) patients had discontinued anti- tumour necrosis factor (TNF) bDMARD, while four and six patients had discontinued the non-TNF abatacept and tocilizumab, respectively. Methotrexate (MTX) was the predominant (69.4%) concomitant csDMARD as an anchor drug for RA in Japan and other countries1,28, while concomitant glucocorticoids were rarely administrated to patients (8.3%) who achieved SDAI remission.
Clinical comparison between patients experiencing RA flare and those maintaining remission
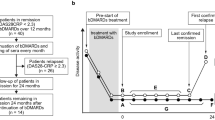
Among the 36 enrolled patients, 20 patients (55.6%) experienced RA flare within 2 years, with a range of 43–651 (median 115) days after the first skipped date of bDMARD infusion/injection (Fig. 1A). Notably, 18 (90%) of those patients received the same bDMARD thereafter and again achieved SDAI remission within 2 months. Another bDMARD was successfully introduced for one patient, and the remaining patient achieved SDAI remission after 9 months without treatment adjustment. Thus, the outcome of patients after experiencing disease flare was very favourable. In addition, two patients had not received any csDMARDs at baseline. One patient flared after tocilizumab discontinuation, and another patient did not flare for 2 years after etanercept discontinuation.
Remission maintenance rate and treatments. (A) All patients (n = 36, solid line) with 95% confidence intervals (dotted lines). (B) Comparison of patients discontinuing TNFi (n = 26, solid line) and non-TNFi (n = 8, dotted line). (C) Comparison of patients discontinuing first bDMARD (n = 24, solid line) and second or third bDMARD (n = 10, dotted line). (D) Comparison of patients with concomitant MTX (n = 23, solid line) and without MTX (n = 11, dotted line). TNFi tumour necrosis factor inhibitors, bDMARD biological disease-modifying antirheumatic drug, MTX methotrexate.
The comparison between flare-positive patients (n = 20) and patients who remained in remission (n = 14) is also shown in Table 1. The demographic characteristics were comparable between the two groups. Among the activity-related parameters, the ESR value and DAS28-ESR were numerically greater in flare-positive patients than in flare-negative patients, although the differences were not statistically significant (p = 0.077 and p = 0.058, respectively). US findings were also comparable for the greyscale (GS), PD, and total scores between flare-positive and flare-negative patients (p = 0.54, p = 0.88, and p = 0.53. respectively). Further, the proportion of patients who had a total PD score ≥ 2 was similar between the flare-positive and flare-negative groups (15.0% and 14.3%, respectively; p = 1.00).
As for the RA treatments, disease flare was similarly observed among patients who had discontinued TNF inhibitors versus non-TNF inhibitors, and those who had discontinued the first bDMARD versus the second or third bDMARD (Fig. 1B,C, Table 1). Patients who received MTX showed a trend for maintaining remission compared with those who did not receive MTX (Fig. 1D and Table 1), although the differences were not statistically significant. Therefore, clinical and imaging prediction of disease flare after bDMARD discontinuation in the patients who achieved the stringent criteria of RA remission was not suggested by this study.
Biomarker comparison between patients experiencing RA flare and those maintaining remission
Next, we compared the baseline plasma concentrations of nine cytokines and three soluble cytokine receptors relevant to the pathogenesis of RA and/or molecular targets of RA treatment (Table 2). Interestingly, although plasma IL-2 concentration was generally very low and undetectable in eight of 36 patients, it was significantly greater in flare-negative patients than in flare-positive patients (p = 0.017). A univariate logistic regression analysis and subsequent receiver operating characteristics (ROC) curve analysis suggested a cut-off value of 0.06287 pg/mL with an area under the curve (AUC) value of 0.74 (Supplementary Fig. 1A).
Moreover, the Kaplan–Meier analysis showed that lower baseline IL-2 concentration was associated with subsequent disease flare (p = 0.020, Supplementary Fig. 1B).
Although plasma concentrations of IL-6, TNF, and soluble tumour necrosis factor receptor 2 (sTNFR2) may be affected by some bDMARDs, a marginal difference in soluble tumour necrosis factor receptor 1 (sTNFR1) concentration between flare-positive and flare-negative patients (p = 0.064) led us to further analyses. The plasma sTNFR1 concentration was not correlated with CRP (r2 = 0.0044, p = 0.70; Fig. 2A), but it was significantly correlated with ESR (r2 = 0.14, p = 0.027; Fig. 2B), matrix metalloproteinase-3 (MMP-3) (r2 = 0.18, p = 0.012; Fig. 2C), and DAS28-ESR (r2 = 0.18, p = 0.011; Fig. 2D).
Correlation of plasma sTNFR1 concentration with RA disease activity at baseline (n = 36). The correlation coefficient (r) and p value were determined by Spearman’s rank test. (A) CRP; r2 = 0.0044, p = 0.70. (B) ESR; r2 = 0.14, p = 0.027. (C) MMP-3; r2 = 0.18, p = 0.012. (D) DAS28-ESR; r2 = 0.18, p = 0.011. sTNFR1 soluble tumour necrosis factor receptor 1, RA rheumatoid arthritis, CRP C-reactive protein, ESR erythrocyte sedimentation rate, MMP-3 matrix metalloproteinase-3, DAS28 disease activity score 28.
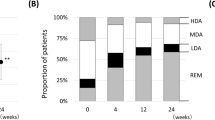
A logistic regression analysis and subsequent ROC analysis suggested a cut-off value of 1267.8 pg/mL with an AUC value of 0.69, and the Kaplan–Meier analysis showed that the baseline sTNFR1 concentration was associated with subsequent disease flare (p = 0.0041, Fig. 3A). The categorical distribution of sTNFR1 was independent of that of IL-2 (p = 0.73), and a higher baseline IL-2 concentration was beneficial for patients with a sTNFR1 concentration below the cut-off value (p = 0.0058, Fig. 3B), but not for those with sTNFR1 concentration above the cut-off value (p = 0.81, Fig. 3C).
Plasma cytokine profile at baseline as a predictive marker of RA flare after bDMARD discontinuation. (A) Comparison of patients with sTNFR1 ≤ cut-off (n = 20, solid line) and sTNFR1 > cut-off (n = 14, dotted line). (B) Comparison of patients with IL-2 > cut-off (n = 12, solid line) and IL-2 ≤ cut-off (n = 8, dotted line) in those with sTNFR1 ≤ cut-off (n = 20). (C) Comparison of patients with IL-2 > cut-off (n = 7, solid line) and IL-2 ≤ cut-off (n = 7, dotted line) in those with sTNFR1 > cut-off (n = 14). bDMARD biological disease-modifying antirheumatic drug, RA rheumatoid arthritis, sTNFR1 soluble tumour necrosis factor receptor 1, IL interleukin.
Discussion
This is the first study to comprehensively evaluate patients achieving clinical remission defined by the ACR/EULAR who had discontinued bDMARDs from the clinical, imaging, and biomarker perspectives. Our results indicated the usefulness of combining biomarker, but not clinical and imaging, assessments for the prediction of disease flare referring to the Outcome Measures in Rheumatology (OMERACT) validation study29 after bDMARD discontinuation in patients fulfilling the stringent criteria of clinical remission.
In this study, the median baseline values of enrolled patients were ‘0’ for TJC28, SJC28, PhGA (mm VAS), HAQ-DI, and total PD score of 40 joints. Despite such sufficient suppression of disease activity, 20 of 36 patients (55.6%) experienced disease flare within the 2 years of a bDMARDs-free period. Interestingly, baseline US examination and the confirmation of imaging remission added little to the prediction of subsequent RA flare in this study, which enrolled patients who had achieved the stringent criteria for RA remission. This fact is concordant with a recent idea that does not support the routine use of magnetic resonance imaging or US joint examination in the treat-to-target strategy30. However, two patients with US PD scores of 22 and 10, experienced disease flare at 55 and 105 days, respectively, after bDMARD discontinuation. These patients had one swollen joint in 28 joints and elevated MMP-3 (229.4 and 176.2 ng/mL, respectively). Therefore, US examination may be useful for patients achieving the stringent remission criteria despite some signs of residual arthritis activity. Nonetheless, it should be noted that imaging remission by US does not guarantee sustained remission after bDMARD discontinuation.
Several previous studies have suggested that longer disease duration, anti-CCP positivity, baseline radiographic damage, and residual disease activity at baseline were associated with disease flare after bDMARD discontinuation1,31,32. In fact, disease duration, anti-CCP positivity, and DAS28-ESR were numerically greater in flare-positive patients than in flare-negative patients, although statistically not significant in this study with a small sample size (Table 1). Instead, we identified sTNFR1 and IL-2 as predictive biomarkers of subsequent disease flare. Recently, a sub-analysis of the Reduction of Therapy in Rheumatoid Arthritis Patients in Ongoing Remission study19 found that multi-biomarker disease activity (MBDA) at baseline was significantly higher in patients with RA who relapsed than in those remaining in stable remission and those tapering/stopping DMARDs33. An MBDA score is calculated by the expression of 12 biomarkers including sTNFR1, IL-6, vascular endothelial growth factor, CRP, and MMP-3 which were also evaluated in this study34. The sTNFR1 is generated as a result of proteolytic shedding of TNFR1 by tumour necrosis factor-α-converting enzyme (TACE), a member of the ADAM (a disintegrin and metalloproteinase) family of zinc metalloproteinases35. As shown in Fig. 2, sTNFR1 concentration was positively correlated with DAS28-ESR, and the DAS28-ESR value was significantly higher in patients with sTNFR1 above the cut-off value than in those with sTNFR1 below the cut-off value (medians, 2.3 and 1.6, respectively, p = 0.022). These results suggest that sTNFR1 which is incorporated in the MBDA score, is a valid biomarker of RA disease activity even in patients achieving SDAI ≤ 3.3. In addition to the results shown in Fig. 3, a sensitivity analysis in patients discontinuing TNF inhibitors (n = 26) revealed that RA flare was observed in 83.3% (10 of 12) of patients with sTNFR1 above the cut-off value which was significantly greater than the flare rate of 28.6% (4 of 14) patients with sTNFR1 below the cut-off value (p = 0.0079). Furthermore, combining the sTNFR1 and IL-2 biomarkers is promising for the prediction of RA flare after bDMARD discontinuation (Fig. 2). Although the blood concentration of IL-2 was also found to be very low (approximately 1 pg/mL) in several other studies of non-rheumatic diseases36,37,38 and mostly below the lower limit of detection in a very recent study of predicting drug-free RA remission by a composite score incorporating three transcripts, IL-27, and Boolean remission39, and thus only detectable using high-sensitivity measurements, IL-2 is crucial for the development and expansion of regulatory T cells40,41 which may be associated with sustained RA remission.
The limitations of this study include the small sample size from a single centre and the lack of histological or cellular analyses. However, the comprehensive and intensive evaluations from multiple aspects including clinical, imaging and biomarker analyses are the strengths of the study.
In conclusion, this was the first study to identify the usefulness of a combined biomarker evaluation of sTNFR1 and IL-2 for the prediction of sustained remission for 2 years after bDMARD discontinuation in patients with RA. Recently, the difference between clinical remission and ‘molecular remission’ has been proposed by multi-omics monitoring of responses to bDMARDs in patients with RA42. Further analyses focusing on the next objectives including earlier detection of RA flare by comprehensive evaluations and the elucidation of relationships among clinical, imaging, and biomarker changes are ongoing in our laboratory.
Methods
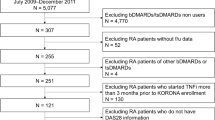
Patients
Patients with RA who visited Toho University Ohashi Medical Center in Tokyo, Japan, between November 2014 and January 2018 were eligible for the Flare Landscape from clinical, imaging, and biomarker Aspects In Rheumatoid arthritis (FLAIR) study when they met all of the following criteria: (1) fulfilling the 2010 ACR/EULAR classification criteria for RA43; (2) maintaining ACR/EULAR clinical remission defined by SDAI ≤ 3.3 for at least 3 months on ≥ 2 visits; (3) being willing to discontinue an ongoing bDMARD with consideration of the risk–benefit balance of bDMARD discontinuation.
Study design
This was a 2-year, prospective, observational study. The primary endpoint was flare DAS28-ESR ≥ 3.2 with an increase from the baseline, > 0.629) within 2 years after bDMARD discontinuation. The study protocol was approved by the Ethics Committee of Toho University Ohashi Medical Center (Ohashi approval number, 14–9), and this study was carried out in compliance with the Declaration of Helsinki. Written informed consent was obtained from all participants.
The target sample size was set to 40 patients to obtain data of 20 patients experiencing disease flare for intensive analyses of clinical, imaging, and biomarker changes estimating a 50% flare rate. Patient recruitment was started in November 2014 and closed in January 2018 with the enrolment of 36 patients.
Clinical assessments
We obtained the following medical information from medical records: age, sex, height, weight, disease duration from the onset of symptoms to enrolment, duration of bDMARD treatment to be discontinued, remission duration, Steinbrocker radiographic stage, anti-CCP, rheumatoid factor, MMP-3, and the treatment for RA. After enrolment in this study, the patients were examined every 2–3 months for TJC28, SJC28, PtGA, PhGA, HAQ-DI, blood tests for ESR, serum CRP, and MMP-3 as well as plasma storage for future examination of cytokine and soluble cytokine receptor concentrations, and also underwent US examination of the 40 joints.
US examination
A Xario (Toshiba Medical Systems, Tochigi, Japan) US machine equipped with a multifrequency linear array probe (7–14 MHz) was used. The PD settings were as follows: PD pulse repetition frequency, 16.5 kHz (flow range, 3.8 cm/s); Doppler frequency, 6.1 MHz, and low wall filter. Colour gain was set just below the level at which noise appeared. The US examination was performed according to the EULAR guidelines for musculoskeletal US in rheumatology44,45 by rheumatologists and ultrasonographers certified by the Japan College of Rheumatology. These examiners evaluated 40 of the joints including the bilateral shoulders, elbows wrists, metacarpophalangeal joints, thumb interphalangeal joints, second through fifth finger proximal interphalangeal joints, knees, ankles, and metatarsophalangeal joints using longitudinal and transverse scans, without knowledge of the other medical information of the patients.
The US examiners performed the final scoring of the recorded US findings according to the OMERACT definitions46. Briefly, the GS was graded semiquantitatively from 0 to 3 (0 = absent, 1 = mild, 2 = moderate, and 3 = marked) in a combined measure of synovial hypertrophy and fluid retention of the articular recess. The intra-articular PD signals were also graded on a 0–3 scale, and the total joint US score was determined by summing all GS and PD scores for each patient.
Measurement of plasma concentration of cytokines and soluble cytokine receptors
Plasma was stored at − 80 °C until measurement. Plasma concentrations of interleukin (IL)-1β, IL-2, IL-6, IL-8, IL-10, interferon gamma, TNF, granulocyte–macrophage colony stimulating factor, vascular endothelial growth factor, sTNFR1, sTNFR2, and soluble IL-6 receptor were measured by electrochemiluminescence assay with the Ultra-Sensitive Kit (Meso Scale Discovery, Rockville, MD, USA) according to the manufacturer’s protocol47.
Statistical analyses
The statistical analyses were performed using JMP Pro (version 14.2, SAS Institute Japan Ltd., Tokyo, Japan). Continuous variables are presented as the median and interquartile range (IQR) and were analysed using the Mann–Whitney U test. Binomial data were compared between two groups using Fisher’s exact test. Kaplan–Meier analysis and log-rank tests were used for the comparison of survival curves between the groups. The correlation coefficient (r) was determined by Spearman’s rank test. Logistic regression analyses followed by ROC curve analyses were conducted for the prediction of RA flare based on the baseline biomarkers. p-values < 0.05 were considered statistically significant.
References
Smolen, J. S. et al. EULAR recommendations for the management of rheumatoid arthritis with synthetic and biological disease-modifying antirheumatic drugs: 2019 update. Ann. Rheum. Dis. 79, 685–699 (2020).
Felson, D. T. et al. American College of Rheumatology/European League Against Rheumatism provisional definition of remission in rheumatoid arthritis for clinical trials. Ann. Rheum. Dis. 70, 404–413 (2011).
Smolen, J. S. et al. A simplified disease activity index for rheumatoid arthritis for use in clinical practice. Rheumatology 42, 244–257 (2003).
Aletaha, D. et al. Difference in disease activity measures in patients with rheumatoid arthritis who achieved DAS, SDAI, or CDAI remission but not Boolean remission. Semin. Arthritis Rheum. 50, 276–284 (2020).
Schoels, M., Alasti, F., Smolen, J. S. & Aletaha, D. Evaluation of newly proposed remission cut-points for disease activity score in 28 joints (DAS28) in rheumatoid arthritis patients upon IL-6 pathway inhibition. Arthritis Res. Ther. 19, 155 (2017).
Ito, H. et al. Global assessments of disease activity are age-dependent determinant factors of clinical remission in rheumatoid arthritis. Semin. Arthritis Rheum. 47, 310–314 (2017).
Einarsson, J. T. et al. Prevalence of sustained remission in rheumatoid arthritis: Impact of criteria sets and disease duration, a Nationwide Study in Sweden. Rheumatology 58, 227–326 (2019).
van Steenbergen, H. W., da Silva, J. A. P., Huizinga, T. W. J. & van der Helm-van Mil, A. H. M. Preventing progression from arthralgia to arthritis: Targeting the right patients. Nat. Rev. Rheumatol. 14, 32–41 (2018).
Tanaka, Y. et al. RRR study investigators. Discontinuation of infliximab after attaining low disease activity in patients with rheumatoid arthritis: RRR (remission induction by Remicade in RA) study. Ann. Rheum. Dis. 69, 1286–1291 (2010).
Klarenbeek, N. B. et al. Discontinuing treatment in patients with rheumatoid arthritis in sustained clinical remission: Exploratory analyses from the BeSt study. Ann. Rheum. Dis. 70, 315–319 (2011).
Detert, J. et al. Induction therapy with adalimumab plus methotrexate for 24 weeks followed by methotrexate monotherapy up to week 48 versus methotrexate therapy alone for DMARD-naïve patients with early rheumatoid arthritis: HIT HARD, an investigator-initiated study. Ann. Rheum. Dis. 72, 844–850 (2013).
Smolen, J. S. et al. Adjustment of therapy in rheumatoid arthritis on the basis of achievement of stable low dose activity with adalimumab plus methotrexate or methotrexate alone: The randomized controlled OPTIMA trial. Lancet 383, 321–332 (2014).
Kurasawa, T. et al. Addition of another disease-modifying anti-rheumatic drug to methotrexate reduces the flare rate within two years after infliximab discontinuation in patients with rheumatoid arthritis: An open, randomized, controlled trial. Mod. Rheumatol. 24, 561–566 (2014).
Nishimoto, N. et al. Drug free REmission/low disease activity after cessation of tocilizumab (Actemura) Monotherapy (DREAM) study. Mod. Rheumatol. 24, 17–25 (2014).
Tanaka, Y. et al. Discontinuation of adalimumab after achieving remission in patients with established rheumatoid arthritis: 1-year outcome of the HONOR study. Ann. Rheum. Dis. 74, 389–395 (2015).
Takeuchi, T. et al. Biologic-free remission of established rheumatoid arthritis after discontinuation of abatacept: A prospective, multicentre, observational study in Japan. Rheumatology (Oxford) 54, 683–691 (2015).
Emery, P. et al. Evaluating drug-free remission with abatacept in early rheumatoid arthritis: Results from the phase 3b, multicentre, randomised, active-controlled AVERT study of 24 months, with a 12-month, double-blind treatment period. Ann. Rheum. Dis. 74, 19–26 (2015).
Tanaka, Y. et al. Adalimumab discontinuation in patients with early rheumatoid arthritis who were initially treated with methotrexate alone or in combination with adalimumab: 1 year outcomes of the HOPEFUL-2 study. RMD Open. 2, e000189 (2016).
Haschka, J. et al. Relapse rates in patients with rheumatoid arthritis in stable remission tapering or stopping antirheumatic therapy: Interim results from the prospective randomised controlled RETRO study. Ann. Rheum. Dis. 75, 45–51 (2016).
Fautrel, B. et al. Step-down strategy of spacing TNF-blocker injections for established rheumatoid arthritis in remission: Results of the multicentre non-inferiority randomised open-label controlled trial (STRASS: Spacing of TNF-blocker injections in Rheumatoid ArthritiS Study). Ann. Rheum. Dis. 75, 59–67 (2016).
Yamanaka, H. et al. Discontinuation of etanercept after achievement of sustained remission in patients with rheumatoid arthritis who initially had moderate disease activity—results from the ENCOURAGE study, a prospective, international, multicenter randomized study. Mod. Rheumatol. 26, 651–661 (2016).
van Vollenhoven, R. F. et al. Full dose, reduced dose or discontinuation of etanercept in rheumatoid arthritis. Ann. Rheum. Dis. 75, 52–58 (2016).
Atsumi, T. et al. Clinical benefit of 1-year certolizumab pegol (CZP) add-on therapy to methotrexate treatment in patients with early rheumatoid arthritis was observed following CZP discontinuation: 2-year results of the CZP discontinuation: 2-year results of the C-OPERA study, a phase III randomised trial. Ann. Rheum. Dis. 76, 1348–1356 (2017).
Kaneko, Y. et al. Tocilizumab discontinuation after attaining remission in patients with rheumatoid arthritis who were treated with tocilizumab alone or in combination with methotrexate: Results from a prospective randomised controlled study (the second year of the SURPRISE study). Ann. Rheum. Dis. 77, 1268–1275 (2018).
Tanaka, Y. et al. The effect of deep or sustained remission on maintenance of remission after dose reduction or withdrawal of etanercept in patients with rheumatoid arthritis. Arthritis Res. Ther. 21, 164 (2019).
Tanaka, Y. et al. Sustained discontinuation of infliximab with a rising-dose strategy after obtaining remission in patients with rheumatoid arthritis: The RRRR study, a randomised controlled trial. Ann. Rheum. Dis. 79, 94–102 (2020).
Prevoo, M. L. et al. Modified disease activity scores that include twenty-eight-joint counts: Development and validation in a prospective longitudinal study of patients with rheumatoid arthritis. Arthritis Rheum. 38, 44–48 (1995).
Kameda, H. et al. Japan College of Rheumatology guideline for the use of methotrexate in patients with rheumatoid arthritis. Mod. Rheumatol. 29, 31–40 (2019).
van der Maas, A. et al. Construct and criterion validity of several proposed DAS28-based rheumatoid arthritis flare criteria: An OMERACT cohort validation study. Ann. Rheum. Dis. 72, 1800–1805 (2013).
Aletaha, D. & Smolen, J. S. Achieving clinical remission for patients with rheumatoid arthritis. JAMA 321, 457–458 (2019).
Schett, G. et al. Tapering biologic and conventional DMARD therapy in rheumatoid arthritis: Current evidence and future directions. Ann. Rheum. Dis. 75, 1428–1437 (2016).
Tweehuysen, L. et al. Little evidence for usefulness of biomarkers for predicting successful dose reduction or discontinuation of a biologic agent in rheumatoid arthritis. A systematic review. Arthritis Rheumatol. 69, 301–308 (2017).
Rech, J. et al. Prediction of disease relapse by multibiomarker disease activity and autoantibody status in patients with rheumatoid arthritis on tapering DMARD treatment. Ann. Rheum. Dis. 75, 1637–1644 (2016).
Eastman, P. S. et al. Characterization of a multiplex, 12-biomarker test for rheumatoid arthritis. J. Pharm. Biomed. Anal. 70, 415–424 (2012).
Levine, S. J. Molecular mechanisms of soluble cytokine receptor generation. J. Biol. Chem. 283, 14177–14181 (2008).
Guo, G.-H., Dong, J., Yuan, X.-H., Dong, Z.-N. & Tian, Y.-P. Clinical evaluation of the levels of 12 cytokines serum/plasma under various storage conditions using evidence biochip arrays. Mol. Med. Rep. 7, 775–780 (2013).
Witkowska, A. et al. Interleukin 2 as a potential cancer marker in patients after kidney transplantation. Ann. Agric. Environ. Med. 22, 320–324 (2015).
Alnek, K. et al. Increased blood levels of growth factors, proinflammatory cytokines, and Th17 cytokines in patients with newly diagnosed type 1 diabetes. PLoS ONE 10, e0142976 (2015).
Baker, K. F. et al. Predicting drug-free remission in rheumatoid arthritis: A prospective interventional cohort study. J. Autoimmun. 105, 102298 (2019).
Katagiri, T. et al. JunB plays a crucial role in development of regulatory T cells by promoting IL-2 signaling. Mucosal. Immunol. 12, 1104–1117 (2019).
Rosenzwajg, M. et al. Immunological and clinical effects of low-dose interleukin-2 across 11 autoimmune diseases in a single, open clinical trial. Ann. Rheum. Dis. 78, 209–217 (2019).
Tasaki, S. et al. Multi-omics monitoring of drug response in rheumatoid arthritis in pursuit of molecular remission. Nat. Commun. 9, 2755 (2018).
Aletaha, D. et al. 2010 rheumatoid arthritis classification criteria: An American College of Rheumatology/European League Against Rheumatism collaborative initiative. Arthritis Rheum. 62, 2569–2581 (2010).
Backhaus, M. et al. Guidelines for musculoskeletal ultrasound in rheumatology. Ann. Rheum. Dis. 60, 641–649 (2001).
Möller, I. et al. The 2017 EULAR standardised procedures for ultrasound imaging in rheumatology. Ann. Rheum. Dis. 76, 1974–1979 (2017).
Wakefield, R. J. et al. Musculoskeletal ultrasound including definitions for ultrasonographic pathology. J. Rheumatol. 32, 2485–2487 (2005).
Nishina, N. et al. Baseline levels of soluble interleukin-6 receptor predict clinical remission in patients with rheumatoid arthritis treated with tocilizumab: Implications for molecular targeted therapy. Ann. Rheum. Dis. 73, 945–947 (2014).
Acknowledgements
The authors thank Editage Japan for editing the manuscript.
Author information
Authors and Affiliations
Contributions
H.K. conceptualized and designed the study, and wrote the draft. T.K., Y.T., Y.I., S.T., H.I., and K.M. collected clinical data from patients with RA. T.O. and A.H. performed the ultrasound examinations and collected those data. H.K. and T.O. performed the statistical analyses. All authors reviewed and approved the manuscript.
Corresponding author
Ethics declarations
Competing interests
This work was partly supported by JSPS KAKENHI Grant Number JP15K09535, Health and Labour Sciences Research Grants for research on intractable diseases (The Research Team for Autoimmune Diseases) from the Ministry of Health, Labour and Welfare of Japan for H.K. H.K. has received consulting fees, speaking fees, and/or honoraria from AbbVie G.K., Asahi Kasei Pharma, Astellas Pharma Inc., Bristol-Myers Squibb, Chugai Pharmaceutical Co. Ltd., Eisai Co. Ltd., Eli Lilly Japan K.K., Gilead Sciences, Janssen Pharmaceutical K.K., Mitsubishi Tanabe Pharma, Novartis Pharma K.K., and Sanofi Pharma; and has received research grants from AbbVie G.K., Asahi Kasei Pharma, Astellas Pharma Inc., Chugai Pharmaceutical Co. Ltd., Eisai Co. Ltd., Mitsubishi Tanabe Pharma, Novartis Pharma K.K., and Sanofi Pharma. T.O. has received honoraria from AbbVie G.K. A.H., T.K., Y.T., Y.I., S.T., H.I. and K.M. declare no potential conflict of interest.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kameda, H., Hirata, A., Katagiri, T. et al. Prediction of disease flare by biomarkers after discontinuing biologics in patients with rheumatoid arthritis achieving stringent remission. Sci Rep 11, 6865 (2021). https://doi.org/10.1038/s41598-021-86335-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-86335-7
This article is cited by
-
Prevalence and predictors of sustained remission/low disease activity after discontinuation of induction or maintenance treatment with tumor necrosis factor inhibitors in rheumatoid arthritis: a systematic and scoping review
Arthritis Research & Therapy (2023)
-
High prevalence of rheumatoid arthritis and its risk factors among Tibetan highlanders living in Tsarang, Mustang district of Nepal
Journal of Physiological Anthropology (2022)
-
Serum level of IFNβ distinguishes early from late relapses after biologics withdrawal in rheumatoid arthritis
Scientific Reports (2022)
-
Demographic and Clinical Characteristics of Patients with Sustained and Switching Treatments Using Biological and Targeted Synthetic Disease-Modifying Antirheumatic Drugs: A Multicenter, Observational Cross-Sectional Study for Rheumatoid Arthritis
Rheumatology and Therapy (2022)
-
A novel multi-biomarker combination predicting relapse from long-term remission after discontinuation of biological drugs in rheumatoid arthritis
Scientific Reports (2021)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.