Abstract
The separation of biomarkers from blood is straightforward in most molecular biology laboratories. However, separation in resource-limited settings, allowing for the successful removal of biomarkers for diagnostic applications, is not always possible. The situation is further complicated by the need to separate hydrophobic signatures such as lipids from blood. Herein, we present a microfluidic device capable of centrifugal separation of serum from blood at the point of need with a system that is compatible with biomarkers that are both hydrophilic and hydrophobic. The cross-flow filtration device separates serum from blood as efficiently as traditional methods and retains amphiphilic biomarkers in serum for detection.
Similar content being viewed by others
Introduction
The separation of serum from whole blood is a necessary first step in many clinical diagnostic blood tests, since serum contains important biomarkers, whether autogenic or pathogenic, for disease diagnosis and monitoring1,2,3. Our focus is on the detection of amphiphilic bacterial biomarkers that are released into the host’s blood stream rapidly after infection4,5,6,7,8. Early detection and specific treatment of bacterial infections is necessary to help prevent the spread of antimicrobial resistance, save lives, and reduce the chances of outbreaks. Ideally, diagnosis will occur at the point of need and provide rapid intervention solutions. The development of rapid, simple, automated, safe, and inexpensive processing of blood samples can therefore benefit many diagnostic assays.
We are working towards a universal diagnostic strategy for all bacterial pathogens, including the development of novel assays to quickly detect biomarkers indicative of bacterial infection9. Our universal bacterial sensing strategy mimics innate immune recognition in the laboratory, facilitating diagnosis of all bacterial infection from a single clinical sample: blood. The bacterial biomarkers targeted by our assays are the same as those targeted by our human innate immune response, and are most often lipidated sugars (lipoglycans or glycolipids, such as lipopolysaccharide, lipoteichoic acid, and lipoarabinomannan). Previous work from our laboratory and others has shown that the amphiphilic biochemistry of these biomarkers causes them to be sequestered by host lipoprotein carriers, including high- and low-density lipoproteins (HDL and LDL)4,6,7,9,10. Because of this sequestration, it is necessary to liberate the amphiphilic biomarkers from their lipoprotein carriers in order to enable sensitive measurement. Detection can then occur via enzyme-linked immunosorbent assays (ELISA’s), waveguide-based biosensors5,6,8,10, or other methods9.
The focus of the work presented in this manuscript is the separation of serum from blood within a microfluidic device that preserves the integrity of relevant amphiphilic biomarkers present in serum. Our current sample processing method, while reliable, requires trained personnel and a multi-step laboratory procedure11. For use in a point-of-care setting, sample preparation should be automated in order to save time and ensure user safety, while preserving sample quality12. The platform must be able to process small volumes of whole blood, have a low cost of production, and offer minimal loss of sample integrity during processing. It is also beneficial to have the ability to integrate additional processing steps as dictated by the specific application.
While there have been many reported microfluidic devices that separate serum from blood, most to our knowledge have emphasized the preservation of protein and nucleic acid signatures12,13,14,15,16,17,18,19,20,21,22,23. Lipidic and amphiphilic biomarkers present a unique challenge, as they tend to adhere to many different surfaces, including certain plastics and dialysis membranes.
Centrifugal microfluidics is a promising area of research for the automation of a variety of processes, including biological assays and sample preparation24,25. The field is especially appealing for point-of-care and deployable devices, due to the fact that minimal instrumentation is needed, and the centrifugal force present is inherently effective for density-based separations25. This applies to our system, as the extraction of serum from blood is essentially a phase separation. We have applied the concepts of centrifugal microfluidics in order to develop a cross-flow filtration scheme for the gentle separation of serum from blood24,26.
During the process of cross-flow filtration, the sample passes tangentially across a filter, which is achieved via the centrifugal force acting on the platform. Components smaller than the membrane’s pores are driven through the filter as pressure increases, while larger components pass over the membrane surface27. In contrast, dead-end filtration can result in clumping of particles that clog the filter (Fig. 1). Cross-flow filtration decreases the chances of clogging, which in turn decreases the chances of red blood cell (RBC) lysis. Lysis of RBCs is of concern, since the release of hemoglobin (a fluorescent molecule) from the cells can interfere with fluorescence-based detection methods28,29,30.
Based on these observations, we chose to develop a cross-flow centrifugal microfluidic platform for the separation of serum from whole blood that is compatible with the biochemistry of amphiphilic biomarkers. While this is not the first time a cross-flow filtration method has been integrated into a centrifugal microfluidic chip, it is the first to our knowledge to specifically preserve amphiphilic molecules within serum31,32,33,34. The design was optimized to purify serum to commercial standards, as validated by performing cell counts on all samples. Materials used for the fabrication of the centrifugal platform were compatible with our sample processing criteria, as confirmed by testing samples from the device on our waveguide-based optical biosensor for the retention of amphiphilic biomarkers of interest6,8,10,35,36. This development greatly simplifies the sample processing requirements for our biosensing assays and facilitates the transition of such technologies to the point of need. In addition, this method can be applied to other detection techniques that require the separation and preservation of serum from whole blood, including in resource limited settings, inexpensively and rapidly.
Working principle
The device consists of multiple chambers stacked on top of each other, separated by a membrane, according to the layout in Fig. 2a,b. Four separation units are present on the centrifugal disc (Fig. 2c), enabling multiple simultaneous experiments on one chip, which could be used for various assays or replicates of the same sample. The following steps take place within each separation unit (Fig. 2a):
Step 1: Blood is introduced into the platform though the sample inlet. The ports are sealed, and the disc is placed on a motor to impart centrifugal force onto the sample at a given revolutions per minute (RPM). The centrifugal force causes the blood to flow away from the center of rotation. RBCs cluster toward the bottom of the sample reservoir in pellet trap #1 due to their density.
Step 2: As the pressure increases in the sample reservoir, serum is able to flow through the embedded membrane, while RBCs are largely prevented from flowing through due to their size. A small number of RBCs may squeeze through the pores of the membrane.
Step 3: Excess RBCs that went through the membrane are caught in pellet trap #2. As RBCs accumulate in pellet trap #2, the serum flows up into the serum reservoir, passing through another membrane section that serves as a secondary filtration step for RBCs. The serum is then collected through the serum outlet.
Our initial cross-flow filtration design included only one pellet trap, but we observed that some RBCs were able to get through the membrane. We realized we could easily integrate another filtration step, without changing our fabrication process, by adding another pellet trap to the design.
Methods
Device fabrication
The cross-flow filtration platform consists of five structural layers of plastic and one thin plastic membrane layer. The device was fabricated using a rapid prototyping method involving laser-based micropatterning and lamination. A pressure-sensitive adhesive (91,022, 3 M) was used to facilitate the lamination process. Layer schematics were drawn using SolidEdge10 2D drafting software. Alignment holes were included on all layers for assembly on a jig. The layers were cut using a CO2 laser cutter (M360, Universal Laser Systems) from stock cast acrylic (McMaster Carr Supply Company), polycarbonate (McMaster Carr Supply Company), and membrane sheets (Sterlitech Corporation). After cutting, the plastic layers were cleaned by bath sonication in water with dish soap for 15 min followed by a manual wash by wiping with isopropyl alcohol.
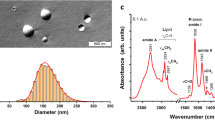
The membrane layers are Sterlitech Corporation’s track-etched hydrophilic polycarbonate with 5 µm pores. The polycarbonate membrane was coated by the manufacturer with polyvinylpyrrolidone (PVP) to ensure hydrophilicity37. The membrane sheets are reported by the manufacturer to be between 3 and 24 µm thick, making them delicate to work with37,38. In order to obtain reproducible separation by the membranes, it was important to integrate suspended membranes that are flat. We have developed a method for membrane integration, described in the Electronic Supplementary Information 1 (ESI), which consistently produces a surface that is free from visible indentations or imperfections.
Device testing and optimization
Device functionality was verified in a series of systematic experiments that determined ideal RPM (from 3500 to 5000, tested in 500 RPM increments), time (from 2 to 5 min, tested in 1 min increments), membrane type (polycarbonate and polyester; 2, 3, and 5 µm pore sizes), and geometric design parameters (pellet trap sizes, tested in 0.5 mm height increments) for phase separations. An example of these systematic testing schemes is described in the ESI. In order to test different conditions, the disc was placed on the jig, and 90 µL of whole sheep’s blood was pipetted into each inlet hole. The inlets were designed to be the same diameter as the pipette tip in order to create a seal and prevent leakage. A one-sided custom polycarbonate tape was aligned on top of the disc to seal all ports and prevent the escape of fluids during processing. A microcentrifuge (SCI-12 High Speed Personal Micro-Centrifuge, Scilogex) was used to test different RPM and time profiles. A central hole (Fig. 2c) was cut into the microfluidic disc to fit over the rotor, and the cap from the microcentrifuge was securely fastened over the disc.
Blood/serum separation efficiency
Serum samples from the microfluidic chip were visually inspected for hemolysis by using the CDC’s hemolysis reference palette39. Serum purity, defined as the percentage of cells removed from whole blood, was determined by using a TC20 Automated Cell Counter (Bio-Rad Laboratories) to compare the number of cells present in whole blood (sheep; Thermo Fisher Scientific) before separation on the microfluidic device to the number of cells present in serum after separation was complete. Serum purity was calculated using the following formula40: serum purity (SP) (%):
Cell counts were also performed on commercially-available sheep serum produced by ultracentrifugation (Thermo Fisher Scientific), and serum separated from whole blood in our lab by traditional benchtop methods, for comparison. Results were analyzed by a Student’s t test for significance.
Biomarker retention
We validated the ability of our microfluidic device to retain serum biomarkers of interest by comparing the efficacy of the process against the benchtop method developed by our team. The benchtop sample processing method consists of two major steps: (1) the separation of serum from blood on a microcentrifuge; and (2) the isolation of amphiphilic biomarkers from serum using a chloroform/methanol extraction5,6,8,10,36,41,42. In this work, we sought to automate the first step of sample processing on a microfluidic chip, and ensure that biomarkers of interest were retained in the sample and not adsorbed to the plastic device materials.
Initial biomarker retention experiments were performed on the Los Alamos National Laboratory’s waveguide-based optical biosensor, which is used for the detection of biomarkers from Gram-negative, -positive, and -indeterminate bacteria6,8,10,36. The technology is described in detail elsewhere6,8,10,35,36,41.
The ability to retain and subsequently detect lipoarabinomannan (LAM), the virulence factor associated with Mycobacterium tuberculosis, was chosen as an assessment of biomarker retention. LAM is an amphiphilic biomarker, and previous work has shown that the antigen associates with HDL7,43,44,45,46. We have evaluated the benchtop sample processing method for the extraction of carrier-associated LAM, followed by its detection on the waveguide biosensor using a tailored method called membrane insertion6,36,46. Herein, we compared benchtop and microfluidic methods by measuring the sensitivity of detection of LAM in serum.
In order to test biomarker retention, whole blood was spiked with LAM to a concentration of 0.5 µM and incubated overnight at 4 °C. This concentration was chosen based on previous work that showed the linear range for LAM detection on the optical biosensor is between 0.2 and 1.0 µM46. The next day, serum was separated from blood using either the microfluidic device or by traditional benchtop separation, depending on the assay. For extractions using the microfluidic device, 90 µL blood was pipetted into each inlet hole, and the disc was centrifuged at 4500 RPM for 3 min. This RPM and time combination was optimized as described earlier. For traditional methods, 500 µL whole blood was pipetted into a microcentrifuge tube and centrifuged at 4500 RPM for 3 min. The serum from each method of separation was analyzed by cell counting, and sample processing was finished by benchtop methods in both cases. 120 µL of serum was mixed by pipetting with 150 µL chloroform and 300 µL methanol in low-retention microcentrifuge tubes. The mixture was spun at 5500 RPM for 1 min on a microcentrifuge, and the supernatant was discarded. The pellet containing biomarkers of interest was re-suspended in 120 µL of 1X PBS, which was injected into the flow cell of the waveguide and incubated for 45 min at room temperature. After incubation, the flow cell was washed, and the specific signal was measured on the waveguide-based optical biosensor. Complete details for the waveguide-based assays can be found in the ESI.
Results
Device functionality
We found that spinning the disc at 4500 RPM (1418 RCF) for 3 min yielded serum with the least amount of RBCs remaining in it. It is speculated that this RPM/time combination provided enough force to drive the serum through the device, but not too much force to cause hemolysis. Three minutes provided enough time for a significant amount of serum to flow through to the serum reservoir, which could then be removed for analysis. Sterlitech’s polycarbonate membrane with 5 µm pores was the most effective at filtering out RBCs. Our design includes two pellet traps for RBC collection (Fig. 2). Pellet trap heights of 5 mm and 2 mm for pellet trap #1 and #2, respectively, were found to be the most effective. A two-step filtration design was determined to be more successful at separating serum from blood when compared to a one-step method, as described in the Working Principle section. Figure 3 shows cross-sections of the one-step vs. two-step filtration designs and the resulting phase separations. An example of systematic testing parameters with results can be found in the ESI.
Schematics of one-step (A) vs. two-step (B) cross-flow filtration, with corresponding photos of phase separations on the microfluidic device; (A) the one-step filtration method was ineffective at separating a large fraction of blood cells from serum; (B) the two-step filtration method was successful at separating serum from blood.
Serum purity
Based on the CDC’s hemolysis reference palette, serum samples processed on the microfluidic chip contained less than 100 mg/dL of hemoglobin, which is the recommended value for serological testing39. We compared the RBC count of serum separated on the microfluidic device to serum separated by traditional centrifugation and to commercially-available serum. The serum processed on our microfluidic platform had a statistically significantly lower cell count (P = 0.0179 for microfluidics vs. benchtop; P = 0.0128 for microfluidics vs. commercial serum). A bar graph of cell counts for whole blood compared to different methods of separating serum is shown in Fig. 4. Serum purity was calculated for benchtop methods of separation and for the microfluidic separation. Both methods yielded a high percentage of cells removed from whole blood, greater than 99.99%.
We determined that our device is suitable for blood/serum separation, a common first step of many sample processing methods. The serum processed on the microfluidic device had a lower cell count than either the serum processed using the benchtop separation method or commercially-available serum, which indicates higher serum purity.
Biomarker retention
We validated biomarker retention for blood separated on the microfluidic chip and compared the results to our benchtop sample processing method. After serum from the microfluidic device was determined to have a significantly lower cell count (Fig. 4) than serum from the benchtop or commercially-available serum, we further validated the device by testing for biomarker retention in the sample. LAM was spiked in whole blood at 0.5 μM before separating serum from blood on the microfluidic device. Blood from the same aliquot was used for benchtop blood/serum separation in microcentrifuge tubes. After separation, the serum was analyzed on our waveguide-based optical biosensor, as described in the Experimental Section. There was no statistically significant difference between LAM levels in serum processed on the microfluidic device vs. by benchtop methods (P = 0.9392), indicating that the microfluidic device preserves amphiphilic biomarkers present in serum as effectively as benchtop processing methods, and the device’s materials are suitable for our application. A comparison is shown in Fig. 5.
Signal intensity (n = 3) of LAM from whole sheep’s blood separated on the microfluidic device vs. benchtop methods. Higher intensity indicates higher concentration of biomarker retained in the serum sample. There was no significant difference between signals, indicating that our cross-flow filtration chip is suitable for the separation of serum from blood and subsequent detection of amphiphilic biomarkers. The fact that serum processed on the microfluidic disc yielded a similar signal intensity indicates that the microfluidic device preserves amphiphilic biomarkers present in serum as effectively as benchtop processing methods.
Discussion
We have integrated a multi-stage cross-flow filtration system into a centrifugal microfluidic platform to perform blood/serum separation. To our knowledge, this is the first cross-flow based microfluidic device capable of the separation of serum from blood with a documented ability to preserve lipidic biomarkers with the same efficiency as benchtop processing. Serum processed on our device contained fewer RBCs when compared to serum separated using benchtop methods and to commercially-available serum. The serum separated on our microfluidic chip was over 99.99% pure. There was no significant loss of signal for detection of the model biomarker of interest, LAM, when compared to benchtop methods of separation, indicating the suitability of our device for amphiphilic and lipidic signature retention.
This method of blood/serum separation offers several advantages. The platform requires only 90 µL of whole blood, which reduces invasiveness and is of importance when working with potentially dehydrated patients in remote areas of the world. This amount of blood could be collected by finger prick, which would eliminate the need for a trained phlebotomist and greatly reduce the cost per test if used at the point-of-care. It is simple to manufacture, disposable, and does not rely on pumps or valves for fluidic movement. It does not interfere with amphiphile detection as validated on our optical biosensor, nor does it require the dilution of blood. The chip itself is modular, as shown by the decision to use two pellet traps instead of one. This highlights the ease with which the design can be adapted for other phase-separation applications, without changing the manufacturing process we developed.
In this work, we have automated the first major step of our specific sample processing method, the separation of serum from blood. The platform is a promising design for the complete automation of sample processing at the point-of-care, whether for bacterial biomarkers or other lipidic signatures, which we plan to do in future work. However, our design has potential applications to human health in its current configuration. Any assays that require the separation of serum from blood could use this device to do so. For example, the common tests for cholesterol and triglycerides are typically performed directly on human serum samples. Since we have shown that our device does not interfere with the detection of lipids in serum, it could be used for this application.
The need for laboratory infrastructure for lipid handling and separation, the loss of lipidic signatures during protein processing, and the inability to process lipidic samples in field conditions remain major challenges. We plan to further develop our engineering capabilities in order to simplify sample collection, storage, processing, and measurement for lipidic signatures in biological matrices in the future.
Data availability
The datasets generated during and/or analyzed used in this manuscript are available from the corresponding author on reasonable request.
References
Song, Y. et al. Point-of-care technologies for molecular diagnostics using a drop of blood. Trends Biotechnol. 32, 132–139 (2014).
Mielczarek, W. S., Obaje, E. A., Bachmann, T. T. & Kersaudy-Kerhoas, M. Microfluidic blood plasma separation for medical diagnostics: Is it worth it?. Lab Chip 16, 3441–3448 (2016).
Sun, K., Oh, H., Emerson, J. F. & Raghavan, S. R. A new method for centrifugal separation of blood components: Creating a rigid barrier between density-stratified layers using a UV-curable thixotropic gel. J. Mater. Chem 22, 2378–2382 (2012).
Stromberg, L. R., Mendez, H. M. & Mukundan, H. Detection methods for lipopolysaccharides: Past and present in Escherichia coli—recent advances on physiology, pathogenesis and biotechnological applicationsrecent advances on physiology, pathogenesis and biotechnological applications 141–166 (IntechOpen, London, 2017).
Kubicek-Sutherland, J. Z. et al. Direct detection of bacteremia by exploiting host-pathogen interactions of lipoteichoic acid and lipopolysaccharide. Sci. Rep. 9, 6203 (2019).
Kubicek-sutherland, J. Z., Hengartner, A. C. & Mukundan, H. Membrane insertion for direct detection of lipoteichoic acid. Trans. Mat. Res. Soc. Jpn. 42, 101–105 (2017).
Sakamuri, R. M. et al. Association of lipoarabinomannan with high density lipoprotein in blood: Implications for diagnostics. Tuberculosis 93, 301–307 (2013).
Mukundan, H. et al. Rapid detection of Mycobacterium tuberculosis biomarkers in a sandwich immunoassay format using a waveguide-based optical biosensor. Tuberculosis 92, 407–416 (2012).
Kubicek-Sutherland, J. Z., Vu, D. M., Mendez, H. M., Jakhar, S. & Mukundan, H. Detection of lipid and amphiphilic biomarkers for disease diagnostics. Biosensors 7, 25 (2017).
Noormohamed, A. et al. Detection of lipopolysaccharides in serum using a waveguide-based optical biosensor. SPIE BiOS 10072, 20 (2017).
Mukundan, H. et al. Immunoassays for the differentiation of bacterial pathogens in human serum. US20170307604A1 (2017).
Hin, S. et al. Membrane-based sample inlet for centrifugal microfluidic cartridges. Microelectron. Eng. 187–188, 78–83 (2018).
Phurimsak, C., Tarn, M. D. & Pamme, N. Magnetic particle plug-based assays for biomarker analysis. Micromachines 7(5), 77 (2016).
Kuo, J. N. & Chen, X. F. Plasma separation and preparation on centrifugal microfluidic disk for blood assays. Microsyst. Technol. 21, 2485–2494 (2015).
Dimov, I. K. et al. Stand-alone self-powered integrated microfluidic blood analysis system (SIMBAS). Lab Chip 11, 845–850 (2011).
Lee, B. S. et al. A fully automated immunoassay from whole blood on a disc. Lab Chip 9, 1548–1555 (2009).
Browne, A. W., Ramasamy, L., Cripe, T. P. & Ahn, C. H. A lab-on-a-chip for rapid blood separation and quantification of hematocrit and serum analytes. Lab Chip 11, 2440–2446 (2011).
Valera, E. et al. A microfluidic biochip platform for electrical quantification of proteins. Lab Chip 18, 1461–1470 (2018).
Wang, J. et al. A self-powered, one-step chip for rapid, quantitative and multiplexed detection of proteins from pinpricks of whole blood. Lab Chip 10, 3157–3157 (2010).
Homsy, A. et al. Development and validation of a low cost blood filtration element separating plasma from undiluted whole blood. Biomicrofluidics 6, 12804–128049 (2012).
Kim, C.-J. et al. Fully automated, on-site isolation of cfDNA from whole blood for cancer therapy monitoring. Lab Chip 18, 1320–1329 (2018).
Liu, W. et al. A fully-integrated and automated testing device for PCR-free viral nucleic acid detection in whole blood. Lab Chip 18, 1928–1935 (2018).
Tripathi, S., Kumar, Y. V. B., Agrawal, A., Prabhakar, A. & Joshi, S. S. Microdevice for plasma separation from whole human blood using bio-physical and geometrical effects. Sci. Rep. 6, 26749 (2016).
Gorkin, R. et al. Centrifugal microfluidics for biomedical applications. Lab Chip 10, 1758–1758 (2010).
Tang, M., Wang, G., Kong, S. K. & Ho, H. P. A review of biomedical centrifugal microfluidic platforms. Micromachines 7, 20 (2016).
Sano, M. B. & Davalos, R. V. Microfluidic Techniques for the Detection, Manipulation and Isolation of Rare Cells in MEMS for Biomedical Applications 337–357 (Woodhead Publishing Limited, Cambridge, 2012).
Bowen, W. R. & Jenner, F. Theoretical descriptions of membrane filtration of colloids and fine particles: An assessment and review. Adv. Colloid Interface Sci. 56, 141–200 (1995).
Anand, S. & Sujatha, N. Fluorescence quenching effects of hemoglobin on simulated tissue phantoms in the UV–Vis range. Meas. Sci. Technol. 23, 25502–25506 (2012).
Moneriz, C., Marín-García, P., Bautista, J. M., Diez, A. & Puyet, A. Haemoglobin interference and increased sensitivity of fluorimetric assays for quantification of low-parasitaemia Plasmodium infected erythrocytes. Malar J. 8, 279 (2009).
Simoni, J., Simoni, G., Lox, C. D., Prien, S. D. & Shires, G. T. Hemoglobin interference with an enzyme-linked immunosorbent assay for the detection of tumor necrosis factor-alpha. Anal. Chim. Acta 313, 1–14 (1995).
Kim, T.-H. et al. FAST: Size-selective, clog-free isolation of rare cancer cells from whole blood at a liquid−liquid interface. Anal. Chem. 89, 1155–1162 (2017).
Lee, A. et al. All-in-one centrifugal microfluidic device for size-selective circulating tumor cell isolation with high purity. Anal. Chem. 86, 11349–11356 (2014).
Wang, Y., Keller, K. & Cheng, X. Tangential flow microfiltration for viral separation and concentration. Micromachines 10, 20 (2019).
van Zwieten, R., van de Laar, T., Sprakel, J. & Schroën, K. From cooperative to uncorrelated clogging in cross-flow microfluidic membranes. Sci. Rep. 8, 5687 (2018).
Mukundan, H. et al. Waveguide-based biosensors for pathogen detection. Sensors 9, 5783–5809 (2009).
Stromberg, L. R. et al. Membrane insertion for the detection of lipopolysaccharides: Exploring the dynamics of amphiphile-in-lipid assays. PLoS One 11, 1–21 (2016).
Sterlitech. Polycarbonate Track Etch (PCTE) Membrane Filters Data Sheet.
Sterlitech. Polyester Membrane Filters Data Sheet.
Centers for Disease Control and Prevention. A Quick-Reference Tool for Hemolysis Status. https://www.cdc.gov/ncezid/dvbd/stories/hemolysis-palette.html (2019).
Li, T., Zhang, L., Leung, K. M. & Yang, J. Out-of-plane microvalves for whole blood separation on lab-on-a-CD. Micromech. Microeng. 20, 105024 (2010).
Mukundan, H. et al. Optimizing a waveguide-based sandwich immunoassay for tumor biomarkers: Evaluating fluorescent labels and functional surfaces. Bioconj. Chem. 20, 222–230 (2009).
Mukundan, H. et al. Quantitative multiplex detection of pathogen biomarkers on multichannel waveguides. Anal. Chem. 82, 136–144 (2010).
Boehme, C. et al. Detection of mycobacterial lipoarabinomannan with an antigen-capture ELISA in unprocessed urine of Tanzanian patients with suspected tuberculosis. Trans. R. Soc. Trop. Med. Hyg. 99, 893–900 (2005).
Jakhar, S., Lenz, K. & Mukundan, H. Current Status of Pediatric Tuberculosis: Diagnostics, Needs, and Challenges in Diagnosis and Management of Tuberculosis 1–13 (Open Access eBooks, Las Vegas, 2020).
Sakamuria, R. M. et al. Association of lipoarabinomannan with human high density lipoprotein in blood: Implications for bio-distribution and serum diagnostics. Tuberculosis 93, 301–307 (2013).
Jakhar, S. et al. Interaction of amphiphilic lipoarabinomannan with host carrier lipoproteins in tuberculosis patients: Implications for blood-based diagnostics. bioRxiv (2020) (Preprint).
Acknowledgements
This work was supported by the Los Alamos National Laboratory, Exploratory Research Project (Engineering category, PI Mukundan); and Defense Threat Reduction Agency (DTRA R-00634-19-0-DOD: Fieldable Automated Biosensor for Universal Diagnostics and Discriminating Bacterial vs. Viral Pathogens, PI Mukundan), program manager, Dr. D. Dutt. Many thanks to Dr. Kirsten McCabe, LANL program manager and Dr. Caitlin Coob, DTRA program administrator, for their support with this work. Many thanks to Aneesh R. Pawar for spending part of his student internship fabricating devices. We appreciate the guidance, suggestions, and participation of the Los Alamos National Laboratory Chemistry for Biomedical Applications team members.
Author information
Authors and Affiliations
Contributions
H.M. devised the main conceptual design of the project, acquired funding, managed and coordinated research execution, and supervised biological assay experiments. P.N. and K.D.L. conceived the centrifugal cross-flow filtration concept. P.N. trained K.D.L to investigate cross-flow filtration and supervised the microfluidic experimental workflow. S.J. and K.D.L. performed biological assay experiments. S.J. developed the LAM waveguide-based assay used for validation. K.D.L. and J.W.C. carried out the microfluidic testing experiments for optimization of RPM, time, and design parameters. K.D.L, J.W.C., D.C.P, and M.O.I. carried out fabrication of device designs and optimized the membrane integration technique used in the fabrication of devices. L.E.A. optimized the use of a custom motor set-up. J.K.S. developed the sample preparation protocol that was semi-automated in this work. A.S.A., J.F.H., and J.K.S. provided guidance and resources to contribute to the validation of this device. K.D.L. performed data analysis and figure creation. K.D.L. wrote the initial draft of the manuscript with input from P.N. and H.M. All authors discussed the results and reviewed and/or edited the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lenz, K.D., Jakhar, S., Chen, J.W. et al. A centrifugal microfluidic cross-flow filtration platform to separate serum from whole blood for the detection of amphiphilic biomarkers. Sci Rep 11, 5287 (2021). https://doi.org/10.1038/s41598-021-84353-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-84353-z
This article is cited by
-
Sample-to-answer lateral flow assay with integrated plasma separation and NT-proBNP detection
Analytical and Bioanalytical Chemistry (2024)
-
Biomimetic on-chip filtration enabled by direct micro-3D printing on membrane
Scientific Reports (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.