Abstract
The new anti-hepatitis C virus (HCV) molecules improve treatment regimens and outcomes, but there are drawbacks. New combinations should target the HCV infectious cycle and be effective against all HCV genotypes. We developed the novel formulation Catvira, composed of epigallocatechingallate (EGCG) + sofosbuvir + ribavirin. Here, we compared Catvira to sofosbuvir + ribavirin tablets in patients with CHC genotype 4 in a randomized open-label efficacy and safety study. Treatment-naïve and treatment-experienced patients (n = 80) were randomly assigned to receive a single daily fixed dose of Catvira or sofosbuvir + ribavirin for 12 or 24 weeks. Both Catvira and sofosbuvir + ribavirin yielded similar outcomes of viral load (p < 0.001). Patients receiving Catvira had a significantly more rapid rate of viral load decline with sustained virologic response (SVR12) achieved by 90% of patients receiving 12 weeks of treatment. Catvira did not impact hemoglobin levels while sofosbuvir + ribavirin showed significant decline in hemoglobin levels after 24 weeks (p < 0.05). In this clinical trial (ClinicalTrials.gov Identifier NCT02483156), we found that Catvira administered daily for 12 or 24 weeks is safe, effective, and well-tolerated in both naïve and treatment-experienced patients with HCV genotype 4.
Similar content being viewed by others
Introduction
According to the World Health Organization (WHO) report in 2020, 71 million people have chronic hepatitis C virus (HCV) infection globally with annul deaths of 400,000 from hepatitis C-related liver diseases1. The prevalence of HCV infection has markedly declined after the availability of direct acting antivirals (DAAs)2. Egypt records the highest HCV prevalence worldwide. HCV genotype 4 represents 93% of infections, while HCV genotype 1 never exceeds 10%2,3.
Recently, new regimens involving DAA agents have been approved for the treatment of HCV4,5,6. However, there are still drawbacks. The ideal inhibitor should work against more than one HCV target, including viral entry, replication, and assembly/secretion. Also, ribavirin (RBV), which is still commonly used in combination with other drugs for treatment of HCV infection, often induces hemolytic anemia even with a reduction of RBV dose7. However, there is still an important role for RBV in HCV treatment, particularly in patients with features that make a cure difficult, i.e., treatment-experienced and cirrhotic8,9.
Sofosbuvir (SOF) was the first interferon (IFN)-free DAA to be developed. In addition to its pangenotypic activity, it can be safely combined with other DAA molecules to achieve high sustained virologic response (SVR) rates in almost all HCV genotypes4. According to the recently published European Association for the Study of Liver recommendations, the combinations SOF/ledipasvir, SOF/daclatasvir (DCV), or SOF/velpatasvir are all considered optimal options for patients with HCV genotypes 1 and 410,11.
Epigallocatechingallate (EGCG), the most important polyphenol component of green tea, has been found to have antiviral and anticancer activity12. Green tea catechins include epigallocatechin-3-gallate (EGCG, which accounts for ~ 50% of the total green tea catechins), epigallocatechin (EGC), epicatechingallate (ECG), and epicatechin (EC). They are structurally different due to the presence or absence of a galloyl moiety and the wide variety of hydroxyl groups on the B-ring. For instance, EC, which lacks the gallic acid ester moiety of EGCG and one additional phenolic hydroxyl group, was inactive against HCV13. Recently, EGCG was recognized as an inhibitor of HCV access, and it targeted viral cellular entry into hepatoma cell lines and primary human hepatocytes14. Also, EGCG has been reported to enhance HCV double stranded RNA-induced antiviral innate immune responses13. Clinical studies have shown that EGCG is safe and well tolerated in healthy human volunteers13,14,15,16.
In our recently published study (ClinicalTrials.gov Identifier NCT03186313), in patients with CHC genotype 4 we used different formulations of Dactavira (EGCG + SOF + DCV, without RBV) compared with the standard of care treatment (SOF + DCV), and Dactavira plus (EGCG + SOF + DCV + RBV) compared with the standard of care plus RBV17. In this current study (ClinicalTrials.gov Identifier NCT02483156), we used the novel formulation of Catvira (EGCG + SOF + RBV) compared with standard of care treatment (SOF + RBV) in a different group of patients with CHC genotype 4.
The aim of this phase 3, open-label study was to compare the novel formulation (EHCV, Catvira), which is composed of EGCG 400 mg + SOF 400 mg + RBV 1000 mg, to SOF 400 mg + RBV 1000 mg individual tablets in patients with CHC genotype 4. Our hypothesis was that this novel formulation effectively inhibits viral entry into human host cells in addition to improving anti-hemolytic effects.
Methods
Patients
The study was conducted in accordance with the guidelines of Good Clinical Practice and was approved by the Research Ethics Committee of the Faculty of Medicine, Mansoura University, number PR/54, and is registered at ClinicalTrials.gov Identifier NCT02483156. All patients were provided written informed consent. Patients were screened and enrolled in this pilot study at a single center, Egyptian Liver Research Institute and Hospital (ELRIAH), Egypt, between July, 2015 and October, 2016. Inclusion criteria were the same as in our previous publication17. In brief, this study included only DAA-naïve, non-cirrhotic, genotype 4 infected patients with male to female ratio of 1:1. Patients were required to be more than 18 years of age, have body mass index ≥ 18 kg/m2 and have chronic genotype 4 HCV infection with a serum HCV RNA level ≥ 104 log IU/ml. Patients with normal liver function tests, renal function tests, hemoglobin level, and platelets > 50,000/µl were included. Patients with any other diseases (e.g., HBV, HIV, and DM) were excluded. Patients could be either treatment-naïve or treatment-experienced; prior treatment with an anti-HCV direct-acting antiviral was exclusionary. Baseline patient characteristics have been included in Table 1.
Study design
Treatment-naïve and treatment-experienced patients with genotype 4 HCV infection (n = 80) were randomly assigned to receive a single daily fixed dose of Catvira or SOF + RBV individual tablets daily for 12 or 24 weeks. Treatment-naïve was defined as having never received treatment for HCV with any IFN, RBV, or other approved or experimental HCV-specific DAAs. Treatment-experienced was defined as IFN intolerant, non-response, or patient with relapse/breakthrough. The random allocation sequence was generated with computer software (EDGAR, Norwich, England).
It was planned that an approximately even number of treatment-naïve and treatment-experienced subjects would be enrolled across the 2 treatment arms. In Arm 1, subjects received SOF + RBV as one tablet for a total dose of SOF 400 mg orally once daily in the morning and 1000 mg RBV divided into 2 doses daily (600 mg in the morning and 400 mg in the evening) and with food, for 12 or 24 weeks. In Arm 2, subjects received a single dose of Catvira as two tablets once daily with each tablet containing SOF 200 mg, RBV 500 mg, and EGCG 200 mg and with food, for 12 or 24 weeks.
Efficacy assessments
As in our previous publication17, serum HCV RNA was measured using the COBAS TaqMan HCV Test v2.0 (Roche Molecular Systems, Pleasanton, CA, USA). Assessment of the serum HCV RNA was performed at baseline, during treatment, and 4–12 weeks post-treatment. Patients with confirmed virologic relapse that occurred at the end of treatment or in post-treatment visits were ruled out. On-treatment virologic failure was defined as: breakthrough, i.e., confirmed HCV RNA ≥ LLOQ after having previously had HCV RNA < LLOQ while on-treatment; rebound, i.e., confirmed > 1-log10 IU/ml increase in HCV RNA from nadir while on-treatment; or, non-response, i.e., HCV RNA persistently ≥ LLOQ through 8 weeks of treatment. Relapse was defined as confirmed HCV RNA ≥ LLOQ during the post-treatment period having achieved HCV RNA < LLOQ at the end of treatment17.
Safety assessments
Safety was evaluated by assessment of clinical laboratory tests, physical examination, vital sign measurements, and documentation of adverse events. Safety data were collected from the first dose of study medication through 30 days after the last dose.
Statistical assessments
The primary efficacy endpoint was the proportion of all randomized patients who achieved SVR 12 weeks after the end of treatment (SVR12). Secondary efficacy endpoints included SVR4 and SVR24, on-treatment virologic failure, and virologic relapse after the end of treatment. In the primary efficacy analysis, SVR12 rates were calculated for each treatment group, along with 2-sided 95% confidence intervals (CIs) based on the Clopper-Pearson exact method. Differences between groups were considered statistically significant for p ≤ 0.05. All statistical analyses were performed using GraphPad InStat 3 (GraphPad, San Diego, CA, USA).
Role of the funding source
The ELRIAH had a role in the study design, data collection, and data analysis. The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Ethics approval
The study (ClinicalTrials.gov Identifier NCT02483156, 26/06/2015) was conducted in accordance with the guidelines of Good Clinical Practice and was approved by the Independent Review Board of the Faculty of Medicine, Mansoura University. All patients provided written informed consent. Special thanks to the ELRIAH clinical trial team and Virothera LLC for supporting the manufacturing and QC for Catvira clinical batches.
Results
Patients
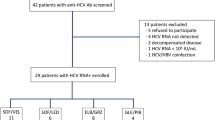
Out of 92 screened patients with chronic HCV, 80 met the inclusion criteria, and 40 were enrolled in Arm 1 and completed the treatment with SOF 400 mg + RBV 1000 mg for 12 or 24 weeks. The other 40 patients were enrolled in Arm 2 and completed Catvira treatment with EGCG 400 mg + SOF 400 mg + RBV 1000 mg for 12–24 weeks.
Efficacy
There was a significant trend for rapid lowering of HCV viral load in both groups (SOF + RBV and Catvira) versus their baseline (p < 0.001). Both SOF + RBV individual tablets and Catvira treatments were effective, with no statistically significant difference regarding SVR12 for both the 12-week (except in week 2) or 24-week study periods. Patients receiving Catvira showed rapid decline in HCV RNA levels upon initiation of treatment, from a mean of 831,425 IU/ml at baseline to 143 IU/ml in the 12-week group and from 515,633.3 IU/ml to 89 IU/ml in the 24-week group after 1 week of treatment. On the other hand, patients receiving SOF + RBV individual tablets showed decline in HCV RNA levels upon initiation of treatment, from a mean of 457,231 IU/ml at baseline to 691 IU/ml in the 12-week group and from 816,392.5 IU/ml to 96 IU/ml in the 24-week group after 1 week of treatment (Fig. 1).
Effects on the viral load (IU/ml) of Catvira treatment versus sofosbuvir (SOF) + ribavirin (RBV) individual tablets treatment in treatment-experienced patients with HCV through (a) 12 and (b) 24 weeks, n = 80. One-way ANOVA was used followed by the Newman-Keuls post-test, *p < 0.001 represents comparison of both groups SOF + RBV (*) and Catvira (+) versus their baseline. There was a significant trend for rapid lowering of HCV viral load in both groups (SOF + RBV and Catvira) versus their baseline (p < 0.001).
Regarding the Catvira group, SVR12 was achieved by 18 patients (90.0%) receiving 12 weeks of treatment and by 17 patients (85.0%) receiving 24 weeks of treatment. However, for patients receiving SOF + RBV, SVR12 was achieved by 19 patients (95.0%) receiving 12 weeks of treatment and by the 20 patients (100%) receiving 24 weeks of treatment.
Safety
Adverse effects in the Catvira group were reported in 4 patients (5%) in the 24-week group and were predominantly mild or moderate in severity. The most common adverse events in both groups were headache and epigastric pain (Table 2). In general, Catvira-related adverse effects were similar or even less than in the SOF + RBV treatment group and for a shorter duration. All these adverse events resolved and no severe adverse events were reported.
Consistent with changes in laboratory values, Catvira treatment did not impact hemoglobin levels (Fig. 2a) or red blood cell (RBC) count (Fig. 2b), but the SOF + RBV individual tablets treatment resulted in a significant decline in both parameters after 24 weeks of treatment (p < 0.05).
Effects on hematological parameters of Catvira treatment versus sofosbuvir (SOF) + ribavirin (RBV) individual tablets treatment in treatment-experienced patients with HCV (24 weeks treatment). (a) Fold changes in hemoglobin levels. (b) Fold changes in RBC counts. Values are expressed as mean ± SEM. There was a significant trend for hematological improvement (*p < 0.05) in patients treated with Catvira when compared to the SOF + RBV treatment group.
We compared the effectiveness of Catvira treatment and the SOF + RBV individual tablets treatment on the liver functions by measuring ALT, AST, bilirubin, and alkaline phosphatase. Both treatments improved liver functions. Furthermore, both treatments achieved significant improvement (p < 0.001) in liver enzymes ALT (Fig. 3a) and AST (Fig. 3b).
Effects on liver enzymes of Catvira treatment versus sofosbuvir (SOF) + ribavirin (RBV) individual tablets treatment in treatment-experienced patients with HCV (24 weeks treatment). (a) Effect on alanine transaminase (ALT) enzymes. (b) Effect on aspartate transaminase (AST) enzymes. Values are expressed as mean ± SEM. A significant difference (***p < 0.001) was observed in patients treated with Catvira and SOF + RBV when compared to control patients with HCV who were not treated.
There were no instances of a patient experiencing an adverse event that led to dose modification, interruption, or discontinuation of either regimen.
Discussion
In this pilot study, 12 and 24 weeks of treatment with Catvira resulted in similar rates of SVR12 in treatment-naïve and treatment-experienced patients with genotype 4 HCV. The regimen was well tolerated, with mostly mild adverse events typically associated with RBV therapy, especially a decrease in RBC count and hemoglobin levels.
Catvira consists of an additional molecule, EGCG, which is the bioactive catechin in green tea. EGCG displays strong preventive effects against different viral infections including HCV, HIV, influenza virus, and human herpes simplex virus18. Particularly, EGCG impairs the close links between the HCV life cycle and the lipid metabolism, which may interfere with HCV infection. Also, it has been reported that EGCG acts at an early step of entry by interfering with viral docking to the cell surface19. Initial binding of HCV particles to hepatocytes is mediated by heparin sulfate proteoglycan, scavenger receptor type B class 1 (SR-B1), and apoE20,21,22,23. Furthermore, the interaction of HCV particle with the low-density lipoprotein receptor (LDL-r) has also been proposed to play a role in the early phase of HCV entry24. Chen et al. reported that EGCG not only interferes with HCV entry, but also inhibits the viral RNA replication by 2- to threefold but only at a very high concentration (80 μM) of EGCG in vitro25. Further studies indicated that an observed bulge was found on the viral particle after EGCG treatment. This structural alteration led to a failure of membrane binding mediated by heparin sulfate- or sialic acid-containing glycans14,26. See Fig. 4 for an illustration of the potential effect of Catvira.
Catvira interferes with HCV entry into human hepatocytes. Cell entry involves an interaction between the extracellular virion that is associated with lipoproteins and several receptors on the host cell membrane. These include scavenger receptor type B class 1 (SR-B1), epidermal growth factor receptor (EGF-R), CD81, and possibly low-density lipoprotein receptor (LDL-r). It has been suggested that the lipoprotein receptors SR-B1 and LDL-r act before CD81. These interactions induce travelling of the virus-receptor complex along the cell surface from the basolateral (blood-side) surface of the hepatic epithelium where LDL-r, SR-B1, and CD81 are localised. These events, stimulated by virion-mediated activation of receptor tyrosine kinase signaling like EGF-R, result in clathrin-dependent endocytosis of the virion. Catvira is a single tablet composed of sofosbuvir (400 mg), ribavirin (1000 mg), and epigallocatechin gallate (EGCG) (400 mg). Catvira is suggested to act on the virus particle and inhibits virus entry by impairing virus binding to the cell surface.
Lin et al. reported that HCV replication was downregulated by epicatechin isomers in vitro in cell-based HCV replicon and JFH-1 infectious systems. Epicatechin isomers have been reported to suppress the expression of inflammatory factors such as IL-1β, TNF-α, iNOS, and COX-227.
EGCG is known to be safe with regard to hepatocytes. Calland et al. reported that EGCG had no toxic effect on Huh-7 cells (LD50 ~ 160 μM)19. Another study found that 400 mg of EGCG was well tolerated and safe in cirrhotic patients with HCV28.
In addition, EGCG has preventive effects against cardiovascular disease, metabolic syndrome, neurodegenerative diseases, and cancer29. EGCG might block hemolytic anemia, which is associated with RBV by acting as a highly efficient free radical scavenger. Consistent with our result, Kim et al. reported the protective effect of EGCG against the hemolytic effect of cyclosporine therapy, which was associated with increased production of free radical species16. Also, EGCG lowered the hemolysis and hydrogen peroxide levels and malondialdehyde produced by normal human erythrocytes (RBCs) incubated with cyclosporine.
Based on these preliminary data, Catvira might be superior to SOF + RBV individual tablet regimen with respect to adverse events, mainly RBV-induced hemolysis. Catvira not only interferes with viral replication, but also inhibits virus entry. However, any such conclusions need to be established with a larger number of patients.
Limitations of this study include the small sample size, no cirrhotic patients were included, and genotype subtypes were not done. Although most cases are now treated with an RBV-free regimen because of RBV’s side effects, RBV has a crucial role in increasing SVR for treatment-experienced and cirrhotic patients. Catvira is anti-hemolytic also; activity improves the tolerability of the therapy.
Catvira, administered daily for 12 or 24 weeks, is safe and effective in both naïve- and treatment-experienced patients with genotype 4 HCV. Catvira’s antiviral-entry mechanism may also play a role in enhancing efficacy and preventing relapse over SOF and RBV individual tablets. In addition to potentially enhanced efficacy, Catvira’s anti-hemolytic activity may improve the safety and tolerability of the therapy.
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
World Health Organization. Hepatitus C. https://www.who.int/en/news-room/fact-sheets/detail/hepatitis-c.
Omran, D. et al. Towards hepatitis C virus elimination: Egyptian experience, achievements and limitations. World J. Gastroenterol. 24, 4330–4340. https://doi.org/10.3748/wjg.v24.i38.4330 (2018).
Messina, J. P. et al. Global distribution and prevalence of hepatitis C virus genotypes. Hepatology 61, 77–87. https://doi.org/10.1002/hep.27259 (2015).
Doss, W. et al. Sofosbuvir plus ribavirin for treating Egyptian patients with hepatitis C genotype 4. J. Hepatol. 63, 581–585. https://doi.org/10.1016/j.jhep.2015.04.023 (2015).
Shiha, G. et al. The Liver Meeting Vol. 63, 436A-437A (Hepatology, Boston, 2016).
Waked, I. et al. Ombitasvir, paritaprevir, and ritonavir plus ribavirin for chronic hepatitis C virus genotype 4 infection in Egyptian patients with or without compensated cirrhosis (AGATE-II): a multicentre, phase 3, partly randomised open-label trial. Lancet Gastroenterol. Hepatol. 1, 36–44. https://doi.org/10.1016/S2468-1253(16)30002-4 (2016).
Eletreby, R. et al. Real life Egyptian experience of efficacy and safety of simeprevir/sofosbuvir therapy in 6211 chronic HCV genotype IV infected patients. Liver Int. 37, 534–541. https://doi.org/10.1111/liv.13266 (2017).
Feld, J. J. et al. Ribavirin revisited in the era of direct-acting antiviral therapy for hepatitis C virus infection. Liver Int. 37, 5–18. https://doi.org/10.1111/liv.13212 (2017).
Shiha, G., Soliman, R., ElBasiony, M., Hassan, A. A. & Mikhail, N. N. H. Sofosbuvir plus Daclatasvir with or without ribavirin for treatment of chronic HCV genotype 4 patients: real-life experience. Hepatol Int. 12, 339–347. https://doi.org/10.1007/s12072-018-9861-2 (2018).
European Association for the Study of the Liver. EASL recommendations on treatment of hepatitis C 2018. J. Hepatol. 69, 461–511. https://doi.org/10.1016/j.jhep.2018.03.026 (2018).
European Association for the Study of the Live. EASL recommendations on treatment of hepatitis C: Final update of the series. J. Hepatol. https://doi.org/10.1016/j.jhep.2020.08.018 (2020).
Sheng, R., Gu, Z. L. & Xie, M. L. Epigallocatechin gallate, the major component of polyphenols in green tea, inhibits telomere attrition mediated cardiomyocyte apoptosis in cardiac hypertrophy. Int. J. Cardiol. 162, 199–209. https://doi.org/10.1016/j.ijcard.2011.07.083 (2013).
Ciesek, S. et al. The green tea polyphenol, epigallocatechin-3-gallate, inhibits hepatitis C virus entry. Hepatology 54, 1947–1955. https://doi.org/10.1002/hep.24610 (2011).
Calland, N. et al. Polyphenols inhibit hepatitis C virus entry by a new mechanism of action. J. Virol. 89, 10053–10063. https://doi.org/10.1128/JVI.01473-15 (2015).
Sriram, N., Kalayarasan, S., Manikandan, R., Arumugam, M. & Sudhandiran, G. Epigallocatechin gallate attenuates fibroblast proliferation and excessive collagen production by effectively intervening TGF-b1 signalling. Clin. Exp. Pharmacol. Physiol. 42, 849–859. https://doi.org/10.1111/1440-1681.12428 (2015).
Kim, H. C., Chang, E. J. & Mun, K. C. Effects of epigallocatechin gallate on the hemolysis induced by cyclosporine. Transplant. Proc. 37, 2385–2386. https://doi.org/10.1016/j.transproceed.2005.03.006 (2005).
Shiha, G., Soliman, R., Elbasiony, M., Darwish, N. H. E. & Mousa, S. A. Addition of epigallocatechin gallate 400 mg to sofosbuvir 400 mg + daclatisvir 60 mg with or without ribavirin in treatment of patients with chronic hepatitis C improves the safety profile: a pilot study. Sci. Rep. 9, 13593. https://doi.org/10.1038/s41598-019-49973-6 (2019).
Wang, Y. et al. (-)-Epigallocatechin-3-gallate enhances hepatitis C virus double-stranded RNA intermediates-triggered innate immune responses in hepatocytes. Sci. Rep. 6, 21595. https://doi.org/10.1038/srep21595 (2016).
Calland, N. et al. (-)-Epigallocatechin-3-gallate is a new inhibitor of hepatitis C virus entry. Hepatology 55, 720–729. https://doi.org/10.1002/hep.24803 (2012).
Dao Thi, V. L. et al. Characterization of hepatitis C virus particle subpopulations reveals multiple usage of the scavenger receptor BI for entry steps. J. Biol. Chem. 287, 31242–31257. https://doi.org/10.1074/jbc.M112.365924 (2012).
Barth, H. et al. Cellular binding of hepatitis C virus envelope glycoprotein E2 requires cell surface heparan sulfate. J. Biol. Chem. 278, 41003–41012. https://doi.org/10.1074/jbc.M302267200 (2003).
Scarselli, E. et al. The human scavenger receptor class B type I is a novel candidate receptor for the hepatitis C virus. EMBO J. 21, 5017–5025 (2002).
Jiang, J., Wu, X., Tang, H. & Luo, G. Apolipoprotein E mediates attachment of clinical hepatitis C virus to hepatocytes by binding to cell surface heparan sulfate proteoglycan receptors. PLoS ONE 8, e67982. https://doi.org/10.1371/journal.pone.0067982 (2013).
Agnello, V., Abel, G., Elfahal, M., Knight, G. B. & Zhang, Q. X. Hepatitis C virus and other flaviviridae viruses enter cells via low density lipoprotein receptor. Proc. Natl. Acad. Sci. USA 96, 12766–12771. https://doi.org/10.1073/pnas.96.22.12766 (1999).
Chen, C. et al. (-)-Epigallocatechin-3-gallate inhibits the replication cycle of hepatitis C virus. Arch. Virol 157, 1301–1312. https://doi.org/10.1007/s00705-012-1304-0 (2012).
Colpitts, C. C. & Schang, L. M. A small molecule inhibits virion attachment to heparan sulfate- or sialic acid-containing glycans. J. Virol. 88, 7806–7817. https://doi.org/10.1128/JVI.00896-14 (2014).
Lin, Y. T. et al. Green tea phenolic epicatechins inhibit hepatitis C virus replication via cycloxygenase-2 and attenuate virus-induced inflammation. PLoS ONE 8, e54466. https://doi.org/10.1371/journal.pone.0054466 (2013).
Halegoua-De Marzio, D. et al. Limited sampling estimates of epigallocatechin gallate exposures in cirrhotic and noncirrhotic patients with hepatitis C after single oral doses of green tea extract. Clin. Ther. 34, 2279.e1-2285.e1. https://doi.org/10.1016/j.clinthera.2012.10.009 (2012).
Yang, C. S., Chen, G. & Wu, Q. Recent scientific studies of a traditional Chinese medicine, tea, on prevention of chronic diseases. J. Trad. Complement. Med. 4, 17–23. https://doi.org/10.4103/2225-4110.124326 (2014).
Acknowledgements
Special thanks to the Egyptian Liver Research Institute and Hospital (ELRIAH), Egypt, clinical trial team especially Dr. Ahmed Farahat, Study Coordinator, for sponsoring the clinical study and to Virothera Pharmaceuticals, Rensselaer, NY, USA for supporting the manufacturing and QC for EHCV (Catvira) clinical batches. We appreciate Dr. Kelly A. Keating, Pharmaceutical Research Institute, for her excellent editing of this manuscript.
Author information
Authors and Affiliations
Contributions
G.S. designed the clinical trial and is the Principal Investigator. R.S. and M.E. conducted the clinical trial and did the patient enrollment and randomization. N.H.E.D. did the data analysis. S.A.M. contributed to the single tablet design and manufacturing and the design of the study and with G.S. contributed to the manuscript write up and data interpretation. All authors have approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
Gamal Shiha has been a Principal Investigator for Gilead and Abbvie. Reham Soliman has been an Investigator for Gilead and Abbvie. Mohamed Elbasiony has been an Investigator for Gilead. Shaker A Mousa has no conflict of interest other than helping HCV patients in underdeveloped countries have access to treatment at low to no cost. Noureldien H. E. Darwish declares no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Shiha, G., Soliman, R., Elbasiony, M. et al. Novel combined single dose anti-hepatitis C therapy: a pilot study. Sci Rep 11, 4623 (2021). https://doi.org/10.1038/s41598-021-84066-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-84066-3
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.