Abstract
Functional gastrointestinal disorders (FGIDs) are common among the aircrew due to their arduous working environment. This study investigated the prevalence of FGIDs in Chinese male pilots and assessed the effects of trigger factors on the FGIDs. A cross-sectional study including 212 male pilots was performed in a Chinese large civil airline company. FGIDs were diagnosed according to the Rome IV diagnostic criteria. The psychological performance, dietary pattern, sleep situation, and physical activity of the respondents were assessed. Logistic regression analysis and structural equation modeling were used to explore the association between these trigger factors and FGIDs. FGIDs were observed in 83 (39.22%) respondents, of which 31 (37.35%) had overlap syndromes. Age, flight level, flight time, high-salt food pattern, anxiety, and sleep performance were found to be associated with FGIDs (all P < 0.05). Stepwise logistic regression analysis revealed that the flight level (OR 0.59, 95% CI 0.31–0.080), high-salt food pattern (OR 2.31, 95% CI 1.28–4.16), and sleep performance (OR 2.39, 95% CI 1.11–5.14) were the influencing factors associated with FGIDs. Structural equation modeling confirmed the correlations between FGIDs and the occupational, dietary, and psychological factors with a reasonable fit. The preventive strategies were necessitated according to occupational and psychological characteristics.
Similar content being viewed by others
Introduction
Functional gastrointestinal disorders (FGIDs) are characterized by chronic or recurrent gastrointestinal (GI) symptoms except for organic lesions, which include irritable bowel syndrome (IBS), functional dyspepsia (FD), functional heartburn(FH), functional constipation (FC), and so on1. An epidemiological study reported that 10–20% of the world population was affected by FGID2, and 1–8% of the FGIDs patients had two or three overlap syndromes3. These functional disorders rendered a negative impact on the quality of life of patients and caused a high disease burden, especially on some arduous occupational persons4,5,6. For example, a survey involving 1217 Korean firefighters reported that 37.9% of the respondents were diagnosed with FGIDs4. A United States’ study revealed that 76.8% of soldiers in Operation Iraqi Freedom and 54.4% of soldiers in Afghanistan experienced diarrhea7.
Commercial airplane pilots are also exposed to a high risk of suffering from FGIDs. The specific occupational environment including cosmic radiation and jet fuel8, long and irregular working patterns9 as well as crossing multiple time zones10 are their common occupational conditions11. Travel fatigue and disturbance of circadian rhythm can break the balance of their private life and induce various health problems12,13. Besides, occupational stress and emotional trauma are also experienced commonly among aircrews. A cross-sectional study on the Chinese air force population reported that 23.5% of 4630 initial participants were identified with more than one FGID, and the prevalence in the 787 aircrew members was as high as 20.33%14.
Besides the physical trauma, the dietary pattern is also closely associated with the onset and exacerbation of the FGIDs in pilots15,16. The diet types of pilots were relatively simple, unbalanced and unscheduled, which may also result in the risk of digestive disorder. On the other hand, psychological factors play an important role in the onset of FGID symptoms17. Previous studies revealed that among the patients with FGIDs, 30% presented with possible depression while 22% presented with possible anxiety18. The symptoms of FGIDs were severe when accompanied by depression, anxiety, and other psychiatric disorders19. In case of aviator occupation, the flight environment, vibration, and noise may lead to anxiety, occupational stress, and other emotional problems. However, pilots with FGIDs may always overlook the importance of psychosocial factors14,20,21.
Until now, only a few studies reported the risk of FGIDs that the pilots faced. Moreover, few study measured the prevalence of FGIDs for Chinese civil pilots and the possible mechanisms between the trigger factors and the development of FGIDs. Given the gender differences on the FGIDs epidemiology22,23 and low proportion of female among civil pilots in China24, this study aimed to investigate the prevalence of FGIDs among the commercial male pilots in China with the new Rome IV diagnostic criteria and assess the effects of the physical and mental performance on the FGIDs, so as to optimize the health care management during their career.
Methods
Participants
The study was conducted in accordance with the principles of the Declaration of Helsinki. The Ethics Committee of the Fourth Military Medical University carefully considered and approved the project proposal. Between November 2018 and December 2018, representative male pilot employees in a large civil airline company in China were recruited using a convenience sampling methodology, and a cross-sectional survey was performed. Male pilots, aged 20–50 years, who had taken sick leave for no more than 4 weeks during the recruitment period were eligible for participation. The pilots with organic esophageal or GI tract disease were excluded. Informed consent was obtained from all individual participants included in the study. All the respondents were assured that no names were registered in the questionnaires and their answers would not impact on their occupational achievement or their future work.
Measures
After being interviewed by flight surgeons, all respondents were required to complete a self-report questionnaire, which consisted of the following parts: part 1 focused on demography and job description such as age, body mass index (BMI), marital status, education, and so on; part 2 included the Rome IV diagnostic criteria25 to evaluate the FGIDs; part 3 assessed the psychological performance using the self-rating anxiety scale (SAS) and self-rating depression scale (SDS)26,27; part 4 assessed the dietary patterns of participants with three-point semi-quantitative food frequency questionnaire(SQFFQ),; and part 5 evaluated the sleep and physical activity situations of pilots using the Pittsburgh sleep quality index (PSQI28 and the International Physical Activity Questionnaire Short Form (last7-self)29. All the responses were recorded on one computer using the EPIDATA 3.1 data documentation software.
FGID
The diagnosis of FGID was based on the new Rome IV criteria25. The questionnaire for Rome IV diagnostic criteria was translated to Chinese according to Chinese culture. Eighty pilots were randomly selected to complete the Chinese questionnaire in order to assess its comprehension and accuracy. The internal consistency reliability estimates for each section were within the desired range with Cronbach’s \(\alpha\) coefficient 0.82–0.89. After two times surveys with the kappa coefficient of 0.83, the Chinese questionnaire was applied to diagnose the FGID. If one of the FGID manifestations was identified, the respondent was diagnosed with FGIDs. The overlap syndrome was defined as at least two of the FGID symptoms. According to the manifestations of FGID, the respondents were divided into three groups: the healthy group, the single FGID group, and the combined symptom FGID group.
Diet
The semi-quantitative food frequency questionnaire was designed to collect the food list, frequency of consumption and the portion size consumed30. Referenced a lot of Chinese food frequency questionnaire31,32,33, we selected 27 food categories often eaten in Chinese dietary, which covered cereals, meat, vegetables, fruits, egg products, nuts, fish, and so on. There was also an open question to detect the subject’s favor food which not contained in the given 27 food categories. The intake frequencies were classified into eight levels: almost never; less than one time per month; 1–3 times per month; one times per week; 2–4 times per week; 5–6 times per week; one time per day; 2–3 times per day and 4 or more times per day. There was no unified portion size in China, and therefore, food types and portion size of local food were surveyed with visual aids, which consisted of photographs of utensils and food portions to assist with description of amounts consumed. Options for the average portion sizes were 0.5, 1, 1.5, 2. Based on the food composition and food model34,35, it investigated the food intake of each subject in the recent half year. And a 3-day 24-h dietary recalls (24 h DRs) was also used to evaluate the reliability and validity of this SQFFQ.
The diet pattern was identified by exploration factor analysis36. The common factors with Eigenvalues > 1.0 were extracted based on the screen plot. An orthogonal rotation procedure was applied to simplify the factor structure and render it more easily interpretable. The derived factors were named as the different dietary patterns according to the food categories that loaded most strongly on the factor. For each participant, the factor score for each pattern was calculated by summing the quantity of each food grouping weighted by their loading on each factor. The dietary pattern scores were expressed as three quartiles for comparison across levels of intake.
Psychology
The evaluations related to psychology, sleep, and physical activity were performed according to the corresponding standard criteria. Specifically, the respondents with the SAS index scored above 50 and the SDS index scored above 0.50 were defined as having anxiety and depression, respectively26,27. A PSQI score of 1–5 was considered as sleep quality, 6–10 as sleep latency, 11–15 as sleep duration, and 15–21 as sleep disturbance28. The physical activity intensity was divided as low (the total physical activity score below 600), median (the total physical activity score between 600 and 3000), and high (the total physical activity score above 3000)29.
Statistical analyses
Statistical analyses were performed using SAS 9.1.3 (SAS Institute Inc., USA). Continuous variables were expressed by mean ± standard deviation when the data was approximately normally distributed, otherwise a non-parametric alternative should be used instead. The categorical variables were expressed by numbers and percentages. A one-way ANOVA was used to compare the normal distribution variables, followed by a LSD test for post hoc analysis to further examine the differences among the groups. The chi-square test was used to test the differences for categorical variables. Stepwise logistic regression analysis was conducted to investigate the associations between various factors and FGIDs. Structural equation modeling (SEM), using M-Plus (Muthen & Muthen, Mplus, Version 7), was applied to explore the associations between latent physical and mental factors and the developing of FGIDs. A two-tailed P value of less than 0.05 was considered to be statistically significant.
Results
Characteristics of participants
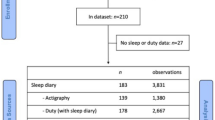
A total of 212 male pilots were sampled in this cross-sectional study. All the participants completed their questionnaire with a response rate of 100%. As shown in Table 1, the respondents demonstrated a mean age of 33.83 ± 7.05 years (range 22–48 years), a BMI of 23.84 ± 2.35 kg/m2 (range 18.94–29.00 kg/m2), and 87.74% of them were Han race. The proportion of smokers and alcohol drinkers was 48.83% and 31.92%, respectively. More than 40% of the respondents were the captain and (senior) first officer. The mean flight time was 19.62 ± 10.11 h within 1 month, with the day-night flight ratio as 2:1. Of all the pilots, almost 50% had no long voyage within 1 month, and 16.98% had long voyages three or four times every month. Approximately 80% of the respondents reported that they had undergone a regular physical examination 6 months prior and had no disease history.
Spectrum of FGID
From a total of 212 respondents, 83 (39.15%) were identified with FGIDs, four major categories of FGIDs were observed based on the Rome IV criteria: bowel disorders (20.28%), gastroduodenal disorders (17.45%), esophageal disorders (13.68%) and central mediated disorders of gastrointestinal pain (0.94%) (Table 2).
The prevalence of individual FGID is as follow. Globus (7.08%), Functional dyspepsia (FD: 13.21%), and IBS (9.43%) were the most frequent diagnoses among bowel disorders, gastroduodenal disorders and esophageal disorders respectively, whereas FC (4.25%), functional chest pain (FCP: 3.77%), and functional abdominal bloating (FAB: 4.72%) also had a moderate prevalence. Only two aviators had rumination syndrome, and two other aviators had central-mediated abdominal pain syndrome.
As for the overlap syndrome, 31 pilots met the criteria for more than one FGID symptom. The categories of FGIDs occurred in different combinations were shown as two-way combination 8.49%, three-way combination 3.33% and four-way combination 2.83% (Table 2 and Fig. 1). Bowel disorders and gastroduodenal disorders were the most prevalent (4.72%) in the two-way combination, whereas central mediated disorders of gastrointestinal pain had no combination. For the detailed syndrome, globus + nausea and vomiting disorders (NVD), FD + IBS and FD + FAB led the two-way combination (1.89%). Among the seven pilots with three-way combined FGIDs (4.72%), four were diagnosed with FD + IBS + globus. While, the six pilots with four-way overlap syndromes all manifested IBS syndromes.
Diet pattern
The SQFFQ demonstrated acceptable relative validity and high reproducibility with intraclass correlation coefficients (ICCs) of 0.44–0.77, spearman’s correlation coefficients of 0.35–0.62 and the three-point quartile agreement of 72.0–95.0% in the same or adjacent quartiles for the food categories referenced 24 h DRs. Via the three-point semi-quantitative food frequency questionnaire, four dietary patterns were retained for analysis as follow: the vegetarian pattern characterized by green vegetables and fruits, the high-salt food pattern characterized by Chinese pickles and bacon, the starch food pattern characterized by the Chinese traditional staple food of rice and noodles and the protein food pattern characterized by high-quality protein products such as fish, milk and mushrooms.
The dietary pattern scores were expressed as three quartiles for comparing the levels of intake between different FGID groups, as shown in Table 3. The vegetarian pattern, the starch food pattern and protein food pattern were not related to the distribution of FGIDs. However, respondents with high-salt food pattern scores above 66.7% were more likely to be identified with FGIDs than those with lower scores (P < 0.001). The odds ratio [OR 2.46, 95% confidence level (CI) 1.71–3.35] indicated that high-salt food pattern was positively associated with FGIDs; for every 33% increase in the high-salt food pattern score, the risk of FGIDs might double.
aThe reference is the low-level group.
Psychological situation
According to the evaluation criteria of the SAS27, the anxiety scores were different between the three groups, as shown in Table 4 (P = 0.006). The overlap syndrome group had the highest anxiety score (48.75 ± 13.30), followed by the single FGID syndrome group (44.48 ± 6.46). In the post hoc analysis, the anxiety score was significantly higher in the overlap syndrome group than in the healthy group, which meant that the more FGID syndromes the respondents had, the higher anxiety scores they got.
The depression and physical activity situation showed no significant difference between the three groups. According to the criteria of PSQI (short version), the single syndrome group had the highest sleep score (11.78 ± 3.31), followed by the combined syndrome group (11.27 ± 2.82) and the healthy control group (10.26 ± 2.84) (P = 0.005). The score of the single syndrome group was significantly higher than that of the control group.
Associations between predictor variables and FGIDs
Table 5 shows a number of variables significantly associated with the prevalence of FGIDs. The respondents over 35 years were more likely to have FGIDs. For the occupation factors, the flight levels were adversely affected by the FGIDs. The captain had the highest prevalence of FGIDs, followed by the first and second officer. The aircrew flying for more than 20 h every month had almost one times higher prevalence of FGIDs than those flying for less than 10 h.
The high-salt food pattern was positively associated with the development of FGIDs. The prevalence of the upper three-quartile score group was almost three times of those in the lower three-quartile score group (56.34% vs 19.18%), which meant that the respondents with high-salt food pattern were more likely to have FGIDs.
The psychological factors and the FGIDs were also related. The prevalence of FGIDs in anxious aircrews was two times than that in aircrews without anxiety (P = 0.002). The depression and physical strength did not correlate with the FGIDs, but a good sleep quality might positively prevent the occurrence of FGIDs. The pilots with sleep scores of 16–21 had the highest prevalence of FGIDs, which was approximately three times than the prevalence in those with good sleep.
The multivariate logistic regression analysis showed that three predictors were found to independently and significantly correlate with the FGIDs: flight level (OR 0.59; 95% CI 0.31–0.80; P = 0.001), high-salt food pattern (OR 2.31; 95% CI 1.28–4.16; P < 0.001), and sleep score level (OR 2.39, 95% CI 1.11–5.14; P = 0.002) (Table 5, Model chi-square test, P < 0.001; Hosmer–Lemeshow’s goodness-of-fit test, P < 0.001).
We also explored a subgroup analysis of the risk factors by FGID types. Given the relatively small number for each specific FGID symptom, this analysis was mainly conducted on the sub-type FGIDs as the esophageal disorders, gastroduodenal disorders, bowel disorders according to Rome IV diagnostic criteria. As shown in Table 6, the trigger factors for the subgroup syndromes were quite similar to those for FGIDs. For example, the higher flight level pilots with anxiety symptoms were more likely to have esophageal disorders. While, age, flight level, flight time per month, and high-salt food pattern were found to associate with the gastroduodenal disorders significantly. The older age, the high flight level, the high-salt food pattern, the anxious psychology and the poor sleep performance might be the potential factors contributing to the bowel disorders.
Structural equation model
A confirmatory factor analysis (CFA) using Structural equation model (SEM) was conducted to assess the linear association between the effects of the trigger factors on the FGIDs. Age, flight factors, food categories with a factor loading of more than 0.4 in the high-salt food pattern, and psychological factors were considered to be enrolled in the analysis. The resulting SEM is illustrated in Fig. 1, in which the chi-square test result was statistically significant (χ2 = 223.72, P < 0.001), the comparative fit index was (0.97) > 0.90, the root-mean-square error of approximation was (0.02) < 0.06, and the degree of freedom ratio was (1.03) < 3.00.
As Fig. 2 indicated, the diet pattern and the latent psychology variable were negatively associated with each other (standardized regression coefficient, − 0.30), which meant that less high-salt food might be related to good psychology. Both of them affected the latent flying variable with \(\beta =\) − 0.44 and \(\beta =\) 0.54, respectively, indicating that the aviators with high flying level might prefer the high-salt food and endure poorer psychology. Finally, the latent flying variable positively correlated with FGIDs (\(\beta =\) 0.72). For the explanatory power of the SEM, the diet and psychology accounted for approximately 50% variance in the flying variable, which resulted in 71.80% of the variance in the FGIDs, indicating that the presence of other latent factors might be linked to FGIDs.
Parameter estimates (standard regression coefficients) of the structure equation model for the effects of the trigger factors on the FGIDs. A1: age, A2: flight level, B1-B6: six food categories with factor loading > 0.4 in the high-salt food pattern, which were B1: chicken, B2: animal giblets, B3: Chinese pickles, B4: water food (one of Chinese pickled vegetable), B5: preserved meat and B6: bacon, C1: anxiety, C2: depression, C3: sleep performance.
Discussion
As studies on the prevalence of FGIDs in Chinese aviators were very limited, this study was conducted to identify the effect of the trigger factors on the FGIDs for the civil pilots. We have just focused on the FGIDs of male pilots. That is because the prevalence of FGIDs varied substantially between female and male37, such as FD22,37,38 and IBS23,39,40. While, the proportion of female in Chinese pilots was very low, which was reported as only 1.85% for the commercial certificate pilots and 0.33% for the aviation transport license pilots24. In this study, we had used the convenience sampling methodology to recruited the subjects. There were too few female pilots attending this research voluntarily in the recruiting phase. On the contrary, female mostly undertake the cabin crews in China. Although both of the pilots and cabin crew are exposed to the same working environment, the potential activity level and occupational variables are quite varied. Considering the gender and occupational difference, we do not include the female pilots in this study. Therefore, it should be cautious when generalizing the results to the characteristics of all the aircrews.
In this study, 39.15% of the respondents had FGIDs. This value was high compared with that in some other studies, in which the prevalence of military aircrews was 7.2% in the USA41 and 3.50% in China14. However, this was lower than those reported by Park (49.7%)42 and Trivedi in their study including soldiers presenting to a home hospital (50%)43. The diversity in prevalence might be because the first survey on the Chinese commercial pilots used Rome IV criteria. It might also be because of the developments in the Chinese aviation and tourism industries, in which the aviator occupation required a highly efficient and error-free performance. The pilots undergo very stressful physical and psychiatric training, which may be the reason of the high prevalence of FGIDs among them. Although the pilots with organic esophageal or GI tract disease were excluded in this survey, the helicobacter pylori status were not evaluated among the participants, which were also an essential for differential diagnosis.
This study also found that FD was the most prevalent FGIDs overall (13.21%), followed by IBS (9.43%) and globus (7.08%). The main subtype rank was similar to that in other studies, such as Bang44, Wu14, and Dong45. However, the prevalence in this study was quite higher than these studies, which were reported as 5.85% and 4.04% for FD and IBS for the Chinese air forth pilots’ prevalence in Wu’s research14. It also showed a higher prevalence of FD and IBS than the general populations, in which the global prevalence of FD was reported as 6.9% (95 CI 5.7–8.2) from a meta-analysis in 2020 comprising 81,144 subjects from 4 studies with the ROME IV criteria22. Another meta-analysis comprising 82,476 individuals from 34 countries claimed the pooled IBS prevalence was 3.8% (95 CI 3.1–4.5) used the Rome IV criteria23. Although researches suggested the Rome IV criteria might be stricter for the diagnostic of FGIDs compare to the prior criterion46,47, the prevalence of FD and IBS in this study were higher than those in the systematic reviews. Therefore, cautious interpretations should be made regarding this aspect.
In terms of overlapping syndromes, the prevalence was estimated as 14.62% of the total population and 37.35% of the patients with FGIDs in this study. In previous studies, the prevalence was reported to range from 1 to 17%3,48,49,50,51, not much different from the results of this study. As for the most combination syndromes, this study showed that FD + IBS, FD + FAB, and NVD + globus (1.89%) were the most prevalent subtype constitutions, which was quite similar to the findings of studies on healthy military males from the USA52 and Korea53.
However, it's worth noting that previous studies had found that there may be few difference for Rome IV criteria compared to the prior Rome criterion46,54. For example, a study recruited 1375 adults self-identified as having IBS found that the Rome IV criteria significantly under reported the prevalence of IBS in comparison to Rome III(59.1% vs. 78.9%)47. Some systematic review also reported that the pooled prevalence of uninvestigated dyspepsia and IBS were lower with Rome IV(dyspepsia: 6.9% vs. 11.5%; IBS: 3.8 vs. 9.2%)22,23. It seemed that Rome IV criteria were more restrictive. The agreement between Rome III and Rome IV is still needed to be detected further. Understanding the impact of these changes to the diagnostic classification system for FGIDs will be important in the future.
In addition, the results also found several trigger factors related to FGIDs. They included occupational exhaustion, dietary pattern, psychological stress, and sleep performance. For the occupational environment, high-speed flying, constant exposure to rapid acceleration and deceleration, and noise and vibration might be the complicated mechanisms resulting in abdomen discomfort55,56,57. Therefore, the flight level and flight time were closely associated with the development of FGIDs.
Similar to other studies57,58, the effects of dietary patterns on the FGIDs were proved by the CFA and SEM results. Although carbohydrates, proteins, and individual fatty acids were the most frequently compounds that influenced the digestive functions, a positive association was found between the high-salt dietary pattern and the FGIDs in this study. The high-salt intake might be of particular importance for the composition and activity of intestinal microbiota59. Specific nutrients could change the microbial metabolic activity, leading to GI discomfort.
In agreement with the results of previous studies, psychological distress was found to be positive related to FGIDs and combined syndromes in our research. The anxiety factor was proved to be an independent risk factor for FGIDs, whereas no statistical correlation was observed between depression and FGIDs. This result was similar to a study of the brain–gut pathway60, but not coincident with some studies, which found that depression had a negative correlation with FGIDs14,44. The exact reason or mechanism was unclear. More studies are needed to elucidate the association between each psychological factor and FGIDs.
In conclusion, this is the first population-based survey using Rome IV criteria to evaluate FGIDs among Chinese pilots, which has found that there is a high overall prevalence of FGIDs among Chinese male pilots, especially on FD, IBS and Globus. The SEM analysis elaborated the effects of the flight factor, food pattern, psychology and sleep performance on the FGIDs. Therefore, further works can be conducted on more integrative prevention and treatment combining psychological and physical approaches for the developing and progression of FGIDs.
This study also had some limitations. First, it could not identify a causal relationship between some influence factors and FGIDs, because it was a cross-sectional study with subjective bias. Second, the information was obtained using self-administered questionnaires, in which may conceal a possibility of subjective bias. Third, only male aviators were included in this study, generalizing the results to the characteristics of all commercial pilots with FGIDs was difficult. More researches are required on a wide range of respondents and the various trigger factors in the future.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Spiller, R. (BMJ Publishing Group, London, 2000).
Ghoshal, U. C. et al. Development, translation and validation of enhanced asian Rome III questionnaires for diagnosis of functional bowel diseases in major Asian languages: A Rome foundation-Asian Neurogastroenterology and Motility Association Working Team report. J. Neurogastroenterol. Motil. 21, 83 (2015).
Locke, G. III., Zinsmeister, A., Fett, S., Melton, L. III. & Talley, N. Overlap of gastrointestional symptom complexes in a US community. Neurogastroenterol. Motil. 17, 29–34 (2005).
Dierkes-Globisch, A., Fallen, H. & Hans-Heinrich, M. Functional gastrointestinal disorders among soldiers in peacetime versus out-of-area missions. Mil. Med. 166, 223–225 (2001).
Koch, T. R. & Emory, T. S. Evaluation of chronic gastrointestinal symptoms following Persian Gulf War exposure. Mil. Med. 170, 696–700 (2005).
Wang, W.-F., Guo, X.-X. & Yang, Y.-S. Gastrointestinal problems in modern wars: Clinical features and possible mechanisms. Mil. Med. Res. 2, 15 (2015).
Putnam, S. D. et al. Self-reported description of diarrhea among military populations in operations Iraqi Freedom and Enduring Freedom. J. Travel Med. 13, 92–99 (2006).
Merchant-Borna, K., Rodrigues, E. G., Smith, K. W., Proctor, S. P. & Mcclean, M. D. Characterization of inhalation exposure to jet fuel among US Air Force personnel. Ann. Occup. Hyg. 56, 736–745 (2012).
Braithwaite, M. et al. Armed Forces occupational health—A review. Occup. Med. 59, 528–538 (2009).
Lucertini, M., Lugli, V., Casagrande, M. & Trivelloni, P. Effects of airsickness in male and female student pilots: Adaptation rates and 4-year outcomes. Aviat. Space Environ. Med. 79, 677–684 (2008).
Caldwell, J. A. Fatigue in aviation. Travel Med. Infect. Dis. 3, 85–96 (2005).
Pierce, P. F., Lewandowski-Romps, L. & Silverschanz, P. War-related stressors as predictors of post-deployment health of Air Force women. Women’s Health Issues 21, S152–S159 (2011).
Lancet, T. Jet lag: Trends and coping strategies.
Wu, W. et al. The prevalence of functional gastrointestinal disorders in the chinese air force population. Gastroenterol. Res. Pract. 2013, 1–6 (2013).
Derwa, Y., Gracie, D., Hamlin, P. & Ford, A. Systematic review with meta-analysis: The efficacy of probiotics in inflammatory bowel disease. Aliment. Pharmacol. Ther. 46, 389–400 (2017).
Brown, K., DeCoffe, D., Molcan, E. & Gibson, D. L. Diet-induced dysbiosis of the intestinal microbiota and the effects on immunity and disease. Nutrients 4, 1095–1119 (2012).
Silva, R. A. D. et al. Functional dyspepsia and depression as an associated factor. Arq. Gastroenterol. 43, 293–298 (2006).
Thijssen, A. Y. et al. Dysfunctional cognitions, anxiety and depression in irritable bowel syndrome. J. Clin. Gastroenterol. 44, e236–e241 (2010).
Mahadeva, S. & Goh, K. L. Anxiety, depression and quality of life differences between functional and organic dyspepsia. J. Gastroenterol. Hepatol. 26, 49–52 (2011).
Rayman, R. B. Irritable bowel syndrome: Aeromedical considerations. Aviat. Space Environ. Med. 82, 1061–1063. https://doi.org/10.3357/asem.3107.2011 (2011).
Feijo, D., Luiz, R. R. & Camara, V. M. Common mental disorders among civil aviation flight attendants. Aviat. Space Environ. Med. 85, 433–439. https://doi.org/10.3357/asem.3768.2014 (2014).
Barberio, B., Mahadeva, S., Black, C. J., Savarino, E. V. & Ford, A. C. Systematic review with meta-analysis: Global prevalence of uninvestigated dyspepsia according to the Rome criteria. Aliment Pharmacol. Ther. 52, 762–773. https://doi.org/10.1111/apt.16006 (2020).
Oka, P. et al. Global prevalence of irritable bowel syndrome according to Rome III or IV criteria: A systematic review and meta-analysis. Lancet Gastroenterol. Hepatol. 5, 908–917. https://doi.org/10.1016/s2468-1253(20)30217-x (2020).
Annual report of Chinese civil aviation pilot development 2018. (2018).
Zeevenhooven, J., Koppen, I. J. & Benninga, M. A. The new Rome IV criteria for functional gastrointestinal disorders in infants and toddlers. Pediatric gastroenterology, hepatology & nutrition 20, 1–13 (2017).
Zung, W. W. A self-rating depression scale. Arch. Gen. Psychiatry 12, 63–70 (1965).
Jegede, R. O. Psychometric attributes of the self-rating anxiety scale. Psychol. Rep. 40, 303–306 (1977).
Buysse, D. J., Reynolds, C. F. III., Monk, T. H., Berman, S. R. & Kupfer, D. J. The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Res. 28, 193–213 (1989).
Bassett, D. R. International physical activity questionnaire: 12-country reliability and validity. Med. Sci. Sports Exerc. 35, 1381–1395 (2003).
Pérez Rodrigo, C., Aranceta, J., Salvador, G. & Varela-Moreiras, G. Food frequency questionnaires. Nutr. Hosp. 31(Suppl 3), 49–56. https://doi.org/10.3305/nh.2015.31.sup3.8751 (2015).
Zhang, C. X. & Ho, S. C. Validity and reproducibility of a food frequency Questionnaire among Chinese women in Guangdong province. Asia Pac. J. Clin. Nutr. 18, 240–250 (2009).
Liu, D. et al. Food frequency questionnaire for Chinese children aged 12–17 years: Validity and reliability. Biomed. Environ. Sci. BES 32, 486–495. https://doi.org/10.3967/bes2019.066 (2019).
Wang, Y. M. et al. Geographical variation in nutrient intake between urban and rural areas of Jiangsu province, China and development of a semi-quantitative food frequency questionnaire for middle-aged inhabitants. J. Epidemiol. 13, 80–89. https://doi.org/10.2188/jea.13.80 (2003).
Institute of Nutrition and Food Safety, C. C. China food composition. 2nd edn, (Peking University Medical Press, Peking, 2009).
Institute of Nutrition and Food Safety, C. C. China Food Composition 2004. (Peking University Medical Press, Peking, 2005).
Basilevsky, A. T. Statistical Factor Analysis and Related Methods: Theory and Applications Vol. 418 (Wiley, Hoboken, 2009).
Chang, L. et al. Gender, age, society, culture, and the patient’s perspective in the functional gastrointestinal disorders. Gastroenterology 130, 1435–1446. https://doi.org/10.1053/j.gastro.2005.09.071 (2006).
Mori, H. et al. Gender difference of gastric emptying in healthy volunteers and patients with functional dyspepsia. Digestion 95, 72–78. https://doi.org/10.1159/000452359 (2017).
Kim, Y. S. & Kim, N. Sex-gender differences in irritable bowel syndrome. J. Neurogastroenterol. Motil. 24, 544–558. https://doi.org/10.5056/jnm18082 (2018).
Lovell, R. M. & Ford, A. C. Effect of gender on prevalence of irritable bowel syndrome in the community: Systematic review and meta-analysis. Am. J. Gastroenterol. 107, 991–1000. https://doi.org/10.1038/ajg.2012.131 (2012).
Storms, P. R. & Kinchen, M. J. Gastrointestinal disease in pilots, 2001–2013. Aerosp. Med. Hum. Perform. 87, 122–127 (2016).
Park, J. M. et al. Functional gastrointestinal disorders diagnosed by Rome III questionnaire in Korea. J. Neurogastroenterol. Motil. 17, 279 (2011).
Trivedi, K. H. et al. The impact of post-infectious functional gastrointestinal disorders and symptoms on the health-related quality of life of US military personnel returning from deployment to the Middle East. Dig. Dis. Sci. 56, 3602–3609 (2011).
Bang, C. S. et al. Functional gastrointestinal disorders in young military men. Gut Liver 9, 509 (2015).
Dong, Y.-Y. et al. A school-based study with Rome III criteria on the prevalence of functional gastrointestinal disorders in Chinese college and university students. PLoS ONE 8, e54183 (2013).
Aziz, I., Törnblom, H., Palsson, O. S., Whitehead, W. E. & Simrén, M. How the change in IBS criteria from Rome III to Rome IV impacts on clinical characteristics and key pathophysiological factors. Am. J. Gastroenterol. 113, 1017–1025. https://doi.org/10.1038/s41395-018-0074-z (2018).
Black, C. J., Yiannakou, Y., Houghton, L. A. & Ford, A. C. Epidemiological, clinical, and psychological characteristics of individuals with self-reported irritable bowel syndrome based on the Rome IV vs Rome III criteria. Clin. Gastroenterol. Hepatol. 18, 392-398.e392. https://doi.org/10.1016/j.cgh.2019.05.037 (2020).
AnJiang, W. et al. The clinical overlap between functional dyspepsia and irritable bowel syndrome based on Rome III criteria. BMC Gastroenterol. 8, 43 (2008).
Kaji, M. et al. Prevalence of overlaps between GERD, FD and IBS and impact on health-related quality of life. J. Gastroenterol. Hepatol. 25, 1151–1156 (2010).
Lee, H.-J. et al. Depressive mood and quality of life in functional gastrointestinal disorders: Differences between functional dyspepsia, irritable bowel syndrome and overlap syndrome. Gen. Hosp. Psychiatry 32, 499–502 (2010).
Lee, S. Y., Lee, K. J., Kim, S. J. & Cho, S. W. Prevalence and risk factors for overlaps between gastroesophageal reflux disease, dyspepsia, and irritable bowel syndrome: A population-based study. Digestion 79, 196–201 (2009).
Porter, C. K., Gormley, R., Tribble, D. R., Cash, B. D. & Riddle, M. S. The incidence and gastrointestinal infectious risk of functional gastrointestinal disorders in a healthy US adult population. Am. J. Gastroenterol. 106, 130 (2011).
Jang, S. H., Ryu, H. S., Choi, S. C. & Lee, S. Y. Psychological factors influence the overlap syndrome in functional gastrointestinal disorders and their effect on quality of life among firefighters in South Korea. J. Dig. Dis. 17, 236–243 (2016).
Bai, T. et al. Comparison of the Rome IV and Rome III criteria for IBS diagnosis: A cross-sectional survey. J. Gastroenterol. Hepatol. 32, 1018–1025. https://doi.org/10.1111/jgh.13642 (2017).
Anand, A., Sashindran, V. & Mohan, L. Gastrointestinal problems at high altitude. Trop. Gastroenterol. 27, 147 (2006).
Gibson, T. Flying in Hunter’s Diseases of Occupational Medicine. 361–382 (Arnold, London, 2000).
Muhm, J. M. et al. Effect of aircraft-cabin altitude on passenger discomfort. N. Engl. J. Med. 357, 18–27 (2007).
Jeziorek, M., Frej-Mądrzak, M. & Choroszy-Król, I. The influence of diet on gastrointestinal Candida spp colonization and the susceptibility of Candida spp. to antifungal drugs. Roczniki Państwowego Zakładu Higieny 70, 195–200 (2019).
David, L. A. et al. Diet rapidly and reproducibly alters the human gut microbiome. Nature 505, 559 (2014).
Koloski, N. A. et al. The brain–gut pathway in functional gastrointestinal disorders is bidirectional: A 12-year prospective population-based study. Gut 61, 1284–1290 (2012).
Acknowledgements
The authors gratefully acknowledge Financial support for this work provided by Research Grants No. 81803328 and No. 81773540 from National Natural Science Foundation of China, and No. 2018ZDXM-SF-047 and No. 2020SF-282 from Social Development Major Project of Shaanxi Province in China.
Author information
Authors and Affiliations
Contributions
L.S. and X.J. conceived the idea for the study and oversaw all aspects of protocol development and final review; C.L. and J.X. contributed to drafting of the study equally; C.L., D.Y. and D.S. contributed to the analysis and the interpretation of data for the work; Y.Z. edited and commented for important intellectual content of the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Li, C., Xu, J., Yin, D. et al. Prevalence and trigger factors of functional gastrointestinal disorders among male civil pilots in China. Sci Rep 11, 2021 (2021). https://doi.org/10.1038/s41598-021-81825-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-81825-0
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.