Abstract
In head and neck cancer, early detection of recurrence after treatment is important. The contemporary development of therapeutic agents have improved the prognosis after recurrence; however, no biomarker has been established for evaluating therapeutic effects or detecting recurrence. Recently, circulating tumor DNA (ctDNA), which comprises DNA derived from tumor cells and exists in the form of cell-free DNA in the blood, has attracted attention as a minimally invasive and repeatable biomarker for detecting cancer. We validated the usefulness of ctDNA of human papilloma virus (HPV)-derived sequences as a biomarker in HPV-related p16-positive oropharyngeal cancer by assessing 25 patients with p16-positive oropharyngeal cancer. Blood samples were collected from each patient at multiple time points during the treatment, and the plasma was preserved. The ctDNA was extracted from the plasma and analyzed using digital polymerase chain reaction. HPV-derived ctDNA was detected in 14 (56%) of the 25 patients. In all the patients, the samples were found to be ctDNA-negative after initial treatment. Cancer recurrence was observed in 2 of the 14 patients; HPV-derived ctDNA was detected at the time of recurrence. Our results indicate that HPV-derived ctDNA can be a prospective biomarker for predicting the recurrence of p16-positive oropharyngeal cancer.
Similar content being viewed by others
Introduction
Head and neck cancers are often diagnosed at the first visit as advanced cancers. Despite intensive treatment using multidisciplinary therapy, residual disease after the treatment and metastatic recurrence are common. Recently, such cases have been treated with molecular-targeted drugs and immune checkpoint inhibitors, which can prolong overall and progression-free survival and improve quality of life, making the early detection of recurrence more important1. However, there are no established biomarkers for determining the response to treatment or for detecting recurrence; therefore, the detection of recurrence still relies on follow-up by palpation and imaging2.
In recent years, circulating tumor DNA (ctDNA) has become a new biomarker for various cancers. ctDNA consists of DNA derived from tumor cells and exists in the blood in the form of cell-free DNA. The detection of ctDNA in blood not only enables quantitative estimation of the presence or absence of tumors and the degree of tumor progression but also provides genomic information such as specific genetic mutations in tumors. Because less than 10 mL of blood is sufficient for ctDNA analysis, it has attracted attention as a new biomarker that can be collected both noninvasively and repeatedly3.
Oropharyngeal cancer can be divided into two categories: one is a p16-negative tumor caused by loss of tumor suppressor gene, p16; the other is a p16-positive tumor caused by the integration of human papilloma viruses (HPVs), type 16 or 18. Given that HPV DNA is only integrated into p16-positive oropharyngeal cancer in the human body, exogenous HPV-derived DNA sequences can provide an ideal target for detecting ctDNA specific to the p16-positive oropharyngeal cancer.
In this study, we aimed to validate the usefulness of ctDNA by targeting HPV-derived DNA sequences as a biomarker in HPV-related, p16-positive oropharyngeal cancer. In p16-positive oropharyngeal cancer, HPV-derived ctDNA in patients with head and neck cancers has been reported using digital polymerase chain reaction (PCR)4, which is more sensitive than conventional real-time PCR.
Methods
We included 25 patients diagnosed with p16-positive oropharyngeal cancer who underwent initial treatment in our department in the University of Tokyo Hospital between January 2017 and December 2018 and provided written informed consent. The patients comprised 22 men and 3 women, and the mean age was 66 years (range, 46–80 years; median, 66 years). The mean observation period was 15 months (range, 3–24 months; median, 16 months). As a negative control, we included four patients who had been diagnosed with nasopharyngeal cancer, which was not associated with HPV integration. This study was approved by the Ethics Committee of the University of Tokyo Hospital [Review No. G10112-(1)], and all the experiments were performed in accordance with relevant guidelines and regulations.
Extraction of cell-free DNA from blood samples
At multiple time points during the course of treatment, we collected an additional 10 mL of blood in addition to samples for routine medical practice. Blood was collected in ethylenediaminetetraacetic acid (EDTA)-containing tubes and centrifuged at 3000 rpm for 10 min at 4 °C followed by 4000 rpm for 10 min within 4 h from blood collection. The supernatant of approximately 4 mL was stored as plasma at − 20 °C. We extracted 50 µL of cell-free DNA solution from 1 mL aliquots of plasma using the Maxwell® RSC ccfDNA Plasma Kit (Promega).
Digital PCR
We used the Taqman probe, which is typically employed in real-time PCR, and prepared the primers and probe sets targeting the specific regions of E6 and E7 of the HPV viral DNA which were integrated into cancer DNA (HPCL purification, Integrated DNA Technology, Inc.) (Table 1). We performed digital PCR using the QX200™ Droplet Digital™ PCR System (Bio-Rad). The reaction solution was prepared by mixing 8 µL aliquots of cell-free DNA solution extracted from plasma, 2 µL of primer and probe solution, and 10 µL of buffer and was converted into approximately 20,000 droplets floating in oil using a droplet generator (Bio-Rad). The PCR reaction was subsequently carried out in a T100™ Thermal Cycler (Bio-Rad); the fluorescence intensity of each droplet was measured and analyzed using a QX200™ Droplet Reader (Bio-Rad). If both E6- and E7-derived sequences were detected, it was judged as ctDNA positive. We used the Ribonuclease P/MRP Subunit P30 (RPP30) gene as a control DNA sequence, and the ratio of the number of the droplets with E6-positive droplets divided by the number of RPP30-positive droplets was used as the ctDNA value.
We used the Fisher exact test and Kruskal–Wallis test to determine significant differences. A p value of < 0.05 was considered significant.
Results
Among the 25 patients, 19 were at clinical stage I, 1 was stage II, 3 were stage III, and 2 were stage IV, according to the 8th edition of the American Joint Committee on Cancer/International Union against Cancer classification. Treatment primarily consisted of surgery for 11 patients and radiotherapy for 14 patients. Induction chemotherapy was performed in one of the surgical cases and in six of the radiotherapy cases. Complete response (CR) was achieved in all patients after the first treatment.
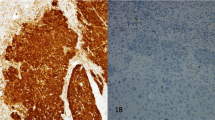
Pretreatment ctDNA was positive in 14 cases, with a positivity rate of 56%, and we found no significant differences in clinical indices such as clinical stage between ctDNA-positive and ctDNA-negative cases (Table 2). In all 14 pretreatment ctDNA-positive cases, ctDNA had become negative after treatment (Fig. 1). Among these cases, 2 developed a tumor recurrence, for whom ctDNA became positive again at the time of the recurrence. Positive and negative results in digital PCR for HPV-E6 and E7 amplification were consistent in all 25 cases. In all four negative control cases, ctDNA was negative.
Case presentation
Case 1: lateral wall cancer, T1N1, stage III
This patient was ctDNA positive before the start of treatment and underwent resection of the primary lesion with neck dissection on the affected side in September 2017. Pathological examination indicated negative results for surgical margins and the absence of extranodal extension. The ctDNA became negative after this surgical treatment. The primary tumor recurred in August 2018, and ctDNA became positive again. Concomitant chemoradiotherapy with CDDP resulted in CR, and ctDNA became negative again (Fig. 2).
(a) Pretreatment computed tomography (CT) image shows the tumor (asterisk) at the right lateral wall of the oropharynx. (b) Magnetic resonance imaging scan after initial treatment shows complete response. (c) CT image shows the local recurrence of the tumor (arrow) at the right lateral wall of the oropharynx. (d) The pretreatment circulating tumor DNA (ctDNA) was positive and became negative after initial treatment with surgery. ctDNA was positive again at the time of local recurrence and turned negative again after concomitant chemoradiotherapy with CDDP.
Case 2: lateral wall cancer, T4N2c, stage IV
The patient was ctDNA positive before the start of treatment. In March 2018, the patient underwent concomitant chemoradiation with CDDP for a primary lesion that extended from the oropharynx to the larynx. At the end of treatment, ctDNA became negative. In October 2018, local recurrence was observed at the larynx and multiple lung metastases, and the ctDNA became positive again. Despite immune checkpoint inhibitor therapy with nivolumab, the disease was progressive, and the ctDNA remained positive (Fig. 3).
(a) Pretreatment computed tomography (CT) image shows the tumor (asterisk) extending from the right lateral wall to the anterior wall of the oropharynx and cervical node metastasis (arrows). (b) CT image after initial treatment shows complete response. (c) CT image shows multiple lung metastases (triangles). (d) The pretreatment circulating tumor DNA (ctDNA) was positive and turned negative after initial treatment with concomitant chemoradiotherapy with CDDP; ctDNA was positive again at the time of local and distant recurrence and remained positive despite the administration of immune checkpoint inhibitor therapy with nivolumab.
Discussion
To investigate the usefulness of ctDNA as a biomarker in head and neck cancer, we measured HPV-derived ctDNA in p16-positive oropharyngeal cancer patients during the course of treatment and compared the results to the clinical course. ctDNA was detected in 14 of 25 (56%) patients, and all patients became negative for ctDNA after the initial treatment. Relapse occurred in 2 of 14 patients, and ctDNA was detected in the blood at the time of relapse for both patients, indicating that ctDNA changes reflected the clinical course of these patients.
Biomarkers are biological substances, such as proteins and DNA, found in tissues or body fluids (e.g., blood and urine) that are correlated with the state of disease and serve as indicators of treatment response. For malignant tumors, biomarkers are used clinically in one of two ways: (1) for the prediction of the treatment effect and (2) for the evaluation of disease activity. As an example of the former, the presence or absence of an epidermal growth factor receptor (EGFR) mutation is used to predict the efficacy of EGFR antagonists in non-small-cell lung cancer5; for the latter, prostate-specific antigen levels in the blood are used to evaluate disease activity in prostate cancer6. In head and neck cancers, the neutrophil-to-lymphocyte ratio7, albumin level, and C-reactive protein level in the blood have recently attracted attention as biomarkers for the prediction of therapeutic efficacy and prognosis but are currently used only for reference. The blood thyroglobulin level in papillary thyroid carcinoma and blood calcitonin and carcinoembryonic antigen level in medullary carcinoma are useful biomarkers for the evaluation of disease activity, but no effective biomarker has been established for squamous cell carcinoma.
The importance of ctDNA has attracted attention since 1994, when DNA fragments with RAS mutations were detected in the blood of patients with various cancers8,9. The KRAS mutations in pancreatic cancer and the KRAS and TP53 mutations in colorectal cancer have been detected in ctDNA, and clinical applications are presently underway10. Sequencing analysis can also be performed, which not only predicts the tumor’s quantitative state but also provides genomic information. When multiple cancer lesions are present, each lesion may contain a differently altered tumor genome, and biopsies performed from a single location may provide biased information. In addition, the tumor genome is known to change during the course of treatment, but repeated tissue biopsies are invasive and are associated with a high burden. ctDNA provides comprehensive genomic information of the entire tumor and is easy to repeat; thus, it has attracted considerable attention as a liquid biopsy.
Weng et al. reported that HPV-derived ctDNA was detected in 41 of 47 (87%) cases of head and neck squamous cell carcinoma and in 18 of 21 (86%) cases of HPV-related cancer11. Chera et al. reported that HPV-derived ctDNA was detected in 84 of 103 (82%) HPV-related oropharyngeal cancers12. In the current study, the sensitivity of ctDNA was 56%, which was lower than those reported by the two aforementioned studies. However, after the completion of the first treatment, all the positive cases became negative, and repositivity was detected at the time of recurrence, suggesting that ctDNA is useful as a biomarker. The storage conditions of the blood samples might be a potential cause for the low sensitivity. In the present study, blood collection for ctDNA and regular clinical examination was often performed early in the morning, and in some cases, a maximum of 4 h had passed before the collected blood was stored as plasma, although the half-life of ctDNA is shown to be relatively short, ranging from 16 min to 2.5 h13. Furthermore, as a result of destruction, the intracellular DNA of normal blood cells might have leaked into the specimen, making trace amounts of ctDNA undetectable. Because the sensitivity of ctDNA was lower than expected, we attempted to shorten the time from blood collection to processing as much as possible in the latter half of the study period. In the first half of the study period, 6 of 13 (47%) specimens were positive for ctDNA, whereas in the second half, 8 of 12 (67%) specimens were positive, which suggests the importance of the time required for specimen processing. Based on previous reports, we used blood collection tubes containing EDTA, which are used clinically for blood typing; however, we expect the detection rate to be improved with the use of tubes specified for cell-free DNA extraction. These tubes might not affect specimens that are processed immediately after collection in research phases substantially, but for clinical applications, the use of dedicated blood collection tubes is desirable because of the time elapsed from blood collection to storage.
ctDNA analysis can be broadly divided into two methods: one by PCR and the other by sequencing analysis. The digital PCR used herein is an analytical method that applies the PCR reaction, and it has attracted attention as a third-generation PCR that enables absolute quantification following conventional PCR for qualitative analysis and real-time PCR for relative quantification14. The PCR reaction is performed after dividing the reaction solution in which the primer and probe are mixed into many micro compartments of approximately 20,000 by transforming the solution into fine droplets. By keeping the concentration of the template DNA sufficiently low, each compartment contains one or zero molecules of DNA, and the amplification reaction occurs only within the droplets that contain the target sequence, and fluorescence is emitted. By analyzing the fluorescence intensity of all the droplets and measuring the percentage of positive droplets, the concentration of the target can be quantified in absolute terms. In particular, with respect to mutations of a low frequency, it is difficult to detect mutations of less than 1% using conventional real-time PCR; however, with digital PCR, it is possible to detect mutations of 0.001%, which is useful for ctDNA analysis that exists in only small amounts15.
The use of sequencing analysis can provide not only quantitative information but also genomic information, as described previously16,17. PCR-based methods require knowledge regarding the tumor-specific genetic abnormalities to be targeted. In cases of head and neck cancers in which there are almost no specific genetic mutations except for p16-positive oropharyngeal and Epstein–Barr virus (EBV)-positive nasopharyngeal cancers, identifying genetic abnormalities is necessary. However, this is not required in sequencing analysis, and the creation of primers and probes is also not needed, which makes the testing process considerably simple. Nevertheless, the cost of sequencing analysis is high, obtaining results requires a substantial amount of time, and specialized knowledge is required to analyze the obtained data.
In this study, we aimed to establish a new biomarker for head and neck cancer using digital PCR. We targeted p16-positive oropharyngeal cancer, for which the target gene abnormality has been established and detected in blood. EBV-positive nasopharyngeal cancer and thyroid cancer would be similarly applicable. We expect ctDNA to be applied in the future to other head and neck cancers through the use of sequencing analysis to identify and target individual tumor-specific genetic abnormalities.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author upon reasonable request.
References
Ferris, R. L. et al. Nivolumab for recurrent squamous-cell carcinoma of the head and neck. N. Engl. J. Med. 375, 1856–1867. https://doi.org/10.1056/NEJMoa1602252 (2016).
Payne, K. et al. Circulating tumor DNA as a biomarker and liquid biopsy in head and neck squamous cell carcinoma. Head Neck 40, 1598–1604. https://doi.org/10.1002/hed.25140 (2018).
Wan, J. C. M. et al. Liquid biopsies come of age: Towards implementation of circulating tumour DNA. Nat. Rev. Cancer 17, 223–238. https://doi.org/10.1038/nrc.2017.7 (2017).
Biron, V. L. et al. Detection of human papillomavirus type 16 in oropharyngeal squamous cell carcinoma using droplet digital polymerase chain reaction. Cancer 122, 1544–1551. https://doi.org/10.1002/cncr.29976 (2016).
Lynch, T. J. et al. Activating mutations in the epidermal growth factor receptor underlying responsiveness of non-small-cell lung cancer to gefitinib. N. Engl. J. Med. 350, 2129–2139. https://doi.org/10.1056/NEJMoa040938 (2004).
Greene, K. L. et al. Prostate specific antigen best practice statement: 2009 update. J. Urol. 189, S2–S11. https://doi.org/10.1016/j.juro.2012.11.014 (2013).
Takenaka, Y. et al. Prognostic role of neutrophil-to-lymphocyte ratio in head and neck cancer: A meta-analysis. Head Neck 40, 647–655. https://doi.org/10.1002/hed.24986 (2018).
Sorenson, G. D. et al. Soluble normal and mutated DNA sequences from single-copy genes in human blood. Cancer Epidemiol. Biomark. Prev. 3, 67–71 (1994).
Vasioukhin, V. et al. Point mutations of the N-ras gene in the blood plasma DNA of patients with myelodysplastic syndrome or acute myelogenous leukaemia. Br. J. Haematol. 86, 774–779. https://doi.org/10.1111/j.1365-2141.1994.tb04828.x (1994).
Schwarzenbach, H., Hoon, D. S. B. & Pantel, K. Cell-free nucleic acids as biomarkers in cancer patients. Nat. Rev. Cancer 11, 426–437. https://doi.org/10.1038/nrc3066 (2011).
Wang, Y. et al. Detection of somatic mutations and HPV in the saliva and plasma of patients with head and neck squamous cell carcinomas. Sci. Transl. Med. 7, 293104. https://doi.org/10.1126/scitranslmed.aaa8507 (2015).
Chera, B. S. et al. Rapid clearance profile of plasma circulating tumor HPV type 16 DNA during chemoradiotherapy correlates with disease control in HPV-associated oropharyngeal cancer. Clin. Cancer Res. 25, 4682–4690. https://doi.org/10.1158/1078-0432.CCR-19-0211 (2019).
Fleischhacker, M. & Schmidt, B. Circulating nucleic acids (CNAs) and cancer—a survey. Biochim. Biophys. Acta 1775, 181–232. https://doi.org/10.1016/j.bbcan.2006.10.001 (2007).
Vogelstein, B. & Kinzler, K. W. Digital PCR. Proc. Natl. Acad. Sci. U.S.A. 96, 9236–9241. https://doi.org/10.1073/pnas.96.16.9236 (1999).
Bharuthram, A., Paximadis, M., Picton, A. C. P. & Tiemessen, C. T. Comparison of a quantitative real-time PCR assay and droplet digital PCR for copy number analysis of the CCL4L genes. Infect. Genet. Evol. 25, 28–35. https://doi.org/10.1016/j.meegid.2014.03.028 (2014).
Diaz, L. A. Jr. & Bardelli, A. Liquid biopsies: Genotyping circulating tumor DNA. J. Clin. Oncol. 32, 579–586. https://doi.org/10.1200/jco.2012.45.2011 (2014).
Lanman, R. B. et al. Analytical and clinical validation of a digital sequencing panel for quantitative, highly accurate evaluation of cell-free circulating tumor DNA. PLoS One 10, e0140712. https://doi.org/10.1371/journal.pone.0140712 (2015).
Acknowledgements
The authors would like to thank the members of the Department of Otolaryngology and Head and Neck Surgery, Graduate School of Medicine, University of Tokyo Hospital and the Division of Molecular Pathology, Institute of Medical Science, University of Tokyo for their constructive criticism and fruitful discussion. The authors also thank Enago (http://www.enago.jp) for the English language review. This work was supported in part by JSPS KAKENHI Grant Numbers JP16H06759 and JP18K16833.
Author information
Authors and Affiliations
Contributions
K.A. conceived and planned the experiments in consultation with all authors. K.A., T.S., O.F., Y.S., M.Y. and M.A. contributed to sample collection and preparation. K.A., T.I. and Y.M. contributed to interpretation of the results and analysis of the data. T.Y. helped supervise the project. Ken Akashi wrote the main manuscript text and prepared all figures and tables. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Akashi, K., Sakai, T., Fukuoka, O. et al. Usefulness of circulating tumor DNA by targeting human papilloma virus-derived sequences as a biomarker in p16-positive oropharyngeal cancer. Sci Rep 12, 572 (2022). https://doi.org/10.1038/s41598-021-04307-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-04307-3
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.