Abstract
The automated blister epidermal micrograft (ABEM) is a newly introduced surgical transplantation for refractory vitiligo. Comparative analysis of other surgical methods is lacking. We conducted a retrospective study to compare the efficacy, safety, and experience of ABEM with conventional suction blister epidermal graft (SBEG). A total of 118 anatomically based vitiligo lesions from 75 patients were included. The primary outcome was the degree of repigmentation; the patient and operator experience were evaluated. SBEG had a significantly greater incidence of repigmentation (p < 0.001), as measured by the Physician Global Assessment, as well as improvements in the Vitiligo Area Scoring Index, particularly on the face/neck area (p < 0.001). ABEM, on the contrary, had reduced donor harvest time, a better patient operative experience, and more significant Dermatology Life Quality Index improvements. In a subgroup of 38 lesions from ten patients who received both SBEG and ABEM concomitantly, there was no difference in the degree of repigmentation in the same recipient area. Overall, the degree of repigmentation for SBEG is higher than ABEM, especially in the mobilized region, and the cost is less expensive. On the contrary, ABEM requires less procedure learning curve and can supply a greater transplanting zone with shorter donor site recovery. Understanding the benefits and drawbacks of two blister grafting procedures is essential for optimal surgical outcomes for vitiligo grafting.
Similar content being viewed by others
Introduction
Vitiligo is an acquired depigmentation of the skin caused by the complete loss of melanocytes. It affects approximately 0.5 to 2 percent of the general population1. The characteristic clinical features are white macules and patches with sharply circumscribed but irregular borders. Various modalities, both conventional and alternative, non-surgical and surgical, are used in the treatment. Vitiligo has a detrimental effect on a patient's quality of life due to social stigma and comorbidities2,3,4,5,6.
Vitiligo is one of the most complex dermatological conditions to manage. The recommended first-line treatment is topical steroids, either alone or in combination with topical calcineurin inhibitors1,7. Systemic steroids or immunosuppressants are used to halt the autoimmune destruction for rapidly progressive unstable lesions. Narrowband ultraviolet B phototherapy and monochromatic excimer laser can enhance melanocyte regeneration and immunomodulatory effect1,7. Patients suffering from stable recalcitrant lesions that have not responded to non-surgical methods may opt for surgical treatment using melanocyte transplant techniques1,7. The two most common types of procedures are tissue grafts and cellular grafts. Melanocyte-rich tissue grafting includes full-thickness, split-thickness, and suction blister grafts7,8,9. A novel automated epidermal harvesting technique that induces blister epidermal micrograft formation is now commercially available10.
This study aims to compare conventional suction blister epidermal graft (SBEG) with automated blister epidermal micrograft (ABEM) technique for patients with stable vitiligo in terms of efficacy, safety, and patient and operator experience. In addition, anatomical areas, including the face, trunk, limbs, and acral parts, were also analyzed. To our knowledge, this is the first study that compares two blister epidermal graft surgical methods for the treatment of stable vitiligo.
Methods
Study design
We conducted a retrospective comparative trial from January 2017 to December 2020 in the Dermatology Department of Chang Gung Memorial Hospital, Linkou, Taoyuan, Taiwan. The protocol was approved by the Chang Gung Medical Foundation Institutional Review Board (No.: 202100274B0) before the initiation of the study. All of the research was carried out in accordance with the applicable rules and regulations.
Patient selection
Patients were recruited from the practice of a single dermatologist in a tertiary medical center. The study included patients with stable vitiligo (both segmental and nonsegmental) who failed to respond to other therapies in the past two years. Stable vitiligo was defined as no deterioration of old lesions and no new lesions within a year. Exclusion criteria included keloidal tendency, active infections, pregnancy, lactation, bleeding diathesis, or any sign of unstable disease (inflammatory or poorly defined border, confetti-like or pentachrome lesion, and Koebner phenomenon). The efficacy and safety of ABEM in segmental and non-segmental vitiligo from the same patients in this study has been investigated and reported in the literature11.
Suction blister epidermal graft (SBEG)
Suction blister epidermal grafting is a low-cost, high-effective technique that results in complete repigmentation in 68–70% of cases12,13. This method requires creating a subepidermal bulla from the donor site by prolonged vacuum application; then, the roof is surgically removed and transplanted to the recipient site. A suction syringe without a plunger is applied to generate constant negative pressure on the donor site through a 3-way connector. An infrared lamp as a heating source was used to shorten the blistering time. The recipient site was prepared by ablation with Erbium: Yttrium–aluminium-garnet (Er: YAG) laser (ProFractional™, Sciton Inc., California, USA) with a 2-mm spot-sized handpiece at the average fluence of 6.3 J/cm2 for optimal graft adherence and uptake. The graft was then transferred after being modified to the proper size and shape and wrapped with a hydrocolloid dressing.
Automated blister epidermal micrograft (ABEM)
The automated blister epidermal micrograft (CelluTome™; Kinetic Concepts, Inc., ACELITY Company, San Antonio, Texas) is a novel option, allowing patients to receive pain-free epidermal skin grafts with reduced donor site trauma (Fig. 1)14,15. With a negative pressure of − 400 to − 500 mmHg and a temperature of 37 to 41 °C, the device automatically produces suction micro domes and harvests epidermal micrografts with an area of 20–25 cm214,15. A silicone-coated nonadherent dressing (Adaptive Touch™, Systagenix, ACELITY Company, Gargrave, UK) was used to transfer the epidermal micrografts perforated design helps fluid to drain from the micro blisters16. After preparing the recipient site with Er: YAG laser ablation, the graft was transferred to the recipient site and wrapped with a hydrocolloid dressing. All patients with ABEM and SBEG received topical tacrolimus 0.1% ointment after grafting procedure. 64% (36/56 anatomical based lesion) with ABEM grafting and 55% (34/62 anatomical based lesion) received excimer light and/or narrow band UVB phototherapy at least once per week after grafting.
Outcome measures
The primary outcome measure was the degree of repigmentation per lesion. The rate of repigmentation, identified as the area of pigments at the recipient site one year after initial treatment, was graded as very good (≥ 75%), good (50–74%), fair (25–49%), and poor (0–24%) using a Physician Global Assessment (PGA) scale. In addition, improvement in Vitiligo Area Scoring Index (VASI), a quantitative parametric score developed by Hamzavi et al., was used to assess the efficacy17. The secondary outcome measure was the patient and operator experience evaluated by operative conditions, pain score, and change in the Dermatology Life Quality Index (DLQI)18. Adverse event was monitored and recorded.
Statistical analysis
Data were analyzed using the R software (R version 3.6.2, 2019 copyright: The R Foundation for Statistical Computing). The descriptive statistic was showed by mean, standard deviation (SD) for continuous variable and count, % for categorical variable.
To compare the results, we used paired sample t-test, chi-square × 2 tests, or Fisher exact tests to compare the difference between various groups. A p-value less than 0.05 was considered statistical significance.
Ethics approval statement
Reviewed and approved by Chang Gung Medical Foundation IRB; approval #202100274B0.
Patient consent of publication statement
We obtained written informed consent from all participants.
Results
In the study, 118 anatomically based lesions from 75 patients with stable vitiligo were enrolled. 62 lesions received conventional suction blister epidermal graft (SBEG), and 56 lesions receiving automated blister epidermal micrograft (ABEM) (Table 1). Their mean age was 34.17 years (range 7–70). The vitiligo lasted an average of 5.89 ± 7.79 years while remaining stable for an average of 4.14 ± 7.12. Patients are all Asians with Fitzpatrick skin types III to IV. The treatment area of ABEM was more extensive than that of SBEG (ABEM 20.09 ± 0.67 cm; SBEG 8.94 ± 5.70, p < 0.001). There were no significant variations between the two groups regarding gender, age, presentation patterns, underlying autoimmune disease, disease duration, disease stability, initial Dermatology Life Quality Index (DLQI), and the initial Vitiligo Area Scoring Index (VASI). The face and neck (74%) were the most commonly grafted area, followed by the trunk (9%) and non-acral limbs (9%).
For the degree of repigmentation after grafting according to the PGA scale, 47 (76%) of the lesions in the SBEG group were scored as very good (≥ 75%); 5 (8%) as good (50–74%); 1 (2%) as fair (25–49%); and 9 (15%) as poor (0–24%) (Table 2). In the ABEM group, 22 (39%) of the lesions were scored as very good; 12 (21%) as good; 13 (23%) as fair; and 9 (16%) as poor. The degree of repigmentation in the ABEM group is significantly lower than in the SBEG group (p < 0.001). When comparing the VASI from baseline, the SBEG group showed significantly more improvement than the ABEM group (p < 0.001). According to the subgroup analysis based on body parts, the changes in VASI were more profound in the SBEG group on the face/neck region compared to ABEM. At the same time, no difference was observed on the trunk, non-acral limbs, or acral area.
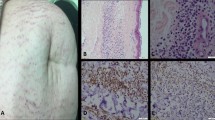
Patient and operator experience
ABEM took significantly less time to harvest the blisters (SBEG: 74.74 ± 23.93 min, ABEM: 48.39 ± 21.07 min, p < 0.001) and to complete the whole procedure (SBEG: 112.87 ± 29.89 min, ABEM: 75.9 ± 27.93 min, p < 0.001) than SBEG (Table 3). The Visual Analogue Scale 10-point score for pain directly after the operation of ABEM was significantly lower than SBEG (SBEG: 5.39 ± 1.32, ABEM: 4.75 ± 1.10, p = 0.004). The duration of hyperpigmentation at the donor site was significantly longer in the SBEG group when comparing with the ABEM group (SBEG: 13.71 ± 5.51 months, ABEM: 3.54 ± 2.17 months, p < 0.001) (Fig. 2). Scar formation occurred in two participants who underwent SBEG, and no scarring event was found in patients treated with ABEM. No side effects such as cobble-stoning and the Koebner phenomenon were found. Interestingly, although the degree of repigmentation was better with SEBG, the improvement of DLQI was more profound in the ABEM group (p = 0.002).
The donor site of a patient received all three procedures: SBEG, ABEM, and punch graft. (A) SBEG donor sites showed prolonged hyperpigmentation (12 months postoperatively, black arrow) in comparison to ABEM donor sites (third months postoperatively, white arrow) and scarring in punch graft (18 months postoperatively, asterisk). (B) (i) Immediate wound at the donor site of SBEG, a hematoma is sometimes noticed (ii) One week after surgery, some shallow abrasions are still visible. (C) (i) Immediate wound at the donor site of ABEM (ii) One week after surgery, wound healed entirely.
Patients received concomitant SBEG and ABEM
Thirty-eight anatomical-based lesions from ten patients underwent SBEG and ABEM treatments concomitantly, with 13 lesions receiving SBEG and 25 receiving ABEM (Table 4). The rate of repigmentation according to the PGA scale (p = 0.293) and the difference in VASI from baseline (p = 0.342) were not significant between the two groups. SBEG took a longer time to complete the entire process than ABEM (p = 0.051). For patient experience and donor side effects, the patient reported a higher pain score with SBEG (p < 0.001) and had prolonged hyperpigmentation at the donor site compare to ABEM (SBEG: 13.65 ± 5.28 months, ABEM: 3.40 ± 0.91 months, p < 0.001).
Discussion
Vitiligo is a common autoimmune skin disorder in which T-cells destroy melanocytes, resulting in depigmentation. It can lead to many social stigmas, which have a negative impact on one's mental health, including low self-esteem, a negative body image, and a substantial psychosocial burden4,6. Surgical therapies benefit stable vitiligo that failed to respond to medical treatment. SBEG is one of the most accessible and reliable surgical interventions available19. ABEM, a commercialized blister epidermal micrograft that automatically applies both heat and suction to the donor site, has been shown to reduce procedure time, minimize discomfort, and enhance the quality of life in a preliminary study15,20. Understanding the distinctions between various forms of vitiligo surgery and the benefits and drawbacks of each procedure are crucial for optimal surgical results.
We report a comparative study for refractory stable vitiligo treated with conventional SBEG versus ABEM. In our study, 83.87% of patients receiving SBEG achieved good to very good results (≥ 50% repigmentation), and 75.81% achieved very good results (≥ 75% repigmentation), which is comparable to the degree of repigmentation in a meta-analysis by Ju et al.19 In this study, SBEG was shown to be more effective than ABEM in terms of the degree of repigmentation as measured by PGA scale repigmentation rates and the difference in VASI from baseline. Based on our experience, this is caused by difficulties in fixation of the silicone-coated nonadherent dressing to the recipient site, particularly around lips, eyelids, and bony prominences. A subgroup analysis based on body parts supported this concept, revealing that the alterations in VASI were more pronounced in the SBEG group on the face/neck region than in the ABEM group. We also noticed that acral areas in both groups had the least amount of pigmentation spread, consistent with previous studies21. An optimal outcome may be achieved by developing or finding a more flexible and adhesive dressing that enhances proper fixation.
In terms of operator experience, ABEM took significantly less time to harvest the blisters and complete the procedure than SBEG, making it more convenient and appropriate for ambulatory surgery. It allows reduced operation time, which is beneficial for both operators and patients, especially children who cannot withstand long harvesting. SBEG, on the other hand, takes longer and is less suitable for broad achromic surfaces. The rounded blisters collected from SBEG must be tailored to the vitiligo area, which is sometimes uneven in shape and can result in graft waste. Furthermore, the quality of harvested blister is occasionally unpredictable, and the operator needs to pay close attention to the orientation of blisters to avoid engraftment problems caused by upside-down grafting. The ABEM contains micrografts aligned on silicone dressing that can be readily tailored to match the shape of the transplanted area and generate 20–25 cm2 of area in a single harvesting. Hence, the treatment area for each grafting with ABEM is larger than of SBEG.
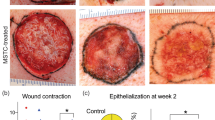
In addition, when compared to SBEG, ABEM had better donor side outcomes, with patients experiencing significantly fewer side effects such as pain, donor site hyperpigmentation, and scarring. In ABEM, dotted repigmentation from the micrografts can be observed within one month and gradually expand centrifugally. Over time, the repigmentation confluent into a more homogenous pattern to cover the recipient area, with an optimal result at around a year after grafting (Fig. 3). On the contrary, the SBEG grafts are designed to cover the recipient area completely; hence, the repigmentation requires less time to cover the entire recipient area completely.
(A) Before surgery: A 5 × 4 cm2 depigmented patch in a 26 years-old stable, nonsegmental vitiligo patient who failed to respond to medical and excimer laser therapy. (B) One month after ABEM, dotted repigmentation corresponds to the micro-blister graft. (C) Three months after ABEM, the dotted repigmentation confluent into a patch with constant improvement over time.
Surprisingly, despite the fact that SBEG had a superior degree of repigmentation and is less expensive, the ABEM reported a more significant improvement in life quality. This result may be due to improved operational experience and fewer negative consequences on the donor side. When we looked at patients who had undergone both procedures, we discovered that ABEM took less time and had fewer side effects than SBEG. Furthermore, our beliefs often affect how we experience medical treatment. The subject-expectancy effect of a better outcome due to ABEM's higher price may explain this discrepancy22,23. ABEM has a higher yield of graft area (20–25 cm2) per harvest than SBEG, making it suitable for a larger recipient area. In the intra-individual study, there was little difference in repigmentation efficacy between SBEG and ABEM. Therefore, ABEM can be an alternative for individuals seeking a less painful and more convenient treatment modality. Furthermore, combining the two treatments to optimize the surgical outcome may be an option (Fig. 4).
There are some limitations to this study. The results are limited to a single operator in a tertiary medical center. Besides, this is a retrospective comparative study. Future randomized and split-control investigations are needed to confirm the findings of this study.
Conclusion
To the best of our knowledge, this is the first study directly comparing the effect and safety for SBEG and ABEM. We found that stable vitiligo treated with SBEG had a significantly higher repigmentation rate than those treated with ABEM, particularly around lips, eyelids, and bony prominences. SBEG should be used on the face and neck because of its better efficacy and cost-effectiveness. ABEM, on the contrary, has some advantages, including better blister quality, a higher yield of graft area (20–25 cm2) at a single harvest, and a better operational experience, which includes a shorter procedure time, fewer donor side problems (scarring, prolonged hyperpigmentation), and improved quality of life. Understanding the benefits and drawbacks of two blister grafting methods is crucial for optimal surgical results.
References
Bergqvist, C. & Ezzedine, K. Vitiligo: A review. Dermatology 236, 571–592 (2020).
Alikhan, A., Felsten, L. M., Daly, M. & Petronic-Rosic, V. Vitiligo: a comprehensive overview: Part I. Introduction, epidemiology, quality of life, diagnosis, differential diagnosis, associations, histopathology, etiology, and work-up. J. Am. Acad. Dermatol. 65, 473–491 (2011).
Homan, M. W. L. et al. The burden of vitiligo: Patient characteristics associated with quality of life. J. Am. Acad. Dermatol. 61, 411–420 (2009).
Ongenae, K., Van Geel, N., De Schepper, S. & Naeyaert, J.-M. Effect of vitiligo on self-reported health-related quality of life. Br. J. Dermatol. 152, 1165–1172 (2005).
Parsad, D., Dogra, S. & Kanwar, A. J. Quality of life in patients with vitiligo. Health Qual. Life Outcomes 1, 1–3 (2003).
Ongenae, K., Dierckxsens, L., Brochez, L., van Geel, N. & Naeyaert, J.-M. Quality of life and stigmatization profile in a cohort of vitiligo patients and effect of the use of camouflage. Dermatology 210, 279–285 (2005).
Felsten, L. M., Alikhan, A. & Petronic-Rosic, V. Vitiligo: A comprehensive overview: Part II: Treatment options and approach to treatment. J. Am. Acad. Dermatol. 65, 493–514 (2011).
Taieb, A. et al. Vitiligo European Task Force (VETF); European Academy of Dermatology and Venereology (EADV); Union Européenne des Médecins Spécialistes (UEMS). Guidelines for the management of vitiligo: the European Dermatology Forum consensus. Br. J. Dermatol. 168, 5–19 (2013).
Mulekar, S. & Isedeh, P. Surgical interventions for vitiligo: An evidence-based review. Br. J. Dermatol. 169, 57–66 (2013).
Smith, O. J. et al. The CelluTome epidermal graft-harvesting system: A patient-reported outcome measure and cost evaluation study. Int. Wound J. 14, 555–560 (2017).
Wang, C.-H. et al. Efficacy and safety of automated epidermal micrograft in patients with stable segmental and nonsegmental vitiligo. J. Cosmet. Dermatol. 2, 2 (2021).
Gou, D., Currimbhoy, S. & Pandya, A. G. Suction blister grafting for vitiligo: Efficacy and clinical predictive factors. Dermatol. Surg. 41, 633–639 (2015).
Maleki, M., Banihashemi, M. & Sanjari, V. Efficacy of suction blister epidermal graft without phototherapy for locally stable and resistant vitiligo. Indian J. Dermatol. 57, 282 (2012).
Serena, T., Francius, A., Taylor, C. & MacDonald, J. Use of a novel epidermal harvesting system in resource-poor countries. Adv. Skin Wound Care 28, 107–112 (2015).
Osborne, S. N., Schmidt, M. A. & Harper, J. R. An automated and minimally invasive tool for generating autologous viable epidermal micrografts. Adv. Skin Wound Care 29, 57 (2016).
Bianchi, J. & Gray, D. Adaptic Touch® nonadherent dressing. Wounds UK 7, 120–123 (2011).
Hamzavi, I. et al. Parametric modeling of narrowband UV-B phototherapy for vitiligo using a novel quantitative tool: the Vitiligo Area Scoring Index. Arch. Dermatol. 140, 677–683 (2004).
Finlay, A. Y. & Khan, G. Dermatology Life Quality Index (DLQI)—a simple practical measure for routine clinical use. Clin. Exp. Dermatol. 19, 210–216 (1994).
Ju, H. J. et al. Surgical interventions for patients with vitiligo: A systematic review and meta-analysis. JAMA Dermatol. 2, 2 (2021).
Janowska, A. et al. Epidermal skin grafting in vitiligo: A pilot study. Int. Wound J. 13, 47–51 (2016).
Gupta, S. & Kumar, B. Epidermal grafting in vitiligo: Influence of age, site of lesion, and type of disease on outcome. J. Am. Acad. Dermatol. 49, 99–104 (2003).
Bingel, U. et al. The effect of treatment expectation on drug efficacy: Imaging the analgesic benefit of the opioid remifentanil. Sci. Transl. Med. 3, 7014 (2011).
Kalauokalani, D., Cherkin, D. C., Sherman, K. J., Koepsell, T. D. & Deyo, R. A. Lessons from a trial of acupuncture and massage for low back pain: Patient expectations and treatment effects. Spine 26, 1418–1424 (2001).
Funding
Chang Gung Memorial Hospital is funding this research under the project number CMRPGBJ0022.
Author information
Authors and Affiliations
Contributions
The presented idea was conceived by C.Y.N., P.-R.G., and C.-H.W. as well as developing the theory. The calculations were done by Y.-J.L. Y.-H.H. verified the analytical methods. Y.-C.C. and W.-H.C. supervised the findings of this work. All authors discussed the results and contributed to the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Gao, PR., Wang, CH., Lin, YJ. et al. A comparative study of suction blister epidermal grafting and automated blister epidermal micrograft in stable vitiligo. Sci Rep 12, 393 (2022). https://doi.org/10.1038/s41598-021-04299-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-04299-0
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.