Abstract
To identify and compare keratometric, corneal thickness, and elevation parameters and indices among healthy children, ocular allergy, and keratoconus using the OCULUS Pentacam Scheimpflug topography system. This study included healthy children, children with ocular allergy (OA) without keratoconus, and children with keratoconus (KC). The study design consisted of a prospective evaluation and review of medical records from a Brazilian ophthalmology department. The exclusion criteria were inability to undergo the ocular exam, other ocular diseases, contact lens wear, and topographic corneal ectasia. The effect of each corneal parameter was evaluated using univariate and multivariate logistic regression models adjusted for sex and age, and ROC curves were used to assess the ability each variable to discriminate among groups. A total of 182 subjects were included: healthy children (n = 99), children with OA (n = 32), and children with KC (n = 51). Groups differed in terms of sex, with more males in the OA group (73.2%) and the KC group (67.7%) than in the control group (40.9%). All corneal parameters studied differed significantly between the control and KC groups, and between the OA and KC groups; they also differed significantly between the three groups in terms of astigmatism, q-value, CCT, TP, BAD-D, and ARTmax values. We present the first study to describe and compare corneal tomographic parameters in healthy children, OA, and KC. Keratometry indices, ACD, ARTmax, AETP, and PETP were found to be the most useful for differentiating between healthy and KC children.
IBR registry number: CAAE 54921916.9.0000.5404.
Similar content being viewed by others
Introduction
Keratoconus (KC) is an ectatic corneal disease characterized by the progressive stromal thinning, protrusion of the cornea, irregular astigmatism, and vision impairment. The prevalence of KC in general population is estimated to be around 1 in 20001, but it varies in different population, ethnicity, age, and studies according to different diagnose criteria, variance in genetics, environmental factors, nutrition, and diagnose tools2. Some studies report incidences between 5 and 23 in 10,000, and prevalence 4 and 60 out of 100,0003. According to the Intelligence Research in Sight Registry of American Academy of Ophthalmology, the prevalence of KC in pediatric population is 0.16% in USA4. The prevalence of pediatric KC Saudi Arabia is reported to be as high as 4.79%5.
Advanced KC can be easily diagnosed in a slit-lamp exam and based on anterior curvature measurements6. However, the subtle changes in the anterior corneal curvature that occur prior to the development of visual abnormalities and the typical clinical findings can be observed only using automated corneal topography methods7. Scheimpflug-based cameras, such as the Pentacam (Oculus, Wetzlar, Germany), Galilei (Ziemer, Biel, Switzerland), and Sirius (Costruzione Strumenti Oftalmici, Florence, Italy), are highly effective in the early detection of KC8. Because the Scheimpflug principle works with maximal possible depth of focus and minimal image distortion, it provides valuable information on the anterior segment of the eye9. Further clinical and technological advances have produced a variety of indices that allow physicians to quantify the severity of corneal irregularity10,11. Despite the vast amount of studies evaluating corneal parameters in adults12 and healthy children13, similar data on children with corneal irregularities are still scarce14. The lack of such information may limit the use of the Scheimpflug technology to identify abnormal corneas earlier in the disease’s progression.
A major risk factor for KC is ocular allergy. Ocular allergy is a blanket term to describe different types of allergies, the most commonly diagnosed of which are seasonal and perennial allergic conjunctivitis. Ocular allergy prevalence ranges from 15 to 25% of the population15, and is increasing in the past few decades. In Brazil, a study in 2006 revealed the prevalence of rhinoconjunctivitis at 12%, while a report in 2012 estimated the prevalence of allergic conjunctivitis at 20.7% in preschool children16. A number of inflammatory mediators are expressed in the cornea and ocular surface of patients with ocular allergy , including histamine, protease, tumoral necrosis factor alpha (TNF-α), interleukins (IL), and matrix metalloproteinases (MMP)17, and these mediators may contribute to the development and progression of KC18,19,20,21,22.
KC onset usually occurs during puberty2,23; however, when it develops earlier, it reaches more advanced stages sooner and progresses faster24, leading to greater decreases in quality of life, worsened visual acuity, and negative impacts on social and educational development25. Childhood KC is also associated with an elevated risk of delayed diagnosis, corneal scarring, and penetrating keratoplasty26. In France, a study found KC stage 4 (Amsler Krumeich classification) was diagnose in 27.8% of patients below 15 years old against 7.8% with age more than 27 years at the time of diagnosis with male predominance24. And Chatzis et al. has observed a KC progression in 88% of children by one year of diagnosis mandating an early advocation of corneal crosslinking (CXL) treatment in these pediatric eyes27. Comprehensive corneal evaluations are sensitive to the subtle changes in parameters in children in subclinical stages of KC and with suspicious corneal patterns; these exams may also be used to evaluate progression and establish therapeutic strategies. These factors highlight the importance of early diagnosis in children, particularly in children with ocular allergy and eye-rubbing habits.
Given the importance of keratometric evaluation in pediatric patients in order to diagnose corneal abnormalities earlier and, ideally, to avoid progression to such advanced stages and subsequent losses in quality of life, this study sought to compare corneal parameters and indices among healthy children, those with ocular allergy, and those with KC using the OCULUS Pentacam Scheimpflug topography system to identify thresholds that can be used to clinically diagnose KC.
Methods
This cross-sectional study was performed at the University of Campinas (UNICAMP), in Campinas, São Paulo, Brazil. Written informed consent was obtained from all participants’ parents or legal guardians, and the study was approved by the University of Campinas (UNICAMP) ethics committee. The protocol was in compliance with Good Clinical Practices and the tenets of the Declaration of Helsinki (1996).
Participants
Children with a diagnosis of KC and/or ocular allergy were enrolled during routine visits to the local ophthalmology department. All participants underwent a comprehensive ophthalmological examination, which included a medical history review, best-corrected visual acuity (BCVA), slit-lamp biomicroscopy, autorefraction, and keratometry. KC was diagnosed by experienced cornea specialists based on clinical (including one or more of the following: refractive error, scissoring reflex during retinoscopy, Vogt’s striae, and Fleischer's ring) and topographic criteria (modified Rabinowitz-McDonnell criteria for keratoconus which is based on keratometric readings greater than or equal to 47.2 diopters (D) and an inferior–superior asymmetry (I–S) value greater than or equal to 1.4 D)28, which included early and advanced KC. The mild ocular allergy diagnosis was based on a medical history of allergic conjunctivitis and ocular pruritus; some severe diseases also had other ocular signs of allergy, such as conjunctival papillae and Horner-Trantas limbal lesions. The exclusion criteria included inability to undergo the ocular exam, other ocular diseases (strabismus, corneal scars, amblyopia, cataracts, retinal disorders), trauma, ocular surgery, and contact lens wear.
A cohort of healthy children was enrolled from a public school that was chosen because of its involvement in a hospital partnership program with the government. The exclusion criteria consisted of the inability to undergo the ocular exam, a history of any ocular diseases (including strabismus, corneal scars, amblyopia, cataracts, retinal disorders, ocular allergy), trauma, ocular surgery, contact lens wear, and a topographic diagnosis of corneal ectasia based on the modified Rabinowitz-McDonnell criteria for keratoconus (see above)28. Finally, informed consent was provided by parents or legal guardians.
Examination
The ocular tomographic exam was performed using the OCULUS Pentacam Scheimpflug topography system according to manufacturer’s instructions. The topographic, pachymetric, and elevation parameters of the images captured were used to create maps, graphs, and indices to be evaluated and compared between the groups. Only eyes that had acceptable image quality were included. If both eyes of a given control subject met the eligibility criteria, the right eye was included; when a given KC patient’s image quality was acceptable for both eyes, the eye with the more advanced case of KC was included.
Statistical analysis
For the descriptive analyses, categorical variables were presented as absolute and relative frequencies, while continuous variables were summarized using means and standard deviation (SD). The effect of potential risk factors was evaluated via univariate logistic regression analysis. The models compared the effect of each variable in paired comparisons of the model groups: healthy controls versus KC patients, healthy controls versus ocular allergy patients, and KC patients versus ocular allergy patients. Since the diagnosis groups differed in terms of sex and age, the multivariate logistic models used were adjusted for the potential confounding factors of those two variables. Finally, the area under the receiver operating characteristic (ROC) curves (AUCs) was used to assess and compare the ability of each variable to discriminate between the eyes in each group, and the optimal diagnostic cutoff was estimated using the method provided by Liu29.
All statistical analyses were performed using the commercially available software Stata, version 16 (StataCorp LP, College Station, TX). The alpha level (type I error) was set at 0.05.
Results
One hundred and eighty-two eyes of 182 children were included in this study. Out of these, 99 (54%) were classified as healthy or normal, 32 (18%) were classified as having as ocular allergy, and 51 (28%) were determined to have KC. Most subjects (69%) were male. Mean subject age was 9.4 ± 1.3 years old.
We found statistically significant differences among all groups in all of the topometric, pachymetric, and relational thickness indices studied. Table 1 summarizes the demographic and clinical characteristics of the eyes included in the study according to their diagnostic group.
As detailed in Table 2 the distribution of the clinical parameters of the ocular allergy group was compared to those of the KC group. There were statistically significant differences in the index of vertical asymmetry (IVA), keratoconus index (KI), central keratoconus index (CKI), index of height asymmetry (IHA), and index of height decentration (IHD) values (p < 0.001), as well as in pupil diameter (p = 0.014).
Healthy children differed significantly from KC children in all parameters. The subjects with ocular allergy differed significantly from KC children in terms of all parameters except for anterior chamber depth (ACD). When children with ocular allergy were compared to the controls, the children with ocular allergy had higher astigmatism values and Belin/Ambrosio enhanced ectasia display (BAD-D) readings than the controls, as well as lower pachymetric readings, q-values, and Ambrosio’s relational thickness maximum (ARTmax) values.
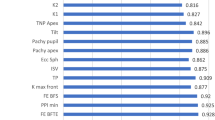
The calculation of the odds ratio (OR) revealed certain parameters that could easily be used to differentiate between the groups. Results of multivariate analysis that were adjusted for potentially confounding variables (i.e., sex and age) are described in Table 3. Figure 1 shows forest plots that illustrate the estimated increase in the OR of each diagnosis group per unit increase or decrease in the value of each topographical parameter of interest. Maximum keratometry (Kmax) differentiates between groups perfectly because it served as an exclusion criterion for both the control group and ocular allergy group and was therefore not considered in this analysis. The keratometry readings, thinnest pachymetry (TP) values, ACD, q-values, ARTmax, average pachymetric progression index (PPIave), and BAD-D values (BAD-D > 2.42 SD was found to predict the diagnosis group perfectly) were the most reliable parameters for differentiating between normal and KC children. ACD and q-value were found to be the most reliable parameters for differentiating between healthy children and children with ocular allergy. Finally, keratometry readings, BAD-D, q-values, TP, ARTmax, and PPIave were determined to be the most reliable parameters for differentiating between children with ocular allergy and those with KC.
Forest plots for the odds ratio (OR) values and 95% confidence intervals from univariate models comparing (A) healthy controls to keratoconus patients, (B) healthy controls to ocular allergy patients, and (C) ocular allergy patients to keratoconus patients. Dashed vertical line represents an OR of 1. K1 flat keratometry, K2 steep keratometry, Kmax maximum keratometry, Astig astigmatism in Sim K, TP thinnest pachymetry, ACD anterior chamber depth, BAD-D Belin/Ambrosio’s Enhanced Ectasia Display, ARTmax Ambrosio’s relational thickness maximum, PPIave average pachymetric progression index, AETP anterior elevation at the thinnest point, PETP posterior elevation at the thinnest point, PE maximum posterior elevation.
The AUC was found to be above 0.975 for certain parameters. In these cases, the result implies high sensitivity and specificity when differentiating between healthy children and KC patients, as well as between ocular allergy patients and KC patients.
Figure 2 displays the ROC curve for these parameters. Kmean, Kmax, BAD-D, q-value, ACD, ARTmax, anterior elevation at the thinnest point (AETP), and posterior elevation at the thinnest point (PETP) were found to have an AUC greater than 0.975 in the comparison between healthy controls and KC patients. In the comparison between ocular allergy and KC patients, Kmax, BAD-D, TP, ARTmax, PPIave, and PETP were found to have high AUCs (> 0.975). The BAD-D value was found to be most reliable parameter to differentiate between healthy controls and KC patients and between ocular allergy and KC, with AUC of 1.000 and 0.998, respectively. In the comparison between the control group and the ocular allergy group, the parameter with the highest AUC was found to be ACD (0.913). The AUCs were used to determine cut-off values with the highest sensitivity and specificity for differentiating between the groups. These results are summarized in Tables 4, 5, and 6.
Discussion
In this study, we calculated the diagnostic ability of different corneal parameters using the OCULUS Pentacam Scheimpflug topography system and estimated cutoffs with high sensitivity and specificity for differentiating children with ocular allergy and children with KC from healthy children. To the best of our knowledge, this is the first study to provide normative values for corneal parameters using an age-matched cohort of healthy children. This information may guide better clinical decisions than the cutoffs currently used, which are based on adult populations, and may thus allow for an earlier diagnosis of corneal ectasia.
All parameters studied differed significantly between healthy controls and KC patients. Kmean (45.0 D), BAD-D (2.42), ACD (3.5 mm), ARTmax (334), AETP (6 µm), and PETP (11 µm) were found to be the most reliable parameters in that they offered well-defined cutoffs for differentiating between healthy controls and cases of KC; these parameters also yielded high sensitivity and specificity (all were found to have AUCs above 0.975). This information shows that the Pentacam can easily identify KC in children (similar to its use on adult populations), and that these parameters are the best tools for use in clinical practice.
When ocular allergy parameters were compared to KC parameters, the results also differed significantly. The best parameters (and their cutoffs) were found to be ARTmax (302), AETP (7 µm), and PETP (12 µm), all of which exhibited AUCs above 0.975. These findings support the use of the Pentacam to identify KC in children with ocular allergy. This type of diagnosis and differentiation is important, since children with ocular allergy face a substantial risk of developing KC. These findings also imply that children with ocular allergy should receive an Scheimpflug topography exam using these cutoffs.
In attempts to distinguish between healthy eyes and eyes with ocular allergy, all of the parameters exhibited suboptimal performance (AUC below 0.975). The most reliable parameter was ACD, with an AUC of 0.913, sensitivity of 84%, and specificity of 88% at 3.34 mm of depth. These numbers imply that the parameter is useful, but ACD alone cannot be used to diagnose ocular allergy children. This finding suggests that healthy eyes are similar to eyes with ocular allergy (since only ACD and q-values differed at a p < 0.001), and that the Pentacam is not a good tool for identifying this condition in children. This could be explained by the fact that children with ocular allergy without opacities do not have structural damage to the cornea.
Our findings showed that BAD-D was the best tool in the diagnosis of keratoconus (comparing with healthy controls), which is congruent with other studies in adults30,31,32. This parameter is calculated based on a linear regression analysis and derives from different indices considering anterior and posterior elevation and the distribution of corneal thickness: Df (deviation of the normality of the front elevation), Db (deviation of normality of the back elevation), Dt (deviation of normality of corneal thinnest point), Da (deviation of normality of Ambrósio relational thickness), Dp (deviation of normality in average pachymetric progression), Dy (displacement of thinnest point along the vertical meridian), anterior elevation at the thinnest point, posterior elevation at the thinnest point, and Kmax12. In the Pentacam display system, each parameter is indicated in yellow (suspicious) if it is ≥ 1.6 SD from the mean or in red (abnormal) if it is ≥ 2.6 SD from the mean12, which is very similar to our findings that showed a BAD-D > 2.42 with AUC 1.000 to distinguish healthy children from KC and a BAD-D > 2.25 with AUC 0.998 to distinguish OA children from KC. Different studies in adults showed similar values between healthy controls and clinical keratoconus, ranging from 1.83 to 2.615 (most of all > 2.00 SD)32,33,34,35,36,37,38. Lower values were found in studies using healthy controls and subclinical keratoconus, ranging from 1.22 to 1.61 SD32,33,36,37,39,40, which is different from our study since we included patients with frank KC. Subclinical keratoconus is widely defined as a topographically normal eye that has frank KC in the fellow eye, or subtle topographic changes without clinical signs of KC or a change in visual acuity41,42,43. This information suggests that lower values used for adults could aid in screening for subclinical KC in children, but more studies are needed to confirm this hypothesis.
This information should help clinically to use Pentacam to diagnose KC in children with important risk factor for development of the disease, that is ocular pruritus. It can identify a normal cornea (that is similar to the cornea of OA cornea) in children and distinguish from KC children (in early and advanced cases). This should help to quickly diagnose KC in all children (normal and with OA) and to find early stages of the disease, preventing loss of quality of life and evolution to more advanced cases, since we can treat much earlier. For this essential task, BAD-D can play an important role, since it could easily distinguish between healthy and KC children, and between OA and KC children.
Previous studies have provided substantial information and many normative values for corneal power, astigmatism, corneal thickness, and pachymetric progression indices in adults and healthy children13. However, such parameters have not been studied in children with keratoconus or ocular allergy using current tomographers, such as the OCULUS Pentacam Scheimpflug topography system. This is the first study to describe corneal parameters in children with ocular allergy and keratoconus using the Pentacam, as well as the first to compare healthy children, children with ocular allergy, and children with keratoconus, providing us the information we needed for the diagnose of KC in children in early and advanced cases.
The parameters found in normal children were very similar to what was found for adults in literature44, which suggests that their corneas are similar too and that the parameters that we use clinically for adults should be very similar for the children, but other studies are needed to confirm this.
This study has certain limitations. Subject age ranged from 7 to 11 years, and it is not known how the corneas of children outside of this age bracket behave or whether these same parameters can be applied to other pediatric age groups. Though the occurrence of KC is more common in adolescents, it is also important to note that, while the tomographic exam takes only two seconds to capture all of the images, the patient must remain immobile with eyes fixated on the target, conditions which could be difficult for younger patients to comply with. Children with ocular allergy can be even more challenging to image because of the inflammation and photosensitivity found in some patients with symptomatic disease; furthermore, severe disease causes corneal opacities, and images therefore cannot be captured with high quality of images using a Scheimpflug topography system.
Conclusion
This is the first study to identify tomographic parameters of the cornea that can be used to distinguish between healthy children, children with ocular allergy, and children with keratoconus. Keratometry indices, q-value, ACD, ARTmax, BAD-D, AETP, and PETP were found to be the most reliable parameters for differentiating between healthy eyes and cases of keratoconus. TP, ARTmax, and PPIave were found to be the most reliable parameters for differentiating between ocular allergy cases and cases of keratoconus. Finally, none of the parameters alone were found to be reliable for distinguishing between healthy eyes and cases of ocular allergy in children. This should help to identify early diseases in children and in children with risk factor for keratoconus.
References
Kennedy, R. H., Bourne, W. M. & Dyer, J. A. A 48-year clinical and epidemiologic study of keratoconus. Am. J. Ophthalmol. 101(3), 267–273 (1986).
Anitha, V. et al. Pediatric keratoconus—Current perspectives and clinical challenges. Indian J. Ophthalmol. 69(2), 214–225 (2021).
Romero-Jiménez, M., Santodomingo-Rubido, J. & Wolffsohn, J. S. Keratoconus: A review. Contact Lens Anterior Eye 33(4), 157–166 (2010) (quiz 205).
Moshirfar, M., Heiland, M. B., Rosen, D. B., Ronquillo, Y. C. & Hoopes, P. C. Keratoconus screening in elementary school children. Ophthalmol. Ther. 8(3), 367–371 (2019).
Torres Netto, E. A. et al. Prevalence of keratoconus in paediatric patients in Riyadh, Saudi Arabia. Br. J. Ophthalmol. 102, 1436–1441 (2018).
de Sanctis, U. et al. Sensitivity and specificity of posterior corneal elevation measured by Pentacam in discriminating keratoconus/subclinical keratoconus. Ophthalmology 115(9), 1534–1539 (2008).
Feizi, S., Yaseri, M. & Kheiri, B. Predictive ability of Galilei to distinguish subclinical keratoconus and keratoconus from normal corneas. J. Ophthalmic Vis. Res. 11(1), 8–16 (2016).
Oliveira, C. M., Ribeiro, C. & Franco, S. Corneal imaging with slit-scanning and Scheimpflug imaging techniques. Clin. Exp. Optom. 94(1), 33–42 (2011).
Shetty, R. et al. Repeatability and agreement of three Scheimpflug-based imaging systems for measuring anterior segment parameters in keratoconus. Investig. Ophthalmol. Vis. Sci. 55(8), 5263–5268 (2014).
Maeda, N., Klyce, S. D., Smolek, M. K. & Thompson, H. W. Automated keratoconus screening with corneal topography analysis. Investig. Ophthalmol. Vis. Sci. 35(6), 2749–2757 (1994).
Rabinowitz, Y. S. & Rasheed, K. KISA% index: A quantitative videokeratography algorithm embodying minimal topographic criteria for diagnosing keratoconus. J. Cataract Refract. Surg. 25(10), 1327–1335 (1999).
Motlagh, M. N. et al. Pentacam® corneal tomography for screening of refractive surgery candidates: A review of the literature, part I. Med hypothesis. Discov. Innov. Ophthalmol. J. 8(3), 177–203 (2019).
Matheus, I. S. V. et al. Corneal evaluation in healthy Brazilian children using a Scheimpflug topography system. J. Clin. Exp. Ophthalmol. 08, 02 (2017).
Zheng, Y., Huang, G., Huang, W. & He, M. Distribution of central and peripheral corneal thickness in Chinese children and adults: The Guangzhou twin eye study. Cornea 27(7), 776–781 (2008).
Gomes, P. J. Trends in prevalence and treatment of ocular allergy. Curr. Opin. Allergy Clin. Immunol. 14(5), 451–456 (2014).
Chong Neto, H. J. et al. Allergic rhinitis in preschool children from Southern Brazil. Allergy 69(4), 545–547 (2014).
Balasubramanian, S. A., Pye, D. C. & Willcox, M. D. P. Effects of eye rubbing on the levels of protease, protease activity and cytokines in tears: Relevance in keratoconus. Clin. Exp. Optom. 96(2), 214–218 (2013).
Sharma, N., Rao, K., Maharana, P. K. & Vajpayee, R. B. Ocular allergy and keratoconus. Indian J. Ophthalmol. 61(8), 407–409 (2013).
Krachmer, J. H. Eye Rubbing Can Cause Keratoconus Vol. 23, 539–540 (Cornea, 2004).
Coyle, J. T. Keratoconus and Eye Rubbing Vol. 97, 527–528 (American Journal of Ophthalmology, 1984).
McMonnies, C. W. Abnormal rubbing and keratectasia. Eye Contact Lens 33(6 Pt 1), 265–271 (2007).
McMonnies, C. W. Mechanisms of rubbing-related corneal trauma in keratoconus. Cornea 28(6), 607–615 (2009).
Mukhtar, S. & Ambati, B. K. Pediatric keratoconus: A review of the literature. Int. Ophthalmol. 38(5), 2257–2266 (2018).
Leoni-Mesplie, S. et al. Scalability and severity of keratoconus in children. Am. J. Ophthalmol. 154(1), 56.e1-62.e1 (2012).
Aydin Kurna, S., Altun, A., Gencaga, T., Akkaya, S. & Sengor, T. Vision related quality of life in patients with keratoconus. J. Ophthalmol. 2014, 694542 (2014).
El-Khoury, S. et al. Pediatric keratoconus in a tertiary referral center: Incidence, presentation, risk factors, and treatment. J. Refract. Surg. 32(8), 534–541 (2016).
Chatzis, N. & Hafezi, F. Progression of keratoconus and efficacy of pediatric [corrected] corneal collagen cross-linking in children and adolescents. J. Refract. Surg. 28(11), 753–758 (2012).
Maeda, N., Klyce, S. D. & Smolek, M. K. Comparison of methods for detecting keratoconus using videokeratography. Arch. Ophthalmol. (Chicago Ill. 1960) 113(7), 870–874 (1995).
Liu, X. Classification accuracy and cut point selection. Stat. Med. 31(23), 2676–2686 (2012).
Ramos, I., Correia, F. F., Lopes, B., Salomão, M. Q. & Correa, R. O. Topometric and tomographic indices for the diagnosis of keratoconus. Int. J. Keratoconus Ectatic Corneal Dis. 1(2), 92–99 (2012).
Ambrósio, R. et al. Enhanced screening for ectasia susceptibility among refractive candidates: The role of corneal tomography and biomechanics. Curr. Ophthalmol. Rep. 1(1), 28–38 (2013).
Hashemi, H. et al. Pentacam top indices for diagnosing subclinical and definite keratoconus. J. Curr. Ophthalmol. 28(1), 21–26 (2016).
Muftuoglu, O., Ayar, O., Hurmeric, V., Orucoglu, F. & Kilic, I. Comparison of multimetric D index with keratometric, pachymetric, and posterior elevation parameters in diagnosing subclinical keratoconus in fellow eyes of asymmetric keratoconus patients. J. Cataract Refract. Surg. 41(3), 557–565 (2015).
Chan, T. C., Wang, Y. M., Yu, M. & Jhanji, V. Comparison of corneal dynamic parameters and tomographic measurements using Scheimpflug imaging in keratoconus. Br. J. Ophthalmol. 102, 1–42 (2017).
Lopes, B. T. et al. Enhanced tomographic assessment to detect corneal ectasia based on artificial intelligence. Am. J. Ophthalmol. 195, 223–232 (2018).
Huseynli, S. & Abdulaliyeva, F. Evaluation of Scheimpflug tomography parameters in subclinical keratoconus, clinical keratoconus and normal Caucasian eyes. Turk. J. Ophthalmol. 48(3), 99–108 (2018).
Shetty, R. et al. Keratoconus screening indices and their diagnostic ability to distinguish normal from ectatic corneas. Am. J. Ophthalmol. 181, 140–148 (2017).
Ambrosio, R. J. et al. Novel pachymetric parameters based on corneal tomography for diagnosing keratoconus. J. Refract. Surg. 27(10), 753–758 (2011).
Ruisenor Vazquez, P. R. et al. Pentacam Scheimpflug tomography findings in topographically normal patients and subclinical keratoconus cases. Am. J. Ophthalmol. 158(1), 32-40.e2 (2014).
Ambrosio, R. J., Valbon, B. F., Faria-Correia, F., Ramos, I. & Luz, A. Scheimpflug imaging for laser refractive surgery. Curr. Opin. Ophthalmol. 24(4), 310–320 (2013).
Ambrosio, R. J. & Belin, M. W. Imaging of the cornea: Topography vs tomography. J. Refract. Surg. (Thorofare N. J. 1995) 26, 847–849 (2010).
Gomes, J. A. P. et al. Global consensus on keratoconus and ectatic diseases. Cornea 34(4), 359–369 (2015).
Kim, J. T. & Zloty, P. Simplified nomenclature for describing keratoconus. Int. J. Keratoconus Ectatic Corneal Dis. 1(1), 31–35 (2012).
Feng, M. T. et al. International values of corneal elevation in normal subjects by rotating Scheimpflug camera. J. Cataract Refract. Surg. 37(10), 1817–1821 (2011).
Author information
Authors and Affiliations
Contributions
M.I.S.V.—conducted the research, compiled the data, and wrote the main manuscript test. A.A.J.—statistical analysis, wrote the manuscript, and prepared the figures. C.E.L.A.—supervised the research, and wrote the main manuscript text. M.A.—supervised the research, and wrote the main manuscript text. J.P.C.d.V.—supervised the research, and wrote the main manuscript text. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Vieira, M.I.S., Jammal, A.A., Arieta, C.E.L. et al. Corneal Scheimpflug topography values to distinguish between normal eyes, ocular allergy, and keratoconus in children. Sci Rep 11, 24275 (2021). https://doi.org/10.1038/s41598-021-03818-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-03818-3
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.