Abstract
Nasal continuous positive airway pressure (nCPAP) is the standard non-invasive respiratory support for newborns with respiratory distress. Nasal injury is a common problem with the interfaces used. To compare the incidence and severity of nasal injury in neonates with respiratory distress and supported on nCPAP with Hudson prong or RAM cannula with Cannulaide, a semipermeable membrane. This is an open-label, parallel-arm, gestational age-stratified, bi-centric, randomized control trial including neonates between 28 and 34 weeks gestational age and birth weight > 1000 g needing nCPAP. The size of the interface was chosen as per the manufacturer’s recommendation. Of the 229 neonates enrolled, 112 were randomized to RAM cannula with Cannulaide and 117 to Hudson prong. The baseline characteristics were similar. Any nasal injury at CPAP removal was significantly lower in the RAM cannula with Cannulaide group [6 (5.4%) vs. 31 (26.4%); risk ratio—0.77 (95% CI 0.69–0.87); p = 0.0001]. The incidence of moderate to severe nasal injury, need for mechanical ventilation within 72 h of age, duration of oxygen, and requirement of nCPAP for > 3 days were similar. For preterm infants on nCPAP, RAM cannula with Cannulaide, compared to Hudson prongs, decreases nasal injury without increasing the need for mechanical ventilation.
Trail registration: CTRI/2019/03/018333, http://www.ctri.nic.in.
Similar content being viewed by others
Introduction
Respiratory distress among premature neonates is one of the commonest indications requiring NICU admission. Nasal continuous positive airway pressure (nCPAP), which maintains the functional residual volume of the lung, is used widely to provide respiratory support for neonates. nCPAP use is shown to reduce mortality, need for mechanical ventilation, and respiratory failure1.
The nasal interface forms a critical element in nCPAP delivery. Various interfaces used include nasopharyngeal tubes, binasal prongs, and nasal masks. For effective delivery of nCPAP, the interfaces are required to maintain a constant and stable airway pressure. However, the force applied on the delicate tissues of the nares and nasal septum by the interfaces compromises the skin integrity and may result in nasal injury. The reported incidence of nasal injuries with the use of nCPAP ranges from 20 to 100%2,3,4,5. The spectrum of nasal injuries ranges from blanchable erythema, non-blanching hyperemia, and skin erosion to excoriation, columellar necrosis, and full-thickness skin loss6. Lower gestational age (< 30 weeks), lower birth weight (< 1500 g), longer duration of nCPAP, incorrect size, and/or fixation of the interface are the reported risk factors for nasal injury6.
Hudson prongs (Hudson-RCI, Temecula, CA) were designed to reduce the nasal trauma associated with the delivery of infant nCPAP. They are soft, anatomically curved prongs available in 6 sizes, allowing greater choices for appropriate sizing. Although they are effective and safe, there is a potential to cause nasal septal pressure injury. The RAM cannula (Neotech, Valencia, CA) was approved by the Food and Drug Administration as a Class I medical device for providing supplemental oxygen with 60–80% nasal occlusion7. It was being used off-label to provide nCPAP because of its ease of use and perception of decreased nasal injury8,9,10,11. The device looks similar to a traditional nasal cannula used to deliver oxygen, but its stiffer design allows a higher flow rate and pressure delivery. As it is made of a soft material, there is lower airflow resistance and a tendency for reduced nasal trauma.
While Hochwald et al. made a similar comparison for preterm neonates receiving NIPPV12, there are no adequately powered studies that compared these two interfaces in reducing nasal injuries. As previous physiological and in vivo studies13,14,15,16,17 demonstrated concerns on the efficacy of RAM cannula to deliver the set pressures, we used Cannulaide, a hydrocolloid protective barrier which secures cannula in place and provides a seal, in RAM cannula group for snugly fitting the nasal cannula, preventing leak and allowing better delivery of CPAP pressures. We aimed to compare RAM cannula with Cannulaide versus Hudson prong for delivery of nCPAP in preterm neonates born between 28 and 34 weeks gestational age and weighing ≥ 1000 g, in reducing nasal injuries. Extremely low birth weight neonates were not included for concerns of increased failure rates.
Methods
This randomized controlled trial was conducted from April 2019 to May 2020at two level-3 neonatal intensive care units (NICU) of tertiary care hospitals in India. The study protocol was prospectively registered in the clinical trial registry of India on 29/03/2019 with a registration number of CTRI/2019/03/018333 (available at http://www.ctri.nic.in). The study was approved by ethics committees of Fernandez hospitals, Hyderabad, India and King Edward Memorial Hospitals, Pune, India. The study was not funded by any source. No changes were made to the study protocol or outcomes after registration. Informed consent was obtained from the guardians of all the participants. The study was performed following the declaration of Helsinki on research on human subjects. Neonates with major congenital malformations such as congenital diaphragmatic hernia, tracheo-oesophageal fistula, Pierre-Robin sequence, and choanal atresia were excluded. We also excluded neonates requiring mechanical ventilation at admission to NICU, those with poor respiratory efforts or apnea, worsening shock, suspected or proven persistent pulmonary hypertension of newborn, severe metabolic acidosis (pH < 7.20 and base deficit > 10), severe respiratory acidosis (pH < 7.20 and PaCO2 > 60 mm Hg) and massive pulmonary haemorrhage.
Neonates were randomly allocated to nCPAP with either Hudson prongs or RAM cannula with Cannulaide by the primary investigator, using random numbers contained in serially numbered opaque envelopes, after taking informed consent from parent/guardian. Individual randomization was done for each infant in multifetal gestation. Block randomization was done using computer-generated numbers, by a person not involved in the study. Stratified randomization technique was used based on gestational age (28–30 weeks and 31–34 weeks). Recording of basic clinical data of neonates was done before opening the coded envelopes to optimize allocation concealment. During the study period, both the neonatal units used double-lumen bubble CPAP (B-CPAP) for delivering nCPAP to preterm neonates. nCPAP initiation, titration, and weaning were as per the standard protocol of the participating centres.
The primary outcomes of interest were the incidence and severity of nasal injury at the removal of nCPAP. The secondary outcomes included nasal injury score at discharge, need for mechanical ventilation, duration of nCPAP, need for a change of interface, mortality, and other neonatal morbidities.
In the Hudson prong group, the neonates were given nCPAP support by using appropriately sized Hudson prongs (as per the manufacturers’ recommendations) till nCPAP was weaned off. The prongs were connected to the nCPAP circuit directly using pins and rubber bands over appropriate-sized bonnets and secured in place with a strip of Velcro tape placed across the infant’s upper lip (Fig. 1). In the RAM cannula group, an appropriately sized RAM cannula as per the manufacturer’s instructions was used for providing nCPAP. A semipermeable membrane (Cannulaide) was used to fix the RAM cannula and to minimize leaks around the nostrils. Cannulaide was prepared by NICU staff using Duoderm (extra thin CGF/Convatec) with two small holes to insert the nasal prongs. As there is no separate expiratory limb to vent out inhaled gases, the infant’s mouth was not actively closed as an important safety measure (Fig. 1).
Routine monitoring of neonate on nCPAP included flow rate, the fraction of inhaled oxygen (FiO2), CPAP pressure, bubbling, humidifier temperature, water level, interface size, fixation, the distance between interface and infant nostrils. All enrolled infants were monitored 8th hourly and assessed for nasal injury by the bedside nurse under the supervision of a neonatal fellow who has observed at least 10 nasal injuries correctly. A standard nasal injury score chart18,19 was used (Table 1). At the removal of nCPAP, in addition, digital photographs were taken and were later reviewed by a senior neonatologist who was blinded to the study group allocation. Informed consent was taken from parents to publish the clinical photographs.
Weaning from nCPAP was attempted if the infant had good respiratory efforts, minimal or no recessions, no tachypnoea, no apnea/bradycardia, and was on stable or decreasing oxygen requirement for 4 to 6 h. nCPAP was tapered to high flow nasal cannula (HFNC) at nCPAP pressure of 4 cm of H2O, FiO2 of < 30%, and the neonate was hemodynamically stable, with good respiratory efforts and no apnea/bradycardia. If the infant remained stable on HFNC for at least 6 h, the infant was considered to have completed the study. If the infant did not tolerate HFNC within the 6-h trial period, the infant was restarted on nCPAP using the same nasal interface as before.
Need for mechanical ventilation or non-invasive positive pressure ventilation (NIPPV) (nCPAP failure) was considered if an infant receiving CPAP pressure > 7 cm water had FiO2 requirement > 0.6, severe respiratory acidosis, severe metabolic acidosis, increasing work of breathing (Silverman Anderson score/SAS increased by > 2 from baseline) or recurrent/severe apneas (> 4 episodes per hour or need for bag and mask ventilation for any apnea). Change of nasal interface was considered if the infant had a nasal injury score ≥ 4. The nCPAP interfaces were changed in a crossover pattern and then analyzed as per intention to treat analysis.
A previous study noted the incidence of moderate to severe nasal injury of 33% among the Hudson prong group18. Assuming the reduction of nasal injury by 50% (an absolute reduction of 16.5%) with RAM cannula with Cannulaide, taking 80% power, 5% alpha error, and 95% confidence interval, we calculated a sample size of 109 neonates in each group in a superiority design (margin of 0.05) to prove our hypothesis.
Descriptive statistics were used to describe baseline variables. Categorical outcome variables were expressed as proportion and analyzed by Chi-square test with continuity correction or Fisher’s exact test, wherever one or more expected cell sizes is less than 5. Estimates of the strength of association were deduced by calculating relative risks with their respective 95% confidence intervals. Continuous variables were expressed as mean (standard deviation) or median (interquartile range) based on their distribution. These variables were first tested for normality utilizing the Kolmogorov–Smirnov test for normality, and analyzed by student ‘t’ test or Wilcoxon rank sign test. All analyses were done using IBM-SPSS v.20 and Microsoft Excel. A p value of < 0.05 was considered significant. Binominal regression analysis was performed to identify the predictors of nasal injury.
Ethical review board
Institutional Ethics Committee, Fernandez Hospital Foundation (Reg. no. ECR/933/Inst/TG/2017); Reference number: 19_2018.
Informed consent
An informed consent was taken from the infant parents or legal guardian before the enrolment into the study.
Results
During the study period, 264 preterm infants were assessed for eligibility and 229 infants were enrolled (205 infants from Fernandez Hospital, and 24 infants from King Edward Memorial Hospital). The participant flow is shown in Fig. 2. The baseline characteristics of neonates including gestational age, birth weight, gender, the incidence of intrauterine growth retardation, distribution of infants in the gestational age strata, Apgar scores, and SNAPPE II (Score for Neonatal Acute Physiology-Perinatal Extension, version 2) scores at admission were similar between the two groups. The maternal characteristics of antenatal steroid coverage, mode of delivery, and multifetal pregnancies were also similar. The characteristics of respiratory illness including the severity of respiratory distress (measured by SAS), number of infants with respiratory distress syndrome, surfactant requirement, age at enrolment, FiO2 at enrolment, CPAP at enrolment, maximum FiO2 required, maximum CPAP required, and age at receiving surfactant were similar between Hudson prong and RAM cannula with Cannulaide groups (Table 2).
Thirty one infants (26.4%) in Hudson prong group and 6 infants (5.35%) in RAM cannula with Cannulaide group had nasal injury (RR—0.77, 95% CI 0.69–0.87, p = 0.0001; Absolute risk reduction—0.21, 95% CI 0.12–0.3; Number need to prevent one injury—4.7, 95% CI 3.32–8.26). In the Hudson Prongs group, 29 infants had a mild nasal injury (score 1–4) while 2 had a moderate nasal injury (score 5–6). All 6 infants in RAM cannula with Cannulaide group had a mild nasal injury. None of the infants suffered from severe nasal injury. Four infants (3.4%) in the Hudson prong group and none of the infants in the RAM cannula group with Cannulaide group had persistence of nasal injury at discharge (RR—0.966; 95% CI 0.93–0.99, p = 0.048). Among the 37 infants with nasal injury, 12 (32%), 6 (16%), 9 (24%) and 8 (22%) infants had maximum nasal injury scores of 1, 2, 3, and 4 at the removal of nCPAP, respectively. One infant each had a maximum nasal injury score of 5 and 6. On subjective evaluation, none had skin excoriation, 32 (87%) infants had erythema, 21 (57%) infants had dilation of nostrils and 4 (11%) infants had indentation. All 4 infants with the persistence of nasal injury at the time of discharge had discolouration over the upper lip.
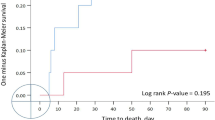
In the Hudson prong group, significantly more neonates required a change of interface as compared to RAM cannula with the Cannulaide group. The duration of nCPAP was significantly longer in RAM cannula with the Cannulaide group. The need for mechanical ventilation within 72 h of age, duration of oxygen therapy, nCPAP requirement for more than 3 days, air leaks, and need for supplemental oxygen at 28 days of life were not different between the two groups (Table 3). The interface was changed for one neonate in the RAM cannula with Cannulaide group because of worsening respiratory distress and for 8 infants in the Hudson prong group for nasal injury (n = 5) or worsening respiratory distress (n = 3).
The neonatal morbidities (culture-positive sepsis, necrotizing enterocolitis, grade 3 or 4 intraventricular hemorrhage, cystic periventricular leukomalacia, retinopathy of prematurity requiring laser, and mortality) except patent ductus arteriosus were not different between the two groups. The mean length of hospital stay and anthropometry at discharge were comparable between RAM cannula and Hudson prong group (Table 3). Five infants (2.2%) died during the hospital stay and 10 infants (4.3%) got transferred to other hospitals for continuing care. Of these, 4 infants were still on nCPAP at the time of transfer. Two hundred and fourteen infants (93.4%) got discharged from the hospital.
The potential predictors included were gestation at birth, birth weight, antenatal steroid coverage, SNAPPE II score, SA score, duration of nCPAP, nCPAP interface, FiO2 at enrolment, and maximum FiO2 required during the study. Nasal CPAP interface and duration of nCPAP were significantly associated with nasal injury (Table 4).
Discussion
In this RCT, we compared the use of RAM cannula with Cannulaide versus Hudson prongs for delivery of nCPAP in preterm infants with birth weight ≥ 1000 g and gestation 280/7–346/7 weeks. Cannulaide was used in fixing RAM cannula for decreasing leaks around the nostrils and delivery of better CPAP pressures. The incidence of nasal injury was significantly lower with the use of RAM cannula with Cannulaide when compared to Hudson’s bi-nasal prongs. Previous studies also reported less nasal injury with RAM cannula. Drescher et al. compared 36 infants on RAM cannula with 36 infants on the nasal mask or bi-nasal prongs in preterm infants born before 29 weeks’ gestation with birth weight < 1500 g8. Nasal injury, described as skin and/or mucosal breakdown, was significantly lower in the RAM cannula group (3 vs. 19; p < 0.001). They used Duoderm dressing for protecting the skin at pressure points. However, this study was done in a before-and-after study design, with small sample size. In an RCT, Gokce et al. compared RAM cannula (n = 64) with Hudson prongs (n = 62) in preterm neonates (26–34 weeks’ gestation) for non-invasive respiratory support11. Incidence of nasal injury (defined as stage I—hyperemia and hemorrhage, stage II—disruption of skin integrity and superficial ulceration, stage III—nasal deformity) was similar between the two groups (8 vs. 7; p = 0.83). Contrary to our study methods, Cannulaide was used for short bi-nasal prongs. This study had a small sample size, the nasal injury was the secondary outcome, and the nasal injury assessment concentrated mainly on the septal injury.
In the present study, we included a more robust assessment of the nasal injury. It could be the reason for identifying many mild nasal injuries in our study, especially in the Hudson prong group. The use of Cannulaide, softness of prongs, ease of fixation, and stability may be the reasons for less nasal injury in the RAM cannula group. However, even in the Hudson prong group, very few had moderate/severe nasal injuries. Use of barrier dressing (Duoderm) over the upper lip, training of nurses in the care of infants on nCPAP, nasal injury monitoring, and using objective scoring were the additional methods that would have reduced nasal injury. These findings also emphasize that, under controlled conditions, reduction of moderate to severe nasal injury is possible with any nasal interface.
The other important concern with RAM cannula is the delivery of pressures and nCPAP failures. In the study by Drescher et al., although the neonates on RAM cannula needed higher settings, and had a shorter time to reintubation, there was no significant difference in non-invasive respiratory support failure rates8. A significant reduction in the duration of respiratory support and a trend towards reduction of bronchopulmonary dysplasia was noted. In the RCT by Gokce et al., more neonates with RAM cannula needed invasive ventilation in the first 72 h, surfactant administration and also, repeated doses of surfactant11. However, there was no increase in the duration of respiratory support and bronchopulmonary dysplasia. Enrolment of smaller infants, a higher threshold for surfactant administration (FiO2 > 0.4), use of Cannulaide in the short binasal prong group but not in the RAM cannula group, and the use of lower CPAP pressures (5–6 cm of H2O) may be the reasons for higher failure rate in RAM cannula group in that study.
In our study, the lesser need for invasive ventilation/NIPPV in both the groups could be due to early and liberal use of surfactant (FiO2 ≥ 30%), use of Cannulaide in RAM cannula group which achieved near 100% nasal seal, enrolment of bigger infants with weight ≥ 1000 g and gestation ≥ 28 weeks and possible use of higher pressures in the RAM cannula group.
Physiological studies showed that RAM cannula had high resistance15, pressure delivered was acceptable with leaks < 30%16, and it could not deliver set CPAP levels when applied using the manufacturer’s recommended 60–80% nares occlusion, even with closed mouth and full nasal prong insertion14. Matlock et al. noted that NIPPV with RAM cannula produced clinically insignificant tidal volumes in preterm neonates between 24 and 34 weeks during non-spontaneous inflations20. Sharma et al. compared the pressures delivered by three different nasal interfaces (nasal mask, Hudson prong, RAM cannula) on 30 neonates in each group with gestation 28–34 weeks and birth weight ≥ 1000 g in our centre, during this study period21. We found that none of the nasal interfaces delivered oropharyngeal pressures equivalent to set CPAP pressures. Nasal mask delivered pressures best matched to the set CPAP pressures, while RAM cannula delivered the least effective pressures.
The incidence of patent ductus arteriosus requiring medical or surgical intervention was significantly higher in the RAM cannula group. On regression analysis, apart from the interface used, birth weight and need for mechanical ventilation within 72 h were found to be significantly associated with the incidence of PDA. It may emphasize that these infants were sicker, or it could also be a chance finding.
Strengths of this study include (a) use of a standard nasal injury chart that was used previously in published nCPAP studies, (b) meticulous monitoring for nasal injury in a structured format, (c) review of photographs by senior consultant neonatologist who was blinded to the outcome assessment, and (d) use of bubble CPAP as a primary mode of respiratory support, making our results more generalizable and applicable in resource-limited settings. Also, this is the largest study to date comparing RAM cannula with Hudson prong for nasal injury and CPAP failure. Limitations of this study are the exclusion of extremely preterm and extremely low birth weight infants, the risk group with maximum nasal injury and possible detection bias due to reporting of nasal injury using photographs.
Conclusion
For preterm infants on nCPAP, the use of RAM cannula with Cannulaide compared to Hudson prongs as interface reduces nasal injury with equivalent success rate for delivering nCPAP. However, this requires the use of a semipermeable dressing to provide a complete nasal seal. Duration of nCPAP was found to be associated with nasal injury apart from the interface. Further studies are needed to evaluate RAM cannula in reducing the nasal injuries when compared to a nasal mask, for efficacy in extremely preterm and extremely low birth weight infants.
Data availability
The data will be shared by the corresponding author on a reasonable request.
References
Ho, J. J., Subramaniam, P. & Davis, P. G. Continuous positive airway pressure (CPAP) for respiratory distress in preterm infants. Cochrane Database Syst. Rev. 10, CD002271 (2020).
de Bonfim, S. F. S. F., de Vasconcelos, M. G. L., de Sousa, N. F. C., da Silva, D. V. C. & Leal, L. P. Nasal septum injury in preterm infants using nasal prongs. Rev. Lat. Am. Enfermagem. 22, 826–833 (2014).
Fujii, K., Sugama, J., Okuwa, M., Sanada, H. & Mizokami, Y. Incidence and risk factors of pressure ulcers in seven neonatal intensive care units in Japan: A multisite prospective cohort study. Int. Wound J. 7, 323–328 (2010).
Ota, N. T., Davidson, J. & Guinsburg, R. Early nasal injury resulting from the use of nasal prongs in preterm infants with very low birth weight: A pilot study. Rev. Bras. Ter. Intensiva 25, 245–250 (2013).
Ottinger, D., Hicks, J., Wilson, S., Sperber, K. & Power, K. The pressure is on!: Neonatal skin and nasal continuous positive airway pressure. Adv. Neonatal Care Off. J. Natl. Assoc. Neonatal Nurses 16, 420–423 (2016).
Imbulana, D. I., Manley, B. J., Dawson, J. A., Davis, P. G. & Owen, L. S. Nasal injury in preterm infants receiving non-invasive respiratory support: A systematic review. Arch. Dis. Child. Fetal Neonatal Ed. 103, F29–F35 (2018).
Ramanathan, R. Nasal respiratory support through the nares: Its time has come. J. Perinatol. 30(Suppl), S67–72 (2010).
Drescher, G. S. & Hughes, C. W. Comparison of interfaces for the delivery of noninvasive respiratory support to low birthweight infants. Respir. Care 63, 1197–1206 (2018).
Singh, N., McNally, M. J. & Darnall, R. A. Does the RAM cannula provide continuous positive airway pressure as effectively as the hudson prongs in preterm neonates?. Am. J. Perinatol. 36, 849–854 (2019).
Claassen, C. C., Hillman, N. H., Brown, K., Williams, H. L. & Strand, M. L. Comparison of bubble CPAP devices using RAM cannula for extubation failure in very low birth weight infants: Randomized and cohort studies. Neonatology 115, 28–35 (2019).
Gokce, I. K., Kaya, H. & Ozdemir, R. A randomized trial comparing the short binasal prong to the RAM cannula for noninvasive ventilation support of preterm infants with respiratory distress syndrome. J. Matern. Fetal Neonatal Med. 34, 1868–1874 (2019).
Hochwald, O. et al. Cannula with long and narrow tubing versus short binasal prongs for noninvasive ventilation in preterm infants: Noninferiority randomized clinical trial. JAMA Pediatr. 175, 36–43 (2021).
Bailes, S. A. et al. Evaluating the effect of flow and interface type on pressures delivered with bubble CPAP in a simulated model. Respir. Care 61, 333–339 (2016).
Gerdes, J. S., Sivieri, E. M. & Abbasi, S. Factors influencing delivered mean airway pressure during nasal CPAP with the RAM cannula. Pediatr. Pulmonol. 51, 60–69 (2016).
Green, E. A., Dawson, J. A., Davis, P. G., De Paoli, A. G. & Roberts, C. T. Assessment of resistance of nasal continuous positive airway pressure interfaces. Arch. Dis. Child. Fetal Neonatal Ed. 104, F535–F539 (2019).
Iyer, N. P. & Chatburn, R. Evaluation of a nasal cannula in noninvasive ventilation using a lung simulator. Respir. Care 60, 508–512 (2015).
Mukerji, A. & Belik, J. Neonatal nasal intermittent positive pressure ventilation efficacy and lung pressure transmission. J. Perinatol. 35, 716–719 (2015).
Bashir, T., Murki, S., Kiran, S., Reddy, V. K. & Oleti, T. P. ‘Nasal mask’ in comparison with ‘nasal prongs’ or ‘rotation of nasal mask with nasal prongs’ reduce the incidence of nasal injury in preterm neonates supported on nasal continuous positive airway pressure (nCPAP): A randomized controlled trial. PLoS ONE 14, e0211476 (2019).
Khan, J. et al. Nasal injury and comfort with jet versus bubble continuous positive airway pressure delivery systems in preterm infants with respiratory distress. Eur. J. Pediatr. 176, 1629–1635 (2017).
Matlock, D. N. et al. Tidal volume transmission during non-synchronized nasal intermittent positive pressure ventilation via RAM® cannula. J. Perinatol. 39, 723–729 (2019).
Sharma, D. et al. Comparison of delivered distending pressures in the oropharynx in preterm infant on bubble CPAP and on three different nasal interfaces. Pediatr. Pulmonol. 55, 1631–1639 (2020).
Funding
This study was not funded from any source.
Author information
Authors and Affiliations
Contributions
S.M.1, S.M.2, S.N., S.K. and T.P.O. conceptualised the study. Data collection was done by S.M.1 and S.N., with help from D.S., S.A. and P.R.V.. R.P.A and S.K.D. provided important inputs to study design, data collection and manuscript. S.M.2, S.K., T.P.O., R.P.A. and S.K.D. supervised study conduct. S.M.1, S.M.2 and R.P.A. prepared the manuscript, with important inputs from S.N., S.K., T.P.O., S.K.D., D.S., S.A. and P.R.V. All authors have approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Maram, S., Murki, S., Nayyar, S. et al. RAM cannula with Cannulaide versus Hudson prongs for delivery of nasal continuous positive airway pressure in preterm infants: an RCT. Sci Rep 11, 23527 (2021). https://doi.org/10.1038/s41598-021-02988-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-02988-4
This article is cited by
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.