Abstract
The objective of this study was to evaluate the influence of exposure to meteorological conditions, including air pollution, on thyroid cancer. A nested case–control study was conducted utilizing 4632 patients with thyroid cancer and 18,528 control subjects who were matched at a 1:4 ratio by age group, sex, income, and region of residence. Korean National Health Insurance Service-Health Screening Cohort data from 2002 to 2015 were used. Odds ratios (ORs) with 95% confidence intervals (CIs) were calculated for thyroid cancer correlated with meteorological and air pollution exposure over a moving average of 3 years before the index dates. For all participants, the adjusted ORs associated with relative humidity (1.01, 95% CI 1.00–1.03, P value = 0.023), ambient atmospheric pressure (1.02, 95% CI 1.01–1.03, P value < 0.001), and sunshine duration (1.17, 95% CI 1.04–1.31, P value = 0.007) indicated correlations with the occurrence of thyroid cancer; however, these results were inconsistent in the subgroup analyses. Overall, exposure to nitrogen dioxide (NO2) (1.33, 95% CI 1.24–1.43, P value < 0.001) and particulate matter (PM10) (0.64, 95% CI 0.60–0.69, P value < 0.001) were related to thyroid cancer. These relationships persisted in the subgroup analyses. In conclusion, thyroid cancer occurrence was positively associated with NO2 exposure and negatively associated with PM10 exposure.
Similar content being viewed by others
Introduction
Thyroid cancer is an endocrine tumor with the highest occurrence, and its incidence has increased in recent decades1. Consequently, thyroid cancer is expected to be the fourth most common cancer in the USA by 20302. Increasing trends in thyroid cancer incidence have also been reported in China, Japan, and Korea3. The reason for these dramatic increasing trends is unclear. Researchers have postulated that overidentification or overdiagnosis of clinically occult, asymptomatic tumors as well as recent advancements in diagnostic technologies are responsible for the increase4,5. However, it is likely that other factors, such as environmental factors, lifestyle, family history and comorbidities, have significant roles in thyroid cancer development6,7.
Several environmental factors suggested to be endocrine disruptors have been associated with the occurrence of thyroid cancer. Exposure to certain chemical pollutants, such as decabromodiphenyl ether, which is a congener of polybrominated diphenyl ethers in flame retardants8, di(2-ethylhexyl)phthalate, which is a metabolite of phthalate in plastic materials and a plasticizer9, organochlorine pesticides10, and nitrates11 have been reported to be associated with thyroid cancer. In addition, exposures to certain environmental conditions have also been reported to have carcinogenic effects on the thyroid gland. For example, physical factors, such as ionizing radiation exposure11; geographic factors, such as living in a volcanic environment12; and a cold climate14 have been reported to be risk factors for thyroid cancer.
However, only a few reports support the potential association between air pollution and thyroid cancer, and no previous articles have been reported from Eastern Asian countries, such as Korea or Japan. When we searched PubMed using the terms ‘air pollution’ and ‘thyroid cancer’, a total of 10 relevant articles written in English were found between January 1991 and September 2021. Of these 10 articles, only two articles specifically evaluated the association between air pollution and thyroid cancer. An ecological study performed within European Union member states revealed a significant association between thyroid cancer incidence in men and benzo(k)fluoranthene (r2 = 0.2142, P value = 0.042) or hexachlorocyclohexane (r2 = 0.9993, P value = 0.0166) exposure13, and a more recently reported case–control study performed in the United States of America revealed that a 5 μg/m3 increase in exposure to fine particulate matter (diameter ≤ 2.5 μm, PM2.5) concentrations over 2 years (adjusted odds ratio [OR] = 1.18, 95% confidence interval [CI] 1.00–1.40) and 3 years (adjusted OR = 1.23, 95% CI 1.05–1.44) was associated with increased odds of papillary thyroid cancer15. A further literature review revealed only two more articles reporting the direct correlation between air pollution and thyroid cancer. Interestingly, air pollution originating from industrial waste gas was significantly positively associated with thyroid cancer occurrences in a Chinese population16, and overall exposure to urban PM10 showed a significant correlation with thyroid cancer incidence in Brazil17.
Because of the potential existence of regional variations in air pollution and racial differences in the response to air pollutants, we sought to perform an additional investigation of the association between air pollution and thyroid cancer in a Korean population by using a national cohort database. It was hypothesized in the present study that meteorological circumstances and air pollution may affect the incidence of thyroid cancer. A nested case–control study was performed to verify our hypothetical correlation between exposure to various meteorological parameters and air pollution for 3 years prior to the date of the initial diagnosis of thyroid cancer and the occurrence of thyroid cancer.
Results
General characteristics of the participants
The male to female ratio among the study participants was 0.27 (4965–18,195). Because the age groups were categorized using 5-year intervals, the mean age could not be defined (Table 1). The age group-, sex-, income level-, and region of residence-matched control group showed significant differences in the rate of obesity, smoking status, alcohol consumption habit, CCI scores, total cholesterol levels, SBP, and DBP compared to the thyroid cancer group. These factors were adjusted for in the subsequent analyses. Meteorological and air pollution parameters for 3 years prior to the index date showed significant differences in mean temperature, highest temperature, lowest temperature, ambient atmospheric pressure, sunshine duration, rainfall, O3, CO, and PM10 between the thyroid cancer and control groups (Table 1).
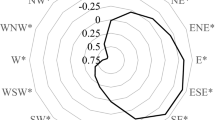
Meteorological conditions, air pollution parameters, and thyroid cancer
All of the meteorological and air pollution parameters except temperature range, mean relative humidity, mean SO2 and mean NO2 concentration were significantly associated with thyroid cancer according to the crude ORs (Table 2). In model 1, the mean temperature (1.04, 95% CI 1.01–1.07), lowest temperature (1.03, 95% CI 1.00–1.06, P value = 0.026), ambient atmospheric pressure (1.02, 95% CI 1.01–1.03), sunshine duration (1.21, 95% CI 1.09–1.34), rainfall (1.09, 95% CI 1.04–1.14), SO2 (0.69, 95% CI 0.48–0.98), O3 (1.17, 95% CI 1.07–1.28), CO (0.42, 95% CI 0.27–0.64), and PM10 (0.81, 95% CI 0.77–0.85) were significantly associated with the occurrence of thyroid cancer (Table 2).
In model 2, relative humidity (1.01, 95% CI 1.00–1.03, P value = 0.023), ambient atmospheric pressure (1.02, 95% CI 1.01–1.03), sunshine duration (1.17, 95% CI 1.04–1.31), NO2 (1.33, 95% CI 1.24–1.43), and PM10 (0.64, 95% CI 0.60–0.69) were significantly associated with the occurrence of thyroid cancer (Table 2).
Subgroup analysis according to age, sex, income, and region of residence
The model 2 outcomes of the subgroup analyses are summarized in Table 3. In the subgroup analysis by age, various meteorological factors and air pollutants were significantly associated with thyroid cancer. NO2 showed a higher OR in the young age group (age < 60 years old: 1.52, 95% CI 1.33–1.73) than in the old age group (age ≥ 60 years old: 1.03, 95% CI 1.02–1.04), and PM10 also showed a higher OR in the young age group (age < 60 years old: 0.66, 95% CI 0.59–0.73) than in the old age group (age ≥ 60 years old: 0.60, 95% CI 0.54–0.67). However, the positive association of NO2 and negative association of PM10 were consistent in both age groups. Inconsistent associations of meteorological factors and other air pollutants with thyroid cancer were observed in the subgroup analyses by sex, income, and region of residence. NO2 showed a higher OR in males (1.77, 95% CI 1.52–2.05) than in females (1.22, 95% CI 1.13–1.31), in the high-income group (1.36, 95% CI 1.25–1.47) than in the low-income group (1.18, 95% CI 1.06–1.31), and in the rural population (2.08, 95% CI 1.76–2.46) than in the urban population (1.27, 95% CI 1.08–1.50). However, NO2 showed a consistent positive association with thyroid cancer regardless of sex, income, or region of residence. In addition, PM10 showed a higher OR in females (0.69, 95% CI 0.63–0.75) than in males (0.51, 95% CI 0.43–0.60), in the low-income group (0.66, 95% CI 0.59–0.75) than in the high-income group (0.64, 95% CI 0.58–0.70), and in the rural population (0.70, 95% CI 0.57–0.86) than in the urban population (0.53, 95% CI 0.46–0.61). However, PM10 showed a consistent negative association with thyroid cancer regardless of sex, income, or region of residence.
Discussion
In the present study, the adjusted ORs associated with relative humidity (1.01, 95% CI 1.00–1.03), ambient atmospheric pressure (1.02, 95% CI 1.01–1.03), and sunshine duration (1.17, 95% CI 1.04–1.31) indicated positive correlations with the occurrence of thyroid cancer. However, these results were inconsistent in the subgroup analyses. Overall, NO2 (1.33, 95% CI 1.24–1.43) and PM10 (0.64, 95% CI 0.60–0.69) were significantly associated with thyroid cancer, and these relationships were consistently significant in the subgroup analyses. Only a few studies have investigated the relationship between air pollution and thyroid cancer. Our study is the first to comprehensively evaluate the association between air pollution and thyroid cancer with adjustments for various meteorological conditions using a nested case–control study design.
Because NO2 exposure induces oxidative stress and systemic inflammation and is involved in other pathogenic mechanisms, it has been recognized as a carcinogen11. Giannoula et al. showed in an ecological study that certain components of air pollutants may increase thyroid cancer incidence13. NO2 is a reactive compound in polluted air that has carcinogenic potential. It can initiate free radical reactions by interacting with unsaturated fatty acids and inducing the autooxidation of organic compounds18,19. A significant association between chronic exposure to NO2 and lung cancer (OR 1.30, 95% CI 1.02–1.66) has been reported20, and genomic instability and thyroid hypertrophy through the overproduction of cellular reactive oxygen species (ROS) have been postulated as potential mechanisms by which NO2 induces thyroid cancer11. Therefore, the positive association between NO2 and the occurrence of thyroid cancer shown in our results may also be related to NO2-induced oxidative stress and the overproduction of cellular ROS.
In addition, NO2 is known as a potential endocrine-disrupting chemical. In a previous report, an increased NO2 concentration in air pollutants showed a strong correlation with elevated odds of primary hypothyroidism (Spearman correlation coefficients; adolescent female = 0.94, adolescent male = 0.94)21. In addition, annual average exposure to ambient NO2 was significantly correlated with a decrease in the free thyroxine (FT4) concentration (β-coefficients [SE]: − 0.0072 [0.0024], P value = 0.003) and an increase in thyroid-stimulating hormone (TSH) (β-coefficients [SE]: 0.0131 [0.0053], P value = 0.01)22. In animals, the release of excess TSH has been reported to induce various thyroid diseases, including thyroid cancer23. Moreover, there is evidence of TSH receptor signaling as an oncogenic pathway in developing thyroid cancer23. Based on these findings, we have also postulated that consistent exposure to NO2 in air pollutants can increase circulating TSH, resulting in increased TSH receptor signaling and an increased incidence of thyroid cancer.
Although higher concentrations of PM2.5 and PM10 (surrogate indicators for air pollution) have been reported to be disruptive to the endocrine system and carcinogenic in humans15,24, previous studies showed inconsistent results of the association between PM and thyroid function. Cong reported that exposure to waste gas-emitted ambient air pollution was positively correlated with an increased thyroid cancer incidence (rs = 0.716, P value < 0.001)16. However, it was reported that outdoor PM2.5 exposure was not correlated with death due to most non-lung cancers, such as thyroid cancer (hazard ratio 0.62, 95% CI 0.34–1.12)25. Additionally, the PM10 concentration was not strongly associated with an elevated risk of primary hypothyroidism (Spearman correlation coefficients; adult female: 0.89, adult male: 0.89)21, and the average level of PM10 exposure was positively associated with the TSH level in only men (β-coefficient [SE]: 0.0159 [0.0074], P value = 0.03); additionally, no significant association with the overall change in the FT4 (β-coefficient [SE]: − 0.0029 [0.0030], P value = 0.33) or TSH level (β-coefficient [SE]: 0.0103 [0.0066], P value = 0.12) was observed22. Ghassabian et al. reported that there were no significant associations between PM10 and decreased FT4 in pregnant women (OR 1.18, 95% CI 0.93–1.48), and only high exposure to PM2.5 was related to hypothyroxinemia (OR 1.21, 95% CI 1.00–1.47)26.
Considering the previously reported carcinogenic effects of PM, our study results unexpectedly showed a negative association between PM10 and thyroid cancer. Yanagi et al. reported that the statistical correlation between overall exposure to urban PM10 and thyroid cancer incidence was high and significant17. The induced systemic inflammation and the immune response to autoantigens resulting in the production of ROS have been proposed as mechanisms of PM carcinogenesis in thyroid cancer patients11. However, our study results support the following study results regarding the endocrine-disrupting effect of PM10. Oziol et al. reported that ambient air in French urban areas had thyroid receptor alpha-1 agonistic effects without competitive effects with regard to T3-dependent transcriptional activity27. Similarly, Nováková et al. conducted an in vitro experiment and found that exposure to PM10 in ambient air significantly increased thyroid receptor-mediated activity, and exposure to a submicrometer fraction of PM10, namely, particles sized 0.49–0.95 µm, was associated with the highest activity28. Additionally, Dong et al. reported that PM2.5 exposure was significantly connected with decreased serum levels of triiodothyronine (T3), T4, and TSH (P value < 0.05) in an in vivo female rat model29. The authors also reported that PM2.5 exposure repressed the biosynthesis and biotransformation of thyroid hormones (THs) by activating the hypothalamic-pituitary-thyroid (HPT) axis and inducing hepatic transthyretin29. Moreover, Zeng et al. conducted a retrospective cross-sectional study and concluded that a 10 µg/m3 increase in PM2.5 was associated with a 0.12 pmol/L decrease in FT4 and a 0.07 pmol/L increase in FT3, and the FT4/FT3 ratio was inversely associated with PM2.5 (coefficient: − 0.06, P value < 0.01)30. Based on these findings, we postulate that PM10 decreases the incidence of thyroid cancer through increased thyroid receptor-mediated activity by increasing FT3, which results in decreased TSH levels, initiation of the HPT axis, and induction of hepatic transthyretin.
Several limitations are present regarding the interpretation of the present results. First, although age group, sex, income, and region of residence were matched and adjusted for, lifestyle factors, such as obesity (BMI), tobacco smoking, and alcohol consumption habits, as well as the CCI score, total cholesterol level, SBP, and DBP, were not matched between the two groups in this study. Moreover, family history of thyroid cancer, dietary habits, physical activity, and history of radiation exposure were not surveyed in this study. Second, interactions of variable combinations of air pollutants and meteorological conditions could not be excluded. Although multiple air pollutants, namely, SO2, NO2, O3, CO, and PM10, were considered in this study, the effect of PM2.5 was not analyzed because PM2.5 was not measured before 2015 in Korea. Third, potential errors of meteorological or air pollutant exposure category was inevitable in this study. Since the estimation of meteorological and air pollutant exposure was conducted by the region of residence of each participant rather than by taking individual patterns of activity and living sphere into account, intersubject variability was possible. Fourth, the positive associations of relative humidity, ambient atmospheric pressure, and sunshine duration were not retained or consistent in the subgroup analyses. There is insufficient evidence to explain the effects of sex, age, socioeconomic status, and site of residence on the association of meteorological conditions and thyroid cancer. Thus, further studies to evaluate associations between various meteorological conditions and exposure to air pollutants in the abovementioned subgroups are required to investigate the exact effect of each component on thyroid cancer. Fifth, information about indoor air pollutant exposure was unavailable. For example, exposure to indoor NO2 from fuel-fired apparatuses and stoves and cigarette smoking might have influenced the present results. Sixth, 3 years prior to diagnosis may not be sufficient for the development of thyroid cancer. However, we tried to overcome this limitation by including the region of residence, which reflected continuous exposure to certain air pollutants and meteorological conditions that affected the occurrence of thyroid cancer, as a cofactor. Seventh, as this study used NHIS data, we could not include thyroid cancer patients who did not visit any medical clinic or hospital. Additionally, those with undetected thyroid cancer might have been included among the control participants. Finally, because meteorological conditions and air pollution levels are distinct by region, the comprehension of this study outcomes may be limited to the Korean Peninsula. Additional studies in distinct geographical regions are needed to contemplate specific characteristics in variable regions.
In conclusion, the mean concentration of NO2 in the 3 years before the onset of thyroid cancer was significantly related to an increased risk of thyroid cancer in the thyroid cancer group, while the mean concentration of PM10 was associated with a significantly decreased risk in the thyroid cancer group compared to that in the control group. In addition, the positive association of NO2 and the negative association of PM10 was consistent regardless of age group, sex, income level, or region of residence. Therefore, consistent efforts to decrease NO2 in the ambient air should be made to relieve the worldwide increase in the incidence of thyroid cancer, while further multinational ecological studies should be performed to ascertain the precise relationship between PM10 and thyroid cancer.
Methods
Ethics
The ethics committee of Hallym University (2019–10-022) permitted this study. Written informed consent was waived by the Institutional Review Board of Hallym University. This study was performed in accordance with the Declaration of Helsinki and followed the STROBE (Strengthening the Reporting of Observational Studies in Epidemiology) guidelines for reporting.
Study population and participant selection
We analyzed Korean National Health Insurance Service-Health Screening Cohort (NHIS-HEALS) data (which is not publicly available data and can be accessed only after acquiring permission from IRB, passing the internal screening held by the National Health Insurance Service of Korea, and paying the cost to acquire the data) between 2002 and 2015 and meteorological and air pollution parameters from the meteorological administration, as described in the supplementary material (S1 description) and in previous studies31,32.
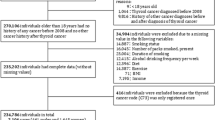
Participants who were diagnosed with thyroid cancer were selected from 514,866 patients with 615,488,428 medical claim codes (n = 5769). To ensure the availability of air pollution exposure data for 5 years before the index date, we excluded thyroid cancer participants who were diagnosed from 2002 to 2006 (n = 1133). The control group comprised participants who did not have thyroid cancer from 2002 to 2015, and they were selected from the total population (n = 509,097). Participants who died before 2007 or had no records since 2007 (n = 10,917) were excluded from the control group. In addition, control participants were excluded if they were diagnosed with the C73 (malignant neoplasm of the thyroid gland) International Classification of Diseases 10th revision (ICD-10) code and did not undergo thyroidectomy (n = 2013). The thyroid cancer group was matched with the control group in a 1:4 ratio by age group, sex, income, and region of residence. The random number method was utilized in selecting the control groups to countervail the selection bias. The time of thyroid cancer diagnosis was referred to as the index date for thyroid cancer patients. A random day within the 1-year period prior to the index date of each thyroid cancer participant was defined as the index date for participants in the control group. Therefore, participants with an index date between 2007 and 2015 were included in the control group. Throughout the matching procedure, 477,639 participants in the control group and 3 participants in the thyroid group were excluded. Consequently, 4632 thyroid cancer participants were matched in a 1:4 ratio with 18,528 control participants (Fig. 1).
A schematic illustration of the participant selection process that was used in the present study. Of a total of 514,866 participants, 4632 thyroid cancer participants were matched with 18,528 control participants for age, sex, income, and region of residence. Then, the thyroid cancer and control groups were linked with meteorological data and air pollution data before the index date.
The meteorological and air pollution parameters over a moving average of 1 year (365 days), 3 years (1095 days), and 5 years (1825 days) before the index date were investigated and compared among the thyroid cancer group and the control group.
Variables
Independent variables
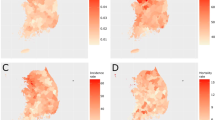
Daily mean temperature (°C), highest temperature (°C), lowest temperature (°C), and temperature range (°C), along with relative humidity (%), ambient atmospheric pressure (hPa), sunshine duration (hr), precipitation (mm), SO2 (ppm), NO2 (ppm), O3 (ppm), CO (ppm), and PM10 (µg/m3) for moving averages of 1 year (365 days), 3 years (1095 days), and 5 years (1825 days) before the index dates, were defined as the independent variables, as described in previous studies31,32.
Covariates
Patients were stratified into age groups with 5-year intervals: 45–49, 50–54…, and 85 + years old (9 age groups). Income level was stratified into 5 classes as follows: class 1 (lowest income) to class 5 (highest income). The region of residence was stratified into urban (Seoul, Busan, Daegu, Incheon, Gwangju, Daejon, and Ulsan) and rural (Gyeonggi, Gangwon, Chungcheongbuk, Chungcheongnam, Jeollabut, Jeollanam, Gyeongsangbuk, Gyeongsangnam, and Jeju) areas according to the classification of administrative districts by the Korean government, which have been described in a previous study33. Tobacco smoking was categorized according to the participant’s current smoking status (nonsmoker, past smoker, or current smoker), alcohol consumption was classified on the basis of the frequency of alcohol consumption (< 1 time a week and ≥ 1 time a week), and obesity regarded by body mass index (BMI, kg/m2) was categorized as underweight (< 18.5), normal (≥ 18.5 to < 23), overweight (≥ 23 to < 25), obese I (≥ 25 to < 30), and obese II (≥ 30) as described in previous studies34,35. Systolic blood pressure (SBP), diastolic blood pressure (DBP), fasting blood glucose, and total cholesterol levels were measured. The Charlson Comorbidity Index (CCI) was used to assess the underlying comorbidity status36, which was rated from 0 (no comorbidities) to 29 (multiple comorbidities), and thyroid cancer was omitted from the rating score.
Dependent variable
The diagnosis of thyroid cancer was referred to as participants with ICD-10 code C73 (malignant neoplasm of the thyroid gland) and treatment claim codes for thyroidectomy (P4551, P4552, P4553, P4554, and P4561)6,7.
Statistical analyses
The comparison of general characteristics of two groups was conducted using the chi-square test (independent variables) and the independent t-test (continuous variables). The mean meteorological and air pollution parameters for 3 years (1095 days) before the index date in the two groups were compared using the independent t-test.
To assess the relationship between meteorological and air pollution exposure and thyroid cancer, each parameter was compared between the thyroid cancer group and the control group. The odds ratios (ORs) with 95% confidence intervals (CIs) of each parameter in the thyroid cancer group were evaluated using conditional logistic regression analysis within three different models constructed as follows: a crude (simple) model, model 1 (adjusted for total cholesterol, SBP, DBP, fasting blood glucose, obesity, smoking status, alcohol consumption habit, and CCI score), and model 2 (adjusted for model 1 plus daily temperature range, relative humidity, pressure, sunshine duration, SO2, NO2, O3, CO, and PM10 applying the forward selection method). Age group, sex, income, and region of residence were stratified in these analyses. Furthermore, the correlation between each of meteorological conditions and air pollution parameters were statistically analyzed to preclude the effect of collinearity between each covariates in model 2 (Table S2). Among 365 days, 1095 days, and 1825 days of exposure durations, we selected 1095 days as the main exposure term. The results of the other durations are presented in the supplemental files (Tables S3 and S4).
For subgroup analysis, we stratified participants by age (< 60 years old and ≥ 60 years old), sex (males and females), income (low and high income), and region of residence (urban and rural area), and ORs in model 2 were evaluated. The outcomes of the subgroup analyses of other durations of exposure are presented in the supplemental files (Tables S5 and S6).
Two-tailed analyses were performed, and a P value less than 0.05 was considered the significance level. SAS version 9.4 (SAS Institute Inc., Cary, NC, USA) was utilized in the statistical analysis.
References
Sanabria, A. et al. Growing incidence of thyroid carcinoma in recent years: factors underlying overdiagnosis. Head. Neck. 40(4), 855–866. https://doi.org/10.1002/hed.25029 (2018).
Rahib, L. et al. Projecting cancer incidence and deaths to 2030: the unexpected burden of thyroid, liver, and pancreas cancers in the United States. Cancer. Res. 74(11), 2913–2921. https://doi.org/10.1158/0008-5472.CAN-14-0155 (2014).
Li, R., Wang, Y. & Du, L. A rapidly increasing trend of thyroid cancer incidence in selected East Asian countries: joinpoint regression and age-period-cohort analyses. Gland. Surg. 9(4), 968–984. https://doi.org/10.21037/gs-20-97 (2020).
O’Grady, T. J., Gates, M. A. & Boscoe, F. P. Thyroid cancer incidence attributable to overdiagnosis in the United States 1981–2011. Int. J. Cancer. 137(11), 2664–2673. https://doi.org/10.1002/ijc.29634 (2015).
Vaccarella, S. et al. The Impact of diagnostic changes on the rise in thyroid cancer incidence: a population-based study in selected high-resource countries. Thyroid 25(10), 1127–1136. https://doi.org/10.1089/thy.2015.0116 (2015).
An, S. Y. et al. Obesity is positively related and tobacco smoking and alcohol consumption are negatively related to an increased risk of thyroid cancer. Sci. Rep. 10(1), 19279. https://doi.org/10.1038/s41598-020-76357-y (2020).
Byun, S. H., Min, C., Choi, H. G. & Hong, S. J. Association between family histories of thyroid cancer and thyroid cancer incidence: a cross-sectional study using the Korean genome and epidemiology study data. Genes. (Basel) 11(9), 1039. https://doi.org/10.3390/genes11091039 (2020).
Alsen, M. et al. Endocrine disrupting chemicals and thyroid cancer: an overview. Toxics. 9(1), 14. https://doi.org/10.3390/toxics9010014 (2021).
Marotta, V. et al. Human exposure to bisphenol AF and diethylhexylphthalate increases susceptibility to develop differentiated thyroid cancer in patients with thyroid nodules. Chemosphere 218, 885–894. https://doi.org/10.1016/j.chemosphere.2018.11.084 (2019).
Han, M. A., Kim, J. H. & Song, H. S. Persistent organic pollutants, pesticides, and the risk of thyroid cancer: systematic review and meta-analysis. Eur. J. Cancer. Prev. 28(4), 344–349. https://doi.org/10.1097/CEJ.0000000000000481 (2019).
Fiore, M. et al. Role of emerging environmental risk factors in thyroid cancer: a brief review. Int. J. Environ. Res. Public. Health. 16(7), 1185. https://doi.org/10.3390/ijerph16071185 (2019).
Vigneri, R., Malandrino, P., Gianì, F., Russo, M. & Vigneri, P. Heavy metals in the volcanic environment and thyroid cancer. Mol. Cell. Endocrinol. 457, 73–80. https://doi.org/10.1016/j.mce.2016.10.027 (2017).
Giannoula, E. et al. Ecological study on thyroid cancer incidence and mortality in association with European Union member states’ air pollution. Int. J. Environ. Res. Public. Health. 18(1), 153. https://doi.org/10.3390/ijerph18010153 (2020).
Lehrer, S. & Rosenzweig, K. E. Cold climate is a risk factor for thyroid cancer. Clin. Thyroidol. 26(10), 273–276. https://doi.org/10.1089/ct.2014;26.273-276 (2014).
Karzai, S. et al. Ambient particulate matter air pollution is associated with increased risk of papillary thyroid cancer. Surgery. S0039–6060(21), 00415–00423. https://doi.org/10.1016/j.surg.2021.05.002 (2021).
Cong, X. Air pollution from industrial waste gas emissions is associated with cancer incidences in Shanghai, China. Environ. Sci. Pollut. Res. Int. 25(13), 13067–13078. https://doi.org/10.1007/s11356-018-1538-9 (2018).
Yanagi, Y., de Assunção, J. V. & Barrozo, L. V. The impact of atmospheric particulate matter on cancer incidence and mortality in the city of Sao Paulo, Brazil. Cad. Saude. Publica. 28(9), 1737–1748. https://doi.org/10.1590/s0102-311x2012000900012 (2012).
Darbre, P. D. Overview of air pollution and endocrine disorders. Int. J. Gen. Med. 11, 191–207. https://doi.org/10.2147/IJGM.S102230 (2018).
Tattersfield, A. Department of health advisory group on the medical aspects of air pollution episodes. Third report: oxides of nitrogen. (Her Majesty Stationary Office, 1993).
Vineis, P. et al. Air pollution and risk of lung cancer in a prospective study in Europe. Int. J. Cancer. 119(1), 169–174. https://doi.org/10.1002/ijc.21801 (2006).
Zaccarelli-Marino, M. A., Alessi, R., Balderi, T. Z. & Martins, M. A. G. Association between the occurrence of primary hypothyroidism and the exposure of the population near to industrial pollutants in Sao Paulo State, Brazil. Int. J. Environ. Res. Public. Health. 16(18), 3464. https://doi.org/10.3390/ijerph16183464 (2019).
Kim, H. J., Kwon, H., Yun, J. M., Cho, B. & Park, J. H. Association between exposure to ambient air pollution and thyroid function in Korean adults. J. Clin. Endocrinol. Metab. 105(8), dgaa338. https://doi.org/10.1210/clinem/dgaa338 (2020).
Rowe, C. W. et al. Targeting the TSH receptor in thyroid cancer. Endocr. Relat. Cancer. 24(6), R191–R202. https://doi.org/10.1530/ERC-17-0010 (2017).
Colao, A., Muscogiuri, G. & Piscitelli, P. Environment and health: not only cancer. Int. J. Environ. Res. Public. Health. 13(7), 724. https://doi.org/10.3390/ijerph13070724 (2016).
Turner, M. C. et al. Ambient air pollution and cancer mortality in the cancer prevention study II. Environ. Health. Perspect. 125(8), 087013. https://doi.org/10.1289/EHP1249 (2017).
Ghassabian, A. et al. Association of exposure to ambient air pollution with thyroid function during pregnancy. JAMA. Netw. Open. 2(10), e1912902. https://doi.org/10.1001/jamanetworkopen.2019.12902 (2019).
Oziol, L. et al. First characterization of the endocrine-disrupting potential of indoor gaseous and particulate contamination: comparison with urban outdoor air (France). Environ. Sci. Pollut. Res. Int. 24(3), 3142–3152. https://doi.org/10.1007/s11356-016-8045-7 (2017).
Nováková, Z. et al. Toxic potentials of particulate and gaseous air pollutant mixtures and the role of PAHs and their derivatives. Environ. Int. 139, 105634. https://doi.org/10.1016/j.envint.2020.105634 (2020).
Dong, X. et al. PM 2.5 disrupts thyroid hormone homeostasis through activation of the hypothalamic-pituitary-thyroid (HPT) axis and induction of hepatic transthyretin in female rats 2.5. Ecotoxicol. Environ. Saf. 208, 111. https://doi.org/10.1016/j.ecoenv.2020.111720 (2021).
Zeng, Y., He, H., Wang, X., Zhang, M. & An, Z. Climate and air pollution exposure are associated with thyroid function parameters: a retrospective cross-sectional study. J. Endocrinol. Invest. 44(7), 1515–1523. https://doi.org/10.1007/s40618-020-01461-9 (2021).
Choi, H. G., Min, C. & Kim, S. Y. Air pollution increases the risk of SSNHL: a nested case-control study using meteorological data and national sample cohort data. Sci. Rep. 9(1), 8270. https://doi.org/10.1038/s41598-019-44618-0 (2019).
Kim, S. Y., Kong, I. G., Min, C. & Choi, H. G. Association of air pollution with increased risk of peritonsillar abscess formation. JAMA. Otolaryngol. Head. Neck. Surg. 145(6), 530–535. https://doi.org/10.1001/jamaoto.2019.0742 (2019).
Kim, S. Y., Min, C., Oh, D. J. & Choi, H. G. Bidirectional association between GERD and asthma: two longitudinal follow-up studies using a national sample cohort. J. Allergy. Clin. Immunol. Pract. 8(3), 1005-1013.e9. https://doi.org/10.1016/j.jaip.2019.10.043 (2020).
World Health Organization. Regional Office for the Western Pacific. The Asia-Pacific perspective : redefining obesity and its treatment. Sydney: Health Communications Australia. https://apps.who.int/iris/handle/10665/206936 (2000).
Kim, S. Y., Oh, D. J., Park, B. & Choi, H. G. Bell’s palsy and obesity, alcohol consumption and smoking: a nested case-control study using a national health screening cohort. Sci. Rep. 10(1), 4248. https://doi.org/10.1038/s41598-020-61240-7 (2020).
Quan, H. et al. Updating and validating the Charlson comorbidity index and score for risk adjustment in hospital discharge abstracts using data from 6 countries. Am. J. Epidemiol. 173(6), 676–682. https://doi.org/10.1093/aje/kwq433 (2011).
Acknowledgements
The manuscript was edited for proper English language, grammar, punctuation, spelling, and overall style by the native English–speaking editors at American Journal Experts.
Funding
This work was supported in part by research grants (NRF-2018-R1D1A1A0-2085328; NRF-2021-R1C1C100498611) from the National Research Foundation (NRF) of Korea. No funding bodies had any role in the study design, data collection and analysis, decision to publish, or preparation of the article.
Author information
Authors and Affiliations
Contributions
H.G.C had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. S.J.P. and H.G.C. contributed to study concept and design; acquisition, analysis, and interpretation of data; study supervision; and drafting of the main manuscript text and H.G.C. also contributed to statistical analysis; administrative, technical, and material support; and obtained funding for this study. C.M. and D.M.Y. contributed to acquisition, analysis, and interpretation of data; statistical analysis; administrative, technical, and material support. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Park, S.J., Min, C., Yoo, D.M. et al. National cohort and meteorological data based nested case–control study on the association between air pollution exposure and thyroid cancer. Sci Rep 11, 21562 (2021). https://doi.org/10.1038/s41598-021-00882-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-00882-7
This article is cited by
-
Socioeconomic disparity in the association between fine particulate matter exposure and papillary thyroid cancer
Environmental Health (2023)
-
Environmental factors and incidence of thyroid cancer in the world (1990–2019): an ecological study
Environmental Science and Pollution Research (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.