Abstract
This study examined associations between dietary intake and gut and systemic inflammation assessed by fecal calprotectin ≤ or > 100 μg/mg (FCP), C-reactive protein ≤ or > 5 mg/L (CRP) and serum cytokine profiles in Crohn’s disease (CD) patients in clinical remission. A 3-month observational study was conducted at the University of Calgary in Calgary, Alberta, Canada between 2016 and 2018 in 66 outpatients with CD in clinical remission. FCP was obtained from stool samples at baseline and 3-months and serum CRP and serum cytokines were assessed at 3-months only (n = 41). Dietary intakes were collected using 3-day food records at baseline and 3-months and categorized as: PREDIMED Mediterranean diet scores (pMDS) total and individual components, the dietary inflammatory index (DII), food groups, and common micro- and macro-nutrients. Statistical models were developed to identify relationships between dietary factors and FCP, CRP and cytokine levels. Daily intake of leafy green vegetables was associated with FCP ≤ 100 μg/mg (p < 0.05). Increasing omega 6:3 ratio was associated with CRP ≤ 5 mg/L (p = 0.02). Different cytokines were significantly associated with various dietary variables. Future studies in patients with greater disease activity should be undertaken to explore these relationships.
Similar content being viewed by others
Introduction
Inflammatory bowel disease (IBD) is believed to arise from a shared interaction between genetic and environmental influences1, resulting in an imbalance between pro- and anti-inflammatory signalling. There has been a steady rise in incident cases of IBD over the past several decades with the highest prevalence rates seen in Europe and North America of approximately 0.3% of the population2. Its recent increase in incidence across newly industrialized countries suggests environmental factors induce or modify disease expression. This has occurred in parallel with global dietary shifts towards a more “Western” style of eating. Common medical therapies include corticosteroids, immunomodulatory and biologic agents, and surgery. However, these therapies are not universally effective, the disease may recur and drugs may be associated with serious side effects. Recently, guidelines have included dietary therapies as a treatment option3.
Western diets are characterized by high intakes of total, polyunsaturated fatty acids (PUFA) and saturated fats, red and processed meats, commercial baked goods, sweetened beverages and food additives such as carrageenan, maltodextrin and emulsifiers together with low intakes of phytochemicals, fibre, fruits, vegetables and fish4,5,6,7,8. This dietary pattern can alter the gut microbiota and impair intestinal barrier function, thus resulting in a cascade of reactions that may trigger an enhanced inflammatory response. In contrast, prospective cohort and intervention studies have identified certain dietary patterns and individual diet components that may reduce gut inflammation and improve symptoms in IBD7,9,10,11,12. While knowledge of dietary relationships with the gut microbiome in IBD is evolving, the effects of dietary patterns and components on systemic markers of immune function is unexplored.
Given this context, it is justified to investigate the effect of dietary patterns and individual dietary components on surrogate biomarkers of Crohn’s disease (CD) activity and systemic markers of inflammation. Fecal calprotectin (FCP) is a useful surrogate marker of gastrointestinal inflammation and levels less than 100 µg/g are consistently associated with disease remission, whereas levels > 250 µg/g predict disease relapse13. C-Reactive Protein (CRP) is a marker of systemic inflammation and is associated with therapeutic response in IBD, and CRP levels correlate modestly with endoscopic disease activity14. Furthermore, serum cytokines have been associated with clinical remission and mucosal healing. With the above described rationale for these disease specific biomarkers, our study objective was to examine associations between gut and systemic inflammation assessed FCP ≤ or > 100 μg/mg, CRP ≤ or > 5 mg/L with dietary intake in patients with CD in remission. Exploratory analyses between serum cytokine profiles and dietary components were undertaken to characterize the relationship between diet and systemic markers of immune status.
Material and methods
Study design
A 3-month observational study of patients with CD was conducted at the gastrointestinal outpatient clinic at the University of Calgary, Alberta, Canada between 2016 and 2018.
Inclusion/exclusion criteria
Inclusion criteria were: (a) ≥ 18 years of age; (b) documented diagnosis of luminal ileal and/or ileocolonic CD based on conventional criteria; (c) steroid-free clinical remission defined by a Harvey Bradshaw Index (HBI) < 5 for at least three months; d) achieved induction of remission either through anti-tumor necrosis factor (anti-TNF) agents or corticosteroids, and maintenance of remission with anti-TNF agents either with or without immunomodulators; and (e) able to provide informed consent, and read and write in English. Patients were excluded if they had (a) > 1 bowel resection; (b) evidence of fistulizing or stricturing disease CD; (c) upper gastrointestinal disease, or; (d) an ostomy.
Data collection
Patient-related characteristics (i.e., age, sex, height, weight, body mass index: BMI) and medical history (i.e., treatment with anti-tumor necrosis factor biologics and immunomodulators at baseline and previous small bowel resection) were captured during the first study visit (n = 66). Stool was obtained at baseline and 3-months for FCP, whereas serum was collected for CRP and cytokine levels at 3 months only in patients who presented for timely follow-up collection (n = 41); patient demographics are presented in Table 1. Several inflammatory (Tumour Necrosis Factor alpha (TNF-α), interferon gamma (IFN-γ), interleukins 4, 6, 8, 17a, and 12/23p40 (i.e., IL-4, IL-6, IL-8, IL-17a, IL-12/23p40) and regulatory (IL-10 and IL-27) cytokines (all pg/mL) were examined. Cytokines were evaluated using electro-chemiluminescent, multi-plex ELISA kits by MesoScale Discovery (Rockville, MD, USA) as per the manufacturer’s protocol.
Dietary intake was determined using 3-day weighed food records at baseline and 3-months. Study participants met with the study coordinator to receive training on how to record an accurate 3-day weighed food record and were instructed to document all food and drinks consumed and preparation method on two representative non-consecutive weekdays, and one weekend day. The study dietitian reviewed the food record with the patient to identify any missing information.
Dietary intake data was analyzed using ESHA Food Analysis Software Version 11.3 X, ESHA Food Processor Nutrition Analysis Software (Salem, OR, USA), and individual macro- and micro-nutrients amounts were calculated. Dietary intakes were categorized using the following:
-
1.
Mediterranean Diet Score (pMDS15), modified to exclude red wine consumption8, was calculated for each patient to measure how closely their overall dietary pattern resembled a Mediterranean diet.
-
2.
The dietary inflammatory index (DII) developed by Shivappa et al.16 was calculated to score the inflammatory potential of individual dietary patterns.
-
3.
Canada’s Food Guide to Healthy Eating (CFGHE) food group serving sizes was used to examine servings of fruits, vegetables, leafy green vegetables, red and processed meats, legumes, fish, and nuts and seeds17. Definitions of serving sizes for each food group have been previously reported8.
Statistical analyses
All data management and statistical analyses were conducted in R version 3.5.318, and a p-value < 0.05 was considered statistically significant. Outcomes of interest included FCP, dichotomized at 100 μg/mg to discriminate between patients in active or inactive intestinal inflammation19; CRP dichotomized at 5 mg/L20, and various inflammatory and/or regulatory cytokines (Table 1). Dietary variables explored in this analysis included total pMDS and its sub-components8; the DII, CFGHE food group servings; macro- and micro-nutrient intake and miscellaneous aspects of dietary intake (Tables 2, 3). Other patient characteristics including age in years at baseline, body mass index, previous bowel surgery, height, sex, taking anti-TNF medication or immunosuppressants, and weight were assessed as potential confounders of the associations of interest.
The association between FCP and diet was assessed using a mixed-effects logistic regression model to account for within-patient correlations between baseline and follow-up, and was implemented using the R package “lme4”21. This allowed the model to account for the within-patient correlation affecting the strength of the associations as it incorporated a random-effects term in the model to capture this correlation. Linear regression models were used to determine the association between diet and cytokine measurements using the R “stats” package (R Core Team, 2019), while logistic regression models were used to determine the association between CRP and diet.
Descriptive statistics and visualization were used to identify and explore outliers. The “ggplot2” library was used for all exploratory visualizations and plotting. Regression models were then built in a mixed stepwise manner, beginning with a forward-stepwise selection based on univariable associations with the outcomes (P < 0.15), followed by a backwards-elimination while assessing confounding (removal of the variable causes a change in the remaining coefficient estimates of ± 30%), and retained only the variables with P < 0.10. Interactions between variables were not assessed due to the small sample sizes resulting from the stratification necessary to test the corresponding interactions.
Ethical approval
The study was approved by the Calgary Health Research Ethics Board (REB15-1805) and informed consent was provided by all patients. All the research was carried out in accordance with relevant guidelines and regulations.
Results
Demographics
Table 1 describes the demographics and health characteristics for patients at baseline and 3-months. At baseline, participants were generally middle aged (Median = 51 years, IQR = 37–58) overweight (Median = 27.3 kg/m2, IQR = 23.5–29.7) and 49% were male. All patients were in clinical remission (HBI < 5) and 64% of patients were in biological remission defined as FCP ≤ 100 μg/mg. At baseline, 53 patients (80%) were receiving anti-TNF biologics, with 29 patients (44%) receiving immunomodulators and no patients receiving corticosteroids.
Dietary pattern and macro- and micro-nutrients
Patients’ DII scores were generally pro-inflammatory (Mean = 1.6, SD = 1.8) and pMDS scores showed only 4–5 healthy behaviours being performed (Mean = 4.6, SD = 1.5) out of a possible 13. Means and proportions of dietary patterns, individual food groups and macro- and micro-nutrients used in the analyses are described in Tables 2 and 3.
Fecal calprotectin
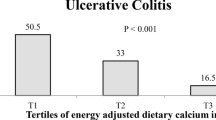
Increasing daily servings of leafy green vegetables were associated with FCP ≤ 100 μg/mg (p < 0.05; Table 4, Fig. 1).
C-reactive protein
When assessing the odds of having a low CRP at 3-months (defined as a serum concentration ≤ 5 mg/L), males had higher odds of having a low CRP than females (Table 4). In addition, a higher omega 6:3 fatty acids ratio increased the odds CRP would be ≤ 5 mg/L (Fig. 2). The mean omega 6:omega-3 (n-6:n-3) PUFA ratio in the low CRP group was 8:1, compared to the high CRP group with a ratio of 4:1.
Serum cytokines
Serum cytokine relationships with dietary variables are presented in Table 4. Different cytokines were significantly associated with various dietary variables. Considering dietary pattern, a negative association between energy adjusted DII and IL-12/23 p40 (P = 0.04), and positive association between pMDS and IL-17A (P = 0.03) was observed, pMDS and DII scores were not associated with the remaining serum cytokines.
Discussion
We present the first prospective study to characterize the relationship between pMDS, DII, CFGHE food groups, micro- and macro-nutrients with serum and fecal biomarkers of disease activity and peripheral cytokine profiles in patients with CD in clinical remission. Daily servings of leafy green vegetables was associated with FCP ≤ 100ug/mg, and an n-6:n-3 PUFA ratio of 8:1 was associated with CRP ≤ 5 mg/L. We did not identify relationships for FCP or CRP with dietary patterns measured by pMDS and energy-adjusted DII.
Epidemiological studies have associated fruit, vegetable and fish intake with lower risk of IBD incidence22,23. Leafy greens are a rich source of carotenoids which may help improve intestinal barrier function and reverse lipopolysaccharides induced intestinal barrier damage through enhancing the expression of tight junction proteins24. A plant-based diet, rich in dietary fiber, appears to be beneficial for human health by promoting the development of a diverse microbial ecosystem25; in this study however, total dietary fiber was not associated with FCP or CRP. Exclusive enteral nutrition (EEN), a low-fibre product, is used effectively as primary therapy for CD in pediatric patients with luminal CD26. EEN may deplete the nutrients (e.g., fibre) necessary for bacterial growth, or create a luminal microenvironment where the functionality of inflammatory microbes is suppressed, inhibiting the gut mediated immune response in patients with CD27. Therefore, the mechanisms underlying the protective benefits of leafy greens may extend beyond their fiber content.
Higher n-6:n-3 PUFA ratios were associated with increased odds of patients having a CRP ≤ 5 mg/L. In typical Western diets this ratio can be as high as 20:128, and disproportionate n-6:n-3 intake ratios may lead toward a proinflammatory response which may affect the onset of IBD29. Supplementation with n-3 PUFA to alter the n6:n3 ratio towards anti-inflammatory effects has shown mixed results in CD and genetic polymorphisms in n-3 metabolism could be one possible mechanism to explain conflicting results29. A study in zebrafish compared various levels of n-6:n-3 ratios in fish consuming a standard diet of 12% total calories from lipids30. Similar to our study, this study identified an 8:1 ratio as optimal compared to a 5:1 and a 2:1 ratio to promote greater gains in lean body mass and less total body fat. In addition, zebrafish eating the n-6:n-3 PUFA 8:1 ratio diet had lower levels of CRP and amyloid, markers of inflammation identified on liver biopsies. The authors concluded the ratio of n6:n3 may influence the inflammatory response less than the total percent of calories consumed from lipids. In our study, total intake of fat grams did not have any significant association with FCP, CRP or inflammatory cytokines.
Having identified dietary associations with FCP and CRP, we proceeded to examine potential immune mediated mechanisms to explain these results. Both expected and unexpected relationships between peripheral cytokines and dietary components and patterns were identified.
Unexpectedly, increasing scores for the pMDS (more anti-inflammatory dietary pattern) were associated with increasing levels of IL-17A. Similarly, lower energy adjusted DII scores (more anti-inflammatory) were associated with increased IL12/23p40. In 320 healthy Iranian women, an inverse relationship with IL-17A and adherence to a Mediterranean diet was identified31 while another study demonstrated increasing consumption of fruit juices reduced IL-17A32. Although IL-17A has generally been classified as a pro-inflammatory cytokine, it may regulate components of the intestinal barrier by reinforcing tight junction proteins in epithelial cells, and it induces the expression of mucin-associated genes and the production of β-defensins in the colon33,34. IL-17A may have protective effects and its role in gut homeostasis may not be completely understood.
In previous work the DII score was associated with increased levels of TNF-α and IFN-γ and not associated with IL12/23p40 as seen in this study35; however, this was in healthy adolescents and not in a diseased cohort of patients. In another study in adults, the DII was positively associated with IL-6 and TNF-α36. The DII was not significantly associated to these cytokines in our study; however, our study collected data using 3-day food records compared to a food frequency questionnaire, did not control for the same confounders as the previous work, and the study populations were different.
We identified a significant relationship between IL-10 and β-carotene intake. IL-10 is an immunoregulatory cytokine that plays a crucial role in orchestrating intestinal immune homeostasis37. However, these data need to be interpreted with caution due to the relatively small sample size and the possible disconnect between serum cytokine levels and gut inflammation. β-carotene is widely distributed in green leafy, yellow and orange coloured vegetables and fruits, and is one of the most abundant carotenoids. β-carotene has been reported to suppress LPS-induced inflammatory responses by inhibiting nuclear factor kappa B expression, suggesting an anti-inflammatory role38.
We demonstrated an inverse relationship between red meat intake and IL-27 serum levels, and an inverse relationship between leafy green vegetables and IL-27. It has not been definitively determined whether IL-27 ameliorates or promotes intestinal inflammation, as contradictory roles for IL-27 have been reported in animal models of IBD. Studies have demonstrated the ability of IL-27 to lessen colonic inflammation by increasing the production of IL-10 in animal models of colitis39,40. These somewhat conflicting results may speak to the dual effects of IL-27 on intestinal inflammation, however mechanistic interpretations cannot be concluded at this time.
Study strengths include dietary data collection and FCP measurements at two time points using dietitian reviewed 3-day food records, and rigorous statistical modeling. Study limitations to the regression-based model analysis were related largely to sample size. We selected inclusion and exclusion criteria that would allow us to have a clinical population that was representative of the typical patient in remission without being too restrictive or broad. All patients presenting to the outpatient clinic were informed of the study and over the 2-year period we were able to achieve an initial n = 66. This sample size allowed us sufficient power to examine our question but certainly suggests that future larger studies are warranted to further confirm the interesting findings of our study.”As the number of variables and dietary factors observed were greater than the number of individuals, a risk factor analysis was underpowered to begin with. This small sample size made it impossible to assess interactions between predictor variables in the models, meaning that some key relationships between variables may not have been identified, as effect modification was not tested. As the purpose of this work was exploratory to provide preliminary associations for further investigation, reducing the number of significant associations detected by adjusting the significance level may result in potential relationships not being further investigated. In addition, while serum cytokine levels do not necessarily reflect mucosal inflammation, the identified relationships may add context and foundation for future dietary mechanistic studies. Raw P-values have been included in the results tables so they can be interpreted independently of a pre-defined significance cutoff.
In conclusion, we have identified relationships between dietary components and FCP and CRP in patients with CD in clinical remission, and provided preliminary associations between dietary components, patterns and nutrients with serum cytokines. The lack of robust associations between the DII and pMDS with FCP and CRP were unanticipated; however, the remitted patient population may limit these associations, and future studies building on this work should be undertaken in patients with greater disease activity.
References
Opstelten, J. L. et al. Dietary intake of patients with inflammatory bowel disease: a comparison with individuals from a general population and associations with relapse. Clin. Nutr. 38, 1892–1898. https://doi.org/10.1016/j.clnu.2018.06.983 (2019).
Ng, S. C. et al. Worldwide incidence and prevalence of inflammatory bowel disease in the 21st century: a systematic review of population-based studies. Lancet 390, 2769–2778. https://doi.org/10.1016/S0140-6736(17)32448-0 (2018).
Levine, A. et al. Dietary guidance from the international organization for the study of inflammatory bowel diseases. Clin. Gastroenterol. Hepatol. 18, 1381–1392. https://doi.org/10.1016/j.cgh.2020.01.046 (2020).
Ananthakrishnan, A. N. et al. A prospective study of long-term intake of dietary fiber and risk of Crohn’s disease and ulcerative colitis. Gastroenterology 145, 970–977. https://doi.org/10.1053/j.gastro.2013.07.050 (2013).
Nickerson, K. P., Chanin, R. & McDonald, C. Deregulation of intestinal anti-microbial defense by the dietary additive, maltodextrin. Gut Microbes 6, 78–83. https://doi.org/10.1080/19490976.2015.1005477 (2015).
Bhattacharyya, S. et al. A randomized trial of the effects of the no-carrageenan diet on ulcerative colitis disease activity. Nutr. Healthy Aging 4, 181–192. https://doi.org/10.3233/NHA-170023 (2017).
Levine, A. et al. Crohn’s disease exclusion diet plus partial enteral nutrition induces sustained remission in a randomized controlled trial. Gastroenterology 157, 440–450 (2019).
Taylor, L. et al. Cross-sectional analysis of overall dietary intake and mediterranean dietary pattern in patients with Crohn’s disease. Nutrients https://doi.org/10.3390/nu10111761 (2018).
Konijeti, G. G. et al. Efficacy of the autoimmune protocol diet for inflammatory bowel disease. Inflamm. Bowel Dis. 23, 2054–2060. https://doi.org/10.1097/MIB.0000000000001221 (2017).
Chiba, M. et al. Lifestyle-related disease in Crohn’s disease: relapse prevention by a semi-vegetarian diet. World J. Gastroenterol. 16, 2484–2495 (2010).
Suskind, D. L. et al. Clinical and fecal microbial changes with diet therapy in active inflammatory bowel disease. J. Clin. Gastroenterol. 52, 155–163. https://doi.org/10.1097/MCG.0000000000000772 (2018).
Shivappa, N., Hebert, J. R., Rashvand, S., Rashidkhani, B. & Hekmatdoost, A. Inflammatory potential of diet and risk of ulcerative colitis in a case-control study from Iran. Nutr. Cancer 68, 404–409. https://doi.org/10.1080/01635581.2016.1152385 (2016).
D’Haens, G. et al. Fecal calprotectin is a surrogate marker for endoscopic lesions in inflammatory bowel disease. Inflamm. Bowel Dis. 18, 2218–2224. https://doi.org/10.1002/ibd.22917 (2012).
Kiss, L. S. et al. High-sensitivity C-reactive protein for identification of disease phenotype, active disease, and clinical relapses in Crohn’s disease: a marker for patient classification?. Inflamm. Bowel Dis. 18, 1647–1654. https://doi.org/10.1002/ibd.21933 (2012).
Martinez-Gonzalez, M. A. et al. A 14-item Mediterranean diet assessment tool and obesity indexes among high-risk subjects: the PREDIMED trial. PLoS ONE 7, e43134. https://doi.org/10.1371/journal.pone.0043134 (2012).
Shivappa, N., Steck, S. E., Hurley, T. G., Hussey, J. R. & Hebert, J. R. Designing and developing a literature-derived, population-based dietary inflammatory index. Public Health Nutr. 17, 1689–1696. https://doi.org/10.1017/S1368980013002115 (2014).
Canada, H. Eating Well with Canada’s Food Guide (Health Canada, Ottawa, 2011).
R Core team: A language and environment for statistical computing (R Foundation for Statistical Computing, Vienna, Austria, 2019). https://www.R-project.org/. Accessed 25 March 2020.
Mumolo, M. G. et al. From bench to bedside: fecal calprotectin in inflammatory bowel diseases clinical setting. World J. Gastroenterol. 24, 3681–3694. https://doi.org/10.3748/wjg.v24.i33.3681 (2018).
Vermeire, S., Van Assche, G. & Rutgeerts, P. C-reactive protein as a marker for inflammatory bowel disease. Inflamm. Bowel Dis. 10, 661–665. https://doi.org/10.1097/00054725-200409000-00026 (2004).
Bates, D., Mächler, M., Bolker, B. & Walker, S. Fitting linear mixed-effects models using lme4. J. Stat. Softw. 67, 48. https://doi.org/10.18637/jss.v067.i01 (2015).
Racine, A. et al. Dietary patterns and risk of inflammatory bowel disease in Europe: results from the EPIC study. Inflamm. Bowel Dis. 22, 345–354. https://doi.org/10.1097/MIB.0000000000000638 (2016).
Papada, E., Amerikanou, C., Forbes, A. & Kaliora, A. C. Adherence to Mediterranean diet in Crohn’s disease. Eur. J. Nutr. https://doi.org/10.1007/s00394-019-01972-z (2019).
He, C. et al. Vitamin A inhibits the action of LPS on the intestinal epithelial barrier function and tight junction proteins. Food Funct 10, 1235–1242. https://doi.org/10.1039/c8fo01123k (2019).
Eom, T., Kim, Y. S., Choi, C. H., Sadowsky, M. J. & Unno, T. Current understanding of microbiota- and dietary-therapies for treating inflammatory bowel disease. J. Microbiol. 56, 189–198. https://doi.org/10.1007/s12275-018-8049-8 (2018).
Ruemmele, F. M. et al. Consensus guidelines of ECCO/ESPGHAN on the medical management of pediatric Crohn’s disease. J. Crohns Colitis 8, 1179–1207. https://doi.org/10.1016/j.crohns.2014.04.005 (2014).
Svolos, V. et al. Treatment of active Crohn’s disease with an ordinary food-based diet that replicates exclusive enteral nutrition. Gastroenterology 156, 1354–1367 (2019).
Simopoulos, A. P. The importance of the ratio of omega-6/omega-3 essential fatty acids. Biomed. Pharmacother. 56, 365–379. https://doi.org/10.1016/s0753-3322(02)00253-6 (2002).
Scaioli, E., Liverani, E. & Belluzzi, A. The imbalance between n-6/n-3 polyunsaturated fatty acids and inflammatory bowel disease: a comprehensive review and future therapeutic perspectives. Int J Mol Sci 18, E2619. https://doi.org/10.3390/ijms18122619 (2017).
Powell, M. L. et al. Effects of the dietary ω3:ω6 fatty acid ratio on body fat and inflammation in Zebrafish (Danio rerio). Comp. Med. 65, 289–294 (2015).
Sakhaei, R. et al. The dietary approaches to stop hypertension (DASH)-style diet and an alternative Mediterranean diet are differently associated with serum inflammatory markers in female adults. Food Nutr. Bull. 39, 361–376. https://doi.org/10.1177/0379572118783950 (2018).
Peluso, I. et al. High fat meal increase of IL-17 is prevented by ingestion of fruit juice drink in healthy overweight subjects. Curr. Pharm. Des. 18, 85–90 (2012).
Lee, J. S. et al. Interleukin-23-independent IL-17 production regulates intestinal epithelial permeability. Immunity 43, 727–738. https://doi.org/10.1016/j.immuni.2015.09.003 (2015).
Hueber, W. et al. Secukinumab, a human anti-IL-17A monoclonal antibody, for moderate to severe Crohn’s disease: unexpected results of a randomised, double-blind placebo-controlled trial. Gut 61, 1693–1700. https://doi.org/10.1136/gutjnl-2011-301668 (2012).
Shivappa, N. et al. Association between dietary inflammatory index and inflammatory markers in the HELENA study. Mol. Nutr. Food Res. https://doi.org/10.1002/mnfr.201600707 (2017).
Shivappa, N. et al. Associations between dietary inflammatory index and inflammatory markers in the Asklepios Study. Br. J. Nutr. 113, 665–671. https://doi.org/10.1017/S000711451400395X (2015).
Kuhn, R., Lohler, J., Rennick, D., Rajewsky, K. & Muller, W. Interleukin-10-deficient mice develop chronic enterocolitis. Cell 75, 263–274 (1993).
Bai, S. K. et al. Beta-carotene inhibits inflammatory gene expression in lipopolysaccharide-stimulated macrophages by suppressing redox-based NF-kappaB activation. Exp. Mol. Med. 37, 323–334 (2005).
Dann, S. M. et al. Attenuation of intestinal inflammation in interleukin-10-deficient mice infected with Citrobacter rodentium. Infect. Immun. 82, 1949–1958. https://doi.org/10.1128/IAI.00066-14 (2014).
Hanson, M. L. et al. Oral delivery of IL-27 recombinant bacteria attenuates immune colitis in mice. Gastroenterology 146, 210–221. https://doi.org/10.1053/j.gastro.2013.09.060 (2014).
Acknowledgements
This study grant was supported by Litwin IBD Pioneers Crohn’s & Colitis Foundation and Alberta’s Collaboration of Excellence for Nutrition in Digestive Diseases (Ascend).
Author information
Authors and Affiliations
Contributions
Study concept and design: M.R., H.B, S.G., K.M., R.R, Acquisition of data: S.N., L.T., N.S., N.H., S.K. Bioinformatics and statistical analysis: S.N. H.B. Analysis and interpretation of data: L.T., M.R., S.G. Drafting of the manuscript: S.N., L.T., M.R. Critical revision of the manuscript for important intellectual content: M.R., H.B, S.G., K.M., R.R, S.N., L.T., N.S., N.H., S.K.,R.P. Technical and material support: L.T., N.S., S.K. Obtained funding: M.R. Supervision: M.R. No additional writing assistance was used for this manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Naqvi, S.A., Taylor, L.M., Panaccione, R. et al. Dietary patterns, food groups and nutrients in Crohn’s disease: associations with gut and systemic inflammation. Sci Rep 11, 1674 (2021). https://doi.org/10.1038/s41598-020-80924-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-80924-8
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.