Abstract
Amino acid (AA) concentrations are influenced by both exogenous (e.g. diet, lifestyle) and endogenous factors (e.g. genetic, transcriptomic, epigenetic, and metabolomic). Fasting plasma AA profiles in adulthood are predictive of diabetes risk over periods of up to 12 years. Data on AA profiles in cross-generational cohorts, including individuals from shared gene-environment settings are scarce, but would allow the identification of the contribution of heritable and environmental factors characterising the levels of circulating AAs. This study aimed to investigate parent–child (familial dyad) concordance, absolute differences between generations- (children versus adults), age- (in adults: 28–71 years), and sex-dependent differences in plasma AA concentrations. Plasma AA concentrations were measured by UHPLC/MS–MS in 1166 children [mean (SD) age 11 (0.5) years, 51% female] and 1324 of their parents [44 (5.1) years, 87% female]. AA concentrations were variably concordant between parents and their children (5–41% of variability explained). Most AA concentrations were higher in adults than children, except for the non-essential AAs arginine, aspartic acid, glutamine, hydroxy-proline, proline, and serine. Male adults and children typically had higher AA concentrations than females. The exceptions were alanine, glutamine, glycine, hydroxy-proline, serine, and threonine in girls; and glycine and serine in women. Age, sex, and shared familial factors are important determinants of plasma AA concentrations.
Similar content being viewed by others
Introduction
Plasma amino acid (AA) concentrations are maintained under tight homeostatic control. Yet, changes in AA concentrations have been described in metabolic diseases1,2, asthma3, autism4, sepsis5, and malnutrition6. Moreover, fasting AA concentrations in middle-aged adults have been reported to predict diabetes onset 12 years later in the Framingham Offspring cohort1. Despite their clear role in health and disease, studies analyzing AA profiles in a shared family setting are scarce and those that exist are typically small in scale (e.g. 200 related individuals7), or only quantitate a limited selection of AAs8. Characterizing the epidemiology of plasma AAs and their familial concordance is of utmost importance given that AA profiles may predict disease1, and reflect both dietary and endogenous factors (i.e. genetic, transcriptomic, epigenetic and metabolic)9,10.
We previously identified strong familial concordance, sex and inter-generational differences, in the plasma concentrations of nutritional metabolites (e.g. Trimethylamine N-oxide (TMAO) and its precursors) in children and adults8. These data implicated gene-environment interactions in the setting and/or maintenance of metabolite concentrations. It may be possible to discern the relative gene/environment contributions to AA concentrations using the fact that some are solely diet-derived (essential), while others can also be synthesized de novo (non-essential)9.
In this study, we characterized AA concentrations in 1,166 children (51% females), and 1324 adults (87% females) from the CheckPoint study of Australian children and adults. We analyzed: (a) parent–child (familial dyad) concordance; (b) absolute differences between generations (adults versus children); (c) age as a continuous variable in the adult group (Mean (SD)) age: 44 (5) years; range 28–71 years in the adult subgroup); and (d) sex-specific effects on individual AA concentrations.
Methods
Ethical approval, consent, and sample collection
The study was approved by The Royal Children’s Hospital (Melbourne, Australia) Human Research Ethics Committee (33225D) and the Australian Institute of Family Studies Ethics Committee and was conducted in accordance with The Declaration of Helsinki. 1874 parent–child dyads participated in a biomedical assessment: The Child Health CheckPoint (CheckPoint), nested between waves 6 and 7 of the Longitudinal Study of Australian Children’s B cohort (LSAC)11. Parents or caregivers provided informed consent for themselves and their child to participate in the study and for the collection of their blood samples12 (Supplementary Fig. 1).
Procedures and UHPLC/MS–MS analysis
Adults and children were semi-fasted. Mean (SD) fasting time was 4.4 (2.1) hours in children, and 3.4 (2.4) h in adults. Venous blood was collected from children and adults in EDTA tubes from single venepuncture split to components including 6 plasma aliquots (used for UHPLC/MS–MS analysis) processed within ~ 1 h (1 min to 3.8 h) prior to storage at − 80 °C12. A total of 2490 EDTA plasma samples were shipped on dry ice in thermally monitored boxes. Samples were then randomised as received from Melbourne on dry ice onto 34 different 96-well FluidX plates (Phenomenex), keeping parent–child pairs (1121 pairs) together on the same plate, and stored at – 80 °C prior to UHPLC/MS–MS analysis.
All AAs were measured using a Vanquish UHPLC + system, coupled with a TSQ Quantiva triple quadrupole mass spectrometer (Thermo Scientific) using a heated electrospray ionisation source (H-ESI) in positive ionization mode. Sample preparation was automated on an Eppendorf robot fitted with a thermal mixer and a vacuum manifold (EpMotion 5075vt, Germany). The UHPLC/MS–MS analysis and robotic automation has been described in detail elsewhere13. Briefly, protein precipitation was conducted by adding 300 µL of 1% formic acid in LC-Grade MeOH to 100 µL of either: (a) calibration curve standards, (b) plasma samples, (b) MilliQ H2O blanks, or (c) stripped plasma quadruplicate quality controls (QCs), at 3 different locations; all in a 96-well IMPACT protein precipitation plate (Phenomenex). 20 µL of an internal standard solution was added to all wells, the plate was capped, mixed (5 min, 800 rpm, room temperature), and the filtrate obtained by vacuum (450 mbar, 10 min). Tris (2-carboxyethyl) phosphine (100 µL, TCEP) was added for disulphide bond reduction. The reduced filtrate was agitated (15 min, 800 rpm, room temperature), and diluted with 200 µL of 1% ascorbic acid in MilliQ H2O. A Kinetex EVO C18 100 Å 150 × 2.1 mm 1.7 µm column (Phenomenex) at 40 °C, coupled with a Krudkatcher (Phenomenex) pre-column filter, was used to chromatographically separate the compounds. A flow of 400 µL/min starting at 2% acetonitrile and 98% mobile phase consisting of 5 mM perfluorohexanoic acid (PFHA) in MilliQ H2O was applied to the column, compounds of interest were eluted using an increasing acetonitrile gradient. The sample injection volume was 7 µL, and the run time was 15.5 min. All quality controls passed the acceptable cut-off for compound recovery and reproducibility, and QC results have been reported in detail elsewhere13.
Statistical analysis
All statistical analyses were performed in R programming environment version 3.6.114. Technical plate effects were removed from all metabolites using the RANEF function (lme4 package in R)15. The reported AAs included essential AAs (i.e. valine, leucine, isoleucine, methionine, threonine, phenylalanine, and tryptophan), non-essential AAs (i.e. alanine, glycine, cysteine, serine, tyrosine, proline, histidine, arginine, asparagine, aspartic acid, glutamic acid, glutamine, taurine and citrulline), AA precursors (i.e. aminoadipic acid), and derivatives: methylated histidine (i.e. 1 and 3-methylhistidine), hydroxylated proline (i.e. OH-Proline), and adenylated methionine (i.e. S-Adenosylmethionine). Chromatographic issues occurred with lysine, cystathionine, and ornithine. Additionally, plasma concentrations of ethanolamine, homocysteine, and S-adenosylhomocysteine (SAH) were below the lowest limit of quantitation (LOQ) for most of our plates. These AAs were therefore excluded from our study.
Histograms of all plate-adjusted variables were plotted to assess normality.
3-Methylhistidine, aspartic acid, isoleucine, methionine, OH-proline, proline, and taurine were positively skewed and therefore log-transformed. The remaining AAs were normally distributed.
Two sets of mixed models were developed to test the effect of (a) family (shared gene-environment setting), and (b) generation (adults versus children) using the lme4 package in R after adjusting for plate effects15. Log likelihoods were compared between models that contained both family (as a random effect) and generation (as a fixed effect), and those excluding one or the other. Pearson’s correlations adjusted for multiple testing using the Holm method in R were also conducted within parent–child dyads to confirm familial concordance. Family effect sizes were calculated as the ratio of the estimated family variance component divided by the total variance of each plate-adjusted variable.
Two sets of linear models for (a) sex, and (b) age (in the adult subgroup of 28–71 years) were also fitted for each plate-adjusted/log-transformed variable in children and adults separately. Given the narrow age distribution in children (11–12 years), we only characterized age-specific differences within the adults (28–71 years on a continuous scale).
Results
Sample characteristics and amino acid measurement
The CheckPoint cohort consisted of 2490 participants (1121 parent–child pairs); 1166 children (51% females), and 1324 adults (87% females, predominantly the children’s biological mothers) (Table 1).
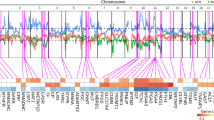
Amino acid profiles are concordant between parents and children
All AA concentrations exhibited a concordance between children and parents from the same family (Table 2, Fig. 1, and Supplementary Figs. 2, 3, and 4). Both likelihood ratio tests and Pearson’s correlations between dyads showed the strongest familial effect to be for 3-methylhistidine (coefficient of correlation R = 0.34; confidence interval [0.29, 0.39]), and isoleucine (R = 0.34; [0.29, 0.39]), and the weakest for glutamine (R = 0.06; [0, 0.12]) and aminoadipic acid (R = 0.09 [0.03, 0.15]). In total, familial effects accounted for approximately 5% of variability in the dataset for glutamine and aminoadipic acid, 34% for isoleucine, and 41% for 3-methylhistidine (Supplementary Figs. 2, 3, and 4).
AA profiles are age-dependent
Most AA concentrations exhibited differences between adults and children (p < 0.05), except for histidine, glutamic acid, isoleucine, tryptophan, tyrosine, and taurine (Table 3). Most AA concentrations were higher in adults, except for non-essential AAs and their derivatives: arginine (Mean (SD): 64.9 (19.1) µM in adults; 67.3 (17.1) µM in children), aspartic acid (3.8 (3.0) µM in adults; 4.43 (2.8) µM in children), glutamine (805.0 (125.0) µM in adults; 826.0 (114.0) µM in children), OH-proline (7.7 (2.2) µM in adults; 17.4 (1.5) µM in children), proline (192.0 (1.4) µM in adults; 197.0 (1.4) µM in children), and serine (90.4 (23.9) µM in adults; 97.8 (20.9) µM in children).
Concentrations of 1-methylhistidine (adjusted R2 of the linear model = 0.01; p = 0.003), citrulline (R2 = 0.03; p < 0.0001), glutamic acid (R2 = 0.005; p < 0.01), glutamine (R2 = 0.01; p < 0.001), phenylalanine (R2 = 0.004; p = 0.01), S-adenosylmethionine (R2 = 0.02; p < 0.0001), and tyrosine (R2 = 0.01; p < 0.001) were all weakly positively associated with increasing age in the adult subgroup. By contrast, threonine concentrations (R2 = 0.002; p = 0.05) exhibited a weak negative association with adult age (Supplementary Table 1).
Amino acid profiles are sex-dependent
Males had significantly higher concentrations for most plasma AAs in both adults and children (p < 0.05) (Table 4). Exceptions, where concentrations were higher in female children, were evident for the essential AA threonine [106.0 (25.2) µM in female children; 97.1 (23.4) µM in male children], and non-essential AAs alanine [307.0 (77.7) µM in female children; 296.0 (79.3) in male children], glutamine [839.0 (105.0) µM in female children ; 812.0 (121.0) µM in male children], glycine [189.0 (42.3) µM in female children; 176.0 (40.2) µM in male children], and serine [99.8 (21.3) µM in female children ; 95.7 (20.3) µM in male children]. Similarly, the AA derivative OH-proline was present at higher concentrations in female [18.1 (1.4) µM] than male children [16.7 (1.6) µM]. Adult females also exhibited higher plasma concentrations for non-essential AAs glycine [195.0 (72.8) µM in female adults; 165.0 (42.7) µM in male adults] and serine [91.5 (24.3) µM in female adults; 83.2 (18.8) µM in male adults].
In children, methionine, tyrosine, proline, histidine, arginine, aspartic acid, glutamic acid, taurine, 1-methylhistidine, and S-adenosylmethionine plasma concentrations were not significantly different between males and females (Table 4). In adults, threonine, histidine, aspartic acid, and taurine plasma concentrations were not significantly different between males and females (Table 4).
Discussion
Our study identifies family, sex, and age as important factors that characterise plasma AA concentrations. Both essential and non-essential AAs exhibited familial concordance in our study. The familial concordance of both essential and non-essential AAs supports a gene-environment contribution to AA profiles.
It has previously been demonstrated that non-essential AA concentrations exhibit a stronger concordance within an individual over time compared to essential AAs, which was proposed to be due to endogenous contributors to these profiles (i.e. genes and gene expression) being more stable than dietary intakes16,17. In our study, a mix of essential and non-essential amino acids exhibited the highest family effects. AAs exhibiting the highest family effects (> 20% of variability explained) were 3-methylhistidine (41%), aspartic acid (35%), isoleucine (34%), proline (33%), phenylalanine (31%), methionine (27%), taurine (25%), leucine (24%) valine (24%), and tyrosine (22%). Two important AA families are represented within this list: branched chain AAs (i.e. valine, leucine, and isoleucine), and aromatic AAs (i.e. phenylalanine, and tyrosine)9. This is interesting as a single overnight fasting plasma measurement of these 5 AAs (out of a total of 61 metabolites) predicted the development of type 2 diabetes up to 12 years later, and significantly improved the fit of predictive models that included traditional risk factors1. Other studies support the relationship between these AAs and adverse metabolic outcomes2,18,19. Identifying family effects for biomarkers of disease risk raises the possibility of characterising early metabolic targets, particularly within high risk families20,21.
Plasma AA concentrations vary with age; essential AAs were all lower in children compared to adults, and only non-essential plasma AA concentrations were higher in children. This profile of AAs in children may reflect an increased turnover of non-essential AAs and/or higher uptakes of essential AAs into peripheral tissues during anabolic growth phases in childhood, as previously postulated22. In the adult subgroup (28–71 years), the concentrations of 1-methylhistidine, citrulline, glutamic acid, glutamine, phenylalanine, and tyrosine were all weakly positively associated with increased age. Only threonine was weakly negatively associated with age. The weak association between these AAs and age may partly be explained by a non-homogenous distribution of adults in the 28–71 years age range. Age-specific differences in AA plasma concentrations may reflect an age-specific hormonal (e.g. insulin) regulation of AA uptake into peripheral tissues (e.g. muscles), where these AAs are utilised23. Decreased insulin sensitivity and lower lean body mass are characteristic of aging24,25, and the ratio of AA clearance in response to insulin has been demonstrated to be higher in younger compared to older adults24. Age is an important contributor characterising AA profiles in paediatric and adult populations26,27, and should be accounted for when interpreting AA concentrations.
We observed sex dependent changes in AA profiles, in agreement with published studies7,22. Sex specificity was more pronounced in adults than children with most AAs being higher in males, consistent with previous observations28,29. This may be explained by hormonal changes in early puberty (11–12 years) versus post-menarche/menopause (adulthood), affecting the concentrations of AAs. Moreover, there may be some age-dependent ‘maturation’ of physiological mechanisms involved in AA metabolism and regulation16. Factors underlying the age-specificity of AA profiles (i.e. insulin concentrations and lean body mass) are also sex-specific24,25,30,31,32. Females (a) have lower lean body mass compared with males25,30; and (b) exhibit higher glucose-mediated insulin sensitivity24, as well as (c) higher insulin secretion in response to the same blood glucose level as males31. Higher circulating insulin concentrations coupled with higher insulin sensitivity may further explain lower circulating AA concentrations in females, mediated by increased AA tissue uptake.
Limitations
This was a large population based cross-sectional study in which plasma samples were only collected at a single timepoint. Extrapolations need to be drawn from our results carefully given that (a) our adults were mostly parents; (b) the sex distribution in the adult subgroup was unbalanced: A 1:10 male to female ratio in our cohort versus a ratio of 1:1 in the wider Australian population33; and that (c) the CheckPoint cohort comprised of socio-economically advantaged Australians: when averaging the top 3 SEIFA scores across Australian states, over 78% of our cohort scored in the middle to most advantaged socio-economic indexes for areas (SEIFA) compared to only 62% of the general Australian population34. Our study was also limited because we did not collect post-prandial samples, and all participants were semi-fasted (~ 4 h fast) at the time of blood collection. However, given that this was a systematic limitation across the entire population, and that fasting time was typically short and had a narrow distribution (children (4.4 ± 2.1 h [Mean ± SD]; Quartiles [Q1, Median; Q3] [3.38 h; 4.08 h; 4.85 h]) and adults (3.4 ± 2.4 [Mean ± SD]; Quartiles [2.19; 2.97; 3.94]), comparisons of relative amino acid concentrations would not have been largely impacted by baseline fasting status. Comparing AA concentrations across fasted and post-prandial states may have clarified the relative contribution of exogenous versus endogenous factors to AA profiles. Moreover, accounting for physical activity status/body composition, as well as anabolic and catabolic hormone concentrations by sex, age, and family relatedness could have further strengthened some of our conclusions. Finally, measures of insulin concentrations and/or sensitivity were not collected from our participants, although these may have informed on the underlying mechanisms of the sex and age specificity of AA concentrations.
Conclusion
In this study, we identified a moderate concordance between children and parents from the same family for essential (diet-derived), and non-essential (diet derived and endogenously produced) AAs, as well as AA derivatives. This highlights a likely gene-environment behavioral contribution to circulating AA concentrations. The strongest familial concordance was evident for branched chain and aromatic AAs, which have been previously reported as strong predictors of diabetes mellitus, and have been also shown to be markedly associated with adverse metabolic outcomes1,2. We also identified age and sex-specific differences in AA profiles, that we suggest are partly attributable to age and sex-specific differences in lean body mass and insulin secretion/sensitivity.
Data availability
Data described in the article will be made available upon request after application and approval by our teams.
Abbreviations
- AA:
-
Amino acid
- BSA:
-
Bovine serum albumin
- EDTA:
-
Ethylenediaminetetraacetic acid
- LOQ:
-
Limit of quantitation
- MeOH:
-
Methanol
- MS–MS:
-
Tandem mass spectrometry
- OH-Proline:
-
Hydroxyproline
- PBS:
-
Phosphate-buffered saline
- SAH:
-
S-Adenosylhomocysteine
- SAM:
-
S-Adenosylmethionine
- TCEP:
-
Tris(2-carboxyethyl)phosphine
- UHPLC:
-
Ultra-high-performance liquid chromatography
- QC:
-
Quality control
References
Wang, T. J. et al. Metabolite profiles and the risk of developing diabetes. Nat. Med. 17, 448–453 (2011).
Yamaguchi, N. et al. Plasma free amino acid profiles evaluate risk of metabolic syndrome, diabetes, dyslipidemia, and hypertension in a large Asian population. Environ. Health Prev. Med. 22, 35 (2017).
Inselman, L. S., Khan, F. & Evans, H. E. Alterations in plasma amino acid levels in children with asthma: A preliminary investigation. Pediatr. Pulmonol. 2, 163–169 (1986).
Liu, A. et al. Altered urinary amino acids in children with autism spectrum disorders. Front. Cell. Neurosci. 13, 7 (2019).
Maldonado, J. et al. Specific serum amino-acid profiles of trauma and septic children. Clin. Nutr. 7, 165–170 (1988).
Ortega, P. A., van Gelder, N. M., Castejón, H. V., Gil, N. M. & Urrieta, J. R. Imbalance of individual plasma amino acids relative to valine and taurine as potential markers of childhood malnutrition. Nutr. Neurosci. 2, 163–173 (1999).
Armstrong, M. D. & Stave, U. A study of plasma free amino acid levels. II. Normal values for children and adults. Metabolism. 22, 561–569 (1973).
Ellul, S. et al. Metabolomics: Population epidemiology and concordance in Australian children aged 11–12 years and their parents. BMJ Open 9, 106–117 (2019).
Mahan, L. K., Escott-Stump, S., Raymond, J. L. & Krause, M. V. Krause’s Food and the Nutrition Care Process. (Elsevier/Saunders, Amsterdam, 2012).
Shin, S.-Y. et al. An atlas of genetic influences on human blood metabolites. Nat. Genet. 46, 543–550 (2014).
Edwards, B. Family Matters—Issue 95—Growing Up in Australia: The Longitudinal Study of Australian Children | Australian Institute of Family Studies. (2014).
Clifford, S. A., Davies, S., Wake, M. & Child Health CheckPoint Team. Child Health CheckPoint: Cohort summary and methodology of a physical health and biospecimen module for the Longitudinal Study of Australian Children. BMJ Open 9, 3–22 (2019).
Andraos, S. et al. Robotic automation of a UHPLC/MS-MS method profiling one-carbon metabolites, amino acids, and precursors in plasma. Anal. Biochem. 592, 113558 (2020).
R Core Team. R: The R Project for Statistical Computing. R Foundation for Statistical Computing, Vienna Austria.
Bates, D., Mächler, M., Bolker, B. & Walker, S. Fitting linear mixed-effects models using lme4. J. Stat. Softw. 67, 1–48 (2015).
Scriver, C. R., Gregory, D. M., Sovetts, D. & Tissenbaum, G. Normal plasma free amino acid values in adults: The influence of some common physiological variables. Metabolism https://doi.org/10.1016/0026-0495(85)90112-X (1985).
Armstrong, M. D. & Stave, U. A study of plasma free amino acid levels. IV. Characteristic individual levels of the amino acids. Metabolism https://doi.org/10.1016/0026-0495(73)90053-X (1973).
Okekunle, A. P. et al. Abnormal circulating amino acid profiles in multiple metabolic disorders. Diabetes Res. Clin. Pract. 132, 45–58 (2017).
Takashina, C. et al. Associations among the plasma amino acid profile, obesity, and glucose metabolism in Japanese adults with normal glucose tolerance. Nutr. Metab (Lond.). 13, 5 (2016).
Zheng, Y. et al. Weight-loss diets and 2-y changes in circulating amino acids in 2 randomized intervention trials. Am. J. Clin. Nutr. 103, 505–511 (2016).
Geidenstam, N. et al. Amino acid signatures to evaluate the beneficial effects of weight loss. Int. J. Endocrinol. 2017, 1–12 (2017).
Gregory, D. M., Sovetts, D., Clow, C. L. & Scriver, C. R. Plasma free amino acid values in normal children and adolescents. Metabolism. 35, 967–969 (1986).
Blomstrand, E. et al. Branched-chain amino acid ingestion stimulates muscle myofibrillar protein synthesis following resistance exercise in humans. Front. Physiol. 8, 390 (2017).
Marchesini, G. et al. Insulin resistance in aged man: Relationship between impaired glucose tolerance and decreased insulin activity on branched-chain amino acids. Metabolism 36, 1096–1100 (1987).
St-Onge, M.-P. & Gallagher, D. Body composition changes with aging: The cause or the result of alterations in metabolic rate and macronutrient oxidation?. Nutrition 26, 152–155 (2010).
Chih-Kuang, C., Shuan-Pei, L., Shyue-Jye, L. & Tuan-Jen, W. Plasma free amino acids in Taiwan Chinese: The effect of age. Clin. Chem. Lab. Med. 40, 378–382 (2002).
Uaariyapanichkul, J. et al. Age-related reference intervals for blood amino acids in Thai pediatric population measured by liquid chromatography tandem mass spectrometry. J. Nutr. Metab. 2018, 1–10 (2018).
Yamamoto, H. et al. Reference intervals for plasma-free amino acid in a Japanese population. Ann. Clin. Biochem. 53, 357–364 (2016).
Hassan, D. A. et al. Normal levels of plasma amino acids among sudanese adults: The effect of gender. J. Med. Sci. 11, 246–249 (2011).
Bredella, M. A. Sex differences in body composition. Adv. Exp. Med. Biol. 1043, 9–27 (2017).
Hale, P. J., Wright, J. V. & Nattrass, M. Differences in insulin sensitivity between normal men and women. Metabolism https://doi.org/10.1016/0026-0495(85)90159-3 (1985).
Felig, P., Marliss, E. & Cahill, G. F. Plasma amino acid levels and insulin secretion in obesity. N. Engl. J. Med. 281, 811–816 (1969).
Australian Bureau of Statistics. Population. https://www.abs.gov.au/population (2019).
Australian Bureau of Statistics. Census of Population and Housing: Socio-Economic Indexes for Areas (SEIFA), Australia, 2016. https://www.abs.gov.au/ (2018).
Acknowledgements
This paper uses unit record data from Growing Up in Australia, the Longitudinal Study of Australian Children. The study is conducted in partnership between the Department of Social Services (DSS), the Australian Institute of Family Studies (AIFS) and the Australian Bureau of Statistics (ABS). The findings and views reported in this paper are those of the authors and should not be attributed to DSS, AIFS or the ABS.
Funding
This study was funded by a MBIE Catalyst grant (The New Zealand-Australia Life Course Collaboration on Genes, Environment, Nutrition and Obesity (GENO); UOAX1611; to JOS, MW, RS, and DB). The Checkpoint study was supported by the National Health and Medical Research Council (NHMRC) of Australia (Project Grants 1041352, 1109355), The Royal Children’s Hospital Foundation (2014-241), the Murdoch Children’s Research Institute, The University of Melbourne, the National Heart Foundation of Australia (100660), Financial Markets Foundation for Children (2014-055, 2016-310) and the Victorian Deaf Education Institute. Research at the Murdoch Children’s Research Institute is supported by the Victorian Government’s Operational Infrastructure Support Program. The funding bodies did not play any role in the study. SA is the recipient of a New Zealand International Doctoral Research Scholarship 2017. The following authors were supported by NHMRC Research Fellowships: MW (1046518, 1160906) and DPB (1064629) as well as an Investigator Grant to DPB (GTN1175744). The following author was supported by the National Heart Foundation of Australia: Honorary Future Leader Fellowship to DPB (100369). MW was supported by Cure Kids New Zealand.
Author information
Authors and Affiliations
Contributions
M.W., R.S. and D.P.B. designed the CheckPoint study, and M.W. and J.M.O. designed and obtained the funding for the sub-study of micronutrients. S.A. conducted the laboratory work, performed all statistical analyses, and wrote the paper. K.L. and S.A.C. provided data support. B.J. provided statistical support. E.B.T. assisted with laboratory analyses. K.L., S.A.C., B.J., E.B.T., M.W., R.S., D.P.B., and J.M.O. discussed, and edited the manuscript. M.W., R.S., D.P.B., and J.M.O. supervised S.A. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Andraos, S., Lange, K., Clifford, S.A. et al. Population epidemiology and concordance for plasma amino acids and precursors in 11–12-year-old children and their parents. Sci Rep 11, 3619 (2021). https://doi.org/10.1038/s41598-020-80923-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-80923-9
This article is cited by
-
New perspectives on ‘Breathomics’: metabolomic profiling of non-volatile organic compounds in exhaled breath using DI-FT-ICR-MS
Communications Biology (2024)
-
Sex differences in the human metabolome
Biology of Sex Differences (2022)
-
Chiral resolution of plasma amino acids reveals enantiomer-selective associations with organ functions
Amino Acids (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.