Abstract
The maximum value of the first derivative of the invasively measured left ventricular (LV) pressure (+ dP/dtmax or P′) is often used to quantify LV contractility, which in mice is limited to a single terminal study. Thus, determination of P′ in mouse longitudinal/serial studies requires a group of mice at each desired time point resulting in “pseudo” serial measurements. Alternatively, a noninvasive surrogate for P′ will allow for repeated measurements on the same group of mice, thereby minimizing physiological variability and requiring fewer animals. In this study we evaluated aortic acceleration and other parameters of aortic flow velocity as noninvasive indices of LV contractility in mice. We simultaneously measured LV pressure invasively with an intravascular pressure catheter and aortic flow velocity noninvasively with a pulsed Doppler probe in mice, at baseline and after the administration of the positive inotrope, dobutamine. Regression analysis of P′ versus peak aortic velocity (vp), peak velocity squared/rise time (vp2/T), peak (+ dvp/dt or v′p) and mean (+ dvm/dt or v′m) aortic acceleration showed a high degree of association (P′ versus: vp, r2 = 0.77; vp2/T, r2 = 0.86; v′p, r2 = 0.80; and v′m, r2 = 0.89). The results suggest that mean or peak aortic acceleration or the other parameters may be used as a noninvasive index of LV contractility.
Similar content being viewed by others
Introduction
The maximum value of the first derivative of left ventricular (LV) pressure (+ dP/dtmax or P′) is often used to quantify ventricular contractility. It is derived from the high-fidelity pressure signal measured invasively, using an intravascular pressure catheter. The invasive technique is frequently used in patients1,2 and in large animal research3,4. While complications are infrequent, repeated invasive pressure measurements are avoided in patients5. Repeated measurements of invasive pressure can be utilized in large animal research, but the invasive nature of this measurement has motivated investigators5,6,7,8,9,10,11,12 to develop noninvasive methods to measure ventricular contractility.
The shift in research from large to small animals such as mice and rats has compelled investigators to adapt techniques and methods designed for large animals for use in small animals13. While the measurement of ventricular pressure in mice was first reported in the 1930s14, its utility to measure contractility in mice began in the 1990s15 and many studies in small animals ensued thereafter16,17,18,19,20,21,22,23,24. However, invasive pressure measurement is problematic in rodents and other small animals as it is limited to a single or a few acute measurements and the study is terminal. The ability to measure LV contractility noninvasively allows researchers to pursue longitudinal studies using fewer animals.
Many indices of cardiac contractility have been developed in humans and large animals in the last several decades, which have been summarized in the report by Lambert et al.25 based on theoretical (references 9–17 of25), empirical (references 1–5 of25), and borrowed concepts (references 6–8 of25). The sensitivity of 24 of these (invasively & noninvasively derived) indices has been evaluated and ranked by Lambert et al.25 through their cardiac contractility study in dogs in the order from the most sensitive to the least sensitive. The first 7 most sensitive indices in their ranking require the invasively measured pressure signal. The next most sensitive indices of their ranking were the noninvasively measured mean and peak aortic accelerations, followed by the invasively measured first derivative of pressure (dP/dt). Therefore, we undertook this study to evaluate and validate aortic acceleration and other aortic parameters derived from Doppler aortic flow velocity as potential noninvasive surrogates to assess LV contractility in mice.
Materials and methods
Studies were conducted in 10 wild-type mice (group 1: avg. age 5 months; 4 males and 6 females; C57BL/6J) and in 6 wild-type mice (group 2: avg. age 9 months, 3 males and 3 females; C57BL/6J). Mice were housed in the animal facility at the Neurosensory vivarium of Baylor College of Medicine. This facility is approved by the American Association for Accreditation of Laboratory Animal Care. Animals were kept in rooms at controlled temperature (24 °C) and lighting (14:10 h light–dark cycle) with free access to food and water. The diets of both groups of mice consisted of normal chow.
Mice from group 1 were anesthetized with 3% isoflurane in oxygen in the induction chamber and then transferred to a heated (38 ± 1 °C) electrocardiogram (ECG) board (Rodent Surgical Monitor, Indus Instruments, Webster, TX) with the limbs taped to electrodes and 1.5% isoflurane anesthesia delivered continuously via nose cone. Body fur was shaved in the neck area and prepared for right carotid artery cannulation. Mice from group 2 underwent similar preparation but body fur was shaved in the chest area to allow for simultaneous Doppler and echocardiography measurements. All animal protocols were approved by the Institutional Animal Care and Use Committee of Baylor College of Medicine in accordance with the National Institutes of Health Guide for the Care and Use of Laboratory Animals (National Research Council 2011. Guide for the Care and Use of Laboratory Animals: 8th Ed. Washington, DC: The National Academies Press). The following experimental studies were conducted in the two groups of mice.
Group 1: Ten mice | Group 2: Six mice |
|---|---|
Simultaneous invasive pressure and noninvasive Doppler measurements | Day 1: Simultaneous noninvasive Doppler and echocardiography measurements Day 4: Noninvasive Doppler measurements Day 7: Noninvasive Doppler measurements |
Simultaneous invasive pressure and noninvasive Doppler measurements
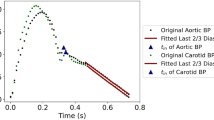
The invasive (aortic and left ventricular blood pressure) and noninvasive (ascending aorta blood flow velocity) measurements were made simultaneously. The surgical procedure to cannulate the mouse right carotid artery for intravascular and intraventricular pressure measurements was done as described previously21. Briefly, the catheter and pressure amplifier were calibrated for each experiment from 0 to 250 mm Hg using a mercury manometer. Blunt dissection techniques were used to expose the right carotid artery for cannulation with an intravascular pressure catheter (SPR1000 - Millar Mikro-tip catheter transducer, Millar, Inc., Houston, TX). The catheter was initially advanced into the ascending aorta and held in place. Aortic blood flow velocity was measured using a 20-MHz pulsed Doppler probe and a real-time signal acquisition and spectrum analyzer system (DFVS-Doppler Flow Velocity System, Indus Instruments, Houston, TX). The Doppler probe was placed slightly to the right of the suprasternal notch and oriented towards the heart and aortic root, the probe orientation adjusted with a micromanipulator in the direction from the right ear of the mouse towards the ascending aorta (Fig. 1). The probe was positioned such that the angle between the sound beam and the direction of aortic flow was less than 20° (velocity underestimation error ≤ 6.03%), and the range gate depth was adjusted between 3 and 4 mm to obtain maximal velocity. With the aortic pressure and velocity signals being displayed simultaneously, a 3-s segment of both signals was recorded. The catheter was then advanced into the LV. Again, 3-s segments of LV pressure and aortic flow velocity signals were recorded at baseline and after IP administration of single dose (1.5 μg/g) positive ionotropic agent dobutamine21. Maximal first derivative of LV pressure (+ dP/dtmax or P′) was calculated from the LV pressure signal. Aortic flow velocity waveforms were processed to calculate peak aortic velocity (vp), peak aortic velocity squared/rise time (vp2/T), peak (v′p) aortic acceleration, and mean (v′m) aortic acceleration. As shown in Fig. 2, v′m is calculated as vp/T, where T is the rise time or the time from foot of the waveform to vp.
Experimental setup to simultaneously measure ascending aortic flow velocity using DFVS, left ventricular pressure using Millar catheter, and ECG in group 1 mice. Here the 20 MHz Doppler probe is oriented (angle ≤ 20°) towards the ascending aorta with sample volume placed at aortic root. Shown in the plot are ascending aortic outflow velocity (sampled at the site shown by blue dot), LV pressure (sampled at catheter tip in LV), and ECG signals.
Waveforms of (A) invasively measured left ventricular pressure (P) waveform and its first derivative (P′) and (B) noninvasively measured aortic outflow velocity (v) waveform and its first derivative (v′). (C) Figure showing the invasive parameter left ventricular P′ and the noninvasive parameters peak aortic velocity (vp), peak aortic velocity squared/rise time (vp2/T), peak aortic acceleration (v′p) and mean aortic acceleration (v′m). Also shown is the ECG waveform and the time in milliseconds.
Simultaneous noninvasive Doppler and echocardiography measurements
The Doppler (ascending aorta blood flow velocity) measurements and Echocardiography (m-mode and ascending aorta blood flow velocity) measurements were made simultaneously. Aortic blood flow velocity was measured as described in the previous section using the 20-MHz pulsed Doppler probe and DFVS. Again, the Doppler probe was placed slightly to the right of suprasternal notch and oriented towards the heart and aortic root, the probe orientation adjusted with a micromanipulator in the direction from the right ear of the mouse towards the ascending aorta (Fig. 3). In this instance we estimated that the angle between the sound beam and the direction of aortic flow was less than 25° (velocity underestimation error ≤ 9.37%), and the range gate depth was adjusted between 3 and 4 mm to obtain maximal velocity. Echocardiography measurements of m-mode and ascending aorta blood velocity were made with VEVO770 system (VisualSonics, Toronto, ON, Canada) and 710B probe (angle estimated at about 70°—see Fig. 3). Simultaneous measurements were made at baseline and after the IP administration of single dose (1.5 μg/g) of positive inotropic agent dobutamine. From the aortic flow velocity signals measured by both systems peak aortic velocity (vp), peak (v′p) and mean (v′m) acceleration, and peak aortic velocity squared/rise time (vp2/T) were calculated (as shown in Fig. 2). Also, left ventricular ejection fraction (%EF), fractional shortening (%FS), and cardiac output (CO) were calculated from the dimensions measured by echocardiography. For demonstration of serial Doppler measurements by DFVS only, we used the above data as first day of measurements followed by Doppler measurements made on the fourth and the seventh days.
Experimental setup to simultaneously measure ascending aortic Doppler flow velocity using DFVS, left ventricular dimensions and ascending aortic flow velocity using VEVO770 system with 710B probe. Also, shown in the figure are lines representing the horizontal plane, and the angle of orientation of 20 MHz Doppler probe (≤ 25°) and that of the 710B probe (≈70°).
Statistics
The body weight of group 1 mice is expressed as mean ± SE (n) and the lowest and highest heart rates are listed. Scatter plots of invasively obtained P′ versus each noninvasively obtained parameters: (1) peak aortic velocity (vp), (2) peak aortic velocity squared/rise time (vp2/T), 3) peak aortic acceleration (v′p), and 4) mean aortic acceleration (v′m) were made. Linear regression analysis was performed and the respective linear fit relationships, the correlation coefficients (r), and the p values were calculated. p values < 0.05 were considered significant.
Bland–Altman analysis26 was used to evaluate the degree of agreement between P′ and each of the four Doppler derived parameters by plotting the difference against mean of the measurements. The data of all animals were normalized to unity (italicized) to compare parameters having different units. The mean of differences (estimation of bias) and standard deviation (measurement error) of: (1) P′ vs. vp, (2) P′ vs. vp2/T, (3) P′ vs. v′p, and (4) P′ vs. v′m, and the respective limits of agreement and 95% confidence intervals were calculated.
The heart rate and body weight of group 2 mice are expressed as mean ± SE (n). The four parameters (vp, vp2/T, v′p, and v′m) derived from baseline aortic velocity signals measured simultaneously with DFVS and echocardiography were compared. The % change from baseline values of the parameters vp, vp2/T, v′p, and v′m obtained by Doppler and echocardiography and the parameters cardiac output, % ejection fraction, and % fractional shortening derived from dimensions measured by echocardiography were calculated and compared. Additionally, the parameters vp, vp2/T, v′p, and v′m were calculated from serial repeated Doppler measurements of ascending aortic flow velocity made by DFVS on the first, the fourth, and the seventh day (at baseline and post-dobutamine) and compared using paired t-tests and p values < 0.05 were considered significant.
Results
Simultaneous invasive pressure and noninvasive Doppler measurements
The average body weight (BW) of group 1 mice was 39.0 ± 1.3 g (10) with males weighing more than females. The heart rate ranged from a low heart rate of 387 bpm measured at baseline to a high heart rate of 701 bpm measured after the administration of dobutamine among the 227 data points used for comparison between the methods. The average percentage change in values in response to dobutamine (inotropic effect) was 28% for vp, 172% for vp2/T, 72% for v′p, 85% for v′m and 90% for P′. Linear regression analysis of the invasively obtained P′ versus each of the four noninvasive Doppler derived parameters (vp, vp2/T, v′p, and v′m) are shown in Fig. 4. Each plot shows the linear relationship, coefficient of determination (r2), correlation coefficient (r), and p value for each of the four noninvasive indices.
Linear regression analysis of (A) peak aortic velocity, vp vs. P′ ( or + dP/dtmax), (B) peak aortic velocity2/T, vp2/T vs. P′, (C) peak aortic acceleration, v′p vs. P′, and (D) mean aortic acceleration, v′m vs. P′. Shown in each plot is the linear fit equation, the coefficient of determination and the correlation coefficient. The p-values of all were p < 0.0001.
The Bland–Altman analysis plots are shown in Figs. 5 and 6 (normalized parameters are italicized). The mean of differences ± SD (meandiff ± SD) and the precision of the estimated limits of agreement (meandiff, + 2SD, -2SD) of all measurements based on 95% confidence intervals (CI) are given in Table 1.
(A) Normalized Bland–Altman plot of the agreement between + dP/dtmax (P′) and peak aortic velocity (vp). Plot of Difference (P′–vp) versus Mean ½(P′ + vp) along with the histogram distribution of the differences. (B) Normalized Bland–Altman plot of the agreement between + dP/dtmax (P′) and peak aortic velocity2/T (vp2/T). Plot of Difference (P′–vp2/T) versus Mean ½ (P′ + vp2/T) along with the histogram distribution of the differences.
(A) Normalized Bland–Altman plot of the agreement between + dP/dtmax (P′) and peak aortic acceleration (v′p). Plot of Difference (P′– v′p) versus Mean ½ (P′ + v′p) along with the histogram distribution of the differences. (B) Normalized Bland–Altman plot of the agreement between + dP/dtmax (P′) and mean aortic acceleration (v′m). Plot of Difference (P′– v′m) versus Mean ½ (P′ + v′m) along with the histogram distribution of the differences.
Simultaneous noninvasive Doppler and echocardiography measurements
The average body weight of group 2 mice was 33.7 ± 3.0 g (6) with males weighing more than females. The average heart rate at baseline was 387 ± 27 bpm and post-dobutamine was 516 ± 16 bpm on the first day of serial measurements. The comparison of measurements made with Doppler (DFVS) and echocardiography system only on the first day of serial measurements are shown in Table 2.
From Table 2 we find that without any angle correction the echocardiography measurements are significantly lower than those made with Doppler using DFVS. When we arbitrarily used a 45° angle correction the parameters generated by both methods were not significantly different. Comparison of the % change from baseline values of the parameters vp, vp2/T, v′p, and v′m obtained by Doppler and echocardiography and the parameters cardiac output, % ejection fraction, and % fractional shortening derived from dimensions measured by echocardiography showed that all parameters increased significantly from baseline (p < 0.05; see Fig. 7).
Table 3 below shows the comparison of parameters body weight, heart rate, vp, vp2/T, v′p, and v′m measured by Doppler on first day (D1), fourth day (D4), and seventh day (D7) to demonstrate serial studies. No significant differences were observed in the parameters at baseline of the 3 days. Also, no significant differences were observed in the parameters except between the post-dobutamine heart rates of D1 and D4.
Discussion
The end systolic pressure–volume relationship is considered as the “gold standard” index of left ventricular contractility but the maximal rate of change of left ventricular pressure (+ dP/dtmax or P′) is considered as a reasonable alternative index of contractility27. This index has been used in humans2,28,29,30 large animals7,8,31,32 and more recently in small animals such as mice16,18,19,21,22,24,33. While humans and large animals survive the invasive measurement of left ventricular pressure, in mice this measurement is made acutely and the study is terminal, making longitudinal/serial studies of cardiac contractility/performance impossible. Unlike in large animals, the placement of the catheter in the left ventricle of the mouse forces the ascending aorta and the heart of the mouse to conform to the rigidity of the catheter. This perturbs the mouse hemodynamics to the extent of making the invasive LV contractility measurement in mice less precise. We conducted this study to evaluate the potential use of aortic acceleration obtained from the noninvasively measured aortic blood flow velocity as a surrogate to P′ obtained from the invasively measured LV pressure in mice. To our knowledge this is the first mouse study to perform this evaluation using simultaneously measured LV pressure (and P′) and aortic blood velocity (and vp, vp2/T, v′p, and v′m).
Precedence of development of noninvasive indices of cardiac contractility
Ever since the 1960s, researchers have attempted to develop noninvasive indices of cardiac contractility in humans11,34,35,36 and in animal models, like dogs5,32,37,38, pigs7,39, sheep8,40, rabbits41, rats9,42,43 and even in mice44. The noninvasive methods included echocardiography44,45,46, tissue Doppler imaging47, Tei index48,49, maximal rate of change aortic volume flow38, to list a few. The imaging methods are cumbersome and time consuming; the tissue Doppler imaging and Tei index calculation depend on the quality of the acquired signals and time resolution, and volume flow measurements are extravascular and partially invasive.
Justification for aortic flow velocity parameters as indices of cardiac contractility
The results from our study demonstrate that there is significant correlation between the invasively derived maximal rate of change of left ventricular pressure (P′) and each of the noninvasively derived indices of: peak aortic velocity (vp), peak aortic velocity squared/rise time(vp2/T), peak aortic acceleration (v′p), mean aortic acceleration (v′m).
The justification for use of peak aortic flow velocity (vp) to define ventricular contractility comes from the definition by Rushmer31 that the initial ventricular impulse is the net force acting over the time from the beginning of ejection to the attainment of peak aortic flow velocity. This net force is due the initial rapid increase in LV pressure as determined by its rate of change and the rate of blood flowing into the aorta during the initial phase of ejection31. We found that P′ was well correlated to vp (r = 0.88, Fig. 4A) and in agreement with the findings by others11,34,35, but found that correlation coefficient of P′ versus vp was the lowest of the four parameters we evaluated. Hunt et al. also found that P′ had the lowest correlation to vp34 and Lambert et al. reported that that vp was much less sensitive than mean or peak aortic accelerations in assessing LV contractility25.
The parameter peak aortic velocity squared/rise time (vp2/T) was adopted from Hunt et al., who derived a mathematical equation from the basic principle that force generated by LV translates into kinetic energy of blood flow, implying that P′ was directly proportional to vp2/T and found that vp2/T had the best correlation with P′ in humans (r = 0.77, p < 0.001)34. In this study we found P′ had the second highest and significant correlation vp2/T (r = 0.93; Fig. 4B).
The force generated by the contracting ventricle causes the acceleration of blood into the aorta. The maximum generated force to overcome inertia in early systole results in peak aortic blood acceleration (v′p), which decreases rapidly before any changes occur, and is therefore considered as the most sensitive index of myocardium contractility37. In our study v′p was also highly correlated P′ (r = 0.89; Fig. 4C) and agrees with the findings by others29,37,50. According to Lambert et al. peak aortic acceleration is the second most sensitive of all the noninvasive parameters25. Harada et al. showed that the product of v′p, pulse wave velocity (c), and the density of blood (ρ) highly correlated with P′ (ρc⋅ v′p = 1.01P′−2, r = 0.97)5. We were unable to confirm this as we did not measure pulse wave velocity in this study. Pulse wave velocity measurement requires the placement of Doppler probes at two additional arterial sites and this would increase the amount of time required for each LV contractility measurement.
Aortic velocity waveforms are computed from Doppler spectrograms which can be noisy. Determination of peak aortic acceleration (v′p) requires high fidelity aortic velocity waveforms that need to be sampled at high rates such that a less noisy first derivative can be calculated. So, mean aortic acceleration (v′m = vp/T), which is simpler to calculate is used instead of peak aortic acceleration. Of the four indices we evaluated, we found that v′m had the highest correlation with P′ (r = 0.94; Fig. 4D). In humans34 and dogs38,50 v′m was found to be significantly correlated to P′. Lambert et al. found v′m to be the most sensitive of all the noninvasive parameters25. Bauer et al. reported that mean aortic acceleration had a strong correlation with maximal LV elastance (another contractility index)8.
Since we compared two parameters whose units were different, we normalized each data set to unity (like that reported by Morimont et al.27) to perform Bland–Altman tests. Bland–Altman analysis plots (Fig. 5 and 6) revealed good agreement between the invasive obtained P′ and each of the noninvasively derived parameters vp, vp2/T, v′p, and v′m. From Table 1, we can see that the 95% CI of estimated limits of agreement are quite narrow and, therefore, acceptable. We cannot compare our findings from Bland–Altman analysis of our parameters with other studies as those studies have not performed the Bland–Altman analysis.
Comparison to echocardiography parameters
Comparison of the four aortic flow velocity parameters without using angle correction showed that the echocardiography method significantly underestimated these parameters (Table 2). When a 45° angle correction was applied only to the signal measured by echocardiography the differences were not significant, but the values were still lower than those measured by DFVS. We did not apply an angle correction (of ≤ 25°) to the Doppler measurements and this would result in a < 10% error in estimating peak aortic velocity. The results we obtained with echocardiography in estimating peak aortic velocity and accelerations agree with the finding by Yang et al.51 that the VEVO770 with 710B probe results in measurement error of about 35% at 40° and about 82% at 70°. In our study the measurements made by echocardiography underestimated peak aortic velocity by 35.5% without angle correction and by 8.3% with a 45° angle correction when compared to the measurement made by DFVS. Other investigators have suggested that for a probe orientation at above 60° the smallest error in estimating the true angle can result in large measurement errors52. We, however, believe that the measurement error needs to be kept as small as possible if serial measurements are planned. With the small footprint of our Doppler probes it is possible for us to achieve angles as low as 10° between the ultrasound beam and the axial direction of blood flow. We previously reported that measurement of Doppler velocity with angle correction within 5° of the true angle, if the probe angle is 25°or less, limits the measurement error to less than 5%53. A noteworthy observation is that, when baseline-to-post-dobutamine %changes were considered, both methods yielded similar results regardless of angle correction.
The percent changes in baseline-to-post-dobutamine responses also showed that all aortic velocity parameters (by both Doppler & echocardiography) including mean aortic velocity (vm; by Doppler) increased significantly in the same direction as cardiac output, % ejection fraction, and % fractional shortening derived from LV dimensions measured by echocardiography (Fig. 7). In the case of myocardial infarction measurements of LV dimensions with echocardiography may depend on where the probe is placed, that is, measurements made in non-infarcted zone can produce results that are totally different from the measurements made from infarcted zone or from somewhere in between the two zones. Serial assessment of function also depends on the consistency of the operator making the measurements at the same location at each time point. By contrast, peak aortic flow velocity and its acceleration represent a comprehensive global systolic (contractile) function with little ambiguity.
Repeatability studies
The body weights, heart rates, and the four aortic flow velocity parameters (vp, vp2/T, v′p, and v′m) measured in the same group 2 mice on 3 different days showed no significant differences in baseline measurements indicating that serial studies done within a short period of time in normal animals do not show significant changes within a few days thereby demonstrating repeatability. In a previous study our group has shown that peak aortic velocity (vp) obtained from repeated measurements of aortic flow velocity can be used to study systolic function in mouse models of myocardial remodeling54. Serial measurements of vp were made in 3 groups of mice categorized as sham controls (SC), permanent occluded (PO), and 2-h occlusion/reperfusion (OR) (of left anterior descending coronary artery) over a period of up to 6 months of age. They reported that vp in both PO and OR groups dropped to about 75% of baseline values, followed by a recovery in the OR group to the same levels as SC by the 8th week, but the PO group remained at about 75% of the baseline at about 6 months indicating a significant decrease in systolic function.
Advantages and potential applications
One obvious advantage of noninvasive measurements is that they can be made repeatedly over the short-term or long-term serially using an animal as its own control. The second advantage is that these measurements can be done without significantly altering the physiology. Shown in Fig. 8 are three conditions under which aortic flow velocity signals are measured in the same mouse. The first panel shows an aortic flow velocity spectrogram in an intact animal with vp around 100 cm/s (considered normal). The second panel shows the simultaneous measurement of aortic velocity spectrogram (with vp increased to 125 cm/s) and aortic pressure signal measured with a 1F (0.33 mm diameter) intravascular catheter. The third panel shows the simultaneous measurement of aortic velocity spectrogram and LV pressure signal (with the same catheter across the aortic valve). In this case vp is further increased to 132 cm/s along with some aortic regurgitation.
Using an allometric equation, AD = 3.6 BW3/8, relating aortic diameter (AD) to body weight (BW) in mammals55 we estimated that the aortic diameter in this 34 g (0.034 kg) mouse was 1.01 mm resulting in a luminal area of 0.8012 mm2. Thus, the presence of the catheter (0.33 mm dia. or 0.0855 mm2 cross-sectional area) in the lumen will cause about 12% increase in vm and peak aortic velocity is expected to change in a similar way. In this mouse we found that vp increased by 21% with the catheter in the aorta and increased by another 7% when the catheter was advanced into the LV. The presence of aortic regurgitation calls into question the correction made to the P′ using LV end diastolic volume or pressure to account for preload.
The validation and use of aortic acceleration as an index of cardiac contractility in humans and large animals has suggested its utility in mice, despite not being evaluated. Our study suggests that this technique is useful in allowing longitudinal studies in mice to assess changes with age or interventions. Previously our group has reported the use of mean aortic acceleration to compare cardiac function in mice that have been injected with saline or AICAR56. or to describe cardiac function in desmin null mice with Bcl-2 overexpression57, or to study the effects of TAC in SRC-2 KO mice58. Others have reported the use of both peak and mean aortic acceleration to describe cardiac function at baseline and post-dobutamine in ApoE-KO mice59. The measurements of aortic velocity signal in all these studies were made with a high-speed and high-fidelity Doppler system (DFVS) and signals were acquired at high sampling rates. The peak velocity envelope calculated by the analysis software60 is critical in calculating the Doppler indices. Another advantage is that Doppler measurements can be made much faster with DFVS than with echocardiography.
Limitations of the study
LV dP/dtmax (P′) can be affected by preload, afterload, heart rate and myocardial hypertrophy. In this study we did not make measurements with changes to preload or afterload. Under the conditions of this study we assumed that preload and afterload are unchanged. Since we are studying the relative responses of invasive and noninvasive parameters to changes in hemodynamics, we assumed that preload and afterload are not significantly altered with single administration of dobutamine. As Lambert et al. have alluded to, experimentally induced changes to preload and afterload are less physiological and therefore, may be less relevant in this evaluative study25. Wallmeyer et al. noted that the correlation between the Doppler indices and P′ was not significantly affected after adjusting preload or heart rate and concluded that both noninvasive and invasive indices are similarly affected by the above variables38.
A limitation of noninvasive Doppler indices is that they do not directly measure cardiac contractility34,38 and therefore are only as sensitive as invasive indices. Since the noninvasive indices do not describe the inotropic state in absolute terms they can be only used for comparisons within a subject (that is, each subject as its own control) which is more practical in animal studies than in clinical applications.
Echocardiography was used in several studies8,44,45,46 to measure aortic flow velocity, but we believe that echocardiography measurement of aortic outflow in mice may not be sensitive enough for serial measurements of LV contractility. Bauer et al. however, noted that v′m calculated from aortic velocity measured at LV outflow tract (LVOT) in sheep consistently reflected changes observed in LV contractility8. All our measurements of aortic velocity were made in the LVOT using a 2 mm Doppler probe mounted on a micromanipulator to optimize the signal and stabilize the position.
Future studies
We did not evaluate the noninvasive indices with the administration of a negative inotrope, which would have provided a reasonable representation of heart failure models. In our future studies we will include negative inotrope intervention as well as preload and afterload variations and study the effects on Doppler indexes of left ventricular performance, and to help identify the Doppler index that best reflects changes in contractility. Since this study was done using young mice, we will conduct studies to validate these results in middle-aged and old mice.
Conclusions
We compared four parameters (peak aortic velocity, peak aortic velocity squared/rise time, peak aortic acceleration, and mean aortic acceleration) derived from aortic velocity waveform to the first derivative of LV pressure. The aortic velocity and the LV pressure waveforms were measured simultaneously at baseline and after the administration of dobutamine. The results showed that the four noninvasive indices had a high degree of correlation and agreement with the first derivative of LV pressure, indicating that mean or peak aortic acceleration, or peak aortic velocity squared/rise time or even peak velocity derived from aortic velocity may be used as a noninvasive index of LV contractility. We also performed repeatability studies to successfully demonstrate that noninvasive serial studies can be done with ease.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Change history
03 December 2021
A Correction to this paper has been published: https://doi.org/10.1038/s41598-021-03203-0
06 April 2021
A Correction to this paper has been published: https://doi.org/10.1038/s41598-021-87101-5
References
Eskander, M. & Kern, M. J. Invasive hemodynamics of myocardial disease: systolic and diastolic dysfunction (and Hypertrophic obstructive cardiomyopathy). Interv. Cardiol. Clin. 6, 297–307 (2017).
Willemen, E. et al. The left and right ventricles respond differently to variation of pacing delays in cardiac resynchronization therapy: A combined experimental–computational approach. Front. Physiol. 10, 17 (2019).
Assis, F. R. et al. Minimally invasive transtracheal cardiac plexus block for sympathetic neuromodulation. Heart Rhythm 16, 117–124 (2019).
Monge Garcia, M. I. et al. Performance comparison of ventricular and arterial dP/dtmax for assessing left ventricular systolic function during different experimental loading and contractile conditions. Crit. Care 22, 325 (2018).
Harada, Y. et al. Principle of a noninvasive method of measuring Max(dP/dt) of the left ventricle: theory and experiments. Heart Vessels 3, 25–32 (1987).
Adachi, T., Ohba, T., Fujisawa, S. & Ono, K. Noninvasive monitoring of cardiac preload and contractility by heart beat-derived mechanical vibration on the chest wall in guinea pigs. J. ATAMIS 1, 15–19 (2016).
A’roch, R., Gustafsson, U., Johansson, G., Poelaert, J. & Haney, M. Left ventricular strain and peak systolic velocity: responses to controlled changes in load and contractility, explored in a porcine model. Cardiovasc. Ultrasound. 10, 22 (2012).
Bauer, F. et al. Left ventricular outflow tract mean systolic acceleration as a surrogate for the slope of the left ventricular end-systolic pressure-volume relationship. J. Am. Coll. Cardiol. 40, 1320–1327 (2002).
9de Wildt, D. J. & Sangster, B. An evaluation of derived aortic flow parameters as indices of myocardial contractility in rats. J Pharmacol Methods 10, 55–64, (1983).
Germano, G., Angotti, S., Muscolo, M., D’Auria, F. & Giordano, M. The (dP/dt)max derived from arterial pulse waveforms during 24 h blood pressure oscillometric recording. Blood Press. Monit. 3, 213–216 (1998).
Kolettis, M., Jenkins, B. S. & Webb-Peploe, M. M. Assessment of left ventricular function by indices derived from aortic flow velocity. Br. Heart J. 38, 18–31 (1976).
Kyriazis, J., Glotsos, J., Bilirakis, L. & Smirnioudis, N. The (dP/dt)max derived from arterial pulse waveforms: Prospective applications in the haemodialysis setting. Nephrol. Dial Transplant. 16, 1087–1088 (2001).
Hartley, C. J., Taffet, G. E., Reddy, A. K., Entman, M. L. & Michael, L. H. Noninvasive cardiovascular phenotyping in mice. ILAR J. 43, 147–158 (2002).
Woodbury, R. A. & Hamilton, W. F. Blood pressure studies in small animals. Am. J. Physiol. 119, 663–674 (1937).
Grupp, I. L., Subramaniam, A., Hewett, T. E., Robbins, J. & Grupp, G. Comparison of normal, hypodynamic, and hyperdynamic mouse hearts using isolated work-performing heart preparations. Am. J. Physiol. Heart Circ. Physiol. 265, H1401–H1410 (1993).
Kitano, Y. et al. General pharmacological profile of the new cognition-enhancing agent nefiracetam. Arzneimittelforschung 44, 199–210 (1994).
Herzum, M. et al. Left ventricular haemodynamics in murine viral myocarditis. Eur. Heart J. 16, 28–30 (1995).
Rockman, H. A. et al. Enhanced myocardial relaxation in vivo in transgenic mice overexpressing the beta2-adrenergic receptor is associated with reduced phospholamban protein. J. Clin. Invest. 97, 1618–1623 (1996).
Hoit, B. D. et al. Influence of transgenic overexpression of phospholamban on postextrasystolic potentiation. J. Mol. Cell Cardiol. 31, 2007–2015 (1999).
Kiriazis, H. et al. Preserved left ventricular structure and function in mice with cardiac sympathetic hyperinnervation. Am. J. Physiol. Heart Circ. Physiol. 289, H1359-1365 (2005).
Reddy, A. K. et al. Cardiac function in young and old Little mice. J. Gerontol. A Biol. Sci. Med. Sci. 62, 1319–1325 (2007).
Shibata, K. et al. Spontaneous development of left ventricular hypertrophy and diastolic dysfunction in mice lacking all nitric oxide synthases. Circ. J. 74, 2681–2692 (2010).
Reddy, A. K. et al. Young little mice express a premature cardiovascular aging phenotype. J. Gerontol. A Biol. Sci. Med. Sci. 69, 152–159 (2014).
Ghimire, A., Bisset, E. S. & Howlett, S. E. Ischemia and reperfusion injury following cardioplegic arrest is attenuated by age and testosterone deficiency in male but not female mice. Biol. Sex Differ. 10, 42 (2019).
Lambert, C. R. Jr., Nichols, W. W. & Pepine, C. J. Indices of ventricular contractile state: Comparative sensitivity and specificity. Am. Heart J. 106, 136–144 (1983).
Bland, J. M. & Altman, D. G. Measuring agreement in method comparison studies. Stat. Methods Med. Res. 8, 135–160 (1999).
Morimont, P. et al. Arterial dP/dtmax accurately reflects left ventricular contractility during shock when adequate vascular filling is achieved. BMC Cardiovasc. Disord. 12, 13 (2012).
Gleason, W. L. & Braunwald, E. Studies on the first derivative of the ventricular pressure pulse in man. J. Clin. Invest. 41, 80–91 (1962).
Klinke, W. P. et al. Use of catheter-tip velocity-pressure transducer to evaluate left ventricular function in man: effects of intravenous propranolol. Circulation 61, 946–954 (1980).
Drake-Holland, A. J., Mills, C. J., Noble, M. I. & Pugh, S. Responses to changes in filling and contractility of indices of human left ventricular mechanical performance. J. Physiol. 422, 29–39 (1990).
Rushmer, R. F. Initial ventricular impulse. A potential key to cardiac evaluation. Circulation 29, 268–283 (1964).
Adler, D., Nikolic, S. D., Sonnenblick, E. H. & Yellin, E. L. Time to dP/dtmax, a preload-independent index of contractility: Open-chest dog study. Basic Res. Cardiol. 91, 94–100 (1996).
Nemoto, S., Defreitas, G., Mann, D. L. & Carabello, B. A. Effects of changes in left ventricular contractility on indexes of contractility in mice. Am. J. Physiol. Heart Circ. Physiol. 283, H2504–H2510 (2002).
Hunt, A. C. et al. Evaluation of a theoretical Doppler index to noninvasively estimate peak dP/dt using continuous wave Doppler ultrasound of ascending aortic flow in man. Cathet. Cardiovasc. Diagn. 23, 219–222 (1991).
Tasu, J. P. et al. Estimation of left ventricular performance through temporal pressure variations measured by MR velocity and acceleration mappings. J. Magn. Reson. Imaging 16, 246–252 (2002).
Zhong, L. et al. Validation of a novel noninvasive cardiac index of left ventricular contractility in patients. Am. J. Physiol. Heart Circ. Physiol. 292, H2764–H2772 (2007).
Noble, M. I. M., Trenchard, D. & Guz, A. Left ventricular ejection in conscious dogs: measurement and significance of the maximum acceleration of blood from the left ventricle. Circ. Res. 19, 139–147 (1966).
Wallmeyer, K., Wann, L. S., Sagar, K. B., Kalbfleisch, J. & Klopfenstein, H. S. The influence of preload and heart rate on Doppler echocardiographic indexes of left ventricular performance: Comparison with invasive indexes in an experimental preparation. Circulation 74, 181–186 (1986).
Vogel, M. et al. Validation of myocardial acceleration during isovolumic contraction as a novel noninvasive index of right ventricular contractility: Comparison with ventricular pressure–volume relations in an animal model. Circulation 105, 1693–1699 (2002).
Hashimoto, I. et al. Myocardial strain rate is a superior method for evaluation of left ventricular subendocardial function compared with tissue Doppler imaging. J. Am. Coll. Cardiol. 42, 1574–1583 (2003).
Moran, A. M. et al. Noninvasive serial evaluation of myocardial mechanics in pressure overload hypertrophy of rabbit myocardium. Herz 28, 52–62 (2003).
Reffelmann, T. & Kloner, R. A. Transthoracic echocardiography in rats. Evalution of commonly used indices of left ventricular dimensions, contractile performance, and hypertrophy in a genetic model of hypertrophic heart failure (SHHF-Mcc-facp-Rats) in comparison with Wistar rats during aging. Basic Res. Cardiol. 98, 275–284 (2003).
Dowell, R. T. & Houdi, A. A. Aortic peak flow velocity as an index of myocardial contractility in the conscious rat. Methods Find Exp. Clin. Pharmacol. 19, 533–539 (1997).
Broberg, C. S. et al. Validation of the myocardial performance index by echocardiography in mice: A noninvasive measure of left ventricular function. J. Am. Soc. Echocardiogr. 16, 814–823 (2003).
Sugawara, M. et al. Noninvasive estimation of left ventricular Max(dP/dt) from aortic flow acceleration and pulse wave velocity. Echocardiography 11, 377–384 (1994).
Chung, N., Nishimura, R. A., Holmes, D. R. Jr. & Tajik, A. J. Measurement of left ventricular dp/dt by simultaneous Doppler echocardiography and cardiac catheterization. J. Am. Soc. Echocardiogr. 5, 147–152 (1992).
Ferferieva, V. et al. Assessment of strain and strain rate by two-dimensional speckle tracking in mice: Comparison with tissue Doppler echocardiography and conductance catheter measurements. Eur. Heart J. Cardiovasc. Imaging 14, 765–773 (2013).
Tei, C., Nishimura, R. A., Seward, J. B. & Tajik, A. J. Noninvasive Doppler-derived myocardial performance index: Correlation with simultaneous measurements of cardiac catheterization measurements. J. Am. Soc. Echocardiogr. 10, 169–178 (1997).
LaCorte, J. C. et al. Correlation of the Tei index with invasive measurements of ventricular function in a porcine model. J. Am. Soc. Echocardiogr. 16, 442–447 (2003).
Sagar, K. B. et al. Comparison of peak and modal aortic blood flow velocities with invasive measures of left ventricular performance. J. Am. Soc. Echocardiogr. 1, 194–200 (1988).
Yang, X. et al. Assessment of spectral doppler in preclinical ultrasound using a small -size rotating phantom. Ultrasound. Med. Biol. 39, 1491–1499 (2013).
Hoskins, P. Principles of Doppler ultrasound. In Diagnostic Ultrasound: Physics and Equipment Vol. 158 (eds Hoskins, P. et al.) (Cambridge University Press, Cambridge, 2003).
Reddy, A. K. et al. Multichannel pulsed Doppler signal processing for vascular measurements in mice. Ultrasound. Med. Biol. 35, 2042–2054 (2009).
Michael, L. H. et al. Myocardial infarction and remodeling in mice: effect of reperfusion. Am. J. Physiol. Heart Circ. Physiol. 277, H660–H668 (1999).
Dawson, T. H. Engineering Design of the Cardiovascular System of Mammals (Prentice Hall, Upper Saddle River, 1991).
Cieslik, K. A. et al. AICAR-dependent AMPK activation improves scar formation in the aged heart in a murine model of reperfused myocardial infarction. J. Mol. Cell Cardiol. 63, 26–36 (2013).
Weisleder, N., Taffet, G. E. & Capetanaki, Y. Bcl-2 overexpression corrects mitochondrial defects and ameliorates inherited desmin null cardiomyopathy. Proc. Natl. Acad. Sci. U S A 101, 769–774 (2004).
Reineke, E. L. et al. SRC-2 coactivator deficiency decreases functional reserve in response to pressure overload of mouse heart. PLoS ONE 7, e53395 (2012).
Vincelette, J., Martin-McNulty, B., Vergona, R., Sullivan, M. E. & Wang, Y. X. Reduced cardiac functional reserve in apolipoprotein E knockout mice. Transl. Res. 148, 30–36 (2006).
Reddy, A. K. et al. Pulsed Doppler signal processing for use in mice: Design and evaluation. IEEE Trans. Biomed. Eng. 52, 1764–1770 (2005).
Acknowledgements
This study was funded in part by the NIH grants R42-HL144342, R43-HL142439, R43-AG059543, R01-AG059599, the DeBakey Heart Center and Hankamer foundation. We would like to thank Chitra Reddy for assisting with data analysis, Tonya Coulthard and Nicholas Pansters for presenting preliminary data of this study at conferences, and Dr. Rodrigo Lankenau for critical reading of the manuscript.
Author information
Authors and Affiliations
Contributions
A.K.R., C.J.H., M.L.E., G.E.T., J.E.T.P. conceived and designed the study. J.E.T.P., J.O.U., C.P.H., T.T.P., A.K.R. conducted the experiments. J.E.T.P., J.O.U., C.P.H., T.T.P., A.K.R. analyzed the data. SM contributed the equipment and auxiliary materials. A.K.R., J.E.T.P. wrote the manuscript. All authors reviewed and edited the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
Dr. Reddy is a member of the faculty at Baylor College of Medicine and a collaborator and consultant with Indus Instruments. Dr. Madala is the president of Indus Instruments and an adjunct faculty at Baylor College of Medicine. All other authors have no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this Article was revised: The original version of this Article contained errors in Table 2, where the values for echocardiography category were incorrect for “v’p (cm/s2)” and “v’m (cm/s2)”.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Perez, J.E.T., Ortiz-Urbina, J., Heredia, C.P. et al. Aortic acceleration as a noninvasive index of left ventricular contractility in the mouse. Sci Rep 11, 536 (2021). https://doi.org/10.1038/s41598-020-79866-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-79866-y
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.