Abstract
Paramedics working on a rotating shift are at an increased risk of developing chronic health issues due to continuous circadian rhythm disruption. The acute effects of shift rotation and objectively measured sleep have rarely been reported in paramedics. This study investigated the relationships between a rotating shift schedule and sleep (using actigraphy), subjective reports of sleepiness, mood, stress and fatigue. Galvanic Skin Response, energy expenditure and physical activity (BodyMedia SenseWear Armband) were also recorded across the shift schedule. Paramedics were monitored for a period of eight consecutive days across pre-shift, day shift, night shift, and 2 days off. Fifteen paramedics (M age = 39.5 and SD = 10.7 years) who worked rotational shifts experienced sleep restriction during night shift compared to pre-shift, day shift and days off (p < 0.001). Night shift was also associated with higher levels of stress (p < 0.05), fatigue (p < 0.05), and sleepiness (p < 0.05). One day off was related to a return to pre-shift functioning. Such shift-related issues have a compounding negative impact on an already stressful occupation with high rates of physical and mental health issues. Therefore, there is an urgent need to investigate methods to reduce rotating shift burden on the health of paramedics. This could be through further research aimed at providing recommendations for shift work schedules with sufficient periods for sleep and recovery from stress.
Similar content being viewed by others
Introduction
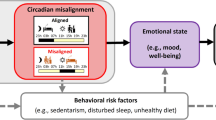
There is an increasing demand for 24-h emergency medical support, which requires paramedics to work around the clock often in rotating shifts1,2. The adverse outcomes of night shift work have previously been reported, and there is a growing evidence indicating that shift work is becoming a serious public health issue3. Thus, there is an increasing need to examine the impact of shift schedules on health and well-being.
A rotating shift is a combination of a night shift and a day shift in one shift schedule, with recovery days (day off) factored in-between schedules to allow readjustment to the new roster3. Rotating shift work is typically adopted to reduce the amount of night work as possible, as it may impact the well-being of the employees4. Although there are a few advantages of rotating shifts over constant night shift, including more stable circadian rhythms and longer sleep times5, it has been shown to impact on a range of health and safety outcomes, including an increased risk of fatigue, accidents, stress, depression, and chronic ailments compared to day shift workers6,7,8,9,10. For example, rotating shift workers reported significantly higher insomnia and excessive daytime sleepiness compared to standard day workers11. Furthermore, nurses working rotating rosters reported more stress as compared to nurses worked in fixed rosters12, and engineers working the same shift reported poor sleep quality and significant levels of fatigue13. Another study reported a strong relationship between a rotating roster and fatigue and sleep problems14. In addition, shift rotation has also been strongly linked to poorer mental health, particularly depression and anxiety15. The majority of these reported the possible consequences of a rotating shift in cross-sectional studies from a chronic point of view. Little is known about the immediate or acute effects of a rotating shift on workers, especially those working in the emergency medical fields such as nurses and paramedics.
The day-to-day interaction between shift rotation and workers health has been described in a few studies that used objective measures of sleep and activity. One study from Japan reported daily sleep patterns and physical activity across an entire rotating schedule16. Physical activity was significantly higher during day shifts than during night shifts, and total sleep time was shorter on day shifts compared to night shifts (5.8 vs 6.4 h)16. Another study investigating nurses working fixed shifts indicated that the nurses’ sleep, measured using a wrist actigraphy, did not differ significantly between day and night shifts17. In the same study, the levels of subjective fatigue and sleepiness also did not differ significantly between day and night shifts17. Another study of nurses working rotating shifts reported that nurses experienced a shorter duration of sleep on both day and night shifts equally18. However, nurses in another study slept less and reported poorer quality of sleep during night shift compared to day shift during a rotating shift schedule19. Thus, rotating shift work may have a more detrimental effect on sleep than fixed shifts. There are some variations in the previous reports due to diversity in occupations, workloads, and shift types. More studies are needed to investigate the effects of rotating shift schedules on health, especially with regard to acute effects contributing to long term outcomes. In particular, paramedics, due to the traumatic and stressful nature of their work20, are a group that generally need more investigation.
The present study aimed to investigate the relationships between a rotating shift schedule, sleep, mood, stress, fatigue, sleepiness, energy expenditure, and physical activity levels among Australian paramedics. Paramedics were monitored for a period of eight consecutive days across pre-shift day, night shift, day shift, and two days off. It was hypothesized that during night shift day, compared to pre-shift, day shift, and days off, paramedics would report lower sleep duration, physical activity, energy expenditure, poorer mood, and higher stress, fatigue, and sleepiness.
Method
All participants provided written informed consent prior to the study and all experimental protocols were carried out in accordance with the Declaration of Helsinki and the Australian National Statement on ethical conduct. The study was approved by the Royal Melbourne Institute of Technology Human Research Ethics Committee (ID# 21420).
Participants
Paramedics working in Victoria, Australia were invited to participate in this study through Ambulance Employees Australia Victoria (AEAV). Participation was voluntary and limited to active full-time paramedics aged at least 18 years old, working rotating shifts and without any self-reported history of/or treatment for the following conditions: insomnia, depression, and anxiety. A single rotating shift roster consisted of two standard days shift, followed by 2 days of night shift, and then 4 days off. Before consent, paramedics were asked if they have any history of/or received treatment for insomnia, depression or anxiety via phone calls or emails, then invited to the study if the previous inclusion criteria were obtained, otherwise they were excluded from the study. All participants reported working the same rotating shift type. A power analysis was conducted based on a previous field study in healthcare workers59, comparing baseline nocturnal total sleep time compared to daytime total sleep time following nightshift measured with actigraphy (effect size = 0.6). It was estimated that a sample size of 23 was required to detect an effect size of 0.6, with an α = 0.05 and β = 0.859.
Materials
BodyMedia SenseWear Armband
The BodyMedia SenseWear Armband (BSA; Jawbone, San Francisco, CA, USA) is a portable device that is connected to sensors where it can measures galvanic skin response, physical activity via steps count, and energy expenditure21. Galvanic skin response (GSR) is a valid mechanism to detect stress levels through changes in the electrical resistance of the skin22. The BSA was required to be worn on the non-dominant hand throughout the study.
Wrist actigraphy
The Actiwatch-2 (Philips Respironics, Murrysville, PA, USA) was used for wrist actigraphy, which worn on the non-dominant wrist. The data from the Actiwatch-2 were extracted via PC using Philips Respironics software. The outcome measures used were total sleep time, sleep efficiency, number of awakenings, wake after sleep onset (WASO), bedtime, get-up time, length of time in bed, and sleep onset latency23,24. The outcome data from the actigraphy were scored using the sleep diary.
Sleepiness and stress
The Karolinska Sleepiness Scale (KSS) was used to assess subjective state sleepiness on a nine-point rating scale, with higher scores indicating greater degree of sleepiness25. Stress was assessed using the question, ‘How stressed do you feel right now?’ answered on a five-point scale from 1 to 5 with higher numbers representing higher levels of stress.
Positive Affect and Negative Affect Scale
The Positive Affect and Negative Affect Scale (PANAS) is a tool with 20 items developed to investigate daily positive and negative emotions26. The present study used an abbreviated eight-item version that had been validated in a previous naturalistic study27.
Fatigue
Subjective fatigue was investigated using the Samn–Perelli Fatigue Checklist28. The checklist uses a ratings scale of 1–7, with higher scores indicating greater fatigue.
The Pittsburgh Sleep Diary
The Pittsburgh Sleep Diary (PSD) is a validated self-report diary consisting of two main parts (bedtime and waketime) and 21 sub items in total that were developed to subjectively measure daily sleep quality. Daily events other than sleep were at night in the bedtime part of the diary and the wake time part to be completed just after waking from sleep29.
Work related questionnaires
In addition to the subjective measurements of sleep and mood, a number of questions were asked during the day including “What was your current shift type: night/day/afternoon/on call/rest day?” “Start and end times for shift/break time and duration”, “How many hours did you spend driving for work purposes?” and “Have you encountered any significant events during the day?”.
Procedure
Participants were invited to take part in this study after completing a previous anonymous survey30. Fifteen paramedics initially accepted to participate in the study out of the 276 invitations. However three participants were excluded due to missing data of either actigraphy or diaries, leaving 12 participants (response rate 4.3%). After obtaining informed consent, participants received the BSA, actigraphy, and sleep and work diaries via post with a prepaid return envelope for returning the devices and diaries at the end of the study. Paramedics were asked to wear the BSA and the actigraphy on their non-dominant arm for a period of eight consecutive days, starting on the day before their new shift cycle to objectively record their stress and sleep (Fig. 1). During that time, participants were asked to complete the sleep diary twice a day (before sleep and after waking) and a customized work diary three times a day (before, during, and after work, or equivalent time on days off). The study investigated paramedics across five time points within their rotating shift schedules including pre-shift day, standard day shifts, night shift/s, days off one and two. Data collection started 24 h before the beginning of the shift cycle and finished 3 days after the shift ended.
Statistical analyses
The data were analyzed using the Statistical Package for the Social Sciences (SPSS) version 24. Data distributions were adequate in terms of normality, linearity, and homoscedasticity. The data were also tested for outliers, missing values, and data entry errors. Data cleaning led to the elimination of three participants due to missing data of either actigraphy or diaries, leaving a final sample of 12 participants. Also, day shift 2, night shift 2 and day off 3 were excluded from the analysis as only 5 of the 12 remaining participants completed these days. One-way repeated measures ANOVA were used to determine the effects of shift period schedule (pre-shift; day shift 1; night shift 1; days off 1 and 2) on sleep, physical activity, GSR, energy expenditure, sleepiness, fatigue, mood, and stress. Post hoc testing was done using the Bonferroni correction. All study outcomes were measured during an entire 24-h period for each time point (e.g., total sleep time during night shift equals sleep during the entire 24-h (from 07:00 to 07:00 h) including any napping opportunity during work or outside work).
Results
A total of 12 paramedics with complete data were included in the final data set. All paramedics were working on a rotating shift schedule. The mean age was 39.5 years (SD = 10.7 years), and there was a total of five men and seven women. The mean BMI was 24.5 (SD = 3.4).
Sleep and sleepiness
The average total sleep time (TST; hours) that was recorded from the current sample during the entire 24-h for each day was as follows: pre-shift (M = 6.6, SD = 1.4), day shift 1 (M = 7.2, SD = 1.1), day shift 2 (M = 6.4, SD = 2.2), night shift 1 (M = 3.8, SD = 1.5), night shift 2 (M = 4.3, SD = 2.0), day off 1 (M = 7.2, SD = 1.1), day off 2 (M = 7.4, SD = 2.2) and day off 3 (M = 7.1, SD = 1.4). During night shift 1 (Day 4), five out of the 12 paramedics napped an average of 2.5 h before the beginning of night duty (daytime sleep) and the rest of sleep time was recorded during the night shift itself. The remaining participants (n = 7) slept during the night shift 1. During night shift 2 (Day 5), only one out of five slept during the day for only 1 h, while the rest slept on shift.
A repeated measures ANOVA determined that mean TST differed significantly across the five time points in the rotating shift schedule, [F(2.06, 22.29) = 12.37, p < 0.001; η2 = 0.51]. Post hoc tests using the Bonferroni correction revealed that there was significantly less TST during the night shift 1 compared to pre-shift (M = 3.8, SD = 1.5 h vs. M = 6.6, SD = 1.4 h, p < 0.001). During the night shift 1, TST was also significantly lower in comparison to day shift 1 (p < 0.05), day off 1 (p < 0.05) and day off 2 (p < 0.05) (Fig. 2A).
The (A) total sleep time in hours (daytime naps included), (B) time in bed in hours, (C) number of awakenings, and (D) WASO measured by actigraphy during a rotating shift schedule across 5-time points within the schedule starting from (1) pre-shift, (2) day shift one, (3) night shift one, (4) day off one, and (5) day off two. Note, *(A) night shift one significantly lower than all days (p < 0.001), (B) night shift one significantly lower than all days (p < 0.05), (C) day off one significantly higher than night shift one (p < 0.05), and (D) day off one significantly higher than night shift one (p < 0.05). **(WASO) wake after sleep onset.
Similarly, the mean time in bed (TIB) differed significantly across the five time points in the rotating shift schedule [F(2.00, 16.01) = 10.18, p < 0.05; η2 = 0.50]. Post hoc tests revealed that there was a significant reduction in TIB during the night shift 1 compared to pre-shift (M = 4.1, SD = 0.5 h vs. M = 7.3, SD = 0.5 h, p < 0.001). In addition, during the night shift 1, the TIB was significantly less than the day shift 1 (p < 0.05), day off 1 (p < 0.05) and day off 2 (p < 0.05) (Fig. 2B).
The mean number of times awakened during sleep differed significantly among the five time points in the rotating shift schedule [F(2.52, 20.14) = 4.736, p < 0.05 η2 = 0.278]. Post hoc tests revealed that the number of awakenings was significantly higher on day off 1 (M = 33.8, SD = 3.1; p < 0.05) as compared to the night shift 1 (M = 15.4, SD = 2.0) (Fig. 2C).
WASO differed significantly among the five time points in the rotating shift schedule [F(2.732, 21.85) = 3.93, p < 0.05; η2 = 0.23]. Post hoc tests revealed that WASO was significantly higher on day off 1 (M = 57.3, SD = 7.1 min; p < 0.05) in comparison to night shift 1 (M = 22.6, SD = 3.2 min) (Fig. 2D). There were no significant differences observed between the shift time points for the sleep efficiency and onset latency variables.
The sleepiness score (before-work levels during work days or morning levels during non-work days) was significantly different across the rotating shift schedule [F(2.611, 20.887) = 4.10, p < 0.05; η2 = 0.25]. Post hoc tests showed significantly higher scores of sleepiness for day off 1 compared to day off 2 (p < 0.05) (Fig. 3A).
The sleepiness level reported (A) before work, (B) during work, and (C) after work during a rotating shift schedule across 5-time points within the schedule starting from (1) pre-shift, (2) day shift one, (3) night shift one, (4) day off one, and (5) day off two. Note, *(A) day off one significantly higher than day off two (p < 0.05), (B) night shift one and day off one significantly higher than pre shift (p < 0.05), and (C) night shift one and day off one significantly higher than pre-shift and day off two (p < 0.05).
The sleepiness score (during-work levels on work days or afternoon levels during non-work days) differed significantly across the rotating shift schedule [F(2.70, 21.61) = 5.28, p < 0.05; η2 = 0.33]. Post hoc tests showed significantly higher scores of sleepiness on night shift 1 and day off 1 compared to pre-shift (p < 0.05) (Fig. 3B).
The sleepiness score (after-work levels during work days or evening levels during non-work days) was significantly different across the rotating shift schedule [F(2.88, 23.11) = 14.34, p < 0.001; η2 = 0.54]. Post hoc tests showed significantly higher scores of sleepiness during the night shift 1 as compared to pre-shift (p < 0.05). Also, sleepiness scores were significantly higher during the night shift 1 and day off 1 compared to day off 2 (p < 0.05) (Fig. 3C).
Mood, stress and fatigue
The average positive and negative affect scores on the abbreviated 8-item PANAS were recorded from the current sample twice during the entire 24-h for each day. The results were as follows (before and after work): pre-shift [positive M = 8.2 (1.2) and M = 9.7 (1.6), negative M = 5.2 (0.5) and M = 6.4 (1.8)], day shift 1 [positive M = 10.7 (1.4) and M = 9.4 (1.2), negative M = 4.9 (0.4) and M = 5.4 (0.3)], night shift 1 [positive M = 11.0 (1.5) and M = 7.7 (1.4), negative M = 4.7 (0.4) and M = 5.1 (0.5)], day off 1 [positive M = 9.0 (1.6) and M = 8.4 (1.2), negative M = 6.0 (0.7) and M = 6.9 (1.5)], and day off 2 [positive M = 9.8 (1.3) and M = 7.6 (1.5), negative M = 5.4 (0.6) and M = 5.9 (0.7)]. A repeated measures ANOVA determined that mean positive and negative affect scores on the PANAS did not differed significantly across the five time points in the rotating shift schedule: positive affect (before work): [F(2.24, 15.70) = 1.43, p = 0.26; η2 = 0.07], positive affect (after work): [F(3.05, 21.35) = 1.25, p = 0.32; η2 = 0.05], negative affect (before work): [F(2.50, 17.54) = 1.27, p = 0.31; η2 = 0.08], and negative affect (after work): [F(1.32, 9.30) = 0.57, p = 0.51; η2 = 0.04].
Stress (before-work levels during work days or morning levels during non-work days) differed significantly among the rotating shift schedule [F(2.78, 22.21) = 8.21, p < 0.05; η2 = 0.45]. Post hoc tests revealed significantly higher levels of stress on day off 1 compared to pre-shift (p < 0.05) and day shift 1 (p < 0.05) (Fig. 4A).
The stress level reported (A) before work, (B) during work, and (C) after work during a rotating shift schedule across 5-time points within the schedule starting from (1) pre-shift, (2) day shift one, (3) night shift one, (4) day off one, and (5) day off two. Note, *(A) day off one significantly higher than pre-shift and day shift one (p < 0.05), (B) day off one significantly higher than pre-shift and day shift one (p < 0.05), and (C) night shift one and day off one significantly higher than all other days (p < 0.001).
Likewise, stress (during-work levels on work days or afternoon levels during non-work days) differed significantly across the rotating shift schedule [F(2.92, 23.35) = 8.43, p < 0.05; η2 = 0.44]. Post hoc tests revealed significantly higher levels of stress on day off 1 as compared to pre-shift (p < 0.05) and day shift 1 (p < 0.05) (Fig. 4B).
Stress (after-work levels during work days or evening levels during non-work days) differed significantly across the rotating shift schedule [F(2.19, 17.54) = 16.85, p < 0.001; η2 = 0.63]. Post hoc tests revealed significantly higher levels of stress on the night shift 1 as compared to pre-shift (p < 0.05) and day off 2 (p < 0.05). Also, the stress level for day off one was significantly higher than pre-shift (p < 0.05), day shift 1 (p < 0.05), and day off 2 (p < 0.05) (Fig. 4C).
The fatigue score (before-work levels during work days or morning levels during non-work days) was not significantly different across the rotating shift schedule (p = 0.06; η2 = 0.20). However, post hoc tests showed significantly higher scores of fatigue for day off 1 in comparison to pre-shift (p < 0.05) (Fig. 5A).
The fatigue level reported (A) before work, (B) during work, and (C) after work during a rotating shift schedule across 5-time points within the schedule starting from (1) pre-shift, (2) day shift one, (3) night shift one, (4) day off one, and (5) day off two. Note, *(A) day off one significantly higher than pre-shift (p < 0.05), (B) night shift one and day off one significantly higher than pre-shift (p < 0.05), and (C) day shift one, night shift one and day off one significantly higher than pre-shift and day off two (p < 0.05).
The fatigue score (during-work levels on work days or afternoon levels during non-work days) was significantly different across the rotating shift schedule [F(3.10, 24.78) = 8.50, p < 0.001; η2 = 0.38]. Post hoc tests showed significantly higher scores of fatigue during the night shift 1 and day off 1 as compared to pre-shift (all p < 0.05) (M = 2.11, SD = 0.26) (Fig. 5B).
Fatigue levels (after-work levels during work days or evening levels during non-work days) also differed significantly across the rotating shift schedule [F(3.18, 25.450) = 20.450, p < 0.001; η2 = 0.66]. Post hoc tests revealed significantly higher scores of fatigue on the night shift one compared to pre-shift (p < 0.05), day shift one (p < 0.05), and day off 2 (p < 0.05). In addition, fatigue levels were significantly higher on day off 1 compared to pre-shift (p < 0.05) and day off 2 (p < 0.05). Also, fatigue levels were significantly higher on the day shift 1 compared to the same time on day off 2 (p < 0.05) (Fig. 5C).
Physical activity
Data from the SenseWear are displayed in Table 1. The mean physical activity, measured by step count, differed significantly among the five time points in the rotating shift schedule [F(2.59, 23.26) = 1.40, p < 0.05; η2 = 0.37]. Post hoc tests showed that physical activity was significantly greater (p < 0.05) on the night shift 1 when compared to pre-shift. However, the average GSR and total energy expenditure were not statistically different across the time points in the shift schedule.
Discussion
This field study investigated paramedics across an entire rotating shift schedule, starting with the pre-shift day, day shift, night shift, and 2 days off. The study investigated sleep (actigraphy and PSD), physical activity (BSA), total energy expenditure (BSA), mood (PANAS), sleepiness (KSS), fatigue (Samn–Perelli Fatigue Checklist), and stress (BSA and a self-reported stress scale). The actigraphy data revealed significantly less TST during the night shift one when compared to the pre-shift day, day shift one, and days off. The number of awakenings and WASO were significantly higher during day off one compared to the night shift. Sleep efficiency and onset sleep latency were not significantly different across the rotating shift schedule. However, paramedics reported significantly higher levels of sleepiness and fatigue during and after the night shift, and across day off one, as compared to pre-shift and the second day off. Levels of stress yielded a similar trend, as paramedics reported significantly higher stress during and after the night shift, and across day off one, when compared to pre-shift, day shift one, and day off two. Significantly more physical activity, measured by step count, was observed during the night shift as compared to pre-shift. Total energy expenditure, GSR (stress) and mood did not change significantly during the rotating shift schedule.
During the first night shift, the paramedics recorded an average of 3.8 h of TST, which was significantly less than the pre-shift day, day shift, and days off. It is plausible that since many of these paramedics were only working one night shift and were transitioning to off days following this shift, they did not attempt to obtain a full 7–8 h of sleep during this period. Five of the paramedics were rostered to a second night shift (Day 5), and recorded slightly more sleep after the night shift, with an average TST of 4.3 h, which is still considerably lower than reported in other shift worker populations. For example, nurses in the United States17 and Japan31 slept an average of 5.2 h after working a night or evening shift. However, airline ground crew slept an average of 4.3 h after the night shift, which is similar to what was recorded from our study32. Even under ideal conditions, simulated night shift studies have shown that sleep after a night shift is severely truncated, which is likely due to the impact of circadian processes in the early afternoon disrupting sleep33. The recorded TST in our sample of paramedics reflects a period of severe sleep restriction after night shift day that was also shorter than the TST measured in other shift worker populations17,31,32. While it should be noted that this was only in a small number of paramedics in our sample, it does raise concerns given the known impact of sleep restriction on decision making and cognitive functioning more generally34.
Other sleep parameters measured by the actigraphy were WASO and the number of awakenings, which were both significantly higher during the first day off compared to night duty. Although not significant, but still considerably high, WASO and the number of awakenings were recorded during the second day off compared to pre-shift measurements. In a previous study using actigraphy, a higher WASO was found a day after working an afternoon shift among midwives35. Also, nurses working evening shifts scored higher WASO compared to non-shift workers31. A greater number of awakenings were reported by rotating shift workers, especially following a shift change, in comparison to workers with fixed shifts36. It seems that paramedics and shift workers from different cohorts share a common sleep pattern where a high WASO and number of awakenings were recorded primarily after night duty or a shift change. Higher WASO and number of awakenings indicates sleep fragmentation which can be an indicator of elevated stress37,38. It is also likely to be the result of unstable and disrupted circadian rhythms, from rapidly switching between day and night schedules. This is one of the adverse effects of working rotating shifts and switching from night to day sleep and back to night sleep every week.
The levels of stress, fatigue, and sleepiness were significantly higher during days off as compared to pre-shift measurements. It is plausible that the restricted sleep during night duty (3.8–4.3 h) contributed to the increases in stress, fatigue, and sleepiness during this time. Previous studies have linked sleep restriction with stress in physicians and nurses39,40. In fact, a study that restricted sleep in a laboratory found that a shorter duration of sleep was strongly related to higher levels of stress41. Also, fatigue and sleepiness were strongly linked to shorter TSTs in nurses, physicians, and airline ground crew17,31,32,42,43. Although the signs of stress, fatigue, and sleepiness were not significantly higher during the second day off when compared to other time points, the levels were still considerably high especially in the beginning and in the middle of day off two compared to pre-shift. In nurses, the signs of stress and fatigue continued beyond night duty, as they reported significant signs of fatigue and stress during 2 days off work after night duty44. Also, airline cabin crew reported significant signs of sleepiness for 2 days after the end of the shift45. The findings of the current study are consistent with previous findings, where subjective levels of stress, fatigue, and sleepiness are impacted by a shorter sleep duration. The effect continues to impact workers during off days, and the levels were still considerably high 1–2 days after the end of the shift.
The level of physical activity, which was measured by step count, was significantly higher during night duty compared to pre-shift. However, rotating shift workers from Japan reported significantly higher physical activity during day compared to night shifts16. Another recent report compared day and night shift healthcare workers indicated no differences in physical activity as measured for 24-h period for both groups46. While more steps count or physical activity typically represent a healthy lifestyle, in the present study, this finding is probably due to the extended awake time and less rest/nap opportunities for paramedics during night duty. It may lead to fatigue and exhaustion, thus impacting their performance or safety47. Despite the fact that more physical activity is linked to better well-being and mental health as well as less fatigue in the general population48, engaging in more physical activity while working against the normal body clock may lead to physical exhaustion49.
The mood of the participants was measured by the PANAS and did not show significant changes across the shift schedule. This finding suggests that a rotating shift has no relationship with the paramedics’ mood. The mood issues reported by previous studies in paramedics may be due to the cumulative effect of shift work2,30,50,51. Based on the findings from the current sample of paramedics, a rotating shift may be related to sleep duration, stress, fatigue, and sleepiness levels but not mood.
In addition to the relationship with stress and fatigue, lack of sleep has been associated with a decline in cognitive function, judgment, and decision-making52. In fact, less than 4 h of TST during night shift simulated in a laboratory was linked to significant deficits in cognitive function when compared to groups that slept more than 5 h, suggesting a dose–response relationship between sleep duration and performance53. Certainly, cognitive functions and performance are two of the most important abilities for healthcare shift workers, especially paramedics. Any deficits in those abilities can compromise the safety of both the workers and their patients. Future studies should focus on assessing paramedics’ performance and cognition during shift work and on off days as well.
Recovery from shift work is crucial in maintaining worker’s health54. The current rotating shift schedule for paramedics in Victoria, Australia includes 2 days of standard day shifts followed by 2 days of night shifts and then 4 days off work or recovery in-between every other roster. The amount of recovery needed in-between shifts may differ from one group of workers to another, as nurses from a recent report required at least 3 days of recovery44. Non-shift workers usually require no longer than 2 days to recover55. Also, the duration of work is an important factor in determining the amount of recovery56, as longer working hours are attributed to the need for longer recovery times57. Outcomes of the present study seem to show improvement from day off 2, although not to pre-shift levels. The current study did not assess these outcomes beyond day off 2, therefore we do not know if 4 days of recovery is sufficient for sleep, mood and stress to return to pre-shift levels in this population. Future studies should focus on days where shift workers required to change their sleep habits, starting from night shifts until the second or third day of recovery after night work, as these appear to be the most challenging days for them.
Fixed shifts would be a solution that avoids the problems of continually having to adjust between different shifts. This could be done on the basis of assigning people to shifts based on their chronotype58. Chronotype was assessed in 136 ambulance workers and found that while it would be possible to staff the day shift, there would always be a shortage of staff that are true evening type to staff the night shift (evening types = 11%)30. It may be difficult to fill workers into a fixed night shift, but it would be advantageous because they only have to adapt to a fixed work schedule and any difficulties in adjusting would result from social demands that may conflict with their permanent shift schedules59. Fixed night shift is detrimental to health and fixed day shift is not possible in some essential services that require 24 h coverage e.g. police, paramedics. Thus, rotating shifts have been adopted.
The present study assessed paramedics through their entire rotating roster and off days using wrist actigraphy to record their sleep and objective information regarding physical activity and subjective levels of stress, fatigue, and sleepiness. Sample size was not large enough to conduct further analyses to investigate the outcomes of the study during the day shift 2, night shift 2 and day off 3. However, from the observed TST during night shift 2, we can speculate similar outcomes to what found during night shift 1. Although our sample size was small, this was due to the intensive assessment of day-to-day data in the field. Further studies in larger samples of paramedics are required to confirm the current findings.
Being a field study, the shift comparisons were restricted by the shifts that were running, with night shifts being 4 h longer than day shift. Ideally, a comparison of shifts of equal duration would be best from an experimental perspective, however it could be argued that these results have ecological validity, reflecting outcomes from shift schedules used in the industry.
This study did not assess employment history, which may be a relevant factor related to these findings, as newly recruited paramedics may react differently than paramedics with experience to rotating shift conditions. The subjective stress rating used was a single question assessing the current state of stress, and it has not been previously validated. In addition, the study did not investigate whether the pre-shift day represented day off 4 from a previous shift or another day (e.g., last day of a vacation).
Although the current study was sufficiently powered to reveal statistically significant findings, with moderate to high effect sizes, the sample size was small (n = 12). Additionally, within this small sample there was a considerable amount of missing data. Thus, the self-reported measures used in the study may be particularly prone to a response bias. However, this data was sampled from first-response paramedics in a highly stressful and demanding work environment, where lives can be at risk. Therefore, we believe such study conditions are highly susceptible to missing data.
In conclusion, this study investigated paramedics across a single rotation of their shift schedule, including two off days. The duration of sleep measured using actigraphy was significantly less during night duty when compared to pre-shift, day shift, and off days one and two. The levels of stress, fatigue, and sleepiness were all related to the sleep restriction that happened during night duty. These levels started to increase significantly after the end of the night duty and peaked significantly throughout day off one. The highest level of physical activity was detected during 24 h periods that included night shift. During these periods paramedics may be at risk of physical fatigue and exhaustion. Therefore, it was observed that working on a rotating shift was associated with sleep restriction, higher stress, fatigue, and sleepiness levels, which together may be detrimental to a worker’s health. Given these preliminary results, there is a need to investigate methods to reduce rotating shift burden on health with a particular focus on night shifts and days off.
References
National Sleep Foundation, What is Shift Work? https://sleepfoundation.org/shift-work/content/what-shift-work (2017).
Courtney, J. A., Francis, A. J. & Paxton, S. J. Caring for the country: Fatigue, sleep and mental health in Australian rural paramedic shiftworkers. J. Commun. Health 38, 178–186 (2013).
Costa, G. Shift work and health: Current problems and preventive actions. J. Saf. Health Work 1, 112–123 (2010).
Knauth, P. The design of shift systems. J. Ergonom. 36, 15–28 (1993).
Alward, R. R. & Monk, T. H. A comparison of rotating-shift and permanent night nurses. J. Int. J. Nurs. Stud. 27, 297–302 (1990).
Akerstedt, T. & Wright, K. P. Sleep loss and fatigue in shift work and shift work disorder. J. Sleep Med. Clin. 4, 257–271 (2009).
Ganesan, S. et al. The impact of shift work on sleep, alertness and performance in healthcare workers. J. Sci. Rep. 9, 4635–4635 (2019).
Angerer, P. et al. Night work and the risk of depression. J. Deutsches Arzteblatt Int. 114, 404–411 (2017).
Ma, C. C. et al. Shift work and occupational stress in police officers. J. Saf. Health Work 6, 25–29 (2015).
Ramin, C. et al. Night shift work at specific age ranges and chronic disease risk factors. J. Occup. Environ. Med. 72, 100 (2015).
Chatterjee, K. & Ambekar, P. Study of insomnia in rotating shift-workers. Ind. Psychiatry J. 26, 82–85 (2017).
Lin, P. C. et al. The association between rotating shift work and increased occupational stress in nurses. J. Occup. Health. 57, 307–315 (2015).
Vangelova, K. The effect of shift rotation on variations of cortisol, fatigue and sleep in sound engineers. J. Ind. Health 46, 490–493 (2008).
De Bacquer, D. et al. Rotating shift work and the metabolic syndrome: A prospective study. Int. J. Epidemiol. 38, 848–854 (2009).
Kalmbach, D. A. et al. Shift work disorder, depression, and anxiety in the transition to rotating shifts: The role of sleep reactivity. J. Sleep Med. 16, 1532–1538 (2015).
Kawada, T. et al. Activity and sleeping time monitored by an accelerometer in rotating shift workers. J. Work 30, 157–160 (2008).
Geiger-Brown, J. et al. Sleep, sleepiness, fatigue, and performance of 12-hour-shift nurses. J. Chronobiol. Int. 29, 211–219 (2012).
Choi, S. J. & Joo, E. Y. Light exposure and sleep–wake pattern in rapidly rotating shift nurses. J. Sleep Med. 13, 8–14 (2016).
Zverev, Y. P. & Misiri, H. E. Perceived effects of rotating shift work on nurses’ sleep quality and duration. Malawi Med. J. 21, 19–21 (2009).
Hegg-Deloye, S. et al. Current state of knowledge of post-traumatic stress, sleeping problems, obesity and cardiovascular disease in paramedics. Emerg. Med. J. 31, 242 (2014).
Sharif, M. M. & BaHammam, A. S. Sleep estimation using BodyMedia’s SenseWear™ armband in patients with obstructive sleep apnea. J. Ann. Thorac. Med. 8, 53–57 (2013).
Perala, C. & Sterling, B. Galvanic Skin Response as a Measure of Soldier Stress (ed. Perala, P.) 20–25 (Army Research Laboratory, Adelphi, 2007).
Morgenthaler, T. et al. Practice parameters for the use of actigraphy in the assessment of sleep and sleep disorders: An update for 2007. J. Sleep. 30, 519–529 (2007).
Kushida, C. A. et al. Comparison of actigraphic, polysomnographic, and subjective assessment of sleep parameters in sleep-disordered patients. J. Sleep Med. 2, 389–396 (2001).
Akerstedt, T. & Gillberg, M. Subjective and objective sleepiness in the active individual. Int. J. Neurosci. 52, 29–37 (1990).
Watson, D., Clark, L. A. & Tellegen, A. Development and validation of brief measures of positive and negative affect: The PANAS scales. J. Person. Soc. Psychol. 54, 1063–1070 (1988).
Zohar, D. et al. The effects of sleep loss on medical residents’ emotional reactions to work events: A cognitive-energy model. J. Sleep. 28, 47–54 (2005).
Samn, S. & Perelli, L. Estimating Aircrew Fatigue: A Technique with Application to Airlift Operations (ed. Samn, S.) 29–33 (PN, 1982).
Monk, T. H. et al. The Pittsburgh sleep diary. J. Sleep Res. 3, 111–120 (1994).
Khan, W. A. et al. The relationship between shift-work, sleep and mental health among paramedics in Australia. J. Natl. Sleep Found. 6, 330–337 (2020).
Kato, C., Shimada, J. & Hayashi, K. Sleepiness during shift work in Japanese nurses: A comparison study using JESS, SSS, and actigraphy. J. Sleep Biol. Rhythms 10, 109–117 (2012).
Shochat, T. et al. Burnout, sleep, and sleepiness during day and night shifts in transition from 8- to 12-hour shift rosters among airline ground crew managers. J. Clocks Sleep. 1, 226–239 (2019).
Jackson, S., Banks, S. & Belenky, G. Investigation of the effectiveness of a split sleep schedule in sustaining sleep and maintaining performance. J. Chronobiol. Int. 31, 1218–1230 (2014).
Lowe, C. J., Safati, A. & Hall, P. A. The neurocognitive consequences of sleep restriction: A meta-analytic review. J. Neurosci. Biobehav. Rev. 80, 586–604 (2017).
Tremaine, R. et al. Actigraph estimates of the sleep of Australian midwives: the impact of shift work. J. Biol. Res. Nurs. 15, 191–199 (2013).
Ohayon, M. M. et al. Prevalence and consequences of sleep disorders in a shift worker population. J. Psychosom. Res. 53, 577–583 (2002).
Shrivastava, D. et al. How to interpret the results of a sleep study. J. Community Hosp. Internal Med. Perspect. 4, 24983 (2014).
Åkerstedt, T., Kecklund, G. & Axelsson, J. Impaired sleep after bedtime stress and worries. J. Biol. Psychol. 76, 170–173 (2007).
Morales, J. et al. Stress and autonomic response to sleep deprivation in medical residents: A comparative cross-sectional study. J. PLoS One. 14, e0214858–e0214858 (2019).
Owens, J. A. Sleep loss and fatigue in healthcare professionals. J. Perinat. Neonatal. Nurs. 21, 92–100 (2007).
Liu, J. C. et al. Sleep deprived and sweating it out: The effects of total sleep deprivation on skin conductance reactivity to psychosocial stress. J. Sleep. 38, 155–159 (2015).
Stanojevic, C., Simic, S. & Milutinovic, D. Health effects of sleep deprivation on nurses working shifts. J. Med. Pregl. 69, 183–188 (2016).
Papp, K. K. et al. The effects of sleep loss and fatigue on resident–physicians: A multi-institutional, mixed-method study. J. Acad. Med. 79, 394–406 (2004).
Haluza, D., Schmidt, V. M. & Blasche, G. Time course of recovery after two successive night shifts: A diary study among Austrian nurses. J. Nurs. Manag. 27, 190–196 (2019).
Åkerstedt, T. et al. Sleepiness and days of recovery. J. Traffic Psychol. Behav. 3, 251–261 (2000).
van de Langenberg, D. et al. Diet, physical activity, and daylight exposure patterns in night-shift workers and day workers. Ann. Work Expo Health 63, 9–21 (2019).
Barker, L. M. & Nussbaum, M. A. Fatigue, performance and the work environment: A survey of registered nurses. J. Adv. Nurs. 67, 1370–1382 (2011).
Yuenyongchaiwat, K. Effects of 10,000 steps a day on physical and mental health in overweight participants in a community setting: A preliminary study. Braz. J. Phys. Ther. 20, 367–373 (2016).
Reilly, T. & Waterhouse, J. Sports performance: Is there evidence that the body clock plays a role?. Eur. J. Appl. Physiol. 106, 321–332 (2009).
Courtney, A. J., Francis, P. & Paxton, S. J. Caring for the carers: Fatigue, sleep, and mental health in Australian Paramedic Shiftworkers. Aust. N. Z. J. Organ. Psychol. 3, 32–41 (2010).
Sofianopoulos, S. et al. The exploration of physical fatigue, sleep and depression in paramedics: A pilot study. Aust. J. Paramed. 9, 2202–7270 (2011).
Luber, B. et al. Extended remediation of sleep deprived-induced working memory deficits using fMRI-guided transcranial magnetic stimulation. J. Sleep. 36, 857–871 (2013).
Belenky, G. et al. Patterns of performance degradation and restoration during sleep restriction and subsequent recovery: A sleep dose–response study. J. Sleep Res. 12, 1–12 (2003).
Merkus, S. L. et al. Self-reported recovery from 2-week 12-hour shift work schedules: A 14-day follow-up. Saf. Health Work 6, 240–248 (2015).
Smith, L. et al. Weekday and weekend patterns of objectively measured sitting, standing, and stepping in a sample of office-based workers: The active buildings study. BMC Public Health 15, 9 (2015).
Wong, K., Chan, A. H. S. & Ngan, S. C. The effect of long working hours and overtime on occupational health: A meta-analysis of evidence from 1998 to 2018. Int. J. Environ. Res. Public Health 16, 2102 (2019).
Ropponen, A. et al. The vicious circle of working hours, sleep, and recovery in expert work. Int. J. Environ. Res. Public Health 15, 1660–4601 (2018).
Vetter, C. et al. Aligning work and circadian time in shift workers improves sleep and reduces circadian disruption. J. Curr. Biol. 25, 907–911 (2015).
Silva, B. et al. Twelve-hour night shifts of healthcare workers: A risk to the patients?. Chronobiol. Int. J. 20, 351–360 (2003).
Author information
Authors and Affiliations
Contributions
W.K. was involved in conceptualizing, design, data collection, data analysis and wrote the manuscript. R.C.,G.K. and M.J. were involved in conceptualizing and designing the study, data analysis and reviewed and revised the manuscript. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Khan, W.A.A., Jackson, M.L., Kennedy, G.A. et al. A field investigation of the relationship between rotating shifts, sleep, mental health and physical activity of Australian paramedics. Sci Rep 11, 866 (2021). https://doi.org/10.1038/s41598-020-79093-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-79093-5
This article is cited by
-
Effectiveness of gamified team competition as mHealth intervention for medical interns: a cluster micro-randomized trial
npj Digital Medicine (2023)
-
Physical Activity and Mortality in Patients with Coronary Artery Disease
Current Cardiology Reports (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.