Abstract
Since the introduction of leukemia-type induction therapies for T-cell lymphoblastic lymphoma (T-LBL), improvements in the long-term outcomes of T-LBL have been reported. However, indications for and the appropriate timing of hematopoietic stem cell transplantation (HSCT) have not yet been established. Therefore, we performed a multicenter retrospective cohort study of patients with T-LBL treated using leukemia-type initial therapies to compare the outcomes after HSCT at different disease stages. We enrolled 21 patients with T-LBL from a total of 11 centers, and all patients received hyper-CVAD as a leukemia-type initial regimen. HSCT was performed during the CR1/PR1 (standard disease) stage in 11 patients, while it was completed at a later or non-remission (advanced disease) stage in 10 patients. Following HSCT, the overall survival rate was significantly greater in standard disease than in advanced-disease patients (79.5% vs. 30.0% at 5 years; hazard ratio (HR) 5.97; p = 0.03), with trend to the lower incidence of relapse in the former group (27.3% vs. 60.0% at 5 years; HR 2.29; p = 0.19). A prognostic difference was not detected between cases treated with allogeneic and autologous HSCTs. Our study suggests that frontline HSCT may be a feasible treatment option for T-LBL, even in the era of leukemia-type initial therapy.
Similar content being viewed by others
Introduction
T-cell lymphoblastic lymphoma (T-LBL) is a rare hematological malignancy that is characterized by mediastinal lesions with minimal bone marrow infiltration1,2,3. Despite its known cellular origin in lymphoblasts, T-LBL is distinguished from acute lymphoblastic leukemia (ALL) due to its distinct clinical presentation involving predominant mass lesions and infrequent bone marrow infiltration (blasts < 20%)4, instead demonstrating clinical features more similar to those of non-Hodgkin’s lymphoma (NHL). Therefore, NHL-type chemotherapeutic regimens have previously been chosen as initial therapies in patients with T-LBL, but unlike in normal NHL cases, upfront hematopoietic stem cell transplantation (HSCT) was also often recommended in order to suppress late-phase relapse and promote more favorable outcomes5,6.
Recently, ALL-type regimens including hyper CVAD (composed of fractionated cyclophosphamide, vincristine, doxorubicin, and dexamethasone) and high-dose cytarabine combined with methotrexate have been standardized as the new initial therapies for T-LBL based on studies reporting higher remission and lower relapse rates in the early phase7. However, under this novel ALL-type initial therapy approach, the indication and appropriate timing of HSCT, if necessary, remain unestablished because the validity of the risk stratification system for relapse after chemotherapies is not confirmed2,8, and moreover, the beneficial effects of HSCT have not yet been evaluated according to each disease status of T-LBL9,10,11.
Therefore, we performed the present multicenter retrospective cohort study of patients with T-LBL treated with ALL-type initial therapies to (1) determine the risk factors for relapse after ALL-type chemotherapies in patients with T-LBL, and (2) compare the outcomes after HSCT performed at different time points and in patients with different disease statuses. Further, this study may provide information helpful in determining the optimal treatment approach to use to attain more favorable outcomes among patients with T-LBL in the current ALL-type therapy era.
Subjects and methods
Inclusion criteria
Data on adult patients (age ≥ 16 years) who underwent their first HSCT between January 2000 and September 2016 at hospitals of the Kyoto Stem Cell Transplantation Group (KSCTG) were obtained through the Japanese Transplant Registry Unified Management Program (TRUMP), which is sponsored by the Japanese Society for Hematopoietic Cell Transplantation and Japanese Data Center for Hematopoietic Cell Transplantation12. We included HSCT-eligible patients who fulfilled the following World Health Organization 2016 criteria for T-LBL4. The study protocol complied with the standards outlined in the Declaration of Helsinki and was approved by the ethical committee of Kyoto University (R-1507). Written informed consent was obtained from each patient or from a parent and/or legal guardian in case of patients below 18 years of age.
Data collection and definition of each covariate
We extracted data from the KSCTG database on basic pretransplant characteristics and the posttransplant clinical course. We also reviewed the medical records and extracted the data available there and discerned the HSCT characteristics and posttransplant clinical course details according to the predefined standardized protocol. The clinical stage was determined according to the Ann Arbor system, with the initial evaluation of bone marrow for all the patients being mandatory. The overall disease risk was calculated using the International Prognostic Index (IPI) at diagnosis. Treatment responses, including relapse, were evaluated according to the Cheson criteria13. The disease status at the time of HSCT was categorized as standard and advanced disease; the prior encompassed patients transplanted at CR1 or PR1 status, while the latter included those transplanted at CR2/PR2 or later, primary induction failure (PIF), or stable (SD) or progressive disease (PD) after the consequences of any chemotherapy. Regarding conditioning regimens, myeloablative conditioning (MAC) and reduced-intensity conditioning (RIC) were defined based on the previously published consensus criteria14.
Statistical analyses
Patient characteristics were compared between the standard- and advanced-disease groups using Fisher’s exact tests for categorical variables and the Mann–Whitney U test for continuous variables. For survival analysis, the overall survival (OS) was measured from the date of diagnosis or HSCT to the last follow-up visit; survival curves were described using the Kaplan–Meier method, and the groups were compared using the log-rank test. Cumulative incidence curves for non-relapse mortality (NRM) and relapse were compared using the Gray test, treating relapse and NRM as competing risks, respectively. For the statistical analysis of these prognostic factors, we employed Cox proportional-hazards regression model and the Fine–Gray proportional-hazards models15. Multivariate analyses included those variables showing the significance (or clinically relevant) in the preceding univariate analyses, and the number of variables in the model was restricted to one per 5–10 events. All statistical analyses were performed using the R statistical software program, version 3.6.1 (R Foundation for Statistical Computing, Vienna, Austria). All p-values are two-sided, and p < 0.05 was considered to be statistically significant.
Results
Patient characteristics
From the total cohort of 2,425 patients, we chose 82 patients categorized as precursor lymphoid neoplasms, finally enrolling a total of 21 patients with T-LBL who received HSCT in a total of 11 centers. The median age at the time of diagnosis was 34 (range 17–54) years (Table 1). The clinical stage at diagnosis ranged from III to IV in 18 patients (85.7%); 13 patients (61.9%) possessed mediastinal lesions, while bone marrow involvement was confirmed in 9 patients (42.9%). The performance status (PS) was 1 or less in 13 patients (61.9%). Meanwhile, the IPI score was 3 or greater (high risk) in 10 patients (47.6%). Other notable patient characteristics at diagnosis are included in Table 1.
Pre-transplant initial treatments
The pretransplant clinical course is summarized in Fig. 1. All patients received ALL-type initial regimens composed of hyper-CVAD or its derivatives [i.e., the addition of cytarabine, 6-mercaptopurine, and/or L-asparaginase (L-ASP)] with or without high-dose methotrexate and/or cytarabine-containing regimens. Prior to introducing the ALL-type initial regimens, four patients received one or two courses of NHL-type regimens including CHOP (cyclophosphamide, vincristine, doxorubicin, and prednisolone) or ICE (ifosfamide, carboplatin, etoposide)-like regimens. The details of initial therapies (induction and consolidation regimens) are summarized in Supplemental Table 1.
After the abovementioned initial treatments were given, 19 patients achieved their first CR (CR1; N = 14; 66.7%) or first PR (PR1; N = 5; 23.8%) (Fig. 1). Those who failed to achieve CR/PR in the initial therapies underwent HSCT at the stage of SD/PD (N = 2). Among CR1/PR1 patients, 11 patients underwent upfront HSCT, while other 8 patients did not. All of the 8 patients experienced relapse, and salvage therapies were introduced, including monotherapies (nelarabine, clofarabine, and L-ASP) and the combination of mitoxantrone, etoposide, medium-dose cytarabine. Five patients responded to the salvage therapies and underwent HSCT at second CR (CR2; N = 2) or second PR (PR2; N = 3) (Fig. 1). Those who failed to achieve CR2/PR2 with salvage therapy were transplanted at SD/PD disease status.
Refractoriness and/or relapse before HSCT was observed in 10 patients during the course of or after the initial chemotherapies; 2 patients did not achieve remission after the induction therapies (PIF) and 8 patients experienced relapse after initial therapies (Fig. 1). Risk analyses using the Fine–Gray proportional-hazards model demonstrated that none of the patient characteristics at diagnosis were significantly correlated with the occurrence of relapse (data not shown). These results support that the risk of relapse cannot be predicted at the time the diagnosis is made, and all patients should be regarded as being at high risk for relapse once diagnosed with T-LBL.
HSCT procedures and post-transplant outcomes
Patient characteristics at the time of HSCT are shown in Table 2. The disease status profile of the study group at the time of HSCT is as follows: CR1 (N = 9), PR1 (N = 2), CR2 (N = 2), PR2 (N = 3), SD/PD (N = 3), and PIF (N = 2). Thus, 11 patients were categorized as standard-disease patients, and 10 patients were categorized as advanced-disease patients. The median time from diagnosis to HSCT in the total study group was 8.2 (2.3–20.4) months; the median time was 6.9 (5.0–9.6) months in the standard-disease group, while it was 10.7 (2.3–20.4) months in the advanced-disease group. Allogeneic donors were selected in 16 cases (76.2%; bone marrow or peripheral blood stem cell transplantation, N = 11, and cord blood transplantation, N = 5), while 5 patients (23.8%) underwent autologous HSCT because allogeneic donors were not available in a timely manner. MAC regimens were adopted in 16 patients (76.2%), while 5 patients (23.8%) received RIC. Detailed information on conditioning regimens is presented in the Supplemental Table 2. No significantly skewed distributions of patient characteristics or HSCT parameters between the standard- and advanced-disease groups were observed (Table 2).
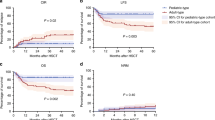
After the median follow-up time of 8.8 (3.2–16.2) years for survivors, post-HSCT relapse was observed in 9 patients, while NRM was marked in 2 patients. Figure 2 shows the curves for OS (at 5 years from HSCT, 56.3%; 95% CI 32.6–74.5%), NRM (at 5 years, 9.5%; 95% CI 1.5–26.7%), and the cumulative incidence of relapse (at 5 years, 42.9%; 95% CI 21.2–63.0%) for the entire cohort.
HSCT-related prognostic factors
Next, aspects of the posttransplant prognosis including, OS, NRM, and relapse, were compared between standard- and advanced-disease patients to determine the appropriate timing of HSCT among the available strategies for T-LBL. As a result, OS from HSCT was superior in the standard-disease group relative to the advanced-disease group at five years (79.5%; 95% CI 39.3–94.5% vs. 30.0% (95%CI 7.1–57.8%), p = 0.01) (Fig. 3A). NRM was in the similar trend (Fig. 3B), while standard-disease patients showed lower relapse with borderline significance when compared with advanced-disease patients (60.0%; 95% CI 21.7–84.3% vs. 27.3%; 95% CI 5.7–55.4%; p = 0.06) (Fig. 3C).
The abovementioned prognostic differences between the two groups concerning the disease risk were subjected to the adjustment by the other confounding factors; univariate and multivariate analyses incorporating various prognostic factors were performed, and the results are shown in Table 3. In the univariate analysis for OS, HCT-CI ≥ 1 was associated with the inferior OS as compared with HCT-CI 0 with the borderline significance [hazard ratio (HR), 3.43; 95% CI 0.91–12.9; p = 0.07], while the advanced-disease patients presented an HR of 5.92 (95% CI 1.22–28.8; p = 0.03) as compared with the standard-disease patients. The other considered factors were not statistically significant including the donor origin (allogeneic vs. autologous), and multivariate analysis indicated that disease risk remained the significant risk factor for poorer OS after HSCT (HR 5.97; 95% CI 1.21–29.4; p = 0.03) (Table 3).
The results concerning relapse are shown in Table 3, and HSCT in the standard-disease group was linked to a lower incidence of relapse, together with a similar rate of NRM (Fig. 3B), resulting in the significantly superior OS seen in this cohort (Table 3).
Regarding donor source, our results indicated that post-HSCT outcomes were the same between patients who received autologous and allogeneic HSCT (Table 3), with the OS rates at 5 years being, 60.0% (95% CI 12.6–88.2%) and 54.7% (95% CI 27.4–75.5%) (p = 0.70), respectively (Supplemental Fig. 1A). NRM and incidence of relapse were also similar between these two subgroups (Supplemental Figs. 1B and 1C). The superiority regarding OS following HSCT in the standard-disease group was also confirmed by the analyses assessing OS from the initial diagnosis; the postdiagnosis OS in the entire cohort was 56.3% (95% CI 32.6–74.5%) (Fig. 4A) and was significantly better in the standard-disease group than in the advanced-disease group (79.5%; 95% CI 39.3–94.5% vs. 30.0%; 95% CI 7.1–57.8%; p = 0.02) (Fig. 4B), though a lead-time bias exists, negatively impacting standard-disease patients.
Discussion
This multicenter retrospective cohort study investigated the risk of relapse and outcomes of HSCT in adult patients with T-LBL who received ALL-type initial therapies and revealed two major findings. (1) relapse after ALL-type chemotherapies without HSCT was frequently observed, and among considered patient- or disease-related variables, no significant risk factors for relapse were statistically extracted; (2) HSCT performed in patients with a CR1/PR1 status is associated with significantly more favorable outcomes (i.e., improved OS both after HSCT and after the initial diagnosis) as compared with those experienced by patients with other disease statuses mainly as a result of the lower incidence of post-HSCT relapse. Our study highlights the potential beneficial role of frontline HSCT in adult patients with T-LBL, even in the era of ALL-type initial chemotherapy. The outlined considerations were explored for the first time in this study, though the size of the study cohort was small due to the rarity of this disease in adults.
Initially, the risk stratification of relapse after ALL-type chemotherapy is one of the most important aspects in T-LBL for the determination of HSCT indication. In our analyses, however, we failed to detect any patient group showing a significantly higher risk of relapse and who especially might require frontline HSCT among the patient subgroups we considered. These results, in part, can be attributed to a beta error16, but at the same time, may indicate the level of difficulty inherent in establishing T-LBL relapse risk-stratification models using the clinical parameters that are currently available. Recent studies have revealed that persistent minimal residual disease in bone marrow17, the mutation status of NOTCH1 and its downstream cascade2, and the expression of several microRNAs8 can possibly predict poorer prognosis in adult patients with T-LBL, but these biomarkers are not readily available in clinical practice, and their usefulness still need to be validated through prospective clinical trials. Until that time, all patients with T-LBL can be designated as candidates for HSCT because of the relatively high incidence of relapse after chemotherapy (from 35% up to 60%)2,7,18,19. Besides, using pediatric ALL-like chemotherapy (which is typically more intensified as compared with the ordinal ALL-like regimen) in young adult patients with T-LBL can suppress the relapse incidence more powerfully after chemotherapy, and this can limit the indication of HSCT2, although this was not analyzed in this study.
Now that certain records of the incidence rate of post-chemotherapy relapse exist and no significant risk factors have been nominated, HSCT should be considered in all eligible patients with T-LBL, and the timing of the transplant procedure should instead be the matter of debate. Regarding this point, we demonstrated that upfront HSCT (at CR1/PR1) can provide significantly superior prognosis when compared to that performed in patients with a CR2/PR2 or later state mainly due to the lower incidence of relapse. This difference in outcomes after HSCT performed at different times is significant not only in the comparison of the survival time after HSCT but also in that after the initial diagnosis, where the lead-time bias is unfavorable for upfront HSCTs. Considering the higher percentage of CR/PR patients in the upfront-HSCT cohort, the prognostic difference is mainly attributed to the pretransplant disease status and following relapse risk; patients with T-LBL, once having relapsed after chemotherapy, often experience difficulty in achieving CR/PR again prior to HSCT20, leading to the poor OS even after allo-HSCT21. In contrast with other hematological malignancies such as B-ALL, few promising therapeutic agents are currently available for relapsed T-LBL; nelarabine and clofarabine, which are candidates for T-LBL salvage therapy approved by the United States Food and Drug Administration, have shown only limited effects so far22,23. Considering that such salvage chemotherapies cannot guarantee the achievement of remission, at present, frontline HSCT may be the optimal feasible option for transplant-eligible patients.
The main suggestion taken away from our study–that is, to perform upfront HSCT in T-LBL initially treated with ALL-type chemotherapies is compatible with the findings of several other studies. In a multicenter retrospective study of 49 patients with LBL treated with the hyper-CVAD regimen, transplanted patients (N = 24) showed better OS (76% at 3 years) and progression-free survival (78% at 3 years) when compared with complete responders without HSCT consolidation5. Other studies have reported the superiority of HSCT consolidation after chemotherapies, but the wide variety of initial chemotherapies (ALL-type regimens were used only in half of the study group)18 and extremely shorter periods of observation (median was 31.5 months)24 unfortunately somewhat dilutes the external validity in these studies. On the other hand, one study suggested that allo-HSCT in CR1 should not be considered due to the relatively favorable outcomes even without HSCT25; their claim, however, depends on the prognosis in mature T-ALL/LBL patients, which is a relatively rare subtype in LBL26.
Regarding donor source (autologous vs. allogeneic), our analysis indicated the existence of a similar prognosis, but this evaluation is insufficient due to the small number of patients included, especially in the autologous HSCT cohort. Several studies have revealed a lower incidence of relapse in patients undergoing allogenic HSCT relative to autologous HSCT8,11; on the other hand, one study suggested the efficacy of tandem autologous HSCTs27. The results are inconclusive among all these studies due to the heterogeneity and the small number of cohorts, but it is suggested that allogenic HSCT is more effective from the viewpoint of perpetuating the continuous suppression of post-transplant relapse mainly due to the graft-versus-leukemia effects11. Autologous HSCT might be a treatment option in patients who are not eligible for allogenic HSCT.
Thus, the present study has analyzed the prognosis of HSCT-eligible patients with T-LBL, reviewing their clinical records comprehensively, yet some limitations to this study exist and must be addressed. First, the pretransplant therapy regimen (basically, hyper-CVAD–based regimens were adopted across the total cohort) and the timing or type of HSCT (at CR1/PR1 vs. later, allogeneic vs. autologous, or MAC vs. RIC regimens) were chosen by the physician in charge at that time, though, in most cases, allogeneic HSCT after the MAC regimen was selected. Second, the number of cases was small due to the rarity of the disease under study, and as a consequence, the evaluation of prognostic factors was insufficient. A prospective nationwide or international multicenter randomized trial in the future might overcome the limitations of this study.
Conclusions
We performed a multicenter cohort retrospective study of patients with T-LBL, analyzing the efficacy of ALL-type regimens and the prognostic impacts of HSCT by obtaining all the necessary data from clinical records and evaluating these based on a standardized protocol. Our study indicated that frontline HSCT is a feasible treatment option in the era of intensive ALL-type therapy. We expect that this study may offer clinically useful information to improve the overall prognosis and trigger the identification of new therapeutic strategies for the patients with T-LBL in the future.
References
Ducassou, S. et al. Clinical presentation, evolution, and prognosis of precursor B-cell lymphoblastic lymphoma in trials LMT96, EORTC 58881, and EORTC 58951. Br. J. Haematol. 152, 441–451. https://doi.org/10.1111/j.1365-2141.2010.08541.x (2011).
Lepretre, S. et al. Pediatric-like acute lymphoblastic leukemia therapy in adults with lymphoblastic lymphoma: the GRAALL-LYSA LL03 study. J. Clin. Oncol. 34, 572–580. https://doi.org/10.1200/JCO.2015.61.5385 (2016).
Hunault, M. et al. Outcome of adult T-lymphoblastic lymphoma after acute lymphoblastic leukemia-type treatment: a GOELAMS trial. Haematologica 92, 1623–1630. https://doi.org/10.3324/haematol.10882 (2007).
Swerdlow, S. H. World Health Organization & International Agency for Research on Cancer. WHO classification of tumours of haematopoietic and lymphoid tissues. Revised 4th edn (International Agency for Research on Cancer, 2017).
Jeong, S. H. et al. Multicenter analysis of treatment outcomes in adult patients with lymphoblastic lymphoma who received hyper-CVAD induction followed by hematopoietic stem cell transplantation. Ann. Hematol. 94, 617–625. https://doi.org/10.1007/s00277-014-2258-y (2015).
Song, K. W. et al. Primary therapy for adults with T-cell lymphoblastic lymphoma with hematopoietic stem-cell transplantation results in favorable outcomes. Ann. Oncol. 18, 535–540. https://doi.org/10.1093/annonc/mdl426 (2007).
Thomas, D. A. et al. Outcome with the hyper-CVAD regimens in lymphoblastic lymphoma. Blood 104, 1624–1630. https://doi.org/10.1182/blood-2003-12-4428 (2004).
Tian, X. P. et al. Prognostic and predictive value of a microRNA signature in adults with T-cell lymphoblastic lymphoma. Leukemia 33, 2454–2465. https://doi.org/10.1038/s41375-019-0466-0 (2019).
Makita, S. et al. Clinical outcomes after allogeneic stem cell transplantation for adult lymphoblastic lymphoma. J. Clin. Exp. Hematopathol. 56, 28–33. https://doi.org/10.3960/jslrt.56.28 (2016).
Kim, S. W. et al. Myeloablative allogeneic hematopoietic stem cell transplantation for non-Hodgkin lymphoma: a nationwide survey in Japan. Blood 108, 382–389. https://doi.org/10.1182/blood-2005-02-0596 (2006).
Levine, J. E. et al. A comparison of allogeneic and autologous bone marrow transplantation for lymphoblastic lymphoma. Blood 101, 2476–2482. https://doi.org/10.1182/blood-2002-05-1483 (2003).
Atsuta, Y. Introduction of Transplant Registry Unified Management Program 2 (TRUMP2): scripts for TRUMP data analyses, part I (variables other than HLA-related data). Int. J. Hematol. 103, 3–10. https://doi.org/10.1007/s12185-015-1894-x (2016).
Cheson, B. D. et al. Revised response criteria for malignant lymphoma. J. Clin. Oncol. 25, 579–586. https://doi.org/10.1200/JCO.2006.09.2403 (2007).
Giralt, S. et al. Reduced-intensity conditioning regimen workshop: defining the dose spectrum. Report of a workshop convened by the center for international blood and marrow transplant research. Biol. Blood Marrow Transplant. 15, 367–369. https://doi.org/10.1016/j.bbmt.2008.12.497 (2009).
Fine, J. P. & Gray, R. J. A proportional hazards model for the subdistribution of a competing risk. J. Am. Stat. Assoc. 94, 496–509. https://doi.org/10.2307/2670170 (1999).
Jekel, J. F. & Jekel, J. F. Epidemiology, Biostatistics, and Preventive Medicine 3rd edn. (Saunders, Philadelphia, 2007).
Cortelazzo, S. et al. Results of a lymphoblastic leukemia-like chemotherapy program with risk-adapted mediastinal irradiation and stem cell transplantation for adult patients with lymphoblastic lymphoma. Ann. Hematol. 91, 73–82. https://doi.org/10.1007/s00277-011-1252-x (2012).
Yang, L. et al. Allogeneic hematopoietic stem cell transplantation should be in preference to conventional chemotherapy as post-remission treatment for adults with lymphoblastic lymphoma. Bone Marrow Transplant. 53, 1340–1344. https://doi.org/10.1038/s41409-018-0184-7 (2018).
Zhu, M. Y. et al. A childhood chemotherapy protocol improves overall survival among adults with T-lymphoblastic lymphoma. Oncotarget 7, 38884–38891. https://doi.org/10.18632/oncotarget.9144 (2016).
Michaux, K. et al. Relapsed or refractory lymphoblastic lymphoma in children: results and analysis of 23 patients in the EORTC 58951 and the LMT96 protocols. Pediatr. Blood Cancer 63, 1214–1221. https://doi.org/10.1002/pbc.25990 (2016).
Burkhardt, B. et al. Poor outcome for children and adolescents with progressive disease or relapse of lymphoblastic lymphoma: a report from the berlin-frankfurt-muenster group. J. Clin. Oncol. 27, 3363–3369. https://doi.org/10.1200/JCO.2008.19.3367 (2009).
Zwaan, C. M. et al. Safety and efficacy of nelarabine in children and young adults with relapsed or refractory T-lineage acute lymphoblastic leukaemia or T-lineage lymphoblastic lymphoma: results of a phase 4 study. Br. J. Haematol. 179, 284–293. https://doi.org/10.1111/bjh.14874 (2017).
Barba, P. et al. Clofarabine-based chemotherapy for relapsed/refractory adult acute lymphoblastic leukemia and lymphoblastic lymphoma. The Spanish experience. Am. J. Hematol. 87, 631–634. https://doi.org/10.1002/ajh.23167 (2012).
Hu, M. et al. Outcome of adult T-lymphoblastic lymphoma depends on ALL-type chemotherapy, prognostic factors, and performance of allogeneic hematopoietic stem cell transplantation. Medicine (Baltimore) 97, e11374. https://doi.org/10.1097/MD.0000000000011374 (2018).
Jain, N. et al. Early T-cell precursor acute lymphoblastic leukemia/lymphoma (ETP-ALL/LBL) in adolescents and adults: a high-risk subtype. Blood 127, 1863–1869. https://doi.org/10.1182/blood-2015-08-661702 (2016).
Patel, J. L. et al. The immunophenotype of T-lymphoblastic lymphoma in children and adolescents: a Children’s Oncology Group report. Br. J. Haematol. 159, 454–461. https://doi.org/10.1111/bjh.12042 (2012).
Liu, Y. et al. Tandem autologous hematopoietic stem cell transplantation for treatment of adult T-cell lymphoblastic lymphoma: a multiple center prospective study in China. Haematologica https://doi.org/10.3324/haematol.2019.226985 (2019).
Acknowledgements
The authors would like to thank all the involved physicians and data managers who contributed valuable data on transplantation to this study. We thank the Kyoto Stem Cell Transplantation Group (KSCTG), which is composed of Kyoto University Hospital, Kobe City Medical Center General Hospital, Japanese Red Cross Osaka Hospital, Kurashiki Central Hospital, Tenri Hospital, Kokura Memorial Hospital, Shizuoka General Hospital, Takatsuki Red Cross Hospital, Japanese Red Cross Wakayama Medical Center, Shinko Hospital, Kyoto City Hospital, Kitano Hospital, Japan Red Cross Otsu Hospital, and Kyoto-Katsura Hospital. This work was supported in part by research funding from the Cell Science Research Foundation, Ono Medical Research Foundation, SGH Foundation, MSD Life Science Foundation, GlaxoSmithKline, and the American Society of Hematology awarded to Y.A.
Author information
Authors and Affiliations
Consortia
Contributions
M.M-F. and Y.A. designed the study, reviewed and analyzed data, and wrote the paper; S.Y., T.I., J.K., T.K., and A.T-K. interpreted data and revised the manuscript; T.A., Y.U, K.I., T.M., K.Y., T.K., A.Y., and M.N. contributed to the data collection and provided critiques on the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Morita-Fujita, M., Arai, Y., Yoshioka, S. et al. Indication and benefit of upfront hematopoietic stem cell transplantation for T-cell lymphoblastic lymphoma in the era of ALL-type induction therapies. Sci Rep 10, 21418 (2020). https://doi.org/10.1038/s41598-020-78334-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-78334-x
This article is cited by
-
Lymphoblastic Lymphoma: a Concise Review
Current Oncology Reports (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.