Abstract
Both neonatal hypothermia and hyperthermia represent important risk factors for neonatal mortality, but information on mortality risk across a full range of neonatal temperatures is lacking in low-resource settings. We evaluated the association between neonatal mortality and a full range of admission temperatures in a low-resource setting. This retrospective observational study was conducted at Beira Central Hospital, Mozambique. The relationship between admission temperature and mortality was evaluated using multivariable analyses with temperature modeled as non-linear term. Among 2098 neonates admitted to the Special Care Unit between January–December 2017, admission temperature was available in 1344 neonates (64%) who were included in the analysis. A non-linear association between mortality rate and temperature was identified. Mortality rate decreased from 84% at 32 °C to 64% at 34.6 °C (− 8% per °C), to 41% at 36 °C (− 16% per °C), to 26% to 36.6 °C (− 25% per °C) and to 22% at 38.3 °C (− 2% per °C), then increased to 40% at 41 °C (+ 7% per °C). Mortality rate was estimated to be at minimum at admission temperature of 37.5 °C. In conclusions, the non-linear relationship highlighted different mortality risks across a full range of neonatal temperatures in a low-resource setting. Admission temperature was not recorded in one third of neonates.
Similar content being viewed by others
Introduction
Maintaining normothermia at birth is a major challenge for newbosrn survival1. Both hypothermia and hyperthermia represent important risk factors for neonatal morbidity and mortality2. Neonatal hypothermia is common in both high- and low-resource settings, but is rarely indicated as direct cause of death, while it is associated with a considerable portion of neonatal mortality, mostly as comorbidity of preterm birth, asphyxia and sepsis3. Neonatal hyperthermia is associated with brain injury and hemodynamic changes4. A recent systematic review including 20,911 participants from 12 studies indicated a 57.2% prevalence of neonatal hypothermia in Eastern Africa5. Of note, hypothermia in low-resource settings involves both term and preterm infants5,6. In low-middle resource settings, neonatal hypothermia was associated with elevated mortality risk in both hospital and community studies7,8,9,10,11,12.
The World Health Organization (WHO) recommends maintaining neonatal temperature between 36.5 and 37.5 °C, with lower temperatures (< 36.5 °C) defining hypothermia ranges and higher temperatures (> 37.5 °C) defining hyperthermia ranges13. Literature offers heterogeneous definitions of neonatal thermal ranges3, in search for an optimal classification that mirrors clinical outcomes.
Although offering the advantages of easy interpretation and application in clinical practice, the classification of a continuous variable has the strong disadvantage of underestimating the variation of the outcome14. In 2015, the Canadian Neonatal Network attempted to overcome such disadvantages by evaluating a large cohort of very preterm infants where neonatal temperature at admission to neonatal intensive care unit (NICU) was categorized in nine groups with 0.5 °C increments from < 34.5 to ≥ 38.0 °C15. The authors suggested a U-shaped relationship between admission temperature and adverse neonatal outcomes, with lowest rate of adverse outcomes between 36.5 and 37.2 °C15. The U-shape relationship highlights that both low and high temperatures impair neonatal outcomes, in agreement with international recommendations2,15,16.
Maintaining normothermia at birth is an even more crucial challenge in low-resource settings, where appropriate thermal care of the newborn is often neglected due to poor provider training, limited awareness of the problem and limited availability of equipment3,17. Furthermore, thermal stability (including warm delivery room, immediate drying, skin-to-skin contact, early breastfeeding, delayed bathing, adequate clothing, warm transport, keeping baby close to the mother) is not a central objective in management protocols in low-resource settings6,13. To our knowledge, information on mortality risk across a full range of admission temperatures is lacking in these settings. This study aimed to evaluate the relationship between mortality and a full range of admission temperatures in a low-resource setting.
Methods
Study design and setting
This is a retrospective study on the relationship between admission temperature and in-hospital neonatal mortality at the Special Care Unit (SCU) of the Beira Central Hospital (BCH) in Beira (Mozambique). The study was approved by the Clinical Board of BCH (January 30, 2018), which waived the need for written informed consent given the retrospective nature of the study and the use of anonymized data from hospital records. Research was performed in accordance with relevant guidelines and regulations.
BCH is located in the province of Sofala, Mozambique and is the referral hospital for a geographical area that covers about 1.7 million people. In the province, average temperature ranges from 21 °C in July to 28.5 °C in January; the hot (and rainy) season runs approximately from November to March, and the cold season from June to August. About 5000 deliveries and 2100 admissions to the SCU occur every year at BCH. Medical transport system was not available in the province and outborn infants were brought to the hospital by their families.
Patients
All neonates admitted to the SCU between January 1 and December 31, 2017 were evaluated for inclusion in the study. All neonates were included in (1) the assessment of availability of temperature at admission, and (2) the comparison of patient characteristics according to availability of temperature at admission. Then, only neonates with available temperature at admission were included in the analysis of mortality.
Data collection
All data were retrieved from hospital records by hospital staff and were collected in an anonymized dataset. Maternal data included maternal age, HIV infection, twin pregnancy and number of previous gestations. Neonatal data included mode of delivery, birthplace, gestational age, sex, birth weight, 5-min Apgar score (for inborns), time to transfer and admission to SCU, diagnosis at admission, temperature at admission, and mortality through facility discharge.
Diagnosis at admission was based on clinical examination because availability of laboratory and instrumental exams was limited18.
At admission to SCU, neonatal axillary temperature was measured by the attending nurse using a digital thermometer (C202; Terumo, Tokyo, Japan). The nurse repeated the measurement of temperature in case of extreme hypothermia (< 35 °C) or extreme hyperthermia (> 39 °C). Severe/moderate hypothermia was defined as temperature < 36 °C, mild hypothermia as 36–36.4 °C, normal temperature as 36.5–37.5 °C and hyperthermia as > 37.5 °C13.
Statistical analysis
Continuous data were reported as median and interquartile range (IQR), while categorical data as number and percentage.
The comparison of included (available temperature at admission) and excluded (unavailable temperature at admission) neonates was performed using Mann–Whitney test (continuous data) and Chi-square test (categorical data).
The relationship between mortality rate and neonatal temperature at admission was investigated with logistic regression models where temperature was modeled with first order polynomial or restricted cubic splines. The number of knots for the temperature was chosen in order to maximize the model likelihood ratio.
In all neonates (inborn, outborn, homebirth), a logistic regression model was estimated to assess the effect of admission temperature (modeled with restricted cubic splines) on mortality, adjusting for a set of pre-defined clinically relevant factors (diagnosis, place and mode of delivery, seasonality, sex, birthweight, twin birth, maternal age, HIV, and number of previous gestations). Model selection was performed by AIC reduction.
In the subgroup of inborn/outborn neonates, the 5-min Apgar score was added among the factors of the logistic regression model. In fact, the 5-min Apgar score is known to be a clinically relevant predictor of mortality, but it is not available in neonates born at home. Model selection was performed by AIC reduction.
Model performance was evaluated with internal validation (c-index) and calibration (calibration-in-the-large and calibration slope) using bootstrap methods (re-sampling with replacement to create 1000 samples of the same size as the original)19.
The results from the two regression models were summarized in two nomograms (one for all admitted neonates and one for inborn/outborn neonates).
All tests were 2-sided and a p value less than 0.05 was considered statistically significant. Statistical analysis was performed using R 3.5 (R Foundation for Statistical Computing, Vienna, Austria)20.
Results
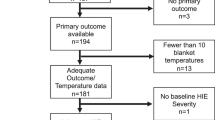
From 1st January to 31st December 2017, 2098 neonates were admitted to SCU for prematurity (648, 30.9%), asphyxia/HIE (559, 26.6%), wet lung (216, 10.3%), trauma (15, 0.7%), congenital malformations (96, 4.6%), fever (67, 3.2%), sepsis (55, 2.6%), seizures (17, 0.8%), jaundice/hyperbilirubinemia (34, 1.6%), or with other diagnoses (381, 18.2%). Neonatal temperature at admission was available in 1344 neonates (64%), who were included in the analysis. The comparison of 1344 included neonates (available temperature at admission) and 754 excluded neonates (unavailable temperature at admission) neonates is reported in Table 1. Birth weight (p = 0.004), 5-min Apgar score (p = 0.006), birthplace (p = 0.02) and diagnosis at admission (p = 0.003) were different between included and excluded neonates (Table 1). Mortality rate was 36.5% in included neonates and 30.5% in excluded neonates (p = 0.007). Among inborns, resuscitation in delivery room was needed in 334 out of 746 included subjects (44.8%) and in 91 out of 193 excluded subjects (57.2%; information not available in 267 outborns) (p = 0.61). Time from birth to admission was not different between included and excluded neonates (p = 0.82, Table 1). Maternal age, number of gestation and HIV infection were not different between included and excluded neonates (Table 1).
Among 1344 included neonates, median temperature at admission was 36.3 °C (IQR 35.8–36.9 °C; min 32 °C, max 41.1 °C). Severe/moderate hypothermia was reported in 395 neonates (29.4%), mild hypothermia in 376 (28.0%), normal temperature in 436 (32.4%) and hyperthermia in 137 (10.2%) (Fig. 1A,B). Birthplace was associated with neonatal temperature at admission (p < 0.0001): the highest proportion of homebirths was found in severely/moderately hypothermic neonates, while the highest proportion of outborn was found in neonates with hyperthermia (Fig. 1C).
After a median length of stay of 4 days (IQR 2–8), 848 neonates were discharged alive and 488 died, while the information was not available in eight neonates. Observed mortality rate was 58% (231 out of 395) in severe/moderate hypothermia, 33% (123 out of 372) in mild hypothermia, 24% (103 out of 432) in normal temperature range and 23% (31 out of 137) in hyperthermia (Fig. 2A). The relationship between mortality rate and neonatal temperature at admission was investigated with logistic regression models where temperature was modeled with first order polynomial and with restricted cubic splines (Fig. 2B,C). A non-linear association between mortality rate and temperature was identified (non-linear term: p < 0.0001), thus the model with cubic splines was preferred over the model with first order polynomial. Four knots were identified in 34.6 °C, 36 °C, 36.6 °C and 38.3 °C. Estimated mortality rate decreased from 84% at 32 °C to 64% at 34.6 °C (mean − 8% per °C), to 41% at 36 °C (mean − 16% per °C), to 26% to 36.6 °C (mean − 25% per °C) and to 22% at 38.3 °C (mean − 2% per °C), then increased to 40% at 41 °C (mean + 7% per °C). Mortality rate was estimated to be at a minimum at admission temperature of 37.5 °C (Fig. 2C). The curve of estimated mortality rate according to admission temperature had similar shape in term and preterm infants (p = 0.78), but the latter had higher mortality rate (p < 0.0001) (Fig. 3).
Since information on gestational age was largely missing, multivariable analysis included the diagnosis of prematurity as proxy of the role of gestational age, although prematurity underlines a wide range of gestational ages. Since all neonates born from caesarean sections were inborns, birthplace and mode of delivery were collapsed in one variable with four categories (caesarean inborn, vaginal inborn, vaginal outborn and vaginal homebirth).
In all infants (inborns, outborns, homebirths), admission temperature (linear term p < 0.0001, non-linear term p < 0.0001), diagnosis (p < 0.0001), delivery (p < 0.0001), birthweight (p < 0.0001), twin birth (p = 0.01) and seasonality (p < 0.0001) were included in the final model. Internal validation and calibration via bootstrapping showed good validation (c-index 0.78) and calibration (calibration-in-the-large − 0.0264 and calibration slope 0.9530). The model was graphically represented by the nomogram in Fig. 4.
In inborn/outborn infants, admission temperature (linear term p < 0.0001, non-linear term p = 0.0002), diagnosis (p < 0.0001), delivery (p < 0.0001), 5-min Apgar score (p < 0.0001) birthweight (p < 0.0001), twin birth (p = 0.01) and seasonality (p < 0.0001) were included in the final model. Internal validation and calibration via bootstrapping showed good validation (c-index 0.79) and calibration (calibration-in-the-large − 0.0286 and calibration slope 0.9407). The model was graphically represented by the nomogram in Fig. 5.
Nomograms for inborn and outborn patients. Diagnosis legend: fever, trauma, jaundice/hyperbilirubinemia, other (A); wet lung (B); asphyxia/HIE (C); sepsis/seizures (D); prematurity (E); congenital malformations (F). Neonatal temperature at admission is expressed in °C. Birthweight is expressed as 100 g.
Information on both models is reported in Supplementary Table 1.
Discussion
Our findings highlighted a substantial underreporting of neonatal temperature at admission, but also showed that the majority of neonates were admitted with hypothermia. Neonatal temperature at admission had a non-linear relationship with mortality, which was the lowest rate at 37.5 °C and increased with different slopes when departing from the interval 36.6–38.3 °C.
To our knowledge, this is the first study to investigate the differences in mortality risk across a full range of admission temperatures and to describe a non-linear relationship between neonatal temperature at admission and mortality in a low-resource setting. Our findings confirm that both hypothermia and hyperthermia at admission are associated with mortality, but add a differentiation of mortality risk according to the specific temperature.
The study has some limitations. First, it is a retrospective study, thus quality of data was limited. For example, information on gestational age was largely missing (a common problem in low-resource settings), thus the model included the diagnosis of prematurity as proxy of the role of gestational age, although prematurity underlines a wide range of gestational weeks. Second, temperature at admission was not available in about one third of neonates. Third, diagnosis at admission was based on clinical examination because availability of laboratory and instrumental exams was limited.
Both hypothermia and hyperthermia represent important predictors of neonatal morbidity and mortality1,2. However, neonatal temperature is often missing in clinical records although being an important and easy-to-measure indicator3. Our findings showed that admission temperature was not available in around one out of three neonates, thus highlighting the substantial underreporting of such indicator. Since neonatal temperature at admission can be used as quick feedback of neonatal care during the immediate postnatal phase, the lack of such data hampers the implementation of quality improvement processes2.
In low resource settings, the incidence of postnatal hypothermia is very high, ranging from 32 to 85%3, while hyperthermia at admission has received less attention1,3,6. Our data indicated that around 57% of neonates were admitted with hypothermia, thus confirming that prevention of postnatal thermal losses is still an underappreciated major challenge in low resource settings3.
Available literature approached the investigation on neonatal temperature based on the few categories indicated by the WHO classification3,6,13. This approach offers the advantages of easy interpretation and application in clinical practice, but constrains the variability of the phenomenon into pre-specified classes14. A recent study attempted to overcome such disadvantage by splitting admission temperature in a larger number of categories and suggested a U-shaped relationship between admission temperature and adverse neonatal outcomes15. The U-shape relationship implicated that both low and high temperatures impaired neonatal outcomes, but the generalizability of these findings was limited by the inclusion of very preterm infants, the high-resource setting and the categorization of the temperature15. Our study adds the information on the differences in mortality risk across a full range of admission temperatures, in both preterm and term infants born in a low-resource setting. In addition, our findings displays the relationship between mortality and temperature as asymmetric inverted omega-shaped curve rather than U-shaped curve. Such non-linear relationship confirmed that both low and high temperatures increased the mortality risk, but highlighted the different slopes when departing from normothermia (Fig. 2C).
These findings reinforce the need for temperature assessment in all admitted neonates and confirm the worse impact on mortality of low temperatures compared to high temperatures in a low-resource setting. Moreover, this approach allows the definition of a personalized risk assessment that goes beyond the categorical approach. Our results are summarized in two nomograms (one for all admitted neonates and one for inborn/outborn neonates) that can be considered among the proposals for the development of a quick mortality-risk calculator to be used in clinical practice. The nomograms require external validation in order to assess their generalizability to other low-resource settings. If confirmed, the nomograms can be transformed in on-line tools or apps for an easy and quick assessment of personalized mortality risk in clinical practice. Available literature offers other neonatal mortality risk scoring systems, such as CRIB-II, SNAP, NMS, NMR-200021,22,23,24. Unfortunately, we could not use such scores because they include some parameters that were not available in the care (hence in the hospital records) of our study setting (i.e. blood gas analysis, oxygen saturation, mechanical ventilation). In addition, some of them were developed for specific categories of neonates (i.e. birthweight < 1500 g or gestational age < 31 weeks; birthweight < 2000 g).
Neonatal temperature at admission should be recorded as prognostic factor as well as quality indicator2. In the present study, the underreporting of such indicator highlights the need for enhancing the awareness of the importance of including temperature measurement among routine care. Appropriate actions may include audits (to identify local reasons for the underreporting), education to health care givers who are involved in neonatal care at admission (to enhance awareness of the importance of neonatal temperature), and continuous feedback on this quality improvement (to monitor the implementation).
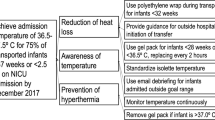
Furthermore, the high rate of hypothermia and hyperthermia at admission calls for implementation of adequate strategies to ensure normothermia immediately after birth in low-resource settings3,17. Quality improvement activities should focus on enlisting thermal stability (i.e. warm delivery room, immediate drying, skin-to-skin contact, early breastfeeding, delayed bathing, adequate clothing, warm transport, keeping baby close to the mother) among the central objectives in management protocols in low-resource settings6,13. Provider training, enhancing awareness and revision of management routines seem to be the key elements for achieving such goal3,6,13,17.
Conclusions
In a low-resource setting, neonatal temperature at admission showed a non-linear relationship with mortality rate, with different impacts of low and high temperatures. Only 32% of the infants were normothermic at admission, indicating the need for implementation of adequate strategies to enhance thermal stability. Temperature at admission was not reported in 36% of the infants, suggesting the need for more closely monitoring the admission temperature.
References
Trevisanuto, D., Testoni, D. & de Almeida, M. F. B. Maintaining normothermia: why and how?. Semin. Fetal Neonatal. Med. 23, 333–339 (2018).
Perlman, J. M. et al. Part 7: neonatal resuscitation: 2015 International consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations. Circulation 132(16 Suppl 1), S204–S241 (2015).
Lunze, K., Bloom, D. E., Jamison, D. T. & Hamer, D. H. The global burden of neonatal hypothermia: systematic review of a major challenge for newborn survival. BMC Med. 11, 24 (2013).
Kasdorf, E. & Perlman, J. M. Hyperthermia, inflammation, and perinatal brain injury. Pediatr. Neurol. 49, 8–14 (2013).
Beletew, B., Mengesha, A., Wudu, M. & Abate, M. Prevalence of neonatal hypothermia and its associated factors in East Africa: a systematic review and meta-analysis. BMC Pediatr. 20, 148 (2020).
Mullany, L. C. Neonatal hypothermia in low-resource settings. Semin. Perinatol. 34, 426–433 (2010).
da Mota Silveira, S. M., Goncalves de Mello, M. J., de Arruda Vidal, S., de Frias, P. G. & Cattaneo, A. Hypothermia on admission: a risk factor for death in newborns referred to the Pernambuco Institute of Mother and Child Health. J. Trop. Pediatr. 49, 115–120 (2003).
Zayeri, F., Kazemnejad, A., Ganjali, M., Babaei, G. & Nayeri, F. Incidence and risk factors of neonatal hypothermia at referral hospitals in Tehran, Islamic Republic of Iran. East Mediterr. Health 13, 1308–1318 (2007).
Ogunlesi, T. A., Ogunfowora, O. B., Adekanmbi, F. A., Fetuga, B. M. & Olanrewaju, D. M. Point-of-admission hypothermia among high-risk Nigerian newborns. BMC Pediatr. 8, 40 (2008).
Bang, A. T., Reddy, H. M., Baitule, S. B., Deshmukh, M. D. & Bang, R. A. The incidence of morbidities in a cohort of neonates in rural Gadchiroli, India: seasonal and temporal variation and a hypothesis about prevention. J. Perinatol. 25(Suppl 1), S18-28 (2005).
Sodemann, M. et al. Hypothermia of newborns is associated with excess mortality in the first 2 months of life in Guinea-Bissau West Africa. Trop. Med. Int. Health 13, 980–986 (2008).
Mullany, L. C. et al. Incidence and seasonality of hypothermia among newborns in southern Nepal. Arch. Pediatr. Adolesc. Med. 164, 71–77 (2010).
World Health Organization. Thermal Protection of the Newborn: A Practical Guide. Report No.: WHO/RHT/MSM/97.2. Geneva: World Health Organization (1997).
Royston, P., Moons, K. G., Altman, D. G. & Vergouwe, Y. Prognosis and prognostic research: developing a prognostic model. BMJ 338, b604 (2009).
Lyu, Y. et al. Association between admission temperature and mortality and major morbidity in preterm infants born at fewer than 33 weeks’ gestation. JAMA Pediatr. 169, 150277 (2015).
Wyllie, J. et al. European resuscitation Council guidelines for resuscitation 2015: section 7. Resuscitation and support of transition of babies at birth. Resuscitation 95, 249–263 (2015).
Lunze, K. & Hamer, D. H. Thermal protection of the newborn in resource-limited environments. J. Perinatol. 32, 317–324 (2012).
Cavicchiolo, M. E. et al. Reduced neonatal mortality in a regional hospital in Mozambique linked to a quality Improvement intervention. BMC Pregnancy Childbirth 16, 366 (2016).
Steyerberg, E. W. Clinical Prediction Models: A Practical Approach to Development, Validation, and Updating (Springer, New York, 2010).
R Core Team. R: A Language and Environment for Statistical Computing (R Foundation for Statistical Computing, Vienna, 2018).
Parry, G., Tucker, J. & Tarnow-Mordi, W. CRIB II: an update of the clinical risk index for babies score. Lancet 361, 1789–1791 (2003).
Shrestha, D. et al. Predicting deaths in a resource-limited neonatal intensive care unit in Nepal. Trans. R. Soc. Trop. Med. Hyg. 111, 287–293 (2017).
Mediratta, R. P. et al. Derivation and validation of a prognostic score for neonatal mortality in Ethiopia: a case-control study. BMC Pediatr. 20, 238 (2020).
Medvedev, M. M. et al. Development and validation of a simplified score to predict neonatal mortality risk among neonates weighing 2000 g or less (NMR-2000): an analysis using data from the UK and The Gambia. Lancet Child Adolesc. Health 4, 299–311 (2020).
Funding
This study was funded by a contribution of the Italian Agency for Development Cooperation (grant AID 11497/CUAMM/MOZ—Healthy Newborn Project: Innovative approaches in protecting the health of the newborn in the Province of Sofala.
Author information
Authors and Affiliations
Contributions
F.C. was responsible for the statistical design and analysis, drafted the manuscript, contributed to interpret the results, and approved the final manuscript as submitted. S.C. contributed to design the study, coordinated and supervised data collection, and critically reviewed the manuscript. V.B. contributed to design the study, collected the data collection, and critically reviewed the manuscript. O.M.W. contributed to design the study, supervised data collection, and critically reviewed the manuscript. A.R.M. contributed to design the study, contributed to data collection, and critically reviewed the manuscript. L.D.D. contributed to design the trial and to interpret the results, and critically reviewed the manuscript. D.P. contributed to design the study, coordinated and supervised data collection, and critically reviewed the manuscript. G.P. contributed to design the study, developed the idea into a formal grant application contributed to interpret the results, and critically reviewed the manuscript. D.T. contributed to the study concept, study design, data interpretation, and writing of the manuscript and critically reviewed the manuscript. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Cavallin, F., Calgaro, S., Brugnolaro, V. et al. Non-linear association between admission temperature and neonatal mortality in a low-resource setting. Sci Rep 10, 20800 (2020). https://doi.org/10.1038/s41598-020-77778-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-77778-5
This article is cited by
-
Thermoregulation for very preterm infants in the delivery room: a narrative review
Pediatric Research (2024)
-
Early neonatal mortality is modulated by gestational age, birthweight and fetal heart rate abnormalities in the low resource setting in Tanzania – a five year review 2015–2019
BMC Pediatrics (2022)
-
The Changing Climate and Pregnancy Health
Current Environmental Health Reports (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.