Abstract
A recent clinical study demonstrated that haemodialysis with a dialysate containing hydrogen (H2) improves blood pressure control in end-stage kidney disease. Herein, we examined whether H2 has a salutary effect on hypertension in animal models. We subjected 5/6 nephrectomised rats to inhalation of either H2 (1.3% H2 + 21% O2 + 77.7% N2) or control (21% O2 + 79% N2) gas mixture for 1 h per day. H2 significantly suppressed increases in blood pressure after 5/6 nephrectomy. The anti-hypertensive effect of H2 was also confirmed in rats in a stable hypertensive state 3 weeks after nephrectomy. To examine the detailed effects of H2 on hypertension, we used an implanted telemetry system to continuously monitor blood pressure. H2 exerted an anti-hypertensive effect not only during daytime rest, but also during night-time activities. Spectral analysis of blood pressure variability revealed that H2 improved autonomic imbalance, namely by suppressing the overly active sympathetic nervous system and augmenting parasympathetic nervous system activity; these effects co-occurred with the blood pressure-lowering effect. In conclusion, 1-h daily exposure to H2 exerts an anti-hypertensive effect in an animal model of hypertension.
Similar content being viewed by others
Introduction
Molecular hydrogen (H2) is a versatile gas with antioxidant and anti-inflammatory properties and no apparent side effects1. We previously demonstrated in animal models that H2 inhalation is a promising therapeutic option for ischaemia–reperfusion injury in emergency and critical care settings such as acute myocardial infarction, cardiac arrest, and haemorrhagic shock2,3,4,5. We also conducted a proof-of-concept clinical study to validate the efficacy and safety of H2 gas inhalation therapy for patients with acute myocardial infarction and post–cardiac arrest syndrome6,7. A multicentre, double-blind, randomised controlled trial is currently underway to test the therapeutic effects of H2 on brain damage in patients resuscitated from cardiac arrest to obtain Pharmaceutical Affairs approval from the Ministry of Health, Labour and Welfare8. Apart from inhibiting ischaemia–reperfusion injury, H2 has been shown in animal studies to effectively suppress cytokine storms in a state of overreaction of the immune system. Notably, the Chinese National Health and Medical Commission recommends H2 inhalation in addition to general O2 therapy for treating coronavirus disease 2019 (COVID-19)-associated pneumonia or acute respiratory distress syndrome, and the effect of H2 inhalation in patients with COVID-19 was recently reported9,10.
The global prevalence of hypertension in adults is estimated to be 1.13 billion11. Hypertension is a strong risk factor for cardiovascular disease and chronic kidney disease, with hypertension observed in more than 80% of patients with chronic kidney disease12,13. As hypertension accelerates the decline in renal function and promotes the development of cardiovascular disease, proper management of hypertension in patients with chronic kidney disease is of paramount importance14,15. Although the importance of controlling blood pressure has been emphasised, more than 60% of patients who are hypertensive fail to adequately lower their blood pressure to the target level16.
Recently, Nakayama et al. developed a novel method to create an H2-enriched dialysate by reverse osmosis of H2 formed via the electrolysis of purified tap water, and demonstrated that compared to haemodialysis with standard dialysate, dialysis with H2-enriched dialysate improves blood pressure control in patients on chronic maintenance haemodialysis17,18. The influence of H2 on blood pressure was apparent only in patients with a post-dialysis systolic blood pressure higher than 140 mmHg.
Based on the evidence of this clinical trial, we investigated whether H2 exerts an anti-hypertensive effect in a rat model of hypertension.
Results
Development of a titrated H2 inhalation system
To determine the appropriate H2 flow rate, we estimated that the respiratory parameters of a rat were as follows: tidal volume, 2 mL; respiratory rate, 115 per minute; and expiratory CO2 concentration, 4%. Based on these parameters, we estimated the volume per minute as 0.23 L/min, with a CO2 excretion volume of 9.2 × 10–3 L/min. Stipulating the allowable CO2 concentration in the box to be less than 0.1% resulted in a calculated required gas flow rate of > 9.2 L/min; we therefore used a gas flow rate of 10 L/min. We tested the homogeneity of the gas flow in the box by flowing pure nitrogen gas at 10 L/min and measuring the O2 concentration at nine different locations. We found that O2 concentration decreased more rapidly near the outlet of the box (i.e. areas 3, 4, 7, and 8; Fig. 1a) than in the other areas (Fig. 1b). To resolve this inhomogeneity, we drilled holes on both sides of the box, which yielded a uniform rate of decrease in O2 concentration in all locations (Fig. 1c). In addition, approximately 2 min were required for the O2 concentration to reach 0%, indicating that at least 2 min are required for purging before a stable gas concentration is obtained. When the gas mixture of 1.3% H2 and 21% O2 in N2 was injected into the box, the H2 concentration was uniform in all areas, reaching 1.3% approximately 2 min from the start of gas flow (Fig. 1d).
Schematic for developing a titrated H2 inhalation device. (a) A portable gas detector was placed at nine areas of an anaesthetic box (indicated by circled numbers) and the gas concentrations were measured. A total of 10 holes were drilled on two sides of the box to improve the homogeneity of the gas concentration. (b) Results of O2 concentration measurement before the holes were drilled. The concentration decreased faster at areas closer to the gas outlet. (c) Results of O2 concentration measurement after 10 holes were drilled on two sides of the box. With the holes, the decrease in the oxygen concentration became uniform among all nine areas. (d) H2 concentration after starting injection. H2 concentration increased uniformly in all areas and the air in the box was replaced by injected H2 after 2 min.
One-hour daily H2 therapy for 4 weeks suppresses blood pressure elevation in 5/6 nephrectomised rats
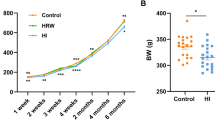
Rats were subjected to sham operation (Sham) or 5/6 nephrectomy (5/6 Nx). Post–5/6 Nx rats were randomised into two groups: 1-h daily exposure to H2 (5/6 Nx + H2) and control (control 5/6 Nx) for 4 weeks (Supplementary Fig. S1a). The one-stage 5/6 Nx conducted by a skilled surgeon using microsurgery yielded reproducible results with very little error, as evidenced by the fact that the levels of renal injury were uniform among individuals (Supplementary Fig. S1b–e). The two groups did not differ in the time course of changes in urine volume (Supplementary Fig. S1b), creatinine clearance (Supplementary Fig. S1c), blood urea nitrogen (BUN) (Supplementary Fig. S1d), creatinine (Supplementary Fig. S1e), or left kidney weight (Supplementary Fig. S1f.). Notably, the 5/6 Nx + H2 group showed faster postoperative weight recovery than the control 5/6 Nx (P = 0.08), although the difference in body weight between the two groups disappeared after 4 weeks (Supplementary Fig. S1g). The arterial blood pressure, measured with a pressure transducer placed at the right femoral artery 4 weeks after 5/6 Nx, was significantly lower in the 5/6 Nx + H2 group than in the control 5/6 Nx group (Supplementary Fig. S1h–j). These results suggest that 1-h daily H2 therapy can suppress the blood pressure increase after 5/6 Nx without affecting the level of renal impairment.
Anti-hypertensive effect of H2 therapy occurs even with delayed treatment
Blood pressure may have decreased because H2 reduced inflammation associated with the nephrectomy. To test this hypothesis, we examined whether the blood pressure–lowering effect persisted even when H2 inhalation was started 3 weeks after 5/6 Nx. Blood pressure was measured weekly using a tail cuff. Thirty-four rats were subjected to 5/6 Nx; of these, 4 rats whose mean blood pressure did not increase to 105 mmHg or more 3 weeks after 5/6 Nx were excluded from subsequent experiments. The remaining 30 rats were randomly assigned to treatment and control groups (Fig. 2a). Four weeks of 1-h daily H2 therapy significantly lowered systolic and mean blood pressure compared with the control group (Fig. 2b–d). It also showed a tendency to decrease the heart rate, although the difference between the 2 groups was not significant (Fig. 2e).
H2 therapy exerts an anti-hypertensive effect even when started 3 weeks after 5/6 nephrectomy. (a) Experimental protocol for measuring the effect of delayed administration of H2 on blood pressure in 5/6 nephrectomised (5/6 Nx) rats. 5/6 Nx was performed on rats (N = 34) 3 weeks prior to starting gas inhalation. Rats were randomly divided to H2 (N = 15) and control (N = 15) groups on the first day of gas inhalation (day 0). Four rats which did not develop hypertension were excluded from this experiment. Daily 1-h gas inhalation was continued for 4 weeks. (b) Systolic BP, (c) mean BP, (d) diastolic BP, and (e) heart rate. Haemodynamic parameters were measured weekly using the tail-cuff method (white arrowhead). BP blood pressure, bpm beats per min, LEW Lewis rats, Nx nephrectomy. Data are expressed as the mean ± SE. N = 15 in each group. Mixed effect model *P < 0.05, **P < 0.01.
H2 alleviates autonomic nervous system imbalance in 5/6 nephrectomised rats
To examine the anti-hypertensive effect of H2 in more detail, we conducted chronic and continuous monitoring of blood pressure using a non-invasive method with a wireless implantable telemetry system (Fig. 3a). Gas inhalation was started on the day of 5/6 Nx and continued for 4 weeks. Again, there was no difference in the time course of change in renal function between the two groups (Supplementary Fig. S2a,b). A longer period of gas inhalation led to a greater decrease in blood pressure in the 5/6 Nx + H2 group, compared to in the control 5/6 Nx group (P < 0.05) (Fig. 3b). As treatment continued, the trend towards a lower heart rate became more pronounced in the 5/6 Nx + H2 group, but the difference was not significant (Fig. 3c).
Anti-hypertensive effect of H2 is associated with an improvement in autonomic nervous system dysfunction. (a) Experimental protocol for non-invasive continuous blood pressure monitoring using wireless implantable telemetry in 5/6 nephrectomised (5/6 Nx) rats. The telemetry transmitter was implanted 1 week before the 5/6 Nx. Daily gas inhalation was initiated immediately after the 5/6 nephrectomy (Nx) (day 0) and was continued for 4 weeks. Haemodynamic monitoring was performed weekly using a telemetry system. The continuously monitored 60 min of blood pressure and heart rate, which were recorded 6 h after inhalation treatment was ceased, were used as resting-state daytime data. The 60 min recorded between 1:30 and 2:30 AM (the middle of the dark cycle) were used as the active-state night-time data. The day on which gas inhalation was initiated was defined as day 0. Thus, the daytime blood pressure on day 0 represents the blood pressure at 6 h after H2 inhalation, and the night-time blood pressure on day 0 represents the blood pressure between 1:30 and 2:30 AM before starting H2 inhalation. (b–e) Telemetry recordings of haemodynamic parameters during the light cycle. (b) Time course of change in mean arterial pressure (MAP) and (c) heart rate. (d) Change (Δ) in low-frequency (LF) power and, (e) high-frequency (HF) power from the first day to 4 weeks after nephrectomy. LFnu low-frequency power in normalised units (nu), HFnu high-frequency power in normalised units, TTI telemetry transmitter implantation. Data are expressed as the mean ± SE. Mixed effect model for MAP and heart rate analysis, *P < 0.05; paired-t test for blood pressure variability analysis, †P < 0.05. (f–i) Telemetry recordings during the dark cycle. (f) Time course of change in MAP, (g) heart rate, (h) LF power, and (i) HF power. Mixed effect model, *P < 0.05.
To examine the influence of H2 therapy on autonomic nervous system activity, we conducted spectral analysis of blood pressure variability. Spectral components were obtained in normalised units (nu). Low-frequency (LF) power indicates a predominantly sympathetic tone, whereas high-frequency (HF) indicates a mostly parasympathetic tone. Although the increase in LF power and decrease in HF power over time associated with 5/6 Nx showed a tendency to be suppressed by H2 inhalation, the results were not significant when compared as continuous variables over a 4-week time course (Supplementary Fig. S2c,d). In contrast, comparing the change from the baseline (day 0) to 4 weeks after starting H2 inhalation, the increase in LF power and decrease in HF power observed in the control 5/6 Nx group was significantly suppressed in the 5/6 Nx + H2 group (Fig. 3d,e).
Next, we examined whether 1-h daily H2 therapy affected blood pressure, heart rate, and autonomic nervous activity even during the nocturnal active period. We analysed 60 min of blood pressure and heart rate data recorded between 1:30 and 2:30, which is in the middle of the dark phase (from 21:00 to 7:00 of the next day). A longer treatment period led to greater reductions in blood pressure, heart rate, and LF power and increases in HF power in the 5/6 Nx + H2 group compared to in the control 5/6 Nx group (Fig. 3f–i).
Discussion
This is the first study to experimentally demonstrate the pharmacological effects of H2 on hypertension in rats. We found that exposing 5/6 Nx rats to 1.3% H2 for 1 h per day for 4 weeks significantly suppressed increases in blood pressure due to 5/6 Nx.
H2 may have reduced blood pressure solely by mitigating local inflammation in the kidney caused by the 5/6 Nx. We tested this by repeating the experiment in rats that had fully recovered from surgical invasion. H2 inhalation treatment was started at 3 weeks after 5/6 Nx and continued for 4 weeks; blood pressure was measured weekly throughout this period with a tail cuff. Our results confirmed that H2 significantly reduced blood pressure in 5/6 Nx rats in the chronic phase, supporting that H2 has an anti-hypertensive effect independent of its anti-inflammatory properties during the perioperative phase.
To investigate the effect of H2 on blood pressure in more detail, we used an implanted telemetry system to continuously monitor blood pressure. This experiment revealed that H2 exerts its anti-hypertensive effect not only during daytime rest, but also during the nocturnal active phase. Our spectral analysis of blood pressure variability revealed that H2 mitigated the autonomic imbalance resulting from 5/6 Nx, namely by supressing the over-active sympathetic nervous system and augmenting parasympathetic nervous system activity; this effect was coincident with its blood pressure-lowering effects.
Our previous study suggested that inhaled H2 lowers blood pressure by acting directly on the brain. Most recently, we measured H2 dynamics in the blood of pigs after a single breath of H219. Our experimental results showed that H2 was not simply diffused from the lungs but was efficiently transported through the arterial bloodstream to organs throughout the body, where it was dynamically metabolised. Inhalation of H2 increased the concentration of H2 in the carotid bloodstream to a higher concentration than anywhere else in the body. These observed dynamics for the H2 concentration in the blood after H2 inhalation suggested that its blood pressure–lowering effect was exerted via a direct impact on the brain.
Accumulating evidence indicates that hypertension in 5/6 Nx rats is mediated through increased sympathetic nerve activity elicited by the pathogenic interaction between the kidney and brain. It has been reported that the turnover rate of norepinephrine from the posterior hypothalamic nuclei was greater in 5/6 Nx rats than in control rats20. Bilateral dorsal rhizotomy has been shown to prevent increases in blood pressure and norepinephrine turnover in posterior hypothalamic nuclei21. These results indicate that increased renal sensory impulses are generated in the injured kidney and transmitted to the brain, where they excite vasomotor centres, which in turn activate efferent sympathetic nerve activity to the cardiovascular system and kidneys and lead to the development of hypertension22,23. Our results show that H2 exerted an anti-hypertensive effect without affecting the levels of 5/6 Nx–related renal dysfunction; this supports the conclusion that H2 acted directly on the brain rather than by reducing the generation of renal sensory impulses.
The therapeutic potential of H2 in humans is highly promising, but the research is still in its early stages. Anecdotal reports of H2 balancing the autonomic nervous system have been used in the sale of H2-related merchandise. H2 has been advertised to improve numerous conditions including autonomic neuropathy, insomnia, depression, stiff shoulders, headaches, loss of appetite, and stress-related diseases. None of these effects have been experimentally demonstrated; this is the first experimental study to show that H2 improves autonomic imbalance. However, these effects have not been demonstrated in humans, and the mechanism by which this effect is achieved remains unknown. Our preclinical research and clinical studies previously demonstrated that H2 reduces organ damage caused by ischemia–reperfusion in various medical emergency situations, including myocardial infarction2,24, haemorrhagic shock5,25, and out-of-hospital cardiac arrest3,4, as well as in organ transplantation26. Selective hydroxyl radical scavenging (•OH) has been widely accepted as the most likely mechanism of action of H2. Although H2 has been shown to selectively eliminate •OH in a test tube27, whether H2 reduces oxidative stress by eliminating •OH at the cellular and tissue levels remains unclear.
Activation of sympathetic nerves can lead to high blood pressure. Hirooka et al. showed that one brain region, the rostral ventrolateral medulla (RVLM), is important for the activation of sympathetic nerves, with a decrease in nitric oxide activity and increase in the production of ROS in RVLM as its possible mechanisms28,29,30. Campese et al. also showed that increased ROS production occurs in the brain during central sympathetic activation, which occurs during kidney injury31,32. H2 may suppress central sympathetic activity by scavenging ROS in the RVLM, thereby lowering the blood pressure and heart rate.
Although not the focus of our study, it is worth noting that postoperative H2 treatment reduced the degree of weight loss and promoted weight recovery after nephrectomy. Postoperative weight loss in humans contributes to poor prognosis by increasing the likelihood of complications and weakening the effectiveness of chemotherapy. Our results suggest that if these effects occur in humans, postoperative administration of H2 may shorten the length of hospital stays and improve the prognosis of patients after a variety of surgeries.
Our study has several limitations. First, insertion of the implanted telemetry system is a stressful procedure for rats and thus may have affected the variability in blood pressure and heart rate in. In addition, environmental factors such as sounds or odours33 may not have been completely eliminated when the measurements were taken. Third, further studies are needed to determine the optimum concentration of H2 and optimise the time of inhalation. Fine-tuning of the concentration of H2 required for different therapeutic outcomes will be required. Although concentrations of 1.3–4% have mostly been used in clinical trials relying on H2 inhalation, an increase in capillary blood flow has been observed by nail capillary microscopy even when inhaling much lower concentrations of H2 and after drinking H2-rich water. The amount of H2 required may vary depending on the biological effects being targeted. As this is the first study to investigate the therapeutic effects of H2 on hypertension, we used H2 with a sufficiently high concentration (1.3%) to ensure that any effect was detected. In fact, the maximum H2 concentration allowed under Japanese regulation to be added to a cylinder containing O2 is 1.3%, which is a third of the lower flammability limit of 4%. Our results revealed that at least 1 h of H2 inhalation per day was required to observe haemodynamic changes; however, whether inhalation of H2 for a longer time has a better effect should be further evaluated. Finally, additional studies are required to elucidate the versatility of H2 on blood pressure in other animal models of hypertension.
In conclusion, our study showed that daily 1-h H2 therapy lowered blood pressure in a rat model of hypertension and improved the imbalance of the autonomic nervous system caused by hypertension. Additional pre-clinical studies are required before the translational research.
Methods
Animals
Male Lewis rats (age, 8 weeks old; body weight, 250–300 g) were used (CLEA Japan, Tokyo, Japan). Animals were fed standard chow ad libitum with free access to water and were not fasted prior to the experiments. Animals were housed under standardised temperature (22 ± 1 °C) and humidity (55 ± 5%) conditions with a 14-h:10-h light: dark cycle. The rats were allowed to acclimatise to the above-mentioned conditions for a minimum of 1 week prior to the experiments. The study was approved by the Institutional Animal Care and Use Committee (Nippon Veterinary and Life Science University [Tokyo, Japan], No. 30 K-61; and Keio University [Tokyo, Japan], No. 13002-4). Allocation to the H2 and control groups was performed randomly. All animal experiments were performed in accordance with ARRIVE guidelines34.
Development of H2 inhalation apparatus
We sought to establish a precisely titrated H2 inhalation system that simultaneously allowed gas inhalation and ambulatory blood pressure monitoring. We used an anaesthetic box (KN-1010 M, Natsume, Tokyo, Japan) for gas administration. The oxygen concentration was measured using a portable complex gas detector (GX-8000, Riken Keiki Co., Ltd., Tokyo, Japan) at nine areas in the box (Fig. 1a). Pure nitrogen gas (Taiyo Nippon Sanso Corporation, Tokyo, Japan) was flowed into the box at a rate of 10 L/min, and the oxygen concentration was recorded in the nine areas every 5 s until the oxygen concentration reached 0% v/v. To reset the experimental space, the box was opened for ventilation after each measurement, and measurements were repeated three times in each area. To achieve uniform filling of the box with gas, holes with a 2-mm diameter were drilled at five locations on both sides of the box to create a total of 10 holes, and the same test was repeated. Finally, 10 L/min of H2 gas (1.3% H2 + 21.0% O2 + 77.7% N2) (Taiyo Nippon Sanso Corporation, Tokyo, Japan) was flowed and H2 and O2 concentrations were measured at nine areas in the box using a GX-2009 detector (GX-2009, Riken Keiki Co., Ltd., Tokyo, Japan). We confirmed that the inside of the box was uniformly filled with the mixed gas.
Gas inhalation
Gas cylinders for injection into the anaesthetic box were filled with H2 gas (1.3% H2 + 21.0% O2 + 77.7% N2) and control gas (21.0% O2 + 79.0% N2) at a factory (Taiyo Nippon Sanso Corporation, Tochigi, Japan). The H2 group and control group inhaled the premixed H2 gas and control gas, respectively. The gas flow rate was 10 L/min and the animals were kept in the box for 1 h at a time. An additional 3 min was set for purging the box (i.e. 63 min in total). In all experimental protocols, the day on which the gas inhalation was initiated was uniformly defined as day 0. The treatment was repeated every day for 4 weeks.
Surgical procedure for partial nephrectomy
To induce renal hypertension, 5/6 nephrectomy was performed as previously described35,36,37, with minor modifications. Briefly, the rats were anaesthetised via isoflurane inhalation (induction at 4%, maintained at 1.5%), and an upper median laparotomy of approximately 4 cm was performed. Surgical procedures were carried out under a microscope; the branches of the left renal artery were identified and then selectively ligated with 7–0 silk sutures as close to the left kidney as possible to grossly infarct approximately 2/3 of the left renal cortex. Subsequently, the right renal artery, renal vein, and ureter were ligated with 4–0 silk sutures and the right kidney was resected. The abdominal wall and skin were closed with 4–0 nylon thread. Sham-operated rats were subjected to the same laparotomy as 5/6 Nx except that surgical interventions to the kidneys was not performed. The anaesthesia time was 30 min, which was uniform for all rats.
Blood pressure measurement
In the first experiment, arterial blood pressure was measured at the right femoral artery using a pressure transducer (PE50, Natsume, Tokyo, Japan; DX-360, Nihon Kohden, Tokyo, Japan) after 4 weeks of gas inhalation under anaesthesia induced by isoflurane inhalation. In the second experiment, blood pressure and heart rate were measured by the tail cuff manometry (BP-98A, Softron, Tokyo, Japan) method. Blood pressure and heart rate were measured in triplicate, and the median value was used as the representative value for that individual.
Implantation of telemetry transmitter
Rats were anaesthetised using isoflurane and the left groin was disinfected with 1% chlorhexidine. An incision of approximately 1.5 cm was made and the left femoral artery was exposed. A telemetric transmitter (HD-S10, Physiotel HD Telemetry, Data Science International, St. Paul, MN, USA) catheter was inserted into the left femoral artery38. The tip of the transmitter catheter was placed in the abdominal aorta caudally from the renal artery bifurcation. The transmitter body was inserted into a subcutaneous pocket created on the left lower back, and the skin was sutured. All surgical interventions were performed in an aseptic manner.
Continuous haemodynamic parameter monitoring
Blood pressure and heart rate were continuously monitored using a telemetry system (Ponemah Ver. 6.3, Data Science International, St. Paul, MN, USA). Data were recorded for 60 min in a breeding cage. Blood pressure data obtained at 1 and 6 h after stopping inhalation were used for analysis. If this measured value was a significant outlier compared to the other measurements of the same individual on the same day, the data obtained from the hour before inhalation were used instead. Of the recorded data, those acquired within the first 15 min of each measurement period were excluded from analysis. Data retrieved in the remaining 45 min were divided into 5-min blocks. Blood pressure and heart rate display great fluctuations when the rats move; thus, in each 5-min data block, the values in the first 1 min of stable measurement were recorded and averaged. Stable measurement was defined as data without body movement and without any parts missing due to loss of signal; if these conditions were not met, the data were considered as invalid. Within each 5-min block, if the data of the first minute was deemed as invalid, data from the following minute were used. In the rare cases in which all single-minute intervals within the 5-min block were invalid, the data from that block were discarded completely.
Spectral analysis of arterial blood pressure variability
Arterial blood pressure variability was analysed using a telemetry system software (Ponemah Ver. 6.3, Data Science International, St. Paul, MN, USA). Frequency domain analysis (500 Hz sampling rate; very low frequency [VLF], 0.05–0.25 Hz; LF, 0.25–1.0 Hz; HF, 1.0–3.0 Hz) was performed using arterial pressure waveform data of the first minute (approximately 300–400 beats) every 5 min. Similar to the method employed for evaluating haemodynamic parameters, in case there was a body movement or any missing data due to loss of signal, the next minute was used, and if all single-minute intervals of the 5-min block were invalid, data from that block were discarded.
Renal function measurement in 5/6 nephrectomy rats
Renal function was assessed before, one day after nephrectomy, and weekly by using a handheld blood analyser (i-STAT cartridge CHEM8 + , Abbott Japan, Chiba, Japan; i-STAT analyser, Abbott, Chicago, IL, USA). Daily urine volume was measured weekly using a metabolic cage (KN-646, Natsume, Tokyo, Japan) and creatinine clearance (mL/min/kg BW) was calculated. The left kidney weight was measured at the end of the experiment after 4 weeks of gas inhalation.
Statistical analysis
Descriptive statistics are presented as the mean ± standard error of mean. Comparisons were conducted using analysis of variance, unpaired t-test, paired t-test, or Mann–Whitney U-test, as appropriate. The Tukey’s multiple comparison test was followed by analysis of variance. The mixed-effect model was used to analyse the repeated measures. All tests were two-tailed, and a P value < 0.05 was considered as statistically significant. All statistical analyses were conducted using GraphPad Prism 8.0 (GraphPad Software, Inc., La Jolla, CA, USA).
Data availability
The datasets generated and/or analysed during the current study are available from the corresponding author upon reasonable request.
References
Sano, M. et al. Promising novel therapy with hydrogen gas for emergency and critical care medicine. Acute Med. Surg. 5, 113–118 (2018).
Hayashida, K. et al. Inhalation of hydrogen gas reduces infarct size in the rat model of myocardial ischemia–reperfusion injury. Biochem. Biophys. Res. Commun. 373, 30–35 (2008).
Hayashida, K. et al. H2 gas improves functional outcome after cardiac arrest to an extent comparable to therapeutic hypothermia in a rat model. J. Am. Heart Assoc. 1, e003459. https://doi.org/10.1161/JAHA.112.003459 (2012).
Hayashida, K. et al. Hydrogen inhalation during normoxic resuscitation improves neurological outcome in a rat model of cardiac arrest independently of targeted temperature management. Circulation 130, 2173–2180 (2014).
Matsuoka, T. et al. Hydrogen gas inhalation inhibits progression to the “irreversible” stage of shock after severe hemorrhage in rats. J. Trauma Acute Care Surg. 83, 469–475 (2017).
Katsumata, Y. et al. The effects of hydrogen gas inhalation on adverse left ventricular remodeling after percutaneous coronary intervention for ST-elevated myocardial infarction: first pilot study in humans. Circ. J. 81, 940–947 (2017).
Tamura, T. et al. Feasibility and safety of hydrogen gas inhalation for post-cardiac arrest syndrome: first-in-human pilot study. Circ. J. 80, 1870–1873 (2016).
Tamura, T., Hayashida, K., Sano, M., Onuki, S. & Suzuki, M. Efficacy of inhaled HYdrogen on neurological outcome following BRain Ischemia During post-cardiac arrest care (HYBRID II trial): study protocol for a randomized controlled trial. Trials 18, 488. https://doi.org/10.1186/s13063-017-2246-3 (2017).
Chinese Non-government Medical Institutions Association. Recommendation for hydrogen-oxygen nebulizer: notice of clinical treatment for novel coronavirus pneumonia. https://www.cnmia.org/NoticeDetail_69B3504FE9124BF3AA2C4FBA0E3F8234.html. (Accessed April 8, 2020) .
Guan, W. J. et al. Hydrogen/oxygen mixed gas inhalation improves disease severity and dyspnea in patients with Coronavirus disease 2019 in a recent multicenter, open-label clinical trial. J. Thorac. Dis. 12, 3448–3452 (2020).
NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in blood pressure from 1975 to 2015: a pooled analysis of 1479 population-based measurement studies with 19.1 million participants. Lancet 389, 37–55 (2017).
The Global Burden of Metabolic Risk Factors for Chronic Diseases Collaboration. Cardiovascular disease, chronic kidney disease, and diabetes mortality burden of cardiometabolic risk factors from 1980 to 2010: a comparative risk assessment. Lancet Diabetes Endocrinol. 2, 634–647 (2014).
Saran, R. et al. US Renal Data System 2018 Annual Data Report: epidemiology of kidney disease in the United States. Am. J. Kidney Dis. 73, Svii–Sxxii (2019).
Schiffrin, E. L., Lipman, M. L. & Mann, J. F. E. Chronic kidney disease: effects on the cardiovascular system. Circulation 116, 85–97 (2007).
Wuhl, E. & Schaefer, F. Managing kidney disease with blood-pressure control. Nat. Rev. Nephrol. 7, 434–444 (2011).
Mills, K. T. et al. Global disparities of hypertension prevalence and control: a systematic analysis of population-based studies from 90 countries. Circulation 134, 441–450 (2016).
Nakayama, M. et al. A novel bioactive haemodialysis system using dissolved dihydrogen (H2) produced by water electrolysis: a clinical trial. Nephrol. Dial. Transplant. 25, 3026–3033 (2010).
Nakayama, M. et al. Novel haemodialysis (HD) treatment employing molecular hydrogen (H2)-enriched dialysis solution improves prognosis of chronic dialysis patients: A prospective observational study. Sci. Rep. 8, 254. https://doi.org/10.1038/s41598-017-18537-x (2018).
Sano, M. et al. Pharmacokinetics of a single inhalation of hydrogen gas in pigs. PLoS ONE 15, e0234626. https://doi.org/10.1371/journal.pone.0234626 (2020).
Bigazzi, R., Kogosov, E. & Campese, V. M. Altered norepinephrine turnover in the brain of rats with chronic renal failure. J. Am. Soc. Nephrol. 4, 1901–1907 (1994).
Campese, V. M. & Kogosov, E. Renal afferent denervation prevents hypertension in rats with chronic renal failure. Hypertension 25, 878–882 (1995).
Sano, M. & Goto, S. Possible mechanism of hematocrit elevation by sodium glucose cotransporter 2 inhibitors and associated beneficial renal and cardiovascular effects. Circulation 139, 1985–1987 (2019).
Sano, M. Inter-organ communication pathway manifested by non-physiological stress to the kidney in type II diabetic patients -why are diabetic patients prone to develop heart failure?. Intern. Med. 59, 1–5 (2020).
Yoshida, A. et al. H2 mediates cardioprotection via involvements of KATP channels and permeability transition pores of mitochondria in dogs. Cardiovasc. Drugs Ther. 26, 217–226 (2012).
Tamura, T. et al. Hydrogen gas inhalation attenuates endothelial glycocalyx damage and stabilizes hemodynamics in a rat hemorrhagic shock model. Shock https://doi.org/10.1097/SHK.0000000000001459 (2019).
Kobayashi, E. & Sano, M. Organ preservation solution containing dissolved hydrogen gas from a hydrogen-absorbing alloy canister improves function of transplanted ischemic kidneys in miniature pigs. PLoS ONE 14, e0222863. https://doi.org/10.1371/journal.pone.0222863 (2019).
Ohsawa, I. et al. Hydrogen acts as a therapeutic antioxidant by selectively reducing cytotoxic oxygen radicals. Nat. Med. 13, 688–694 (2007).
Hirooka, Y. Oxidative stress in the cardiovascular center has a pivotal role in the sympathetic activation in hypertension. Hypertens. Res. 34, 407–412. https://doi.org/10.1038/hr.2011.14 (2011).
Hirooka, Y., Kishi, T., Sakai, K., Takeshita, A. & Sunagawa, K. Imbalance of central nitric oxide and reactive oxygen species in the regulation of sympathetic activity and neural mechanisms of hypertension. Am. J. Physiol. Regul. Integr. Comp. Physiol. 300, R818-826. https://doi.org/10.1152/ajpregu.00426.2010 (2011).
Kishi, T. et al. Increased reactive oxygen species in rostral ventrolateral medulla contribute to neural mechanisms of hypertension in stroke-prone spontaneously hypertensive rats. Circulation 109, 2357–2362. https://doi.org/10.1161/01.CIR.0000128695.49900.12 (2004).
Campese, V. M. et al. Reactive oxygen species stimulate central and peripheral sympathetic nervous system activity. Am. J. Physiol. Heart Circ. Physiol. 287, H695-703. https://doi.org/10.1152/ajpheart.00619.2003 (2004).
Ye, S., Zhong, H., Yanamadala, S. & Campese, V. M. Oxidative stress mediates the stimulation of sympathetic nerve activity in the phenol renal injury model of hypertension. Hypertension 48, 309–315. https://doi.org/10.1161/01.HYP.0000231307.69761.2e (2006).
Sorge, R. E. et al. Olfactory exposure to males, including men, causes stress and related analgesia in rodents. Nat. Methods 11, 629–632 (2014).
Kilkenny, C., Browne, W. J., Cuthill, I. C., Emerson, M. & Altman, D. G. Improving bioscience research reporting: the ARRIVE guidelines for reporting animal research. PLOS Biol. 8, e1000412. https://doi.org/10.1371/journal.pbio.1000412 (2010).
Griffin, K. A., Picken, M. & Bidani, A. K. Method of renal mass reduction is a critical modulator of subsequent hypertension and glomerular injury. J. Am. Soc. Nephrol. 4, 2023–2031 (1994).
El Nahas, A. M., Bassett, A. H., Cope, G. H. & Le Carpentier, J. E. Role of growth hormone in the development of experimental renal scarring. Kidney. Int. 40, 29–34 (1991).
Zhang, Y. & Kompa, A. R. A practical guide to subtotal nephrectomy in the rat with subsequent methodology for assessing renal and cardiac function. Nephrology (Carlton) 19, 552–561 (2014).
Sugai, K. et al. A microsurgical technique for catheter insertion in the rat femoral artery. Acta Cir Bras 35, e202001004. https://doi.org/10.1590/s0102-865020200100000004 (2020).
Acknowledgements
This study was supported by the Japan Society for the Promotion of Science (KAKENHI [Number: 16K11420]) (M. Suzuki) and a research grant from Taiyo Nippon Sanso Corporation (no identifiable grant number) (M. Sano). The funders had no role in the study design, data collection, analysis, writing of the manuscript, or the decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Contributions
M.Sano., E.K., and Y.H. conceived the experiments; K.S., T.T., S.U., M.F., E.K., and Y.H. conducted the experiments; K.S. and T.T. analysed the results; M.Sano. and T.T. wrote the manuscript; and J.Y., Y.K., J.E., K.H., M.Suzuki., M.Sano., J.S., and Y.H. critically revised the manuscript. All authors reviewed the manuscript and consented to its publication.
Corresponding authors
Ethics declarations
Competing interests
M. Sano receives advisory fees and commissioned research fees from Taiyo Nippon Sanso Co., Ltd. And Doctors Man Co., Ltd.; M. Suzuki received advisory fees and commissioned research fees from the Taiyo Nippon Sanso Co., Ltd. E.K receives advisory fees and commissioned research fees from Doctors Man Co., Ltd. Other authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sugai, K., Tamura, T., Sano, M. et al. Daily inhalation of hydrogen gas has a blood pressure-lowering effect in a rat model of hypertension. Sci Rep 10, 20173 (2020). https://doi.org/10.1038/s41598-020-77349-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-77349-8
This article is cited by
-
Impact of hemodialysis solutions containing different levels of molecular hydrogen (H2) on the patient-reported outcome of fatigue
Renal Replacement Therapy (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.