Abstract
The exponential character of the recent Covid-19 outbreak requires a change in strategy from containment to mitigation. Meanwhile, most countries apply social distancing with the objective to keep the number of critical cases below the capabilities of the health care system. Due to the novelty and rapid spread of the virus, an a priori assessment of this strategy was not possible. In this study, we present a model-based systems analysis to assess the effectiveness of social distancing measures in terms of intensity and duration of application. Results show a super-linear scaling between intensity (percent contact reduction) and required duration of application to have an added value (a lower number of fatalities). This holds true for an effective reproduction of \(R>1\) and is reverted for \(R<1\). If R is not reduced below 1, secondary effects of required long-term isolation are likely to unravel the added value of disease mitigation. If an extinction is not feasible, we recommend moderate social-distancing that is well balanced against capability limits of national health-care systems.
Similar content being viewed by others
Introduction
This article is written in mid-April 2020 where globally the number of confirmed COVID-19 cases is above 2.5 million resulting in over 170,000 deaths1. Due to these large numbers, the initial approach of containment, i.e. tracing contacts of patients with laboratory-confirmed infection2, is not applicable anymore and may even have unintended consequences of hampering effective healthcare delivery3. Instead, the majority of countries decided to use community interventions, like cancellation of events, general social distancing and travel restrictions4.
These community mitigation measures reduce transmission, hence flatten the curve and push the peak of new infections further into the future which eventually helps preventing an epidemic peak that overwhelms health-care systems5. The need for mitigation measures is also evident from the actions taken by European countries who implemented interventions including the closure of schools and universities, banning of mass gatherings, and most recently, widescale social distancing including local and national lockdowns6.
Numerous studies support this strategy3,4,7,8. Applied in the long-term, however, school closure and home confinement will negatively affect children’s health9 and the global economy, to name only two big drawbacks of these measures. In this light, it is of particular interest, for what duration these exceptional interventions must remain in place. According to recent estimates, we are probably at least 1 year to 18 month away from large-scale vaccine production5. Independent of the time it takes to develop a vaccine, the epidemic spread will also come to an end, if sufficient people have been infected to establish herd immunity. Studies on the effectiveness of the concept of disease mitigation with the objective to establish herd immunity shows some potential in the case of pandemic influenza10.
In this study, we present an exploratory and model-based systems analysis that is aimed at investigating the application of social distancing strategies to Covid-19. Specific objectives of this research are: 1) to investigate the effectiveness of contact reduction policies with respect to intensity and duration and 2) to estimate the amount of time to establish herd immunity by considering the national health care systems of Austria and Sweden, which are very different in terms of critical care capabilities (Austria: 21.8 beds Sweden: 5.8 beds per 100k population, respectively)11. A detailed description of model equations, assumptions as well as uncertainty of currently available data are presented in the following section. Data uncertainty is addressed by the analysis of alternative scenario runs to enhance robustness of model results. In a concluding section, we compare our results to similar studies, discuss current limitations of data availability and give recommendations based on exploratory results.
Method
Adapted SIR model
The current scenario of novel pathogen emergence includes considerable uncertainty12. This means that a reliable scientific evidence base on Covid-19 is yet to be established. Under these preconditions, the use of models for exploratory rather than predictive purposes is more appropriate13. Accordingly, the simulation model presented in this study was designed to identify and systematically explore important qualitative behavior of this dynamic system that remains unchanged irrespective of parameter variations. An adaptation of the popular susceptible-infected-resistant (SIR) model turned out to be most suitable for this purpose (see Fig. 1). In order to meet the specific requirements of a simulation model on Covid-19 mitigation, the structure of the original model was adapted accordingly.
For instance, pathological findings of Covid-19 indicate that there is a considerable number of cases that develop mild or no symptoms14. To account for this characteristic, we separated the infected population into those that are asymptomatic and those that are not, which in the latter case leads to isolation or hospitalization. The asymptomatic infected get resistant without prior isolation.
Exponential growth in numbers of infected poses a challenge to health care facilities. In Italy, specialists are already considering denying life-saving care to the sickest and giving priority to those patients most likely to survive15. This will inevitably cause potentially avoidable deaths. In the model, deaths caused by a lack of intensive care is considered independently.
The calculation of population quantities in respective compartments (see Fig. 1) is in line with the logic of the standard SIR model. The model makes the simplified assumption that initially everyone in the total population N is susceptible. The number of susceptible is reduced over time by infections as
where \(i_{r}\) is the infection rate (rate of contacts between uninfected and infected that result in infections) and \(c_{ui}\) is the number of contacts between infected and uninfected, which is calculated as
where \(\hbox {c}_{{d}}\) is the personal contacts per day, S(t) is the susceptible at time t and I(t) is the number of unknown infections. To take account for a lower infection rate of asymptomatic infected, the unknown infections I(t) in equation 2 is substituted by
with IC(t) being the unknown infected corrected for asymptomatic infected, \(a_{f}\) the fraction of asymptomatic among infected and \(a_{p}\) the asymptomatic population’s potential to infect.
The flows from compartment I(t) - i.e. asymptomatic cases getting resistant (see Eq. 5) and isolation of symptomatic infected (see Eq. 4)—are calculated by
Parameter d is the time between infection and isolation (corresponds to the duration of infectiousness) and \(d_{a}\) is the duration of asymptomatic infection. The flows from compartment II(t) are given by
where parameter \(d_{s}\) is the duration of distinct symptomatic sickness, CFR is the case fatality rate and \(ICU_{d}\) and \(ICU_{s}\) is the intensive care demand and supply respectively.
The intensive care demand \(ICU_{d}\) is calculated by taking the critical fraction of infected in isolation II(t). The fraction of infected who are admitted to intensive care is denoted as \(c_{f}\) (see Table 1).
Model inputs and exploration
Despite the novelty of Covid-19, the body of literature on key parameters like basic reproduction, case fatality rates and proportion of asymptomatic cases is quite substantial and growing. The wide range of suggested parameter values, however, poses a considerable challenge to model parametrization. For instance, estimates of the basic reproduction number R0 vary within a range from 1.416 to 4.7117. Part of this variation is explained by geographic variation of population densities as well as by heterogeneous social and cultural habits18.
Moreover, there is uncertainty in the percentage of asymptomatic cases. The outbreak in a smaller isolated population is an opportunity to derive representative numbers by applying comprehensive and repeated laboratory testing. One such example is the outbreak of Covid-19 on board of the Diamond Princess cruise ship. However, given that most of the passengers were 60 years and older, the nature of the age distribution may lead to underestimation of asymptomatic cases if older individuals tend to experience more symptoms19. The assumed age dependence of asymptomatic infection is supported by a screening of pregnant woman admitted for delivery in New York-Presbyterian Allen Hospital between March 22 and April 4, 2020 (n\(=\)215) that show an asymptomatic fraction at presentation of 87.9% among 33 patients who were tested positive for SARS-CoV-220 In a normal population ratios of about 50% asymptomatic carriers of Covid-19 are expected21. The question whether or not asymptomatic carriers are able to infect others is still controversial (e.g.22).
The severity of the disease does also play an important role in estimating the ratio of critically ill patients who need intensive care. According to Chinese statistics, 5% of positively tested patients are admitted to intensive care23. This number was adopted by the World Health Organization24 and other studies (e.g.25), whereas national statistics show significant deviations; e.g. 9 to 11% in Italy15 and 2.2% in Austria26. A potential explanation for these considerable differences is that in Italy a lot of the older population were infected27.
The specific age distributions of affected communities may also show some biasing effect on estimated case fatality rates. Another factor that contributes to regional differences in case fatality is the occupation or over-occupation of available intensive care beds (ICU beds). In a few instances, national critical care capabilities are exceeded by the number of critically ill patients (e.g. Italy and France), which drastically elevates fatality rates. By contrast, the true case fatality rates are lower if theoretically all cases were found by testing the entire population. Accordingly, a lower case fatality rate (CFR) was reported by countries who were effective in extensive testing and maintaining the prevalence of critical cases below critical care capabilities like South Korea28. A higher CFR was reported by countries who refrain from extensive testing and/or are overwhelmed by the pace of new infections like Iran, Italy and others29. In the model, we use the more reliable South Korean figures and simulate the additional fatalities due to the critical care limit based on capability limits of national critical care units (see Eqs. 6 and 7).
Among the parameters in Table 1, the basic reproduction number R0 is the only parameter without explicit representation in the model equations. This parameter is the number of secondary cases, which an infected person produces in a completely susceptible population33. In the absence of asymptomatic infections, R0 in the model is equivalent to the arithmetic product of d the time between infection and isolation, \(c_{d}\) the personal contacts per day and \(\hbox {i}_{{r}}\) the infection rate.
To account for asymptomatic infection, \(R0_{s}\) is modified by the specific duration of infectiousness (\(d_{a}\)) and infection potential (\(a_{p}\)) of asymptomatic infected. This can be expressed as
The numerator scales R0 by the asymptomatic populations’s infectiousness, whereas the denominator scales R0 by the asymptomatic population’s duration of infectiousness.
In response to an epidemic disease outbreak, measures are implemented to reduce contacts between people thereby reducing the reproduction of the disease. This is implemented in the model by lowering the personal contacts per day \(c_{d}\). We refer to this modified reproduction as effective reproduction number R.
The choice of appropriate scenarios is based on parameter uncertainty and model sensitivity. Sensitivity analysis indicate a linear response in model output to variations in CFR and \(c_{f}\), and interestingly non-linear effects in response to variations in R, \(a_{f}\) and \(a_{p}\). Accordingly, the latter variables were selected as scenario parameters (see Table 2).
Moreover, prolonged and intermittent social distancing16 was applied in respective scenarios (see Table 2). Whereas prolonged social distancing is defined by constants \(c_{r}\) and \(d_{m}\) , intermittent social distancing is implemented by dynamic adaptation of contact reduction \(c_{r}\) during simulation runtime dependent on the amount of ICU beds available. If more than 70% of ICU beds are vacant, measures are loosened (daily change of \(c_{r}\) -20% until initial \(c_{d}\) is reached), whereas measures are tightened (daily change of \(c_{r}\) +20% until \(c_{d}=0\) is reached) in case less than 30% of ICU beds are available. The linear adjustment in measures is based on the assumption that a complete lockdown (\(c_{r}=100\%\), \(c_{d}=0\) ) can be removed or implemented within 5 days.
Results and discussion
Effectiveness of contact reduction
An increase in asymptomatic cases will overall increase the potential of the infected population to infect susceptible people, i.e. increase the basic reproduction R0, provided asymptomatic and symptomatic cases have a similar potential to infect. This is due to the extended duration asymptomatic cases remain undetected and thus infectious. The reduction of potentially infective contacts has the opposite effect and thus diminishes R0.
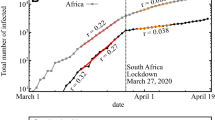
Moreover, the simulation shows that a lowering of the effective reproduction number flattens the curve and delays the peak of new infections, whereas an increase has the opposite effect (see Fig. 2). Consequently, social distancing flattens the curve of daily infections, while higher proportions of asymptomatic cases elevate the peak (provided \(a_{p}=1\) and \(d<d_{a}\)).
This flattening effect can be expressed analytically. The daily infections resemble a normal distribution, which is defined by a mean \(\mu\) (days between outbreak and peak of daily infections) and a standard deviation \(\sigma\). A lower R will lead to a higher \(\mu\) (see Fig. 3) and a higher \(\sigma\) (see Fig. 4). Additionally, the number of initial infected people reduces \(\mu\) (see Fig. 5), whereas \(\sigma\) is independent of it. These inverse relationships can be explained by mechanisms of viral spread. The effective reproduction of the disease at a given time t diminishes with every new infection that depletes the susceptible population (denoted as R(t)). Once R(t) drops below 1, the curve of new infections has passed its peak. In the case where initial effective reproduction R is low, the pool of susceptible individuals is slowly depleted (slow viral spread) and the peak at R(t)\(=\)1 is reached at a later point in time, which produces a flatter curver (high \(\mu\) and \(\sigma\)).
These non-linear relationships have an important impact on the effectiveness of interventions. Social contact reduction and associated reduction in R push new infections further into the future. Hence, the more intense the social distancing measures in terms of contact reduction, the longer the duration needs to be to have an added value; i.e. a lower number of fatalities. In other words, the harder you break, the longer it takes.
For instance, 40% contact reduction needs to be applied for additional 600 days to outperform a 30% contact reduction in scenario 2 (see Fig. 6). The lower the basic reproduction in the scenarios, the larger the time lag associated with an intensification of social distancing (see Fig. 6, scenarios 1, 2, 4, 5 and 6). This is in line with above-mentioned relationships that show increased effects of R on \(\mu\) and \(\sigma\) with lower R.
Given the trade-offs associated with required long-term lockdown, the effectiveness of additional social distancing decreases with R close to 1. The secondary effects of lock down have not been modelled, but it is speculated that reductions in social contacts will increase mortality (e.g. social isolation and homicide; obesity and cardiovascular diseases etc.) making moderate contact reduction more adequate.
Interestingly, if social distancing is intense enough to drop R below one, a further increase in intensity reduces the needed duration of social distancing. For example, in scenario 3 (see Fig. 6), a 30% contact reduction as well as 40% contact reduction push R below one. The 40% contact reduction shows a positive effect (a lower number of fatalities) earlier than the 30% contact reduction. This is contrary to the case of \(R>1\) where the effectiveness of more intense measures is in danger to be unraveled by the super-linear increase in duration.
The curve flattening effect of social contact reduction also explains why drastic contact reduction may cause more deaths than mild contact reduction, if measures are applied for too short time. In the worst case, intense social distancing will hardly have any effect (see Fig. 7).
Duration to establish herd immunity
Intensity and duration are also closely related in the intermittent social distancing and herd immunity scenario (see Fig. 8). The strategic objective in this scenario is to keep the demand for ICU beds within the bounds of ICU supply until herd immunity is established.
In the simulation, the demand for ICU beds behaves like a damped oscillation (see Fig. 8). This is explained by the delay in the system, diminishing number of susceptible people and the negative feedback between number of available ICU beds and social contacts.
In the early phase of the outbreak, the number of patients exceeds the number of available ICU beds due to high reproduction potentials. Higher basic reproduction R0 results in additional over-occupation of ICU capabilities (see Fig. 8, scenario 9 and 10).
Moreover, the variation of available intensive care brings about a shift in the time needed to achieve the strategic objective of herd immunity (compare Sweden and Austria in Fig. 8). This relationship exhibits an almost linear scaling. Furthermore, results show that even under favorable conditions, social distancing and herd immunity strategies require extraordinary endurance.
In Austria, for instance, it is estimated that only 2.2% of confirmed cases are admitted to ICU26. Combined with Austria’s high performance health care system and low effective reproduction, the time to establish herd immunity is still estimated to be about 2 years (see Fig. 9). Given that the ICU beds are also needed for patients other than Covid-19, an even longer period has to be expected.
Conclusion
In this article, we used methods of exploratory systems simulation to assess the effectiveness of social distancing measures in the mitigation of Covid-19. The simulated behavior is governed by a non-linear relationship between the intensity of applied measures (i.e. expressed as reduction of social contacts) and delay in the peak of new infections. As a consequence of this delay, measure intensity scales super-linearly with the required duration of application to show added value; i.e. a lower number of fatalities. Given the large scale of temporal delay (up to multiple years for a 10% increment of additional contact reduction), secondary effects of long-term social isolation such as psychological distress, depression34, and increased mortality35 are likely to unravel the added value of intense social distancing measures. This holds true for effective reproduction numbers above one. Below this threshold, an intensification of measures reduces the required duration of measure application.
In the absence of a vaccination, mitigation strategies are crucial to keep the number of severe and critical cases below the capabilities of the health care system. If the use of mitigation interventions is well balanced against capability limits, the time required to establish herd immunity linearly scales with available capabilities of the health care system (defined by the number of ICU beds in the simulation). Other important factors are the reproduction number and the severity of the disease (expressed by the fraction of cases that need ICU admission). Depending on the calibration of those factors, it is estimated that herd immunity on a national level will be established in more than 2 years from now. This is in line with an agent-based simulation study by36, who indicate a duration of 2 years and 4 months for the Netherlands. According to a deterministic simulation by16 in the United States the epidemic could last into 2022 under current critical care capabilities. Given this timescale, the success of a strategy based on social distancing, delay and herd immunity is unrealistic under known preconditions.
According to37, an extinction strategy implemented by intense countermeasures seems promising. This is supported by our low effective reproduction scenario (\(R<1\)).
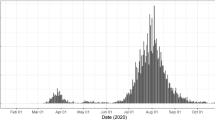
If an extinction is not feasible, interventions should be as moderate as possible. Negative societal and economic consequences associated with drastic social-distancing are likely to undermine a required long-term measure application. The identified super-linear scaling (for \(R>1\)) between intensity and required duration of measure application does amplify this problem. As a result, countries whose policy is exclusively aimed at minimizing the number of cases are in danger of experiencing an untimely termination of countermeasures and a large second wave of outbreaks (compare model output in Fig. 7). Data on government response stringency38 and daily confirmed deaths39 reveal an association between intense measures and large second waves in countries like Albania, Bosnia and Herzegovina, Bulgaria, Egypt, Israel, Palestine, Romania or Serbia (data acquired at the end of August 2020). The probability that more resilient countries will experience similar problems rises every day without vaccination. So far (August 2020), countries like New Zealand or Vietnam did well in containing the virus by an aggressive elimination approach combined with comprehensive international travel restrictions40 and by implementing timely, intense action41 To date, a differentiated assessment of such ambitious policies is primarily constrained by the limited availability of studies on secondary effects of social distancing and isolation in the case of a global pandemic. Similarly, the assessment of more targeted countermeasures such as the selective isolation of vulnerable individuals or approaches of contact tracing and isolation are limited by data scarcity and in part data inconsistency.
For instance, there is little reliable information about age-stratified asymptomatic ratios. Moreover, the impact of country-based measures has hardly been empirically assessed by methods of inferential statistics. While such studies will shed light on important system dependencies, large-scale investment into health care and medical research is essential to spawn game-changing innovation such as the development of vaccines, drugs and affordable test kits.
References
Medicine, J. H. U. Coronavirus COVID-19 Global Cases by the Center for Systems Science and Engineering (CSSE) at JHU [WWW Document]. online (2020).
Ng, Y., Li, Z., Chua, Y. X., Chaw, W. L., Zhao, Z., Er B. et al. Evaluation of the Effectiveness of Surveillance and Containment Measures for the First 100 Patients with COVID-19 in Singapore-January. online (2020).
Parodi, S. M. & Liu, V. X. From Containment to Mitigation of COVID-19 in the US. Jama 323, 1441–1442 (2020).
Ebrahim, S. H., Ahmed, Q. A., Gozzer, E., Schlagenhauf, P. & Memish, Z. A. Covid-19 and Community Mitigation Strategies in a Pandemic (British Medical Journal Publishing Group, London, 2020).
Anderson, R. M., Heesterbeek, H., Klinkenberg, D. & Hollingsworth, T. D. How will country-based mitigation measures influence the course of the COVID-19 epidemic?. The Lancet 395, 931 (2020).
Flaxman, S., Mishra, S., Gandy, A. et al. Estimating the Number of Infections and the Impact of Non-pharmaceutical Interventions on COVID-19 in 11 European Countries. in Imp Coll Prepr (2020).
Preiser, W., van Zyl, G. & Dramowski, A. COVID-19: getting ahead of the epidemic curve by early implementation of social distancing. S. Afr. Med. J. 110, 1 (2020).
Tuite, A., Fisman, D. N. & Greer, A. L. Mathematical modeling of COVID-19 transmission and mitigation strategies in the population of Ontario, Canada. medRxiv (2020).
Brooks, S. K., Webster, R. K., Smith, L. E., Woodland, L., Wessely, S., Greenberg, N. et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. The Lancet 395, 912–920 (2020).
Lugner, A. K. & Postma, M. J. Mitigation of pandemic influenza: review of cost-effectiveness studies. Expert Rev. Pharmacoecon. Outcomes Res. 9, 547 (2009).
Rhodes, A. et al. The variability of critical care bed numbers in Europe. Intensive Care Med. 38, 1647 (2012).
MacGregor, H. Novelty and uncertainty: social science contributions to a response to COVID-19. Somathosphere Sci. Med. Anthropol. 6, 2020 (2020).
Kwakkel, J. H. The exploratory modeling workbench: an open source toolkit for exploratory modeling, scenario discovery, and (multi-objective) robust decision making. Environ. Model Softw. 96, 239 (2017).
Xu, Z. et al. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir. Med. 8, 420–422 (2020).
Remuzzi, A. & Remuzzi, G. COVID-19 and Italy: what next? The Lancet (2020).
Kissler, S. M., Tedijanto, C., Lipsitch, M., Grad, Y. Social distancing strategies for curbing the COVID-19 epidemic. medRxiv (2020).
Shen, M., Peng, Z., Xiao, Y. & Zhang, L. Modelling the epidemic trend of the 2019 novel coronavirus outbreak in China. bioRxiv 10, 23–916726 (2020).
Huynh, T. L. D. Does culture matter social distancing under the COVID-19 pandemic?. Saf. Sci. 104872 (2020).
Mizumoto, K., Kagaya, K., Zarebski, A. & Chowell, G. Estimating the asymptomatic proportion of coronavirus disease 2019 (COVID-19) cases on board the Diamond Princess cruise ship, Yokohama. Jpn. Eurosurveillance 25, 2000180 (2020).
Sutton, D., Fuchs, K., Dalton, M. & Goffman, D. Universal screening for SARS-CoV-2 in women admitted for delivery. N. Engl. J. Med. 382, 2163–2164 (2020).
Rocklov, J. COVID-19 health care demand and mortality in Sweden in response to non-pharmaceutical (NPIs) mitigation and suppression scenarios. medRxiv (2020).
Bai, Y. et al. Presumed asymptomatic carrier transmission of COVID-19. Jama 323, 1406–1407 (2020).
Guan, W., Ni, Z., Hu, Y., Liang, W., Ou, C., He, J. et al. Clinical characteristics of 2019 novel coronavirus infection in China. MedRxiv (2020).
Organization, W. W. H. Health Systems Respond to COVID-19—creating surge capacity for acute and intensive care Recommendations for the WHO European Region. Technical Guidance WHO. 2 (2020).
Grasselli, G., Pesenti, A. & Cecconi, M. Critical care utilization for the COVID-19 outbreak in Lombardy, Italy: early experience and forecast during an emergency response. Jama 323, 1545–1546 (2020).
Hofmarcher, M. & Singhuber, C. Schutzschirm für das Gesundheitswesen in Zeiten von COVID-19. Health Systems Intelligence (2020).
Onder, G., Rezza, G. & Brusaferro, S. Case-fatality rate and characteristics of patients dying in relation to COVID-19 in Italy. Jama 323, 1775–1776 (2020).
Shim, E., Tariq, A., Choi, W., Lee, Y. & Chowell, G. Transmission potential and severity of COVID-19 in South Korea. Int. J. Infect. Dis. 93, 339–344 (2020).
Khafaie, M. A. & Rahim, F. Cross-country comparison of case fatality rates of COVID-19/SARS-COV-2. Osong Public Health Res. Perspect. 11, 74 (2020).
Jung, S. et al. Real-time estimation of the risk of death from novel coronavirus (covid-19) infection: Inference using exported cases. J. Clin. Med. 9, 523 (2020).
Liu, Y., Gayle, A. A., Wilder-Smith, A., & Rocklov, J. The reproductive number of COVID-19 is higher compared to SARS coronavirus. J. Travel. Med. 27, 1–4 (2020).
Koo, J. R., Cook, A. R., Park, M., Sun, Y., Sun, H., Lim, J. T., et al. Interventions to mitigate early spread of SARS-CoV-2 in Singapore: a modelling study. Lancet Infect Dis. 20, 678–688 (2020).
Dietz, K. The estimation of the basic reproduction number for infectious diseases. Stat. Methods Med. Res. 2, 23 (1993).
Hawryluck, L. et al. SARS control and psychological effects of quarantine, Toronto, Canada. Emerg. Infect Dis. 10, 1206 (2004).
Cacioppo, J. T. & Cacioppo, S. Social relationships and health: The toxic effects of perceived social isolation. Soc. Personal. Psychol. Compass. 8, 58 (2014).
de Vlas, S. J. & Coffeng, L. E. A phased lift of control: a practical strategy to achieve herd immunity against Covid-19 at the country level. medRxiv (2020).
Bock, W., Adamik, B., Bawiec, M., Bezborodov, V., Bodych, M., Burgard, J. P., et al. Mitigation and herd immunity strategy for COVID-19 is likely to fail. medRxiv (2020).
Hale, T., Webster, S., Petherick, A., Phillips, T., & Kira, B. Oxford COVID-19 Government Response Tracker, Blavatnik School of Government. online (2020).
ECDC. Data on COVID-19 (coronavirus) by Our World in Data. online (2020).
Cousins, S. New Zealand eliminates COVID-19. The Lancet 395, 1474 (2020).
Huynh, T. L. D. The COVID-19 containment in Vietnam: what are we doing? J. Glob. Health 10 (2020).
Author information
Authors and Affiliations
Contributions
N.C. conducted simulations and wrote the main manuscript text G.C. conducted analytical calculus, prepared the figures and formatted the text. M.T. proofread the mansucript and helped developing the model.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Neuwirth, C., Gruber, C. & Murphy, T. Investigating duration and intensity of Covid-19 social-distancing strategies. Sci Rep 10, 20042 (2020). https://doi.org/10.1038/s41598-020-76392-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-76392-9
This article is cited by
-
Investigation of turning points in the effectiveness of Covid-19 social distancing
Scientific Reports (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.