Abstract
Renal cyst is a common disease in humans and laparoscopic renal cyst decortication is the gold standard for treatment. However, specialized surgical skills are required for the treatment of renal parapelvic cysts. In this study, we describe an improved laparoscopic method for the treatment of renal parapelvic cysts involving the use of continuous infusion of methylene blue. Sixteen patients with renal parapelvic cyst were enrolled in this study. All patients underwent retrograde ureteral catheterization, with continuous perfusion of the renal pelvis using a solution of 0.2% methylene blue and saline, during laparoscopic decortication of the parapelvic cyst. In one patient, the cyst communicated with the renal collection system which was injured, but this was immediately repaired intraoperatively. All operations were successful, and none was converted to open surgery. There were no occurrences of persistent urinary fistula, bleeding, or other complications postoperatively. All patients were followed-up for 3–24 months, and results of postoperative imaging investigations revealed that all of our patients experienced either complete recovery or a greater than 50% decrease in size of the cysts. Our study demonstrates that methylene blue-assisted laparoscopic treatment is a safe, effective and practical method for the treatment of renal parapelvic cysts.
Similar content being viewed by others
Introduction
Renal cysts are the most common lesion of the kidney1, with a prevalence of 20–50% in the general population2. The incidence of renal cysts increases with age3. Most are simple renal cysts and are often asymptomatic. By comparison, renal parapelvic cysts are less common, with an incidence of approximately 1–3%4; however, they are more likely to be symptomatic5. Laparoscopic decortication of renal cysts is one of the most commonly used surgical methods. However, renal parapelvic cysts are usually located close to the collecting system, which makes them difficult to find and prone to injury during surgery. Therefore, some serious complications may occur after surgery, such as infection, long-term urinary leakage, and even nephrectomy. However, studies on how to identify the relationship between cysts and the collecting system during surgery in order to reduce the incidence of damage to the renal collecting system, are currently rare. In this study, we used methylene blue to aid in distinguishing the cysts from the renal collection system, in order to find and repair the damaged collection system quickly during surgery, to avoid postoperative urinary fistula or secondary surgery, and to achieve other results, as described below.
Methods
Study population
This study was approved by the Ethical Committee of the Third Central Hospital of Tianjin, and all methods were performed in accordance with the relevant guidelines and regulations. All patients provided written informed consent before participating in this study. Between May 2017 and December 2019, a total of 115 cases of renal cysts were treated, comprising 16 cases of renal parapelvic cysts (13.9%) that were included in this study. The inclusion criteria were: (1) symptoms, such as lumbago, hematuria, renal stones, and a history of repeated infection; and (2) renal cyst larger than 4 cm in diameter, or cysts that increases rapidly in volume over a short duration”. The exclusion criteria were: (1) Bosniak III–V complex renal cyst; (2) completely endogenous renal parapelvic cyst; and (3) patients with poor physical condition that were not fit for surgery. The basic information of the included cases are shown in Table 1. The patients included 9 males and 7 females; the mean age was 59.9 years (range, 41–74 years).The mean maximum diameter of the cysts was 6.6 cm (range, 4.8–10.5 cm). Eight patients presented with flank pain, and the other eight were asymptomatic patients that were incidentally identified on physical examination. One patient was diagnosed with an ipsilateral renal cell carcinoma, with no association between the renal cell carcinoma and the location of the cyst. One patient had ipsilateral kidney stones (0.6 cm), six patients had ipsilateral hydronephrosis, four patients also had ipsilateral simple renal cysts. All patients were diagnosed using color doppler abdominal ultrasonography, enhanced computed tomography urography and/or intravenous urography prior to surgery. Laparoscopic renal cyst decortication was performed with the assistance of continuous methylene blue ureteral infusion.
Laparoscopic renal cyst decortication using methylene blue
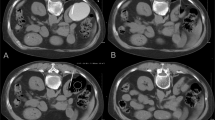
All of patients underwent general anesthesia with endotracheal intubation in a lithotomy position, and an F6 zebra ureteral catheter (Shangyi Kangge, Shanghai, China) was inserted retrogradely into the renal pelvis of the affected side. The indwelling catheter and the zebra ureteral catheter were fixed to prevent prolapse. The zebra ureteral catheter was then connected to a mixed solution of 0.2% methylene blue and saline (1000 ml saline plus 2 ml methylene blue) (Fig. 1A). The patient who had a coexisting renal cell carcinoma was then placed in a 45 degree healthy lateral recumbent position prior to undergoing renal parapelvic cyst decortication in addition to a partial nephrectomy through an abdominal approach. The other 15 patients were placed in a lateral position with the side to be operated upward. Retroperitoneal laparoscopic decortication of the renal parapelvic cyst was performed using the procedures of a conventional 3-hole method. The patients who had simple renal cysts received treatment for those cysts during the same surgery. The 0.2% methylene blue solution was infused continuously into the pelvis through the zebra ureteral catheter during the surgery in order to stain the collecting system (Fig. 1B,C). During the procedure, the patients were visually monitored for the presence of methylene blue liquid effluent, which would indicate that the renal collection system was injured.
The surgical procedure. (A) The ureteral catheter was connected to a mixed solution of 0.2% methylene blue saline (white arrow). (B) The cyst (white arrow) was positioned near the collecting system (black arrow). The perfused methylene blue stained the collection system, differentiating it from the cyst wall. (C) The renal parapelvic cyst was resected with no secondary damage. (D) The cyst was connected to the collection system and leakage of a blue liquid was seen from the cyst wall (white arrow).
Duration and outcome of follow-up
The patients were followed-up every 3 months. During each follow-up visit investigations, such as renal ultrasound scan or enhanced computer tomograph scans were performed. to evaluate mainly the size of residual lesions after surgery. The presence or absence of infection, urinary fistula, or hydronephrosis were also assessed. Those that had coexisting renal stones, were evaluated to ascertain whether the stones had resolves or had recurred.
Results
All 16 patients in this study successfully underwent laparoscopic surgery and there was no need to change to open surgery. The mean operation time was 40.8 min (range, 25–105 min) and the mean amount of blood loss was 8.3 ml (range, 3–40 ml). In one case, blue colored fluid leaked from the medial wall of the cyst after the lateral wall of the cyst was resected (Fig. 1D). It was determined that this cyst was connected to the collection system that was injured. A running suture using absorbable 4-0 monocryl was immediately used to repair the renal collection system near the wall of the parapelvic cyst until the leakage of blue colored liquid was no longer observed. The cavity of the cyst was then filled with fat from the pedicle of the kidney in order to prevent recurrence6. In this patient, the zebra ureteral catheter was removed after 2 weeks, while the other 15 patients had their catheters removed immediately after surgery. A retroperitoneal drainage tube that was inserted to drain any retroperitoneal fluid collection, was removed after confirming that there was no fluid drainage 1–3 days after surgery. The wounds healed very well, and the mean length of post-operative hospital stay was 2.6 days (range, 2–7 days). The wall of the cyst in all 16 cases were biopsied and pathological examination revealed that they were benign lesions. The pathological examination of the patient with a coexisting ipsilateral renal tumor revealed that it was a renal clear cell carcinoma.
All patients underwent following-up for 3–24 months. The cysts disappeared completely in 9 patients (Fig. 2). However, in the other 7 cases the size of the cysts decreased by more than 50%. Hydronephrosis was significantly alleviated in affected patients. The patient with a 0.6 cm kidney stone passed the stone into the ureter 20 days after surgery, probably because the obstruction was relieved, and the stone was discharged after extracorporeal shock wave lithotripsy. There were no complications related to the administration of methylene blue.
Discussion
Renal parapelvic cysts occur in the renal sinus and are histologically divided into urinary and non-urinary cysts7. It is difficult to distinguish renal parapelvic cysts from hydronephrosis using ultrasonography or ordinary computer tomography; therefore renal parapelvic cyst can be misdiagnosed. Correct diagnosis can be made with enhanced computed tomography. Renal parapelvic cysts are located close to the collecting system and this often causes discomforting features, such as flank pain, hematuria, infection, urinary obstruction, and renin-mediated hypertension8. Therefore, surgical intervention is performed more often for renal parapelvic cysts than for simple renal cysts. Secondary kidney stones also occur due to obstruction and infection9.
Nephrectomy was previously used as a treatment option for renal cysts10. Currently, the methods for the treatment of renal parapelvic cysts include open surgery, percutaneous renal cyst puncture, flexible ureteroscopy, and laparoscopic decortications11.
Open surgery is rarely used because it is quite invasive and is associated with more tissue trauma. Percutaneous renal cyst puncture produces less trauma but has a higher recurrence rate12. Injecting a sclerosant into the cyst can reduce the recurrence rate. The puncture procedure is difficult because renal parapelvic cyst are located close to the collecting system and the procedure may result in injury to the collecting system and renal blood vessels. Additionally, leakage of the sclerosant can cause severe perinephritis, ureteropelvic junction obstruction, abscess, fever, and other complications13.
With the continuous development and improvement of ureteroscopy, incision and drainage of renal cysts using flexible ureteroscopy and holmium laser is becoming increasingly popular. It is associated with minimal trauma and a short postoperative hospital stay14. Unfortunately, accurately locating of the cyst is sometimes difficult, especially in patients with thick-walled cysts. Zhixian Wang et al., reported that injecting methylene blue into the cyst during percutaneous renal puncture greatly improved the accuracy of finding cysts and shortened the operation time15. However, this type of surgery requires the use of an indwelling double J stent before and after surgery, which brings additional inconvenience to the patient and increases the risk of infection after surgery16. Furthermore, this procedure cannot be used in patients with a ureteral stricture and cannot be combined with the simultaneous treatment of simple renal cysts or other kidney lesions.
Laparoscopic renal cyst decortication is safe and effective, especially for large simple renal cysts, and is the gold standard for the treatment of renal cysts16. Laparoscopic decortication can also be used in the treatment of renal parapelvic cysts17,18, but it requires specialized surgical skills19. Renal parapelvic cysts are usually located close to the renal collecting system and the renal blood vessels; therefore, the separation process is associated with the risk of secondary damage, including the probability of vascular injury (1.7%), of visceral injury (0.25%), and renal pelvic injury (0.12%)20. It can be difficult to determine if the collecting system is injured during surgery; however, damage to the collecting system can lead to persistent urinary fistula after surgery. According to our results, we achieved good outcomes with this method, some advantages of out method are: (1) After injecting methylene blue through the ureteral catheter, the collection system will stain blue which improves the visibility of the collecting system relative to the cyst wall, and allows for complete resection of the cyst wall. The ureteral catheter plays a guiding and a protective role in the ureter; therefore, we can greatly avoid secondary ureteral damage during surgery. (2) If the renal cyst is connected to the collecting system, identifying the renal cyst during traditional laparoscopic renal cyst decortication surgery can be difficult. If continuous exudation of urine is seen in the drainage tube after surgery, additional surgery will be required to repair the collecting system. This would cause the patient more pain. However, if this situation is encountered while using our methodology, leakage of a blue colored liquid from the wall of the cyst can be seen during surgery, and we can simultaneously repair the injured wall at the same time. The zebra ureteral catheter inserted during the operation can remain in situ for 2 weeks and acts as an internal drain. The ureteral catheter can be removed directly without the aid of a cystoscope. (3) If other lesions are present, they can be treated along with this procedure during the surgery. In this study, one patient with renal cell carcinoma and four patients with simple renal cysts also underwent relevant treatment for their respective conditions during the same surgery. (4) Compared with flexible ureteroscopy, there is no need to use a double J stent before and after surgery, and this reduces the cost of treatment21. Patient with ureteral stricture can also undergo this surgical approach. Francesco et al., reported that the infection rate following flexible ureteroscopy was about 7.7%22, but our surgical procedure had a lower infection rate, as no patient in this study had infections after surgery. (5) Methylene blue is a tricyclic phenothiazine that inhibits guanylate cyclase. It has been used in several fields of medicine. The most common side effects of methylene blue administration are self-limiting blue-green cutaneous discoloration and urine discoloration23. In our study, methylene blue entered the renal pelvis or calyces and flowed out through the ureter, without entering the general circulation. Even if a small amount had entered the body, methylene blue is a mature drug that can be excreted in the urine with little metabolism or side effects24, and no special treatment would be required. Compared with enhanced computer tomography, methylene blue is not radioactive and can be used continuously during surgery.
Conclusions
Renal parapelvic cysts are often encountered by urologists and they are difficult to manage. Laparoscopic renal cyst decortication is still the preferred treatment; however, it is associated with the risk of secondary injury to nearby structures20. In this study, the combination of methylene blue and laparoscopy achieved good results and was found to be a safe, effective, and practical method for the treatment of renal parapelvic cysts. However, further studies with longer follow-up periods are required to verify the effectiveness of this method.
Data availability
The datasets used and/or analyzed in this study are available from the corresponding author upon reasonable request.
References
Sigmon, D. F., Shikhman, R. & Nielson, J. I. Renal cyst. StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; (2020).
Bas, O. et al. Management ofrenalcysts. JSLS 19, e2014.00097 (2015).
Agarwal, M. M. & Hemal, A. K. Surgical management of renal cystic disease. Curr. Urol. Rep. 12, 3–10 (2011).
Yu, W. et al. Flexible ureteroscopic management of symptomatic renal cystic diseases. J. Surg. Res. 196, 118–123 (2015).
Zhao, Q. et al. Treatment of parapelvic cyst by internal drainage technology using ureteroscope and holmium laser. West Indian Med. J. 64, 230–235 (2015).
Esposito, C. et al. Laparoscopic or robotic deroofing guided by indocyanine green fluorescence and perirenal fat tissue wadding technique of pediatric simple renal cysts. J. Laparoendosc. Adv. Surg. Tech. A 30(4), 471 (2020).
Na, Y.Q. et al., Chinese Association of Urology Guidelines. Beijing, People's Health Publishing House, 366–67(2014).
Shah, J. B., Whitman, C., Lee, M. & Gupta, M. Water under the bridge: 5-year outcomes after percutaneous ablation of obstructing parapelvic renal cysts. J. Endourol. 21, 1167–1170 (2007).
Kang, N., Guan, X., Song, L., Zhang, X. & Zhang, J. Simultaneous treatment of parapelvic renal cysts and stones by flexible ureterorenoscopy with a novel four-step cyst localization strategy. Int. Braz. J. Urol. 44, 958–964 (2018).
Kropp, K. A., Grayhack, J. T., Wendel, R. M. & Dahl, D. S. Morbidity and mortality of renal exploration for cyst. Surg. Gynecol. Obstet. 125, 803–806 (1967).
Yang, D. et al. A modified laparoendoscopic single-site renal cyst decortication: single-channel retroperitoneal laparoscopic deco-rtication of simple renal cyst. J. Laparoendosc. Adv. Surg. Tech. A 23, 506–510 (2013).
Rossi, S. H., Koo, B., Riddick, A., Shah, N. & Stewart, G. D. Different successful management strategies for obstructing renal parapelvic cysts. Urol. Int. 101, 366–368 (2018).
Skolarikos, A., Laguna, M. P. & De la Rosette, J. J. Conservative and radiological management of simple renal cysts: a comprehensive review. BJU Int. 110, 170–178 (2012).
Mao, X., Xu, G., Wu, H. & Xiao, J. Ureteroscopic management of asymptomatic and symptomatic simple parapelvic renal cysts. BMC Urol. 15, 48 (2015).
Wang, Z. et al. Methylene blue injection via percutaneous renal cyst puncture used in flexible ureteroscope for treatment of parapelvic cysts: a modified method for easily locating cystic wall. Urology 125, 243–247 (2019).
Eissa, A. et al. Non-conservative management of simple renal cysts in adults: a comprehensive review of literature. Minerva Urol. Nefrol. 70, 179–192 (2018).
Yoder, B. M. & Wolf, J. S. Jr. Long-term outcome of laparoscopic decortication of peripheral and peripelvic renal and adrenal cysts. J. Urol. 171, 583–587 (2014).
Shiraishi, K., Eguchi, S., Mohri, J. & Kamiryo, Y. Laparoscopic decortication of symptomatic simple renal cysts: 10-year experience from one institution. BJU Int. 98, 405–408 (2006).
Porpiglia, F. et al. Retroperitoneal decortication of simple renal cysts vs decortication with wadding using perirenal fat tissue: results of a prospective randomized trial. BJU Int. 103, 1532–1536 (2009).
Rabii, R. et al. Retroperitoneal laparoscopic treatment of parapelvic renal cysts: report of 5 cases. Prog. Urol. 15, 1070–1073 (2005).
Li, E. C. et al. Pure natural orifice translumenal endoscopic surgery management of simple renal cysts: 2-year follow-up results. J. Endourol. 25, 75–80 (2011).
Francesco, B. et al. Infective complications after retrograde intrarenal surgery: a new standardized classification system. Int. Urol. Nephrol. 48, 1757–1762 (2016).
Booth, A. T., Melmer, P. D., Tribble, B., Mehaffey, J. H. & Tribble, C. Methylene blue for vasoplegic syndrome. Heart Surg. Forum 20, E234–E238 (2017).
Tucker, D., Lu, Y. & Zhang, Q. From mitochondrial function to neuroprotection-an emerging role for methylene blue. Mol. Neurobiol. 55, 5137–5153 (2018).
Acknowledgements
We would like to thank Editage (www.editage.cn) for English language editing. This study was supported by a project of Tianjin Medical Talent Plan (2018-19) from Tianjin Municipal Government.
Author information
Authors and Affiliations
Contributions
Z. M: Project development, Data collection, Data analysis, Manuscript writing. S. L: Project development, Data collection, Data analysis. F.M.C: Project development, Data analysis, Manuscript editing, Surgical operator. D.H.Y, X.G.Z, and K.L: Project development, and Manuscript editing. M.H.Z, S.T, and Q.W: Project development, data collection, and data analysis.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ma, Z., Li, S., Chen, FM. et al. The preliminary experience of methylene blue assisted laparoscopy in the treatment of renal parapelvic cysts. Sci Rep 10, 18757 (2020). https://doi.org/10.1038/s41598-020-76006-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-76006-4
This article is cited by
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.