Abstract
Visceral fat is associated with cardiovascular and kidney disease. However, the relationship between body composition and anthropometric measures in type 1 diabetes is unknown. Using z-statistics, we ranked the ability of body mass index (BMI), waist circumference (WC), waist-hip ratio (WHR), waist-height ratio (WHtR) and a body shape index (ABSI) to capture measures of body composition from 603 Dual-energy-X-Ray-Absorptiometry scans of adults with type 1 diabetes. Albuminuria was defined as urinary albumin excretion rate of at least 30 mg/24 h. Women with albuminuria had higher visceral fat mass % (VFM%) (0.9 vs. 0.5%, p = 0.0017) and lower appendicular lean mass % (AppLM%) (25.4 vs 26.4%, p = 0.03) than those without. Men with albuminuria had higher VFM% (1.5 vs. 1.0%, p = 0.0013) and lower AppLM% (30.0 vs 32.3, p < 0.0001) than those without. In men, WHtR estimated VFM% best (z-statistics = 21.1), followed by WC (z = 19.6), BMI (z = 15.1), WHR (z = 14.6) and ABSI (z = 10.1). In women, the ranking was WC (z = 28.9), WHtR (z = 27.3), BMI (z = 20.5), WHR (z = 12.7) and ABSI (z = 10.5). Overall, the ranking was independent of albuminuria. Adults with type 1 diabetes and albuminuria have greater VFM% and lower AppLM% than those without. WHtR and WC best estimate the VFM% in this population, independently of albuminuria and sex.
Similar content being viewed by others
Introduction
The obesity epidemic is spreading worldwide. Along with this global trend, also people with type 1 diabetes have exhibited weight gain over the last years1. Such an increase in body weight will most likely have a harmful impact on the cardiovascular mortality rate of this population2,3. Previous research from our group showed that the mortality rate of individuals with type 1 diabetes increases starting from a body mass index (BMI) of 24.8 kg/m2, which is still within the normal range1. Therefore, it brings up the question of whether the BMI cut-off to define central obesity and cardiovascular risk in individuals with type 1 diabetes should be lower than the traditionally used 30 kg/m2.
BMI is the most commonly used tool to classify obesity, although it is an inadequate biomarker of abdominal obesity4. It does not differentiate muscle from fat nor give the precise information regarding the amount of body fat mass, which better defines obesity5 and which is positively associated with cardiovascular disease (CVD)6,7. Furthermore, BMI neither distinguishes women from men concerning their body fat nor provides any information about the fat distribution, which is relevant for the risk of CVD8. Given that obesity is causally related to diabetic nephropathy (DN) in individuals with type 1 diabetes9, it would be of utmost importance to understand how the anthropometric measures are related to their body composition and especially visceral fat, which has been associated with dyslipidemia, insulin resistance, CVD8,10, and chronic kidney disease11,12 in the general population.
The Dual-energy X-ray Absorptiometry (DXA) is a well-recognized method to study fat distribution and body composition5. Unfortunately, the high cost hinders its use in routine clinical practice. On the other side, anthropometric measures such as waist circumference (WC) and waist-hip ratio (WHR) are accessible and of low cost, although they have certain limitations13. Another practical anthropometric measure is the waist-height ratio (WHtR) that has been associated with CVD in the general population and has the advantage to have a unisex cut-off value of 0.513,14,15,16, moreover, a meta-analysis has shown that WHtR is a better screening tool than WC and BMI for adult cardiometabolic risk factors16. A body shape index (ABSI) is another formula in which WC is adjusted for weight and height and has been a predictor of mortality, independently of BMI, in an American population from the National Health and Nutrition Examination Survey (NHANES)17.
Thus far, the relationship between these anthropometric measures and the body composition of adults with type 1 diabetes at different stages of DN, expressed as the presence or absence of albuminuria, has not previously been investigated. Therefore, this study aimed to explore these relationships and seek to identify the anthropometric measure to best estimate the visceral fat in this population with high cardiovascular risk.
Results
Data were available from a total of 246 men (30.5% with albuminuria) and 357 women (20.4% with albuminuria) (Table 1). In both men and women, individuals with albuminuria were older, had longer diabetes duration, higher systolic blood pressure and worse glycaemic control (Table 1).
Body composition according to the albuminuric stage
In men, BMI was no different between individuals with or without albuminuria (25.5 kg/m2 vs. 26.5 kg/m2, p = 0.08), albeit the two groups presented a different body composition. Men with albuminuria had greater BFM% (29.1% vs. 27.0%, p = 0.03), greater AFM% (3.0% vs. 2.4%, p = 0.02), and greater VFM% (1.5% vs. 1.0%, p = 0.001) compared with those without albuminuria (Table 1). On the other hand, men with albuminuria had lower BLM% (67.3% vs. 69.2%, p < 0.04) and lower AppLM% (30.0% vs. 32.3%, p < 0.0001) than the normoalbuminuric men (Table 1).
In women, BMI was greater in the albuminuric group (27.2 kg/m2 vs. 25.4 kg/m2, p = 0.04) than in the normoalbuminuric group. The BFM% (36.9% vs. 35.6%, p = 0.39) and the AFM% (3.0% vs. 2.7%, p = 0.16) were no different between women with or without albuminuria. However, we observed greater VFM% (0.9% vs. 0.5%, p = 0.001) in women with albuminuria (Table 1). Regarding the muscle mass, women with albuminuria had lower AppLM% (25.4% vs. 26.4%, p = 0.02) despite no difference in the BLM% (59.6% vs. 61.0%, p = 0.29) compared to the normoalbuminuric women (Table 1).
Body composition according to sex
In the whole cohort (independently of the presence or absence of albuminuria), men and women had comparable BMI (25.9 kg/m2 vs. 25.9 kg/m2, respectively, p = 0.87), despite different body composition (Table 2). Men had lower BFM% (27.91% vs. 35.98%, p < 0.0001), greater BLM% (68.41% vs. 60.73%, p < 0.0001), and greater AppLM% (31.49% vs. 26.27%, p < 0.001) than women (Table 2). Although the AFM% was comparable between men and women (2.63% vs. 2.71%, p = 0.54), the VFM% was greater in men (1.20% vs. 0.58%, p < 0.0001).
Associations between body composition and anthropometric measures
Measures of BFM%
WHtR, followed by the WC, was the anthropometric measure to best estimate the BFM% in men, independently of albuminuria (Table 3). In women, BMI followed by WC was the measure to best estimate the BFM%, also independently of albuminuria (Table 3). WHtR explained 60% of the BFM% variation in all men and 63% of the BFM% variation in all women. The BMI explained 47% of the BFM% variation in all men and 70% of the BFM% variation in all women (Table 3). In our linear model, the WHtR cut-off of 0.5 corresponded to a BFM% of 25.0 in all men and a BFM% of 34.6 in all women (Table 4).
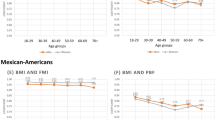
Measures of VFM%
WHtR, followed by the WC, was the anthropometric measure to best estimate the VFM% in men, while WC followed by WHtR was the best in women, independently of albuminuria (Fig. 1 and Table 3). The WHtR explained 68% of the VFM% variation in all men and 69% of the VFM% variation in all women (Table 3). WC explained 65% of the VFM% variation in all men and 71% of the VFM% variation in all women (Table 3). In our linear model, the WHtR cut-off of 0.5 corresponded to a VFM% of 1.1 in all men and a VFM% of 0.7 in all women (Table 4).
Measures of BLM%
WHtR, followed by WC, was the anthropometric measure to best estimate BLM% in all men, while BMI followed by WC was the best measure in women, independently of albuminuria (Table 3). The WHtR explained 59% of the BLM% variation in all men and 62% of the BLM% variation in all women (Table 3). BMI explained only 46% of the BLM% variation in all men but 69% of the BLM% variation in all women (Table 3).
The BLM% was negatively associated with the VFM% in all men (beta − 5.58 [− 6.17, − 4.98], r2 = 0.59, p = 7.09 × 10–48) and in all women (beta − 7.88 [− 8.65, − 7.11], r2 = 0.53, p = 1.23 × 10–60). The same association pattern was seen for both the normoalbuminuric and the albuminuric stage.
The BFM%, VFM% and BLM% associations with anthropometric measures according to the albuminuric stages are shown in Table 3.
WHR and ABSI showed a low association with the BFM%, VFM% and BLM%, independently of the albuminuric stage and sex (Table 3).
Misclassification of body fat
Considering the normal threshold of BFM% below 25 for men and below 30 for women, the BMI misclassified 26.4% of the total cases (Table 5) by underestimating the body fat percentage in 20.6% of the cases and overestimating it in 5.8% (Table 5). The misclassification of BFM% by WC, WHR and WHtR were 22.6% (Table S1), 37.1% (Table S2) and 26.6% (Table S3), respectively.
Discussion
In this study, we investigated for the first time the body composition of individuals with type 1 diabetes with and without albuminuria. We showed that individuals with albuminuria, regardless of sex, had greater visceral fat percentage and lower appendicular lean mass percentage, which is a dangerous combination regarding the risk of CVD8,18,19. This finding is even more relevant if we consider that this population already has a high cardiovascular risk because of diabetes and DN1,3,20.
We showed that individuals with similar BMI have very different body composition, especially concerning the percentage of visceral fat and lean mass. This result emphasizes the importance of knowing the body composition instead of only BMI in a high cardiovascular risk population. The increase in body weight with a central distribution favours the accumulation of visceral fat that leads to an inflammatory state and insulin resistance10, which has been associated with kidney disease11,12,21. To make the situation worse, low lean mass22 and kidney disease23 are also associated with muscle insulin resistance. Considering that this is a cross-sectional study, it is not possible to say if the visceral fat, which is linked to chronic inflammation and insulin resistance, is contributing to the development of albuminuria or the albuminuric stage is worsening the visceral fat and insulin resistance due to physical inactivity, inflammation, changes in the microbiome or other factors21.
Most importantly, in this study, we found a strong association between VFM% and simple measures such as WHtR and WC, independently of the albuminuric stage and sex. We are not aware of any other study in individuals with type 1 diabetes that have previously assessed such relationships, especially looking at different stages of albuminuria. WHtR has been associated with central obesity and cardiovascular risk in the general population and in people with type 2 diabetes13,14,15. Furthermore, in a large prospective study including 109,536 postmenopausal women, it has been linked to cardiovascular events24. However, the relationship between WHtR and VFM% has never been described in individuals with type 1 diabetes with and without albuminuria. Given that DN increases cardiovascular mortality several-fold20,25 and that visceral fat is closely associated with CVD8, 18, our results regarding the association between WHtR and visceral fat are consistent with the literature which has shown the WHtR is a better screening tool than BMI for cardiometabolic risk factors16. Therefore, this study brings up new important information regarding central obesity in individuals with type 1 diabetes, a subject that most of the time has been related to type 2 diabetes. In this respect, it is important to acknowledge that obesity is increasing among individuals with type 1 diabetes and at the same time, there has been an increase in the mortality rate starting from a normal range of BMI1.
Another novel finding of this study was the negative association between BLM% and WHtR and WC, independently of the albuminuric stage. Although BLM% was best estimated by WHtR in men and by BMI in women, the simple measurement of WC was the second-best for the estimation of BLM% in both sexes. A plausible explanation for why WC and WHtR can estimate the percentage of body lean mass is the negative association between BLM% and VFM%. Although a recent publication showed that the fat-free mass was not associated with CVD7, it does not exclude the relevance of our findings, since one has to take into consideration that the fat-free mass measured by bioimpedance includes not only the muscle mass and, in our study, we measured the body lean mass by DXA, which has better accuracy than the bioimpedance5. From a clinical perspective, we found a simple and accessible tool to estimate the body lean mass in individuals with type 1 diabetes, independently of albuminuria.
Since low skeletal muscle mass is linked to CVD19 and muscle wasting has been associated with premature death in individuals with end-stage renal disease26 another important clinical finding was that, independently of sex, individuals with albuminuria have lower AppLM% compared to those without albuminuria, which might contribute to the increase in the cardiovascular risk of this high-risk population. Muscle wasting is not rare in individuals with end-stage renal disease26,27 and although we did not include such individuals in our analyses, we showed that individuals with type 1 diabetes at the earlier stages of DN (micro and macroalbuminuria) already show a decrease in their BLM% compared to those with normoalbuminuria.
According to previous publications including individuals with obesity and/or type 2 diabetes, in the current study, the ABSI was positively associated with central obesity and negatively associated with body lean mass28,29. However, it was inferior to the other anthropometric measures for the estimation of BFM%, VFM% and BLM% in our sample composed by Caucasian-Finnish individuals with type 1 diabetes. Since ABSI is a formula composed by WC adjusted for weight and height, the association between ABSI and body composition may vary depending on the characteristics of the studied population and on ethnicity.
In our study, BMI was not the anthropometric measure to best estimate VFM% in both sexes, and this inability of BMI to reflect the abdominal fat has been discussed erlier4. It was not useful to estimate BFM% and BLM% in men either, although it was in women. The relationship between BMI and BFM% was studied previously in the general population30 and the percentage of body fat mass related to the BMI was similar to our study. However, the American study30 did not investigate the associations between VFM%, BLM% with BMI, not either with WHtR and WC such as our study.
Furthermore, BMI misclassified BFM% in 26% of the total cases and underestimated it in 21% of them. Although the level of misclassification by BMI in our study is lower than in a previous study31, it might be explained by the different methods used to assess the body composition. In the previous study, they used bioimpedance while we used DXA, which provides better accuracy5. However, such as misclassification is clinically relevant, since individuals considered to have normal body weight by BMI might, in fact, have an excess of body fat and visceral fat, which are both closely associated with cardiovascular mortality8,13,32,33. The misclassification by BMI is another possible explanation of why the mortality rate in individuals with type 1 diabetes starts to increase already from the normal range of BMI1 Interestingly, the WC and WHtR misclassify the BFM% at least similarly to BMI, although they are in fact measures to estimate the central fat and not the total body fat. This finding is clinically important since a simple measure of WHtR or WC could not only better estimate visceral fat than BMI, but was able to classify obesity (BFM%) as well as BMI.
Another novelty of this study is to show, by our linear models, how much of the body fat mass and visceral fat mass percentages are related to the cut-offs of BMI, WC and WHtR. Interestingly, the BFM% and VFM% related to the BMI of 25 kg/m2 are similar to BFM% and VFM% related to the WHtR of 0.5. Therefore, our finding may provide a clue, why there is an increase in the mortality rate of this population starting from a BMI of 24.8 kg/m2 1. These results may question whether the BMI of 25 kg/m2 is the best cut-off to define central obesity and cardiovascular risk in individuals with type 1 diabetes.
A limitation of this study is that we can not exclude confounding factors such as lifestyle and ethnicity. Since we studied a homogenous all-Caucasian Finnish population with type 1 diabetes and there are different thresholds for waist circumference and BMI for different ethnicities4,34, our results may not be applicable for all ethnicities. Another limitation is its cross-sectional design; therefore, it is not possible to conclude any causality between the associations we found nor any prediction of CVD risk. However, these results motivate further prospective studies to investigate the impact of body composition on chronic diabetes complications in individuals with type 1 diabetes. Another strength is its wide applicability to clinical practice since we here provide easily applicable tools to estimate the percentage of visceral fat and lean mass in a population with a high cardiovascular risk.
In conclusion, this study shows that simple measures such as WHtR and WC can estimate the VFM% in adults with type 1 diabetes independently of albuminuric stage and sex. Furthermore, it showed that individuals with type 1 diabetes and albuminuria, a population of high CVD risk, have greater VFM% and lower AppLM% compared to those with normoalbuminuria. From the clinical perspective, this study supports the routine monitoring of WHtR in adults with type 1 diabetes.
Methods
Study design and population
In this cross-sectional study, we explored the body composition and its relationship with anthropometric measures in individuals with type 1 diabetes with and without albuminuria. Adults with type 1 diabetes (n = 579) from the Finnish Diabetic Nephropathy (FinnDiane) Study cohort that had a DXA scan (n = 603) between August 2011 and June 2019 were included in this analysis. For 24 individuals, two scans were performed 5.3 ± 1.4 years apart as part of a regular follow-up visit. Sensitivity analysis including only the first scan (n = 579) for each individual led to the same conclusions (data not shown). Since 1997 the FinnDiane Study is recruiting and thoroughly characterizing individuals with type 1 diabetes 18 years or older at 93 centers across Finland. Type 1 diabetes is defined as age at onset of diabetes under 40 years and permanent insulin treatment initiated within a year from the diabetes diagnosis. The study protocol is designed according to the principles of the Declaration of Helsinki as revised in 2000 and was approved by the Ethics Committee of Helsinki and Uusimaa Hospital District. Written informed consents are obtained from each FinnDiane Study participant.
Diabetic nephropathy (DN) stage
Normoalbuminuria was defined as an urinary albumin excretion rate (UAER) < 20 µg/min or < 30 mg/24 h in at least two out of three urine samples. Microalbuminuria was defined as a UAER ≥ 20 and < 200 µg/min or ≥ 30 and < 300 mg/24 h and macroalbuminuria as a UAER ≥ 200 µg/min or ≥ 300 mg/24 h. Individuals with micro- or macroalbuminuria were pooled together for analyses and will be referred throughout the paper as the albuminuric group. Individuals with end-stage renal disease (either on dialysis or have received a kidney transplant) were not included in this study.
Body composition and anthropometric measurements
Body composition was evaluated by DXA (GE Healthcare Lunar version 16, Wisconsin, USA) according to the manufacturer’s instructions and visceral fat was measured by CoreScan35. A total body fat percentage below 25 was considered normal for men and below 30 for women30,31. The body fat mass percentage (BFM%), android fat mass percentage (AFM%), visceral fat mass percentage (VFM%), body lean mass percentage (BLM%), and appendicular lean mass percentage (AppLM%) were calculated by dividing the variable (grams) by total body weight (grams). Appendicular lean mass refers to the lean mass of both legs and arms.
BMI was calculated as total body weight (kilograms) divided by the square of the height (meters)36 and individuals were stratified by their BMI as normal weight (19–24.9 kg/m2), overweight (25–29.9 kg/m2) and obese (≥ 30 kg/m2)36. WC was measured in centimeters by a stretch‐resistant tape at the horizontal plane midway in the distance of superior iliac crest and the lower margin of the last rib34. The WC was considered normal if it was below 94 cm for men and below 80 cm for women37. The hip circumference was measured with the same tape around the widest part over the great trochanters and WHR was calculated by dividing the WC by the hip circumference34. A WHR below 0.9 for men and below 0.85 for women were considered normal34. The WHtR was calculated by dividing the WC by the height and values below 0.5 were considered normal for both men and women13. ABSI was calculated by the formula WC/(BMI2/3height½)17.
Statistical analyses
For the analyses, we split the cohort into men and women and further distinguished between individuals with and without albuminuria.
Data on categorical variables are presented as frequencies, while continuous variables as medians (interquartile ranges, IQR). Between-group comparisons were conducted via permutation tests with 10,000 permutations. To compare the anthropometric measures for their capacity to estimate body composition, we performed linear regression analyses adjusted for age with the measurements of body composition as the dependent variables and anthropometric measures as the independent variables. The regressions’ R2 values were used to describe the proportion of the variance of a body composition measure that is explained by an anthropometric measure. The relevance ranking of each variable was based on the z statistics allowing comparisons across risk factors independently of their measurement units38. WHR and WHtR were scaled by a factor of 10. All analyses were performed in R39.
Abbreviations
- AFM:
-
Android fat mass
- AFM%:
-
AFM/total body weight × 100
- AppLM:
-
Appendicular-lean-mass (both legs and arms lean mass)
- AppLM%:
-
AppLM/total body-weight × 100
- BFM:
-
Body fat mass
- BFM%:
-
BFM/total body weight × 100
- BLM:
-
Body lean mass
- BLM%:
-
BLM/total body weight × 100
- BMI:
-
Body mass index
- DN:
-
Diabetic nephropathy
- DXA:
-
Dual-energy X-ray Absorptiometry
- HDL:
-
High-density lipoprotein cholesterol
- VFM:
-
Visceral fat mass
- VFM%:
-
VFM/total body weight × 100
- WC:
-
Waist circumference
- WHR:
-
Waist-hip-ratio
- WHtR:
-
Waist-height ratio
References
Dahlström, E. H. et al. Body mass index and mortality in individuals with type 1 diabetes. J. Clin. Endocrinol. Metab. 104, 5195–5204 (2019).
Conway, B. et al. Adiposity and mortality in type 1 diabetes. Int. J. Obes. 33, 796–805 (2009).
Edqvist, J. et al. BMI, mortality, and cardiovascular outcomes in type 1 diabetes: findings against an obesity paradox. Diabetes Care 42, 1297–1304 (2019).
Ross, R. et al. Waist circumference as a vital sign in clinical practice: a Consensus Statement from the IAS and ICCR Working Group on Visceral Obesity. Nat. Rev. Endocrinol. 16, 177–189 (2020).
Parente, E. B. Is body mass index still a good tool for obesity evaluation?. Arch. Endocrinol. Metab. 60, 507–509 (2016).
Larsson, S. C., Bäck, M., Rees, J. M. B., Mason, A. M. & Burgess, S. Body mass index and body composition in relation to 14 cardiovascular conditions in UK Biobank: a Mendelian randomization study. Eur. Heart J. 41, 221–226 (2020).
Larsson, S. C. & Burgess, S. Fat mass and fat-free mass in relation to cardiometabolic diseases: a two-sample Mendelian randomization study. J. Intern. Med. 288, 260–262 (2020).
Després, J.-P. Body fat distribution and risk of cardiovascular disease. Circulation 126, 1301–1313 (2012).
Todd, J. N. et al. Genetic evidence for a causal role of obesity in diabetic kidney disease. Diabetes 64, 4238–4246 (2015).
Després, J.-P. Health consequences of visceral obesity. Ann. Med. 33, 534–541 (2001).
Kang, S. H., Cho, K. H., Park, J. W., Yoon, K. W. & Do, J. Y. Association of visceral fat area with chronic kidney disease and metabolic syndrome risk in the general population: analysis using multi-frequency bioimpedance. Kidney Blood Press. Res. 40, 223–230 (2015).
Sarathy, H. et al. Abdominal obesity, race and chronic kidney disease in young adults: results from NHANES 1999–2010. PLoS ONE 11, e0153588 (2016).
Browning, L. M., Hsieh, S. D. & Ashwell, M. A systematic review of waist-to-height ratio as a screening tool for the prediction of cardiovascular disease and diabetes: 0·5 could be a suitable global boundary value. Nutr. Res. Rev. 23, 247–269 (2010).
Ashwell, M. & Hsieh, S. D. Six reasons why the waist-to-height ratio is a rapid and effective global indicator for health risks of obesity and how its use could simplify the international public health message on obesity. Int. J. Food Sci. Nutr. 56, 303–307 (2005).
Ashwell, M. & Lejeune, S. Ratio of waist circumference to height may be better indicator of need for weight management. BMJ 312, 377 (1996).
Ashwell, M., Gunn, P. & Gibson, S. Waist-to-height ratio is a better screening tool than waist circumference and BMI for adult cardiometabolic risk factors: systematic review and meta-analysis. Obes. Rev. J. 13, 275–286 (2012).
Krakauer, N. Y. & Krakauer, J. C. A new body shape index predicts mortality hazard independently of body mass index. PLoS ONE 7, e39504 (2012).
Hsieh, S. D. & Yoshinaga, H. Abdominal fat distribution and coronary heart disease risk factors in men-waist/height ratio as a simple and useful predictor. Int. J. Obes. Relat. Metab. Disord. J. 19, 585–589 (1995).
Kang, D. O. et al. prognostic impact of low skeletal muscle mass on major adverse cardiovascular events in coronary artery disease: a propensity score-matched analysis of a single center all-comer cohort. J. Clin. Med. 8, 712 (2019).
Groop, P. H. et al. Excess mortality in patients with type 1 diabetes without albuminuria-separating the contribution of early and late risks. Diabetes Care 41, 748–754 (2018).
Spoto, B., Pisano, A. & Zoccali, C. Insulin resistance in chronic kidney disease: a systematic review. Am. J. Physiol. Ren. Physiol. 311, F1087–F1108 (2016).
Cleasby, M. E., Jamieson, P. M. & Atherton, P. J. Insulin resistance and sarcopenia: mechanistic links between common co-morbidities. J. Endocrinol. 229, R67–R81 (2016).
DeFronzo, R. A. et al. Insulin resistance in uremia. J. Clin. Invest. 67, 563–568 (1981).
Lo, K. et al. Prospective associations of waist-to-height ratio with cardiovascular events in postmenopausal women: results from the women’s health initiative. Diabetes Care 42, e148–e149 (2019).
Groop, P.-H. et al. The presence and severity of chronic kidney disease predicts all-cause mortality in type 1 diabetes. Diabetes 58, 1651–1658 (2009).
Stenvinkel, P., Carrero, J. J., von Walden, F., Ikizler, T. A. & Nader, G. A. Muscle wasting in end-stage renal disease promulgates premature death: established, emerging and potential novel treatment strategies. Nephrol. Dial. Transplant. 31, 1070–1077 (2016).
Robinson, K. A., Baker, L. A., Graham-Brown, M. P. M. & Watson, E. L. Skeletal muscle wasting in chronic kidney disease: the emerging role of microRNAs. Nephrol. Dial. Transplant. 35, 1469–1478 (2020).
Biolo, G. et al. Inverse relationship between ‘a body shape index’ (ABSI) and fat-free mass in women and men: Insights into mechanisms of sarcopenic obesity. Clin. Nutr. Edinb. Scotl. 34, 323–327 (2015).
Gomez-Peralta, F. et al. Relationship between ‘a body shape index (ABSI)’ and body composition in obese patients with type 2 diabetes. Diabetol. Metab. Syndr. 10, 21 (2018).
Heo, M., Faith, M. S., Pietrobelli, A. & Heymsfield, S. B. Percentage of body fat cutoffs by sex, age, and race-ethnicity in the US adult population from NHANES 1999–2004. Am. J. Clin. Nutr. 95, 594–602 (2012).
Frankenfield, D. C., Rowe, W. A., Cooney, R. N., Smith, J. S. & Becker, D. Limits of body mass index to detect obesity and predict body composition. Nutr. Burbank Los Angel. Cty. Calif 17, 26–30 (2001).
Lee, C. M. Y., Huxley, R. R., Wildman, R. P. & Woodward, M. Indices of abdominal obesity are better discriminators of cardiovascular risk factors than BMI: a meta-analysis. J. Clin. Epidemiol. 61, 646–653 (2008).
Dobbelsteyn, C. J., Joffres, M. R., MacLean, D. R. & Flowerdew, G. A comparative evaluation of waist circumference, waist-to-hip ratio and body mass index as indicators of cardiovascular risk factors. The Canadian Heart Health Surveys. Int. J. Obes. Relat. Metab. Disord. 25, 652–661 (2001).
World Health Organization. Waist circumference and waist-hip ratio: report of a WHO expert consultation, Geneva, 8–11 December 2008. (World Health Organization, Geneva, 2011).
Meredith-Jones, K., Haszard, J., Stanger, N. & Taylor, R. Precision of DXA-derived visceral fat measurements in a large sample of adults of varying body size. Obes. Silver Spring Md. 26, 505–512 (2018).
WHO Consultation on Obesity (1999: Geneva) & World Health Organization. Obesity : preventing and managing the global epidemic : report of a WHO consultation. Obésité Prév. Prise En Charge Épidémie Mond. Rapp. Une Consult. OMS (2000).
Alberti, K. G. M. M., Zimmet, P. & Shaw, J. Metabolic syndrome: a new world-wide definition. A Consensus Statement from the International Diabetes Federation. Diabet. Med. 23, 469–480 (2006).
Hainsworth, D. P. et al. risk factors for retinopathy in type 1 diabetes: the DCCT/EDIC study. Diabetes Care 42, 875–882 (2019).
R Core Team. R: A Language and Environment for Statistical Computing. (R Foundation for Statistical Computing, Vienna, 2018).
Acknowledgements
The authors would like to acknowledge all physicians and nurses at each FinnDiane center participating in patient recruitment and characterization.
Funding
This research was funded by grants from the Folkhälsan Research Foundation, Academy of Finland (316664 and 275614), Wilhelm and Else Stockmann Foundation, Liv och Hälsa Society, Novo Nordisk Foundation (NNF OC0013659) and The Diabetes Research Foundation.
Author information
Authors and Affiliations
Contributions
E.B.P. was responsible for the study design. E.B.P. and S.M. contributed equally to the manuscript preparation (shared first authors). S.M. and V.H. were responsible for the statistical analysis. P.H.G., E.B.P., S.M., V.H. interpreted the results and contributed to the critical revision of the manuscript. C.F. and A.J.A. contributed to acquisition of the data and critical revision of the manuscript. P.H.G. is the guarantor of this work and takes full responsibility for the integrity of the data and the accuracy of the data analysis. All authors reviewed the manuscript and approved the final version.
Corresponding author
Ethics declarations
Competing interests
EBP reports receiving lecture honorariums from Eli Lilly, Abbott, Astra Zeneca, Sanofi, Boehringer Ingelheim and is an advisory board member of Sanofi. P-.H.G. reports receiving lecture honorariums from Astellas, Astra Zeneca, Boehringer Ingelheim, Eli Lilly, Medscape, MSD, Mundipharma, Novo Nordisk, PeerVoice, Sanofi, SCIARC and being an advisory board member of Astellas, Astra Zeneca, Boehringer Ingelheim, Eli Lilly, Medscape, MSD, Mundipharma, Novo Nordisk, and Sanofi. SM, VH, AJA and CF report no conflict of interest.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Parente, E.B., Mutter, S., Harjutsalo, V. et al. Waist-height ratio and waist are the best estimators of visceral fat in type 1 diabetes. Sci Rep 10, 18575 (2020). https://doi.org/10.1038/s41598-020-75667-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-75667-5
This article is cited by
-
Double diabetes—when type 1 diabetes meets type 2 diabetes: definition, pathogenesis and recognition
Cardiovascular Diabetology (2024)
-
The new visceral adiposity index outperforms traditional obesity indices as a predictor of subclinical renal damage in Chinese individuals: a cross-sectional study
BMC Endocrine Disorders (2023)
-
Waist to height ratio as a simple tool for predicting mortality: a systematic review and meta-analysis
International Journal of Obesity (2023)
-
The impact of central obesity on the risk of hospitalization or death due to heart failure in type 1 diabetes: a 16-year cohort study
Cardiovascular Diabetology (2021)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.