Abstract
Low serum ferritin is diagnostic of iron deficiency, yet its published lower cut-off values are highly variable, particularly for pediatric populations. Lower cut-off values are commonly reported as 2.5th percentiles, and is based on the variation of ferritin values in the population. Our objective was to determine whether a functional approach based on iron deficient erythropoiesis could provide a better alternative. Utilizing 64,443 ferritin test results from pediatric electronic health records, we conducted various statistical techniques to derive 2.5th percentiles, and also derived functional reference limits through the association between ferritin and erythrocyte parameters: hemoglobin, mean corpuscular volume, mean cell hemoglobin concentration, and red cell distribution width. We find that lower limits of reference intervals derived as centiles are too low for clinical interpretation. Functional limits indicate iron deficiency anemia starts to occur when ferritin levels reach 10 µg/L, and are largely similar between genders and age groups. In comparison, centiles (2.5%) presented with lower limits overall, with varying levels depending on age and gender. Functionally-derived limits better reflects the underlying physiology of a patient, and may provide a basis for deriving a threshold related to treatment of iron deficiency and any other biomarker with functional outcomes.
Similar content being viewed by others
Introduction
Iron deficiency is the major cause of anemia that affects up to 32.9% of the global population, with the highest burden seen in young children1. Iron requirements are increased during rapid growth of early childhood, and during adolescence for females, making these population groups particularly vulnerable2. Untreated iron deficient erythropoiesis can lead to anaemia3, which is associated with reduced cognitive development among children4.
Although a variety of laboratory assessments for iron status is available, serum ferritin provides the highest diagnostic accuracy in relation to the gold standard, bone marrow aspirate5. Low serum ferritin is pathognomonic of uncomplicated iron deficiency6. Serum ferritin tests are commonly accompanied by erythrocyte parameters: hemoglobin, mean corpuscular volume (MCV), mean corpuscular hemoglobin (MCH), mean cell hemoglobin concentration (MCHC), and red cell distribution width (RDW), when investigating iron deficiency anemia. Iron deficiency anemia is characterized with a reduction in all erythrocyte parameters except RDW6.
Thresholds for defining iron deficiency based on serum ferritin are highly variable, particularly for children7,8,9. Ideally, reference intervals are determined from healthy populations and stratified according to age, gender, and other physiological states when they show distinct subpopulation distributions10. Establishing reference intervals for children is a difficult task, with significant logistic and resource challenges in collecting samples from a large population of healthy children. Nevertheless, a number of international initiatives have established robust and nationally harmonized reference intervals; a prominent example being the Canadian laboratory initiative on pediatric reference intervals (CALIPER) study11. Most reference interval harmonization initiatives follow the direct approach recommended by Clinical and Laboratory Standards Institute (CLSI), with 2.5th and 97.5th percentiles calculated as reference intervals from a ‘healthy’ population12,13.
In recent years the indirect approach of deriving reference intervals has gained interest, where secondary data sources such as hospital pathology records14 and pathology laboratory databases15 are explored as alternative populations13. Through use of stringent inclusion criteria to derive a ‘healthy’ population16 and/or through novel statistical methods17, secondary data sources are proving to be a viable option.
Regardless of the approach, reference intervals dependent on measured values within the population selected. If iron deficiency is highly prevalent, which may be asymptomatic, then both direct and indirect approaches will under-estimate the lower limit of “normal”.
Through a novel approach based on the functional association between serum ferritin and erythrocyte parameters, studies have identified serum ferritin thresholds with clinical relevance to iron deficiency anaemia18,19. Our objective was to determine whether a functional approach based on clinically relevant iron deficient erythropoiesis could provide a more clinically useful alternative to direct and indirect approaches.
Methods
Data source
In this study, we used de-identified pathology data from 211 general practices collected from the Population Level Analysis and Reporting (POLAR) data space, provided by the data custodians, Outcome Health20. Outcome Health collects data on behalf of primary health networks (PHNs), which are geographically localized health districts aiming to improve provision of healthcare services. In this study, data from three PHNs from Victoria, Australia: South-Eastern Melbourne, Eastern Melbourne, and Gippsland were used.
Our analyses included all laboratory results of ferritin (µg/L and ng/mL, standardized to µg/L), hemoglobin (g/L), MCV (fL), MCHC (g/L), MCH (pg), and RDW (%) measured between 2008 and 2018 for those aged 2 to 18 years, as identified by test names and Logical Observation Identifiers Names and Codes (LOINC)21. Biomarkers were assessed for differences in measurement years by investigating variation in medians and inter-quartile ranges. No significant variations were observed.
Exclusion/inclusion criteria
Ferritin is a positive acute phase reactant, and can increase during acute infection/inflammation, even in iron deficiency. C-reactive protein (CRP), an inflammation marker, is helpful in interpreting ferritin results in such cases, although the criteria used to define iron deficiency during infection/inflammation not well established22. Therefore, results associated with increased CRP results above reported reference intervals (as ≥ 10 mg/L23,24), were excluded. Furthermore, participants who had a diagnostic record for thalassemia, and participants on iron supplement medication within the last year of the test were excluded. If several tests were recorded for a participant, only the earliest record was included.
Statistical analyses
Various approaches were used to determine lower reference limit for ferritin.
Clinical and Laboratory Standards Institute (CLSI) parametric approach
In this analysis, the lower reference limit was derived according to principles outlined in CLSI guidelines, as reported by Solberg25. The dataset was stratified by gender, as recorded in patients’ electronic health records, and the lower reference limit was determined for each age between 2 to 18 years (calculated as: year at time of laboratory test – year of birth).
Initially, distribution of ferritin values were plotted as a scatterplot by gender and age. The data was transformed to a Gaussian distribution through Box–Cox26 transformation at each age value. A presentation of the overall distribution of serum ferritin values, and an overall Box–Cox transformation reducing the skew of the distribution can be found in supplementary figure S1. Ferritin results ≥ 1000 µg/L were excluded from further analysis. Remaining data were subjected to outlier detection according to Tukey’s method27, where values lying outside of ‘outer fences’ were excluded:
or
Tukey’s outlier removal was performed in two replicates for each age and gender category. Distribution of remaining data was evaluated by Q–Q (quantile–quantile) plots. Lastly, parametric fractiles at each year of age by gender, and their respective 90% confidence intervals were estimated using the following formulas25, respectively:
Final values were converted back into their original forms by reversing Box–Cox transformations.
Clinical and Laboratory Standards Institute (CLSI) non-parametric (rank method) approach
This analysis follows the rank-based procedure outlined by Solberg25. We determined rank-based fractiles for the lower-level of the reference interval for ferritin, stratified by gender for ages between 2 and 18 years. Initially, results values were sorted from lowest to highest. The position of the lower fractile in the rank was determined using the following formula:
Results obtained from this formula determined the position where the lower reference lies in the sorted list of ferritin test results.
Multivariate fractional polynomial
In this analysis, a non-parametric approach to derive the 2.5th percentile for ferritin was used. For each gender category, bivariate fractional polynomial models based on median for the association between ferritin test results and age were formed, with quantile regression at the 2.5th percentile calculated. Based on these models, the 2.5th percentiles for each year of age between 2 and 18 were estimated using post-estimation calculations, including their respective 95% confidence intervals.
Correlation between serum ferritin and erythrocyte parameters
By using a similar approach in the study performed by Markus et al.18, we modelled the correlation between ferritin and erythrocyte parameters: hemoglobin, MCV, MCHC, MCH and RDW. The rationale in this approach is that reduced iron stores, as reflected by serum ferritin concentrations are followed by a reduction in hemoglobin, MCV, MCHC and MCH, and an increase in RDW as it progresses towards anaemia6.
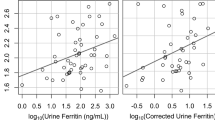
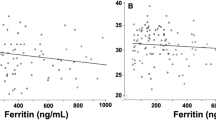
The best model to describe the association between ferritin and erythrocyte parameters were explored through scatterplots and median-spline plots. We determined that 2-degree fractional polynomial models would best describe the correlations, and multivariate fractional polynomials were plotted, modelling quantile regression at medians (Figs. 2, 3, 4, 5, 6).
Our models were stratified by age groups and gender. Ages were categorized into three groups: ages 2–4, 5–12, and 13–8 years, similar to those described by Markus el al.18. We then estimated the erythrocyte value at each ferritin concentration from 1 to 60 µg/L, including their respective 95% confidence intervals, and plotted values for each age and gender group.
We determined the point where iron deficiency starts to progress to anemia based on the correlation between ferritin and erythrocyte parameters beginning to asymptote. Asymptote occurred when erythrocyte value differences between subsequent correlated ferritin values became less than 1 (to one decimal place). All statistical analyses were conducted using Stata/MP 16.0 (StataCorp., TX, USA).
Ethics
Ethics to extract and analyze de-identified general practice data for research was obtained by data custodians of the POLAR data space from RACGP National Research and Evaluation Ethics Committee (NREEC 17–008). Our research team obtained ethics to conduct research on these data from Macquarie University Human Research Ethics Committee (5201700872). Informed consent from patients was not required, as approved by both RACGP National Research and Evaluation Ethics Committee and Macquarie University Human Research Ethics Committee.
Our study was conducted and reported according to the Reporting of Studies Conducted Using Observational Routinely Collected Health Data Statement for Pharmacoepidemiology (RECORD-PE) guideline28.
Results
Number of test results included in each analysis is summarized in Table 1. A total of 39,910 ferritin tests were ordered for females, and 24,533 for males. Figure 1 shows the different distributions of serum ferritin test results between females and males for serum ferritin results < 60 µg/L. Parametric and rank-based CLSI results presented similar distributions for both genders until age of 10, after which females had markedly lower values compared to males (Tables 2, 3). Similar results were observed for our fractional polynomial model, with females having lower values beginning at age 7 compared to males. Overall, males had a relatively linear increase in ferritin values with age, whereas for females, an increase was observed until near adolescence, after which a decrease occurred.
Median spline, scatterplot, and smoothed quantile regression based on 2-degree fractional polynomial models of the correlation between ferritin result values and hemoglobin (Hb) values. Results for females plotted on top, and results for males plotted on bottom for the three age groups, 2–4, 5–12, and 13–18 years.
Median spline, scatterplot, and smoothed quantile regression based on 2-degree fractional polynomial models of the correlation between ferritin result values and mean corpuscular volume (MCV) values. Results for females plotted on top, and results for males plotted on bottom for the three age groups, 2–4, 5–12, and 13–18 years.
Median spline, scatterplot, and smoothed quantile regression based on 2-degree fractional polynomial models of the correlation between ferritin result values and mean corpuscular hemoglobin concentration (MCHC) values. Results for females plotted on top, and results for males plotted on bottom for the three age groups, 2–4, 5–12, and 13–18 years.
Median spline, scatterplot, and smoothed quantile regression based on 2-degree fractional polynomial models of the correlation between ferritin result values and mean corpuscular hemoglobin (MCH) values. Results for females plotted on top, and results for males plotted on bottom for the three age groups, 2–4, 5–12, and 13–18 years.
Median spline, scatterplot, and smoothed quantile regression based on 2-degree fractional polynomial models of the correlation between ferritin result values and red cell distribution width (RDW) values. Results for females plotted on top, and results for males plotted on bottom for the three age groups, 2–4, 5–12, and 13–18 years.
In our analysis of the correlation between ferritin and erythrocyte parameters, decrease in hemoglobin and MCHC levels occurred first, followed by MCV levels, and lastly, MCH and RDW levels. For hemoglobin, females presented with decreasing hemoglobin levels at 10 µg/L among younger children, and at 11 µg/L among adolescents (Table 2). For males, the level was slightly higher (12 µg/L) for adolescents, and slightly lower (9 µg/L) for young children (Table 3). MCHC levels started decreasing at a similar level to hemoglobin, near 10–11 µg/L for both genders. MCV levels started deteriorating at a lower corresponding value for ferritin, between 6 and 8 µg/L for both genders. Levels were lower for MCH and RDW: between 4 to 5 µg/L for females and 5–6 µg/L for males MCH, and 3–5 µg/L for females and 5–6 µg/L for males RDW. These results are graphically represented in Figs. 2, 3, 4, 5 and 6.
Discussion
Generating pediatric reference intervals is a resource-intensive task. Laboratories frequently resort to using guideline-based diagnostic cut-offs or published reference intervals29,30. In our study, we used various approaches to derive a lower reference limit for ferritin from a large clinical laboratory dataset. Our results suggest that ‘functional’ reference limits based on disease progression (i.e. iron deficient erythropoiesis leading to anemia) may be more meaningful than commonly reported population distribution-based reference limits for nutritional biomarkers, such as ferritin.
In our analyses based on the conventional method of reporting population distribution based reference limits, we observed a decrease in the lower ferritin reference limit beginning with adolescence for females; which was also reported by Katayev et al.31 in their study using routinely collected data from laboratories, in the CALIPER study of healthy children11, and also in Australian studies by Southcott et al.32 and Hoq et al.33 on a healthy children (Table 2). In comparison, males had increasing lower ferritin reference limits by age (Table 3).
Females have a high prevalence of subclinical iron deficiency34, which could possibly be reflected into reference limits of these studies and ours. Southcott et al.32 compared their results to the CALIPER study, and suggested that a number of subjects in the CALIPER study could have had subclinical iron deficiency32. Although our study population was not representative of healthy children, our results were comparable to these studies. Therefore, the presence of subclinical iron deficiency could be affecting the reference intervals derived from conventional population distribution-based methods.
Our analysis on the correlation between ferritin and erythrocyte parameters, which was initially described by Markus et al.18, presents a functional lower reference limit that is associated with progression towards anemia. An advantage of this approach is that the reference limit is less influenced by potential subclinical iron deficiencies in the population. We observed a deterioration in hemoglobin concentration beginning near 10 µg/L ferritin, while MCV concentrations begin to decline at a lower ferritin level, of 7–8 µg/L. This is in line with the known progression of iron deficiency anemia: as iron deficiency remains, depleted iron stores results in a physiological response whereby a reduction of hemoglobin production occurs (i.e. lower hemoglobin MCH, and MCHC levels), which eventually leads to smaller erythrocytes (reduced MCV levels) and variable red cells widths (high RDW levels). Our results provide levels of serum ferritin correlating with this progression35,36.
Our results suggest that overall, a value of around 10 µg/L ferritin is the point at which iron deficiency anemia begins to occur. Anemia manifests late in clinical progression of iron deficiency erythropoiesis6. Therefore, the point of inflection for ferritin just prior to overt iron deficiency is expected to be higher than 10 µg/L37. Our results based on CLSI and fractional polynomial analyses, as well as other studies based on healthy children, suggested a reference limit lower than 10 µg/L. The definition and selection of healthy population in relation to iron metabolism is challenged by general lack of symptoms until the condition is relatively severe. This raises the question of whether the reference limit of nutritional markers should be based on functional limits or a fixed percentile of a reference (‘healthy’) population. Differences in results from functional correlation analysis of ferritin and hematological parameters, and population averaged analyses (i.e. CLSI and polynomial models), suggest the need for more nuanced consideration when deciding which methods are best suited to its clinical utility.
Using routinely collected data has limitations that should be considered. One limitation is the likely presence of unwell children, which has implications for population distribution based functional limits. We are unable to exclude unwell children with no record of their illness, or, in the case of inflammation, those without a CRP test. Previous studies have reported differences in reference values related to variation in laboratory methods11,38, and studies presenting indirect reference intervals are recommended to describe pre-analytical and analytical processes13. As our results are from general practices across a large region, the results would have been derived from a number of laboratories, possibly with different methods and analyzers. Determining and describing these procedures in our study is not possible as this information is not available. Nonetheless, our assessment of variation indicated that the results are stable across the study period, and does not present with significant variations. Although our results are similar to studies from other regions, it should be noted that our data comes from one state in Australia, and may not necessarily be representative of the general population. Larger studies in Australia, and replication of our methodology elsewhere would provide a greater understanding of ferritin levels in various regions. Our study has strengths, including the good overview from potentially healthy and ill patients, which is necessary for the correlation model described by Markus et al.18 to be fitted, and the large sample size from routinely collected data.
Conclusion
Information-rich, routinely collected data sources provide an opportunity to correlate test results with patient outcomes and may be utilized in deriving or assessing clinical representativeness of reference intervals. Functionally derived reference limits with clinical utility provide a more meaningful reference limit for ferritin in diagnosing iron deficiency compared to commonly used population centiles. Ferritin concentration of 10 µg/L correspond to erythrocyte levels indicative of iron deficiency anemia. Therefore, the lower reference limit for ferritin should ideally be at a level above 10 µg/L, prior to progression to anemia.
Data availability
De-identified individual participant data can be made available by the data custodians to researchers who provide a methodologically sound proposal for use in achieving the goals of their approved proposal, on condition of approval of the primary health networks on whose behalf the data is being collected for. Proposals can be submitted to Outcome Health at admin@outcomehealth.org.au.
References
Kassebaum, N. J. et al. A systematic analysis of global anemia burden from 1990 to 2010. Blood 123, 615–624 (2014).
Beard, J. L. Why iron deficiency is important in infant development. J. Nutr. 138, 2534–2536 (2008).
German, C. E. The treatment of iron deficiency without anaemia (in otherwise healthy persons). Swiss Med. Wkly. 147, 14434 (2017).
Pasricha, S.-R. Should we screen for iron deficiency anaemia? A review of the evidence and recent recommendations. Pathology (Phila.) 44, 139–147 (2012).
Parkin, P. C. & Borkhoff, C. M. Practical tips for paediatricians: assessment and management of young children with iron deficiency. Paediatr. Child Health 23, 433–434 (2018).
Soppi, E. T. Iron deficiency without anemia - a clinical challenge. Clin. Case Rep. 6, 1082–1086 (2018).
Domellöf, M., Dewey, K. G., Lönnerdal, B., Cohen, R. J. & Hernell, O. The diagnostic criteria for iron deficiency in infants should be reevaluated. J. Nutr. 132, 3680–3686 (2002).
Kelishadi, R. et al. Pediatric-specific reference intervals in a nationally representative sample of Iranian children and adolescents: the CASPIAN-III study. World J. Pediatr. 12, 335–342 (2016).
Tahmasebi, H. et al. Pediatric reference intervals for biochemical markers: gaps and challenges, recent national initiatives and future perspectives. EJIFCC 28, 43–63 (2017).
Ozarda, Y. Reference intervals: current status, recent developments and future considerations. Biochem. Medica 26, 5–11 (2016).
Adeli, K., Higgins, V., Trajcevski, K. & Habeeb, N.W.-A. The Canadian laboratory initiative on pediatric reference intervals: a CALIPER white paper. Crit. Rev. Clin. Lab. Sci. 54, 358–413 (2017).
Horowitz, G. L. CLSI C28–A3: Defining, Establishing, and Verifying Reference Intervals in the Clinical Laboratory; Approved Guideline, Third Edition, C28A3E (Clinical and Laboratory Standards Institute, Wayne, 2008).
Jones, G. R. D. et al. Indirect methods for reference interval determination—review and recommendations. Clin. Chem. Lab. Med. 57, 20–29 (2018).
Shaw, J. L. V. et al. Validity of establishing pediatric reference intervals based on hospital patient data: A comparison of the modified Hoffmann approach to CALIPER reference intervals obtained in healthy children. Clin. Biochem. 47, 166–172 (2014).
Tate, J. R. et al. Harmonising adult and paediatric reference intervals in Australia and New Zealand: an evidence-based approach for establishing a first panel of chemistry analytes. Clin. Biochem. Rev. 35, 213–235 (2014).
Drees, J. C., Huang, K., Petrie, M. S., Lorey, T. S. & Dlott, R. S. Reference intervals generated by electronic medical record data mining with clinical exclusions: age-specific intervals for thyroid-stimulating hormone from 33038 euthyroid patients. J. Appl. Lab. Med. 3, 231–239 (2018).
Katayev, A., Fleming, J. K., Luo, D., Fisher, A. H. & Sharp, T. M. Reference intervals data mining no longer a probability paper method. Am. J. Clin. Pathol. 143, 134–142 (2015).
Markus, C., Saxon, B. & Metz, M. Ferritin as a functional biomarker of iron status in children and young adults. Br. J. Haematol. 184, 640–642 (2019).
Foy, B. H., Li, A., McClung, J. P., Ranganath, R. & Higgins, J. M. Data-driven physiologic thresholds for iron deficiency associated with hematologic decline. Am. J. Hematol. 95, 302–309 (2020).
Pearce, C., McLeod, A., Rinehart, N., Ferrigi, J. & Shearer, M. What a comprehensive, integrated data strategy looks like: the population level analysis and reporting (POLAR) program. Stud. Health Technol. Inform. 264, 303–307 (2019).
Stram, M. et al. Logical observation identifiers names and codes for laboratorians: potential solutions and challenges for interoperability. Arch. Pathol. Lab. Med. 144, 229–239 (2020).
Cook, J. D. Diagnosis and management of iron-deficiency anaemia. Best Pract. Res. Clin. Haematol. 18, 319–332 (2005).
Schlenz, H. et al. C-reactive protein reference percentiles among pre-adolescent children in Europe based on the IDEFICS study population. Int. J. Obes. 38, S26–S31 (2014).
Gabay, C. & Kushner, I. Acute-phase proteins and other systemic responses to inflammation. N. Engl. J. Med. 340, 448–454 (1999).
Solberg, H. E. The theory of reference values. Part 5. Statistical treatment of collected reference values. Determination of reference limits. Clin. Chim. Acta 137, 95–114 (1984).
Box, G. E. P. & Cox, D. R. An Analysis of Transformations. J. R. Stat. Soc. Ser. B Methodol. 26, 211–243 (1964).
Tukey, J. W. Exploratory Data Analysis (Pearson, London, 1977).
Langan, S. M. et al. The reporting of studies conducted using observational routinely collected health data statement for pharmacoepidemiology (RECORD-PE). BMJ 363, (2018).
Poole, S., Schroeder, L. F. & Shah, N. An unsupervised learning method to identify reference intervals from a clinical database. J. Biomed. Inform. 59, 276–284 (2016).
Schnabl, K., Chan, M. K., Gong, Y. & Adeli, K. Closing the gaps in paediatric reference intervals: the CALIPER initiative. Clin. Biochem. Rev. 29, 89–96 (2008).
Katayev, A., Balciza, C. & Seccombe, D. W. Establishing reference intervals for clinical laboratory test results: is there a better way?. Am. J. Clin. Pathol. 133, 180–186 (2010).
Southcott, E. K. et al. Establishment of pediatric reference intervals on a large cohort of healthy children. Clin. Chim. Acta 411, 1421–1427 (2010).
Hoq, M. et al. Reference values for 30 common biochemistry analytes across 5 different analyzers in neonates and children 30 days to 18 years of age. Clin. Chem. 65, 1317–1326 (2019).
Rushton, D. H. & Barth, J. H. What is the evidence for gender differences in ferritin and haemoglobin?. Crit. Rev. Oncol. Hematol. 73, 1–9 (2010).
Braunstein, E. Iron deficiency anemia—hematology and oncology. Merck Manuals Professional Edition https://www.merckmanuals.com/professional/hematology-and-oncology/anemias-caused-by-deficient-erythropoiesis/iron-deficiency-anemia (2020).
Pasricha, S.-R.S. et al. Diagnosis and management of iron deficiency anaemia: a clinical update. Med. J. Aust. 193, 525–532 (2010).
Barragán-Ibañez, G., Santoyo-Sánchez, A. & Ramos-Peñafiel, C. O. Iron deficiency anaemia. Rev. Médica Hosp. Gen. México 79, 88–97 (2016).
Hoq, M. et al. A prospective, cross-sectional study to establish age-specific reference intervals for neonates and children in the setting of clinical biochemistry, immunology and haematology: the HAPPI Kids study protocol. BMJ Open 9, e025897 (2019).
Funding
This study was supported by funding from the Quality Use of Pathology Program, Department of Health, Government of Australia (4-2QFVW4M). The funder played no role in the design, conduct, or reporting of this study.
Author information
Authors and Affiliations
Contributions
G.S. conceptualized the study, carried out the statistical analysis, drafted the initial manuscript, and reviewed and revised the manuscript. P.M. and V.I. conceptualized the study, contributed to the drafting of the initial manuscript, provided expertise, and critically reviewed the manuscript for important intellectual content. M.H. contributed to the drafting of the initial manuscript, provided expertise, and critically reviewed the manuscript for important intellectual content. T.P.L. conceptualized the study, and critically reviewed the manuscript for important intellectual content. L.L. provided expertise on the statistical analysis, contributed to the design of the study, and reviewed and revised the manuscript for important intellectual content. A.M. and C.P. developed the data collection instruments, collected data, contributed to the interpretation of the data, and reviewed and revised the manuscript. J.W. and A.G. contributed to the design of the study, critically reviewed the manuscript for important intellectual content, and revised the manuscript. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sezgin, G., Monagle, P., Loh, T.P. et al. Clinical thresholds for diagnosing iron deficiency: comparison of functional assessment of serum ferritin to population based centiles. Sci Rep 10, 18233 (2020). https://doi.org/10.1038/s41598-020-75435-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-75435-5
This article is cited by
-
Association of single nucleotide polymorphism at BMP2 gene with iron deficiency status among anaemic patients in Hospital Universiti Sains Malaysia
Egyptian Journal of Medical Human Genetics (2024)
-
Opioid prescribing among aged care residents during the first year of the COVID-19 pandemic: an analysis using general practice health records in Australia
BMC Geriatrics (2023)
-
Haemoglobin diagnostic cut-offs for anaemia in Indian women of reproductive age
European Journal of Clinical Nutrition (2023)
-
Detection of factors affecting kidney function using machine learning methods
Scientific Reports (2022)
-
COVID-19: protocol for observational studies utilizing near real-time electronic Australian general practice data to promote effective care and best-practice policy—a design thinking approach
Health Research Policy and Systems (2021)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.