Abstract
Coronavirus disease 2019 (COVID-19) is an important and urgent threat to global health. Inflammation factors are important for COVID-19 mortality, and we aim to explore whether the baseline levels of procalcitonin (PCT), C-reaction protein (CRP) and neutrophil-to-lymphocyte ratio (NLR) are associated with an increased risk of mortality in patients with COVID-19. A retrospective study was conducted and a total of 76 patients with confirmed COVID-19 were included between January 17, 2020 to March 2, 2020, of these cases, 17 patients were dead. After adjusting covariates, PCT (≥ 0.10 ng/mL) and CRP (≥ 52.14 mg/L) exhibited independent increasing risks of mortality were used hazard ratio (HR) of 52.68 (95% confidence interval [CI]: 1.77–1571.66) and 5.47 (95% CI: 1.04–28.72), respectively. However, NRL (≥ 3.59) was not found to be an independent risk factor for death in our study. Furthermore, the elevated PCT levels were still associated with increasing risk of mortality in the old age group (age ≥ 60 y), and in the critically severe and severe patients after adjustment for complications. Thu Baseline levels of PCT and CRP have been addressed as independent predictors of mortality in patients with COVID-19.
Similar content being viewed by others
Introduction
The mysterious outbreak of atypical pneumonia was reported in late December, 2019, in Wuhan, China, and the pathogen and its genomic characterization was quickly identified1,2,3. The highly infectious severe acute espiratorysyndromecoronavirus2 (SARS-CoV-2) began to spread to other countries around the world, which presented an important and urgent threat to global health. Then World Health Organization (WHO) named the disease as “Coronavirus disease 2019” (COVID-19) and declared it as a public health emergency of international concern on January 30, 2020. Globally, almost 2.5 million cases of COVID-19 and more than 160,000 deaths have been reported4, and a total of 82,798 confirmed cases with 4,632 deaths were reported in China up to April 22, 20205.
Currently, no specific medicine has been developed against for this highly infectious disease. Although most patients have mild symptoms and good prognosis, patients with critically severe disease are at high risk of mortality. Therefore, it is urgent to find appropriate indicators to discriminate the severity and improve the progress to reduce the mortality rate of patients with COVID-19.
At present, several clinical features to estimate the risk of patients being experiencing a poor outcome from the infection could assist medical staff in triaging patients when allocating limited healthcare resources. A series of inflammation factors have been recognized as an enabling characteristic for COVID-19 severity and mortality6,7,8. As markers of systemic inflammation, procalcitonin (PCT), C-reaction protein (CRP) and neutrophil-to-lymphocyte ratio (NLR) are objective and easy to implement, and usually taken to measure patient’s susceptibility to mortality.
Li had found elevated serum CRP levels in the severe COVID-19 patients compared with the moderate patients8, however, from a cohort of 17 patients with COVID-19, Zhou did not found this situation in the aggravation group9. A retrospective study observed higher serum PCT and CRP levels in critical cardiovascular disease patients with COVID-19 than in the general patients10. A meta-analysis had shown that the NLR levels in severe patients with COVID-19 were increased compared with patients without severe disease11. Meanwhile, according to a retrospective study in early patients in Wuhan, Liu indicated NLR as an independent risk factor for mortality in hospitalized patients with COVID-1912.
Many studies were focused on the epidemic center of Wuhan, and the clinical characteristics and outcomes in other areas of Hubei province were not systematically reported. Xiaogan city is adjacent to the Wuhan, only 50 miles away, and the reported patients with COVID-19 was 3,518 up to April 24, 2020, ranked second in the Hubei province13. Hanchuan, one of seven county cities of Xiaogan, has a total area of 1658.56 km2 with the population of 1.08 million at the end of 201814, and 763 cases with 29 cases dead were reported up to April 24, 202015.
Due to controversial results and small sample size, there is still scarce and limited information regarding the inflammation factors associated with mortality in patients with COVID-19, especially for PCT, CRP and NLR. The relationship between these three factors and their independent associations with survival are not well studied. In this study, we aim to explore whether the baseline inflammation factors of PCT, CRP and NLR are associated with an increased risk of death in patients with COVID-19.
Materials and methods
Study design
This was a two-center, retrospective study in patients hospitalized to designated Hanchuan People’s Hospital and the First Hospital of Suihua. Suihua is small city located in the northeast of China, with a total of 47 confirmed cases up to April 24, 202016. Because of small sample size, the critically severe patients from the First Hospital of Suihua were analyzed together. The informed consent were obtained from the patiens hospitalized to the above hospitals or theie relatives. This study was approved by the Institutional Ethics Board of Heilongjiang Provincial Hospital, and is in full compliance with the Helsinki Declaration.
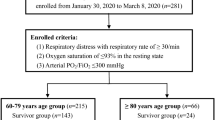
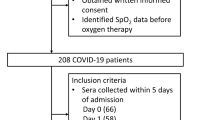
Study population
Patients with confirmed COVID-19 from January 17, 2020 to March 2, 2020 were enrolled in this study. All cases before hospitalization were laboratory-confirmed by human infection SARS-CoV-2 from throat swab samples17,18, following the recommendation by the National Institute for Viral Disease Control and Prevention of China19. According to the guidelines for diagnosis and management of COVID-19 (7th edition, in Chinese) issued by the National Health Commission of China, clinical conditions are classified into four types: mild, moderate, severe, and critically severe20. Because of patients with clinical mild type were in the mobile cabin hospitals, thus, in this research, we only enrolled patients of COVID-19 with moderate, severe and critically severe patients.
Markers of inflammation
Laboratory measurements were conducted at hospitalization as close to initiation of antibiotics and antivirus as possible and received lab test when changing in health condition. Our primary measures of inflammation were PCT, CRP and NLR, because not all the patients were measured regularly, thus, we only included baseline levels of PCT, CRP and NRL during the treatment periods. The serum concentrations of PCT were determined using Maglumi 2000 Plus automated platform (Snibe, Shenzen, China) and CRP were measured by a specific protein immune analyzer using CRP-M100 instrument (Mindray, Shenzen, China). NLR was calculated for each case by dividing the reported total absolute neutrophil counts by the total absolute lymphocyte counts, which were detected by BC-6900 (Mindray, Shenzen, China) automatic blood cell analyzer.
Other covariates
We reviewed the electronic medical records of patients with standardized data collection form to extract other covariates, including demographic (age, sex, time from illness onset to first hospital admission, chronic heart disease, chronic lung disease, chronic kidney disease, diabetes and hypertension), clinical symptoms (fever, cough, headache, myodynia, chills, nausea and vomiting, chest distress or shortness of breath), complications (acute respiratory distress syndrome [ARDS], hypohepatia, renal insufficiency, heart failure and shock) and therapeutic strategies including use of glucocorticoid, mechanical ventilation and immune globulin.
Definition of clinical outcomes
The clinical outcomes, including discharge and death were monitored up to February 15, 2020 and March 19, 2020 in the First Hospital of Suihua and Hanchuan People’s Hospital, respectively. If the patient’s condition improved significantly and would be discharged when there were no respiratory symptoms, normal temperature for more than 3 days, and pulmonary imaging showed significant improvement in acute exudative lesions and most important thing was patients must pass 2 consecutive nucleic acid tests20.
Statistics
Continuous variables were expressed as mean (standard deviation, SD) when values were normally distributed, otherwise, the results were presented in terms of median (interquartile range, IQR). The significant differences between the groups for continuous variables were compared using one-way analysis of variance when the data were normally distributed, otherwise, the Kruskal–Wallis H-test was used. Categorical variables were described as frequency and percentages, and proportions for categorical variables were compared using the independent sample chi-square test. The Logistic regression was used to prediction the combined effect.
To detect if PCT, CPR, NLR and their combined effect are more sensitive in predicting for mortality, the area under the curve (AUC) and the 95% CI of the receiver operator characteristic (ROC) curve was computed regarding discharge as negative whereas mortality as positive. The optimal cut‐off values for PCT, CPR, NLR and their combined effect to predict the mortality of patients with COVID‐19 were determined by Youden's index which could be utilized as the reference for clinical classification.
Survival curves of PCT, CPR, NLR and their combined effect were plotted using the Kaplan–Meier method and log-rank tests were used to compared difference. Cox proportional hazard ratio (HR) models were used to determine HRs and 95% CIs for each covariate to determine the risk factors for death during hospitalization in patients with COVID-19. Next, we examined PCT, CRP and NLR as independent predictors of survival in multivariable-adjusted Cox HR models, which were adjusted for age, sex, cancer, ARDS, hypohepatia, renal insufficiency, heart failure and shock. Furthermore, we also explored different effects stratified by age and sex, as well as clinical types. Because no death was in the moderate group, we only analyzed the risks of PCT, CPR and NLR in combined critically severe and severe groups. Time to death was defined as the time from hospital admission to mortality, and individuals alive were censored at the time of discharged.
Two-tailed P value less than 0.05 was considered statistically significant. All analyses were performed with R software, version 3.5.1.
Results
Characteristics among three groups
From January 29, 2020 to March 2, 2020, a total of 68 patients with COVID-19 from Hanchuan City people’s hospital and 8 cases from Suihua first hospital were included in this research, of these cases, 32 patients were in the critically severe group, 18 patients in the severe group, and the remaining 26 patients in the moderate group. The frequent clinical symptoms for patients with COVID-19 were fever (84.21%), cough (64.47%) and chest distress or shortness of breath (44.74%) on admission. Compared with moderate group, hypertension and chest distress or shortness of breath tended to be more common in the critically severe and severe groups (P < 0.05).
The patients with critical clinical type had higher rates of ARDS, renal insufficiency, heart failure ad shock compared with the other two groups, and renal insufficiency, heart failure and shock were only developed in critically severe group. More frequent treatments of glucocorticoid and mechanical ventilation were used in patients with critical severe and severe types than those with moderate clinical type.
22.37% (17/76) patients with COVID-19 were dead during the treatment, and those only developed in the critically severe group. Patients with moderate clinical type had longer days of stay in hospital (median 28 days) than in the critically severe (17 days) and severe groups (16.5 days), shown in Table 1.
Relationships between PCT, CRP, NLR and clinical types
The PCT, CRP and NLR displayed statistically significant among three groups, and patients with critical and severe clinical types had elevated levels of PCT and NLR compared with moderate group (P < 0.05). Meanwhile, there was a statistical increased trend of CRP among the three groups, with the lowest in the moderate group (median 10 mg/L), then in the severe group (median 26.86 mg/L), and the highest in the critically severe group (median 92.2 mg/L) (P < 0.05), shown in Fig. 1.
Diagnostic value of PCT, CRP and NLR for COVID-19 mortality
From the Fig. 2 and Table 2, the PCT, CRP, NLR and their combined effect had diagnostic values for COVID-19 mortality (P < 0.05), and the AUC from highest to lowest was combined effect > CRP > PCT > NLR, respectively. However, the diagnostic value for combined effect was not statistically superior to CRP with specificity of 0.64 and 0.71, respectively.
ROC analysis of the PCT, CRP, NLR and combined effect for prediction of COVID-19 mortality. The reference line was coloured with grey; the ROC of CRP was coloured with light-green; ROC of PCT was coloured with light-purple; ROC of NLR was coloured with light-blue; and ROC of combined PCT, CRP and NLR together was coloured with light-pink.
Risk factor for COVID-19 mortality using univariate analysis
According to the cut-off-value of AUC, the levels of PCT, CRP and NLR were categorized into two groups. Results shown that several clinical factors were statistically significant risk associated with COVID-19 mortality, which included cancer, ARDS, hypohepatia, renal insufficiency, heart failure and shock. Furthermore, we found that PCT (≥ 0.10 ng/mL), CRP (≥ 52.14 mg/L) and NLR (NLR ≥ 3.59) had higher risks associated with higher likelihood of developing death with HRs of 12.82, 12.30 and 8.6, respectively (see Supplementary Table S1 online and Fig. 3).
Kaplan–Meier plot for probability of survival for PCT, CRP, NLR and combined effect for prediction of COVID-19 mortality. The blue lines were the patients with COVID-19 with lower levels of inflammatory factors, and the red lines were the patients with COVID-19 with higher levels of inflammatory factors.
Risk factor for COVID-19 mortality using multivariate analysis
Adjustment for age and sex, the risk associations did not weaken between the PCT, CRP and NLR and death. Furthermore, PCT (≥ 0.10 ng/mL) and CRP (≥ 52.14 mg/L) exhibited independent increasing risks of mortality after adjusting for age, sex, cancer, ARDS, hypohepatia, renal insufficiency, heart failure and shock in model 2, with HRs of 52.68 (95% CI: 1.77–1571.66) and 5.47 (95% CI: 1.04–28.72), respectively. However, NRL (≥ 3.59) was not found to be an independent risk factor for death in multivariate analysis (Table 3).
Risk factor for COVID-19 mortality in the subgroup analysis
In the subgroup analysis (Table 4), we found the elevated PCT level was associated with increasing risk of mortality in the old age group (age ≥ 60 y), and the association did not change after adjusting for complications. In the severe group, a marginal association was found between PCT level and death (HR = 7.46, 95% CI: 0.98–56.54), however, the association increasing risk of mortality was observed after adjustment for complications (HR = 39.37, 95% CI: 1.50–1,036.84).
We also found the elevated CRP levels were associated with increasing risk of mortality in the old age group (age ≥ 60 y), in male group and severe group. However, there were no risk associations after adjusting for complications (P > 0.05). Unfortunately, NLR level had not been addressed as independent predictor of survival in patients with COVID-19 in different age, sex and severe groups (P > 0.05).
Discussion
Our results had demonstrated that patients in the critically severe and severe groups had elevated levels of PCT and NLR compared with moderate group, and the CRP level was highest in the critically severe group, the lowest in the moderate group as expected. After Adjusting for other covariates, the serum elevated PCT (≥ 0.10 ng/mL) and CRP (≥ 52.14 mg/L) were independent risk factors for mortality in hospitalized patients with COVID-19. However, elevated NLR (≥ 3.59) was not the independent risk factor for mortality in our study. Furthermore, the elevated PCT levels were still associated with increasing risk of mortality in the old age group (age ≥ 60 y) and in the critically severe and severe patients after adjusting for complications.
The reported observed symptoms of COVID-19 were generally non-specific, the fever was the most common symptom, followed by cough and fatigue, dyspnea and et al.21. In our study, the fever and the cough were also found as the common symptoms, followed the chest distress or shortness of breath. This may be because the patients with COVID-19 in our study were not included the mild clinical type. The overall case-fatality rate was 22.37% in our study, and all the deaths were observed in the critically severe group with mortality rate of 53.13% (17/32), which was consistently with previous research22.
COVID-19 is a highly infectious pneumonia caused by a SARS-CoV-2, and other sensitive indicators such as inflammation factors had to reflect lung lesion changes and disease severity except for CT scan23. PCT is a calcitonin-related gene product expressed by human epithelial cells in response to bacterial infections24, which is used as a blood infection biomarker for the purpose of guiding antibiotic therapy in the context of pulmonary infection25,26. CRP, an acute-phase protein secreted by the liver, is another parameter used to response to bacterial infection, which was used in the early diagnosis of pneumonia27.
In this study, our results had found that the levels of PCT and CRP were associated with COVID-19 severity, which indicated patients with COVID-19 always companied by the bacterial infections. Also, the serum levels of PCT and CRP had diagnostic values for COVID-19 mortality with higher sensitivity. After adjusting for other covariates, the serum elevated PCT (≥ 0.10 ng/mL) and CRP (≥ 52.14 mg/L) were independent risk factors for mortality in hospitalized patients with COVID-19. It’s worth noting that the death for old patients (age ≥ 60 y) and severe patients were more susceptible to elevated PCT. However, this association was not observed in the CRP biomarker after adjusting for complications. From the infinity HRs and marginal P value (0.065), we expected that small sample size may be the most reasons for this association. Thus, elevated levels of PCT and CRP may help to identify patients with dismal prognosis and prompt intervention in order to improve outcomes, especially in the old and severe patients with COVID-19.
NLR was an another important inflammation indicator, which was associated with a poor prognosis for patients with many disease28,29. The NLR reflects the balance between the innate (i.e., neutrophils) and adaptive (i.e., lymphocytes) immune responses in the body30, and the elevated NLR values were susceptible for progress of COVID-19 infection11,31. Researches had indicated that several factors may contribute to COVID-19 associated lymphopenia. Firstly, the angiotensin-converting enzyme 2 (ACE2) plays an important role in cellular entry for SARS-CoV-2, which invades host human cells by binding to ACE2 receptor, thus the ACE2-expressing cell lymphocytes act as target cell and are leaded to lysis by COVID-19 infection32. Secondly, COVID-19 was found to be characterized as a “cytokine storm” with a pronounced systemic increase of inflammatory mediators and cytokines33, and those increased concentrations of cytokines may promote lymphocyte apoptosis34. Furthermore, increased activation of cytokines may impair lymphocyte turnover by atrophy of lymphoid organs35 or inhibiting lymphocyte proliferation36.
Our results had demonstrated that critical and severe clinical patients had elevated NLR levels compared with moderate group. However, in this study, we did not find the elevated NLR (≥ 3.59) was associated with increased risk of death, neither in other subgroup population.
Furthermore, we also explored the associations between the highest levels of PCT, CRP and NLR and mortality in patients with COVID-19 during the treatment, however, no significant risk factors were observed. Meanwhile, we categorized PCT and CPR levels into different groups according to the normal reference values of less than 0.05 ng/mL and 3 mg/L, respectively, and no significant associations with increased risk of death were found.
Some limitations existed in the present study. First, the available sample size and number of deaths were limited, which may reduce the validity when building prediction model and increase the risk of overfitting the model. Second, the inflammation factors were not monitored regularly, thus we could not longitudinally evaluate the association between the dynamic changes of PCT, CRP and NLR and death during the disease course. Third, the identified cutoffs for PCT, CRP and NLR in this study need to be validated in external patients with COVID-19.
Conclusions
In this study, we confirmed that baseline levels of PCT (≥ 0.10 ng/mL) and CRP (≥ 52.14 mg/L) have been addressed as independent predictors of survival in patients with COVID-19, but the elevated NLR do not seem useful for discriminating the death in COVID-19 infected patients. Furthermore, elevated PCT levels were still associated with increasing risk of mortality in the old age group (age ≥ 60 y) and in the critically severe and severe patients after adjustment for complications. Therefore, early laboratory indices at baseline can assist clinicians in formulating a tailored treatment approach and promptly provide intensive care to those who are in greater need. However, small sample size of patients is short of representive, in the future, the researchers will collaborate in the world with a few medical facilities in the area to confirm the relationship between the inflammation factors and survival in patients with COVID-19 to improve the reliability of the study.
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Wang, D. et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA https://doi.org/10.1001/jama.2020.1585 (2020).
Zhu, N. et al. A novel coronavirus from patients with pneumonia in China, 2019. N. Engl. J. Med. 382, 727–733. https://doi.org/10.1056/NEJMoa2001017 (2020).
Chan, J. F. et al. Genomic characterization of the 2019 novel human-pathogenic coronavirus isolated from a patient with atypical pneumonia after visiting Wuhan. Emerg. Microbes Infect. 9, 221–236. https://doi.org/10.1080/22221751.2020.1719902 (2020).
4World Health Organization. WHO Director-General's Opening Remarks at the Media Briefing on COVID-19–22 April 2020. https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19--22-april-2020 (2020).
5National Health Commision of the People's Republic of China. Novel Coronavirus (SARS-CoV-2) Situation Reports. https://www.nhc.gov.cn/xcs/yqtb/202004/ab35f22c371149ad95284b1539f2a8a6.shtml (2020).
Liu, Y. et al. Clinical and biochemical indexes from 2019-nCoV infected patients linked to viral loads and lung injury. Sci. China Life Sci. 63, 364–374. https://doi.org/10.1007/s11427-020-1643-8 (2020).
Wang, Y. Q. et al. Analysis of myocardial injury in patients with COVID-19 and association between concomitant cardiovascular diseases and severity of COVID-19. J. Med. Virol. 48, E008. https://doi.org/10.1002/jmv.2575710.3760/cma.j.cn112148-20200225-00123 (2020).
Li, H. et al. SAA is a biomarker to distinguish the severity and prognosis of Coronavirus Disease 2019 (COVID-19). J. Infect. https://doi.org/10.3233/xst-20067010.1016/j.jinf.2020.03.035 (2020).
Zhou, Y., Zhang, Z., Tian, J. & Xiong, S. Risk factors associated with disease progression in a cohort of patients infected with the 2019 novel coronavirus. J. Clin. Med. 9, 428–436. https://doi.org/10.3390/jcm904094110.21037/apm.2020.03.26 (2020).
Peng, X. et al. Clinical characteristics and outcomes of 112 cardiovascular disease patients infected by 2019-nCoV. Pediatr. Pulmonol. 48, E004. https://doi.org/10.1002/ppul.2471810.3760/cma.j.cn112148-20200220-00105 (2020).
Lagunas-Rangel, F. A. Neutrophil-to-lymphocyte ratio and lymphocyte-to-C-reactive protein ratio in patients with severe coronavirus disease 2019 (COVID-19): a meta-analysis. Radiology https://doi.org/10.1148/radiol.202020123710.1002/jmv.25819 (2020).
Liu, Y. et al. Neutrophil-to-lymphocyte ratio as an independent risk factor for mortality in hospitalized patients with COVID-19. J. Infect. https://doi.org/10.1016/j.jinf.2020.04.002 (2020).
13Health Commission of Hubei Province. Epidemic Situation of COVID-19 in Hubei Province on April 24, 2020. https://wjw.hubei.gov.cn/fbjd/dtyw/202004/t20200425_2246903.shtml (2020).
14Statistical Bureau of Xiaogan City. Statistical Yearbook of Xiaogan in 2018. https://tjj.xiaogan.gov.cn/ndsj/846271.jhtml (2020).
15Health Commission of Xiaogan City. Epidemic Situation of COVID-19 in Xiaogan City (March 20, 2020). https://wjw.xiaogan.gov.cn/gsgg/844468.jhtml (2020).
16Suihua Municipal People's Government. Epidemic Situation of COVID-19 in Suihua City (April 24, 2020). https://www.suihua.gov.cn/pages/website/content.html?permission_id=43&id=26182 (2020).
Li, Q. et al. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N. Engl. J. Med. 382, 1199–1207. https://doi.org/10.1056/NEJMoa2001316 (2020).
18World Health Organization. Clinical Management of Severe Acute Respiratory Infection When Novel Coronavirus (nCoV) Infection is Suspected: Interim Guidance, 13 March 2020. https://www.who.int/publications-detail/clinical-management-of-severe-acute-respiratory-infection-when-novel-coronavirus-(ncov)-infection-is-suspected (2020).
19National Institute for Viral Disease Control and Prevention of China. Pecific Primers and Probes for Detection 2019 Novel Coronavirus. https://ivdc.chinacdc.cn/kyjz/202001/t20200121_211337.html (2020).
20The National Health Commission of People's Republic of China. Interpretation of New Coronavirus Pneumonia Diagnosis and Treatment Plan (Trial Version 7) (in Chinese). https://www.nhc.gov.cn/yzygj/s7653p/202003/46c9294a7dfe4cef80dc7f5912eb1989.shtml (2020).
Xu, G. et al. Clinical pathway for early diagnosis of COVID-19: updates from experience to evidence-based practice. Clin. Rev. Allergy Immunol. https://doi.org/10.1007/s12016-020-08792-8 (2020).
Novel Coronavirus Pneumonia Emergency Response Epidemiology. The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19) in China. Zhonghua liu xing bing xue za zhi = Zhonghua liuxingbingxue zazhi 41, 145–151. https://doi.org/10.3760/cma.j.issn.0254-6450.2020.02.003 (2020).
Wang, L. C-reactive protein levels in the early stage of COVID-19. Medecine et maladies infectieuses https://doi.org/10.1016/j.medmal.2020.03.007 (2020).
Muller, B. et al. Calcitonin precursors are reliable markers of sepsis in a medical intensive care unit. Crit. Care Med. 28, 977–983. https://doi.org/10.1097/00003246-200004000-00011 (2000).
25US Food and Drug Administration. FDA Press Release. FDA Press Release. FDA Clears Test to Help Manage Antibiotic Treatment for Lower Respiratory Tract Infections and Sepsis. Feb 23, 2017. https://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm543160.htm (2017).
Lee, S. H. et al. Procalcitonin as a diagnostic marker in differentiating parapneumonic effusion from tuberculous pleurisy or malignant effusion. Clin. Biochem. 46, 1484–1488. https://doi.org/10.1016/j.clinbiochem.2013.03.018 (2013).
Kalra, L. et al. Elevated C-reactive protein increases diagnostic accuracy of algorithm-defined stroke-associated pneumonia in afebrile patients. Int. J. Stroke Off. J. Int. Stroke Soc. 14, 167–173. https://doi.org/10.1177/1747493018798527 (2019).
Li, W., Ai, X., Ni, Y., Ye, Z. & Liang, Z. The association between the neutrophil-to-lymphocyte ratio and mortality in patients with acute respiratory distress syndrome: a retrospective cohort study. Shock (Augusta, Ga.) 51, 161–167. https://doi.org/10.1097/shk.0000000000001136 (2019).
Lu, A. et al. Prognostic significance of neutrophil to lymphocyte ratio, lymphocyte to monocyte ratio, and platelet to lymphocyte ratio in patients with nasopharyngeal carcinoma. Biomed. Res. Int. 2017, 3047802. https://doi.org/10.1155/2017/3047802 (2017).
Afari, M. E. & Bhat, T. Neutrophil to lymphocyte ratio (NLR) and cardiovascular diseases: an update. Expert Rev. Cardiovasc. Ther. 14, 573–577. https://doi.org/10.1586/14779072.2016.1154788 (2016).
Zhu, J. et al. Clinical characteristics of 3,062 COVID-19 patients: a meta-analysis. J. Med. Virol. https://doi.org/10.1016/j.jinf.2020.04.00310.1002/jmv.25884 (2020).
Zou, X. et al. Single-cell RNA-seq data analysis on the receptor ACE2 expression reveals the potential risk of different human organs vulnerable to 2019-nCoV infection. Front. Med. https://doi.org/10.1007/s11684-020-0754-0 (2020).
Li, T., Lu, H. & Zhang, W. Clinical observation and management of COVID-19 patients. Emerg. Microbes Infect. 9, 687–690. https://doi.org/10.1080/22221751.2020.1741327 (2020).
Singh, S., Sharma, A. & Arora, S. K. High producer haplotype (CAG) of -863C/A, -308G/A and -238G/A polymorphisms in the promoter region of TNF-alpha gene associate with enhanced apoptosis of lymphocytes in HIV-1 subtype C infected individuals from North India. PLoS ONE 9, e98020. https://doi.org/10.1371/journal.pone.0098020 (2014).
Chan, J. F. et al. Simulation of the clinical and pathological manifestations of Coronavirus Disease 2019 (COVID-19) in golden Syrian hamster model: implications for disease pathogenesis and transmissibility. Clin. Infect. Dis. Off. Publ. Infect. Dis. Soc. Am. https://doi.org/10.1093/cid/ciaa325 (2020).
Fischer, K. et al. Inhibitory effect of tumor cell-derived lactic acid on human T cells. Blood 109, 3812–3819. https://doi.org/10.1182/blood-2006-07-035972 (2007).
Acknowledgements
The authors would like to thank the doctors, nurses and supportive staffs worked in the Hanchuan City people’s hospital and Suihua first hospital, who were fighting for COVID-19 together.
Author information
Authors and Affiliations
Contributions
X.J. and X.C. collected data, interpreted data, and drafted the initial manuscript. Z.R., W.M., P.C. and L.X. collected data and conducted an initial literature review, and W.Q. cleared the data. Z.F. and Z.S. conceptualized and designed the study, supervised the analysis, critical revision of the manuscript for important intellectual content and took responsible for the article.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Xu, Jb., Xu, C., Zhang, Rb. et al. Associations of procalcitonin, C-reaction protein and neutrophil-to-lymphocyte ratio with mortality in hospitalized COVID-19 patients in China. Sci Rep 10, 15058 (2020). https://doi.org/10.1038/s41598-020-72164-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-72164-7
This article is cited by
-
The clinical and epidemiological characteristics of a series of patients living with HIV admitted for COVID-19 in a district hospital
BMC Infectious Diseases (2023)
-
The role of procalcitonin in predicting risk of mechanical ventilation and mortality among moderate to severe COVID-19 patients
BMC Infectious Diseases (2022)
-
The cerebrospinal fluid neutrophil to lymphocyte ratio is a sensitive biomarker for bacterial meningitis in children
Child's Nervous System (2022)
-
Leukocyte glucose index as a novel biomarker for COVID-19 severity
Scientific Reports (2022)
-
Multimodal single-cell omics analysis identifies epithelium–immune cell interactions and immune vulnerability associated with sex differences in COVID-19
Signal Transduction and Targeted Therapy (2021)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.