Abstract
Accumulating evidence indicates that persistent Helicobacter pylori gastric infection influences immune responses to oral enteric vaccines. We studied the association between pre-existing H. pylori serum IgG and serum pepsinogens levels (PGs) as markers of gastric inflammation and the immune response to single-dose live oral cholera vaccine CVD 103-HgR in Malian adults. Baseline sera obtained during a phase 2 safety/immunogenicity clinical trial of cholera vaccine CVD 103-HgR among 93 healthy Malian adults were tested for H. pylori IgG antibodies and PGI and PGII levels using enzyme linked immunosorbent assays. Overall 74/93 (80%) vaccine recipients were H. pylori IgG seropositive at baseline. Vibriocidal antibody seroconversion (≥ fourfold increase 14 days following administration of CVD 103-HgR compared to baseline) among vaccine recipients was 56%. However, vibriocidal antibody seroconversion was markedly higher among H. pylori seropositives than seronegatives 64% vs. 26% (p = 0.004); adjusted relative risk: 2.20 (95% confidence intervals 1.00–4.80; p = 0.049). Among H. pylori seropositive vaccine recipients, there were no significant associations between PGI, PGII and PGI:PGII levels and vibriocidal seroconversion. The enhanced seroconversion to oral cholera vaccine CVD 103-HgR among H. pylori seropositive African adults provides further evidence of the immunomodulating impact of H. pylori on oral vaccine immunogenicity.
Similar content being viewed by others
Introduction
Live attenuated oral enteric vaccines have played an important role in global public health by reducing the disease burden caused by the target pathogens. Thus, oral polio vaccine (OPV) led to eradication of transmission of wild type 2 (WPV2) (no cases since 1999) and presumed eradication of WPV3 transmission (no cases since 2012). WPV1 transmission is currently limited to just two countries, Pakistan and Afghanistan1. Similarly, attenuated oral rotavirus vaccines have substantially reduced gastroenteritis hospitalizations and mortality following their introduction as a routine infant vaccine2. Mass immunization of Chilean schoolchildren with live oral Ty21a typhoid vaccine markedly reduced the incidence of both confirmed typhoid and paratyphoid B disease3,4. Oral cholera vaccines have blunted the intensity of seasonal cholera epidemics in endemic areas5. These successes have been achieved despite the lower immunogenicity and efficacy of oral vaccines in persons living in developing countries compared to persons living in industrialized nations (reviewed in6,7). However, the reason(s) for the diminished immunologic response to oral live attenuated vaccines in developing countries is incompletely understood. Experience with live oral cholera vaccine CVD-103-HgR exemplifies the above phenomenon6. A single 5 × 108 colony forming unit (CFU) dose of CVD-103-HgR elicits high titers of serum vibriocidal antibody in ~ 92–95% of US adults, and is highly protective against cholera8,9,10. However, in vaccinated children and adults living in developing countries, a higher dose (~ 5 × 109 CFU) is needed to achieve similarly high vibriocidal seroconversion rates6,11,12,13. Low socioeconomic status13, pre-existing elevated vibriocidal titers13 and small bowel bacterial overgrowth were some risk factors associated with diminished vibriocidal responses14. Individuals with blood group O were shown to develop higher vibriocidal titers15, and the pre-immunization elimination of helminths was shown to significantly raise the vibriocidal antibody response in non-blood group O children16.
Achieving the desired immune response to a live oral vaccine requires successful passage of viable vaccine organisms through the hostile acidic gastric environment to reach the immunologic inductive sites of the gut-associated lymphoid tissue in the small intestine. Helicobacter pylori chronically colonizes the stomach of persons in developing countries, sometimes resulting in the development of peptic ulcers17 and gastric cancer in older individuals18 (reviewed in19,20). Given the high prevalence of chronic H. pylori infection in developing countries, the role such chronic infection in modulating the immune response to oral enteric vaccines is of particular interest. Chronic H. pylori infection can markedly alter gastric physiology, including gastric acid secretion19,20, and as a consequence can indirectly influence immune responses to a variety of antigens delivered orally, including cholera vaccine.
We previously reported a notable inverse association between baseline H. pylori seropositivity and vibriocidal antibody seroconversion following oral vaccination with CVD 103-HgR in Chilean children < 5 years of age21. In contrast, in older children 5–9 years of age, a positive association was found in relation to gastric inflammation, as measured by serum pepsinogen I (PGI)21. In a somewhat analogous study of a live oral typhoid vaccine conducted among U.S. adults, superior immune responses were recorded following immunization with oral attenuated Salmonella Typhi vaccine strain CVD 908-htrA in adults who were seropositive for H. pylori and whose serum PGs indicated more advanced gastritis22. Thus, the association between chronic H. pylori infection and the immune response to oral vaccines is complex and multifactorial, and differences according to age and socioeconomic level should be assessed.
A study of the immunogenicity of CVD 103-HgR in Malian adults offered the opportunity to examine in another geographic site (West Africa) the association of pre-existing H. pylori immunoglobulin G (IgG) serum antibodies and serum PGs as markers of gastric inflammation with vibriocidal antibody seroconversion following immunization of adults with this live oral cholera vaccine. Based on our previous data in different populations, our hypothesis was that H. pylori seropositivity would be associated with higher vibriocidal antibody seroconversion in Malian adults.
Materials and methods
Study design and population
We used anonymized specimens of stored sera obtained from participants in a phase II clinical trial with CVD 103-HgR vaccine in Mali, West Africa23. Healthy adults aged 18–45 years from Bamako received a single oral dose of ≥ 2 × 108 CFU (low-dose) or ≥ 2 × 109 CFU (high-dose) of CVD 103-HgR administered in a buffer cocktail. The original trial included in its design the tertiary objective of assessing the association between H. pylori IgG sero-prevalence and the immune response to CVD 103-HgR.
Definition of the study variables
The dependent variable, vibriocidal seroconversion23, was defined as a ≥ fourfold increase in serum vibriocidal antibody titer 14 days post-vaccination compared to the baseline titer.
The main independent variable was H. pylori seropositivity at baseline defined as the presence of H. pylori-specific IgG antibodies in the pre-vaccination sera (for cutoff value please see the laboratory methods section). H. pylori-positive sera were further tested for the presence of IgG antibodies to the cytotoxin-associated gene A (CagA) protein, a marker for virulent H. pylori strains. Additional independent variables included serum levels of PGs as a measure of gastric inflammation24,25. Serum PGI and PGI are proenzymes of the enzyme pepsin. The PGs are secreted into the gastric lumen and can be found in the serum26,27. With increasing severity of H. pylori gastritis, serum PGI and PGII levels become elevated, but when atrophic changes occur in the corpus, the PGI level and the PGI:PGII ratio decrease. These markers can predict atrophic gastritis, intestinal metaplasia and gastric cancer24,25,28,29. A cutoff value of serum PGI of < 30 μg/L or of a PGI:PGII ratio < 3.0, is used to determine the presence of atrophic gastritis/ gastric atrophy, as recommended by the manufacturer. However, there is no consensus in the literature regarding the best cut-off values24,25,28,29,30,31,32. A PGI:PGII ratio of 4 to 6 was proposed to enhance the sensitivity of serum PGs in identifying atrophic gastritis24,30,31,32. The occurrence of atrophic gastritis is low, and increases after age 45 years33. Thus, the expected number of persons with atrophic gastritis in this small sample of healthy young adult (ages 18–45, median 22 years) is low. Accordingly, we used the lowest quartiles as cut-off values (73.6 μg/L for PGI and 5.35 for PGI:PGII); these are equivalent to clinically relevant values24,30,31,32.
The following variables were considered as covariates and potential confounders: age in years (analyzed as a continuous variable), and sex. Pre-vaccination vibriocidal antibody titer was also assessed, given our previous observations of an inverse association between baseline levels and the immune response to CVD 103-HgR6,13,15.
Since H. pylori infection might be a marker of broad exposure to enteric pathogens, we assessed the level of serum IgG antibodies to Shigella flexneri 2a lipopolysaccharide as an additional independent variable. This enhances the understanding of the specificity of the association between H. pylori infection and oral enteric vaccines.
The categories of S. flexneri 2a serum IgG antibody were defined according to the knowledge that Shigella is highly endemic in developing countries, already at a very young age34,35,36. Thus, Malian adults were presumed to have been exposed to Shigella infections during their life course. Therefore, we compared participants with the highest levels of S. flexneri 2a serum IgG antibody (highest quartile [Q4]) to those with lower levels (Q1–Q3).
Laboratory methods
Sera obtained in the course of the above-mentioned clinical trial23 were shipped from Mali to the Center for Vaccine Development and Global Health, University of Maryland School of Medicine, Baltimore, USA and stored at − 20 °C until testing. Vibriocidal antibody levels before and after vaccination were examined as described23. Sera were shipped to Tel Aviv University for measurement of H. pylori IgG antibody and PGs levels testing. H. pylori IgG antibodies were measured using a commercial enzyme linked immunosorbent assay (ELISA) kit (Enzygnost Anti-Helicobacter pylori II/IgG kit, Siemens Diagnostics Product GmbH, Marburg, Germany) following the manufacturer's instructions. An optical density (OD) of 0.250 or greater were considered positive. The presence of IgG antibody against recombinant CagA protein was measured in H. pylori-positive sera according to an in-house ELISA protocol18,33. Concentrations of serum PGI and PGII were quantified by ELISA (Biohit Inc., Helsinki, Finland) following the manufacturer's instructions. Serum IgG antibody titers to S. flexneri 2a lipopolysaccharide was measured using an in-house ELISA protocol at the laboratory of Prof. Daniel Cohen, Tel Aviv University, Israel37 and results were expressed in ELISA units.
Statistical analysis
Descriptive statistics (medians and interquartile ranges (IQR) for continuous variables, and frequencies and percentages for categorical variables) were used to describe the study sample. Chi square and Fisher Exact tests, where appropriate, were used to examine differences between H. pylori IgG seropositive and seronegative vaccinees in categorical variables and Mann–Whitney test for continuous variables (e.g., serum PGs). The Chi square test was also used to examine differences in the percentage of vaccinees who developed vibriocidal antibody seroconversion 14 days following vaccination with CVD 103-HgR, according to H. pylori seropositivity and other categorical variables. The difference in the median age between participants with and without seroconversion at day 14 was assessed using the Mann–Whitney test.
A log-binomial model of the generalized linear models38,39,40 was performed to examine the association between H. pylori IgG seropositivity and vibriocidal seroconversion, while controlling for potential confounders. The use of the log-binomial model is recommended38,40 if the dependent variable is common, as in our study, in which 52/93 (55.9%) of the participants had vibriocidal antibody seroconversion 14 days following immunization with CVD 103-HgR.
The selection of variables to be included in the multivariable analysis was based on our pre-specified main hypothesis of the relation between H. pylori seropositivity (the main independent variable) and vibriocidal seroconversion following immunization with CVD 103-HgR, while relying on microbiological, immunological and epidemiological knowledge in the field21,22. We adjusted for age given the evidence that this variable might affect the immune response to oral enteric vaccines21,22, and that H. pylori gastric inflammation and pathology might increase with age41,42,43,44. Lastly, we considered S. flexneri IgG serum antibody as a proxy for exposure enteric infections21. Accordingly, we assessed the specificity of the association between H. pylori sero-prevalence and vibriocidal seroconversion following immunization with CVD 103 HgR. Relative risk (RR) and 95% confidence intervals (CI) were obtained from this model.
The Mann–Whitney test and box plot were used to assess difference in vibriocidal antibody seroconversion level (with natural logarithm transmutation) according to H. pylori seropositivity. In additional analyses we assessed difference in the median baseline level of vibriocidal antibody titer (with natural logarithm transmutation) between participants with and without seroconversion at day 14, using the Mann–Whitney test and box plot. We also performed a multivariable model that included both H. pylori seropositivity and baseline vibriocidal antibody level. Statistical significance was set at p < 0.05. Data were analysed using IBM SPSS version 25 (Armonk, New York, USA).
Ethical aspects
The Institutional Review Board (IRB) of the University of Maryland, Baltimore and the local Malian IRB approved the original trial with CVD 103-HgR including the objective of this study that was defined as a tertiary objective. Volunteers were enrolled after providing an informed consent23. The ethics committee of Tel Aviv University also approved the protocol of the current study.
We confirm that all methods were performed in accordance with the relevant guidelines and regulations.
Results
The 93 of 97 participants who had data on both H. pylori serostatus and vibriocidal antibody seroconversion 14 days after vaccination with CVD 103-HgR were included in the study. Of these, 39 were males [42%] and the median age was 22 years. The high-dose of CVD 103-HgR (≥ 2 × 109 CFU) was given to 46 participants (49.5%) and the low-dose (≥ 2 × 108 CFU) to 47 subjects (50.5%). H. pylori IgG seropositivity was evident in 74 participants (80% [95% CI 70–87%]), of whom 55 (74%) tested positive for CagA IgG antibody. There was no significant difference between H. pylori seropositive and seronegative participants with respect to age (p = 0.9), sex (p = 0.6) or vaccine dose (p = 0.2) (Table 1). Serum PGI levels were similar between H. pylori seropositive and seronegative vaccinees (median 98.7 µg/L vs. 90.3 µg/L, p = 0.3) but a significantly higher level of PGII was found in the H. pylori seropositive group (median 14.6 µg/L vs. 10.6 µg/L, p = 0.012). The PGI:PGII ratio was significantly lower among H. pylori seropositive vaccinees compared to seronegatives: median of 6.6 vs. 8.7, p = 0.022 (Table 1).
The fold-increase in vibriocidal antibody titer at day 14 compared to the baseline level ranged from 0.02 to 1,024, the value of the 25th percentile was 0.5, the median was 4, and the 75th percentile value was 16. The distribution of the fold increase is presented in Supplementary Table S1. The levels of fold-increase of vibriocidal antibody titer was higher among H. pylori positive vs. negative vaccinees (p = 0.034 by the Mann–Whitney test, see Supplementary Fig.S1 online).
Four-fold increase in vibriocidal antibody seroconversion 14 days post-vaccination compared to baseline level was evident in 52 participants (56% [95% CI 46–66%]). The median age of participants with vibriocidal antibody seroconversion was 24 years (IQR 9) vs. 21 (IQR 8) among those without seroconversion at day 14, following immunization with CVD 103-HgR (p = 0.07 by the Mann–Whitney test). Table 2 describes the bivariate analysis of vibriocidal antibody seroconversion at day 14, after vaccination with CVD 103-HgR, according to other independent variables.
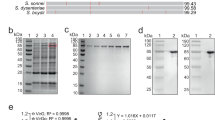
There was no significant difference in vibriocidal antibody seroconversion according to sex (p = 0.7), or vaccine dose (p = 0.9). The pre-vaccination vibriocidal antibody level was significantly lower (p = 0.001) among persons who seroconverted than among those who did not (Fig. 1).
Box plots of baseline vibriocidal antibody titer (natural logarithm transmutation) (Y-axis) according to seroconversion status at day 14 after vaccination with the cholera vaccine CVD 103-HgR (X-axis) among Malian adults. Vibriocidal antibody titer seroconversion was defined as fourfold rise at day 14 after vaccination compared to baseline level. The line in the mid of the box represents the median level, lower bound of the box represents the 25th percentile, the upper bound of the box represents the 75th percentile, the lowest point of the lower whisker represents the minimum and the highest point of the upper represents the maximum. p value = 0.001 by Mann–Whitney test.
Vibriocidal antibody seroconversion was significantly higher among H. pylori seropositive vaccinees than seronegative ones (64% vs. 26%, p = 0.004), and in individuals with high-level (highest quartile) of S. flexneri 2a serum IgG anti-LPS antibody than those with lower antibody levels (75% vs. 49%, p = 0.029) (Table 2).
Among H. pylori seropositive individuals, there was no significant difference between vaccinees with and without vibriocidal antibody seroconversion with respect to CagA IgG seropositivity (70% vs. 82%, p = 0.2) or serum PGI, PGII or PGI:PGII levels (Table 3).
A multivariable model that adjusted for age (as a continuous variable) and levels of S. flexneri 2a serum IgG anti-LPS antibody, showed a significant positive association between H. pylori seropositivity and vibriocidal seroconversion: adjusted RR 2.20 (95% CI 1.00–4.80), p = 0.049 (Table 4). This model showed no significant association between age and vibriocidal antibody seroconversion (adjusted RR 1.00 [95% CI 0.99–1.03], p = 0.4) or levels of S. flexneri 2a IgG anti-LPS (adjusted RR 1.32 [95% CI 0.95–1.84), p = 0.1).
An additional multivariable model included H. pylori seropositivity, and baseline vibriocidal antibody level as an additional independent variable (continuous), this did not affect the positive association observed between H. pylori and vibriocidal antibody seroconversion (adjusted RR 2.41 [95% CI 1.13–5.12], p = 0.022). This model also showed that baseline vibriocidal was inversely related to vibriocidal seroconversion after vaccination with CVD 103-HgR (adjusted RR 0.73 [95% CI 0.60–0.88], p = 0.001).
Discussion
We found a positive association between baseline H. pylori IgG antibody seropositivity and vibriocidal antibody seroconversion 14-days following immunization with a single dose of CVD 103-HgR live oral cholera vaccine among Malian adults. This association is reported for the first time in persons from a very low-income country, a setting in which many oral enteric vaccines have shown lower immunogenicity and efficacy compared to populations in high-income countries. The positive association between H. pylori infection and vibriocidal antibody seroconversion was independent of age among these adults and of a high level of S. flexneri serum IgG anti-LPS antibody, a proxy for exposure to enteric pathogens. Interestingly, the association between H. pylori seroprevalence and the immune response to CVD 103-HgR was not affected by baseline vibriocidal antibody level, serum PGs levels, markers of gastric inflammation or infections with H. pylori CagA-positive (putatively more virulent) strains.
Age and S. flexneri IgG antibodies were related to vibriocidal antibody serconversion in the bivariate analysis only. There was no significant correlation between age and S. flexneri IgG antibodies, likely since exposure to Shigella infection occurs during childhood in Mali34,35,36.
Findings from the current study confirm our previous observations regarding the involvement of H. pylori infection in the immune response to oral enteric vaccines21,22. The positive association between baseline H. pylori seropositivity and vibriocidal antibody seroconversion following vaccination with CVD 103-HgR among Malian adults is in agreement with findings documented among school-age (5–9 years) Chilean children21. In younger Chilean children < 5 years of age, on the other hand, H. pylori seroprevalence was inversely related to vibriocidal antibody seroconversion after immunization with CVD 103-HgR21. These observations can be explained by the age-related impact of H. pylori infection on gastric physiology. H. pylori infection is acquired in childhood45 and typically most people do not develop symptoms. However, the histopathological severity of gastritis increases with age, even in the absence of symptoms44. H. pylori antral-predominant chronic gastritis might increase the secretion of gastric acid, resulting in an enhanced gastric acid barrier20,46, while H. pylori infection and corpus-predominant gastritis might induce gastric hypochlorhydria, which usually occurs in adulthood. Thus, the transit of attenuated oral vaccine strains from the stomach into the small intestine might be enhanced in the presence of hypochlorhydria, and the immune responses to oral vaccines might actually increase. This likely explains our observations in Malian adults.
The finding of a positive association between H. pylori seropositivity at baseline and vibriocidal antibody seroconversion following vaccination with CVD 103-HgR in Malian adults corroborates our findings among U.S. adults who were immunized with a live oral typhoid vaccine. In the US adults we observed stronger humoral immune responses following immunization with oral attenuated Salmonella Typhi vaccine strain CVD 908-htrA22 in persons who were H. pylori seropositive at baseline and exhibited evidence of advanced gastritis22.
In the current study, we did not find an association between serum pepsinogen levels and the immune response to the cholera vaccine CVD 103-HgR among Malian adults. This contrasts with the finding of a positive association between serum pepsinogen level and advanced gastritis among US volunteers22. A number of possibilities could explain this discrepancy between the studies, in the associations of serum pepsinogens and the immune response with oral enteric vaccines. One explanation relates to the variation in the epidemiology of H. pylori infection and its related diseases; another relates to differences in public health between the US and the sub-Saharan Africa populations47,48.
Salmonella and V. cholerae are both acid sensitive bacteria49,50, thus supporting the notion that hypochlorhydria can be the mechanism for the association between H. pylori infection and the enhanced immune responses to these vaccines. Further support stems from early studies on cholera disease, showing that hypochlorhydria increases the risk of cholera49,50,51,52,53, as well as studies following the discovery of H. pylori showing a positive association between H. pylori infection and cholera54,55,56 and typhoid fever57,58.
The longstanding systemic and local immune responses induced by H. pylori infection cannot clear the infection19,20. The consequences of persistent H. pylori infection may include having an immunomodulatory influence on the immune response to oral enteric vaccines, in particular to cholera and typhoid vaccines. The findings of Mattsson et al.59 who assessed the production of antibody responses in the stomach as well as serum antibodies following immunization with an oral B subunit whole-cell cholera vaccine in Swedish volunteers59, are consistent with this assumption. Most of their study participants had high levels of vaccine-specific antibody-secreting cells (ASCs) in the duodenum and high serum antibody titers. At the gastric mucosa level, a high frequency of vaccine-specific ASC in the antrum was observed among most H. pylori-infected vaccine recipients but not among those who were not infected with H. pylori. The H. pylori-infected group had substantially higher frequencies of total immunoglobulin A (IgA) ASC in the antrum as compared to the non-infected group59. This report with oral killed cholera vaccine is consistent with our findings with live vaccine that pre-existing H. pylori infection enhances the immune response to oral cholera vaccines. These observations add evidence to support the hypothesis that although there are deleterious effects of chronic H. pylori infection (duodenal ulcers and gastric adenocarcinoma), there may be beneficial effects such as reduced risk of asthma and allergies46,60 and less diarrheal disease in some populations61,62.
Recent reports showed associations between the gut microbiota and the immune response to oral rotavirus vaccines in Ghana and Pakistan63,64,65, which suggest that modulation of the gut microbiome might yield better immune responses65. Collectively, these and our findings support the notion that pre-existing colonization of the gastrointestinal tract with certain bacterial microflora might affect the immunogenicity of oral enteric vaccines.
The relatively small sample size is a potential limitation of our study. Nonetheless, the positive association between H. pylori seropositivity and the immune response to CVD 103-HgR was strong and clear, despite the high prevalence of H. pylori infection in this cohort, which corroborates prevalence estimates from low-income countries19,66. Further studies with larger sample sizes are needed to confirm our findings. Moreover, larger studies with sufficient statistical power are needed to assess possible interactions between H. pylori infection and the vaccine dosage on the immune response to the vaccine. The discrepancy between findings from the current study and our previous findings among Chilean children on the association between H. pylori sero-prevalence and the immune response to CVD 103-HgR, may stimulate the need for multi-center international studies employing the same protocol to explore differences across populations in this association. Although H. pylori seropositivity was measured in baseline sera, prior to immunization, the observational design of our study does not enable causal inference. Since the serological assay that measures H. pylori IgG antibody level does not differentiate between past and recent infection, our findings reflect past exposure to H. pylori and not necessarily recent infection. However, it is well documented that H. pylori infection is mostly acquired in childhood and persists throughout adulthood19,20. Moreover, use of a serological assay in this setting in Mali might be the best tool in terms of specificity given reports of potential misclassification due to non-H. pylori urease-producing bacteria identified by urea breath test67.
Our study has several strengths stemming from both the study design and the novelty of the findings. First, H. pylori IgG seropositivity was correlated with serum PGII and PGI:PGII ratio markers of gastric inflammation, rather than just exposure to the infection. Second, the infection was examined in baseline sera, thus establishing a temporal association. Third, the association was specific to H. pylori and not related to exposure to other enteric infection such as S. flexneri, as demonstrated in the multivariable model. Lastly, the unique positive association between H. pylori seroprevalence and the immune response to an oral enteric vaccine (i.e., V. cholerae oral vaccine strain CVD 103-HgR) is reported for the first time in sub-Saharan Africa, a setting with frequent cholera outbreaks and a high prevalence of H. pylori infection. This increases the generalizability of our findings to other populations in low-income countries.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Bandyopadhyay, A. S., Garon, J., Seib, K. & Orenstein, W. A. Polio vaccination: past, present and future. Future Microbiol. 10, 791–808. https://doi.org/10.2217/fmb.15.19 (2015).
Burnett, E., Jonesteller, C. L., Tate, J. E., Yen, C. & Parashar, U. D. Global impact of rotavirus vaccination on childhood hospitalizations and mortality from diarrhea. J. Infect. Dis. 215, 1666–1672. https://doi.org/10.1093/infdis/jix186 (2017).
Levine, M. M. et al. Ty21a live oral typhoid vaccine and prevention of paratyphoid fever caused by Salmonella enterica Serovar Paratyphi B. Clin. Infect. Dis. 45(Suppl 1), S24-28. https://doi.org/10.1086/518141 (2007).
Gauld, J. S., Hu, H., Klein, D. J. & Levine, M. M. Typhoid fever in Santiago, Chile: Insights from a mathematical model utilizing venerable archived data from a successful disease control program. PLoS Negl. Trop. Dis. 12, e0006759. https://doi.org/10.1371/journal.pntd.0006759 (2018).
Reyburn, R. et al. The case for reactive mass oral cholera vaccinations. PLoS Negl. Trop. Dis. 5, e952. https://doi.org/10.1371/journal.pntd.0000952 (2011).
Levine, M. M. Immunogenicity and efficacy of oral vaccines in developing countries: lessons from a live cholera vaccine. BMC Biol. 8, 129. https://doi.org/10.1186/1741-7007-8-129 (2010).
Steele, A. D. et al. Experiences with rotavirus vaccines: can we improve rotavirus vaccine impact in developing countries?. Hum. Vaccin. Immunother. https://doi.org/10.1080/21645515.2018.1553593 (2019).
Tacket, C. O. et al. Randomized, double-blind, placebo-controlled, multicentered trial of the efficacy of a single dose of live oral cholera vaccine CVD 103-HgR in preventing cholera following challenge with Vibrio cholerae O1 El tor inaba three months after vaccination. Infect. Immun. 67, 6341–6345 (1999).
Levine, M. M. et al. PaxVax CVD 103-HgR single-dose live oral cholera vaccine. Expert Rev. Vaccines. 16, 197–213. https://doi.org/10.1080/14760584.2017.1291348 (2017).
Chen, W. H. et al. ingle-dose live oral cholera vaccine CVD 103-HgR protects against human experimental infection with Vibrio cholerae O1 El Tor. Clin. Infect. Dis. 62, 1329–1335. https://doi.org/10.1093/cid/ciw145 (2016).
Su-Arehawaratana, P. et al. Safety and immunogenicity of different immunization regimens of CVD 103-HgR live oral cholera vaccine in soldiers and civilians in Thailand. J. Infect. Dis. 165, 1042–1048 (1992).
Suharyono, et al. Safety and immunogenicity of single-dose live oral cholera vaccine CVD 103-HgR in 5-9-year-old Indonesian children. Lancet 340, 689–694 (1992).
Gotuzzo, E. et al. Safety, immunogenicity, and excretion pattern of single-dose live oral cholera vaccine CVD 103-HgR in Peruvian adults of high and low socioeconomic levels. Infect. Immun. 61, 3994–3997 (1993).
Lagos, R. et al. Effect of small bowel bacterial overgrowth on the immunogenicity of single-dose live oral cholera vaccine CVD 103-HgR. J. Infect. Dis. 180, 1709–1712. https://doi.org/10.1086/315051 (1999).
Lagos, R. et al. Attenuated live cholera vaccine strain CVD 103-HgR elicits significantly higher serum vibriocidal antibody titers in persons of blood group O. Infect. Immun. 63, 707–709 (1995).
Cooper, P. J. et al. Albendazole treatment of children with ascariasis enhances the vibriocidal antibody response to the live attenuated oral cholera vaccine CVD 103-HgR. J. Infect. Dis. 182, 1199–1206. https://doi.org/10.1086/315837 (2000).
Nomura, A. M. Y., Perez-Perez, G. I., Lee, J., Stemmermann, G. & Blaser, M. J. Relation between Helicobacter pylori cagA status and risk of peptic ulcer disease. Am J. Epidemiol. 155, 1054–1059 (2002).
Blaser, M. J. et al. Infection with Helicobacter pylori strains possessing cagA is associated with an increased risk of developing adenocarcinoma of the stomach. Cancer Res. 55, 2111–2115 (1995).
Suerbaum, S. & Michetti, P. Helicobacter pylori infection. N. Engl. J. Med. 347, 1175–1186. https://doi.org/10.1056/NEJMra020542347/15/1175[pii] (2002).
Atherton, J. C. & Blaser, M. J. Coadaptation of Helicobacter pylori and humans: ancient history, modern implications. J. Clin. Invest. 119, 2475–2487 (2009).
Muhsen, K. et al. Age-dependent association among Helicobacter pylori infection, serum pepsinogen levels and immune response of children to live oral cholera vaccine CVD 103-HgR. PLoS ONE ARTN e8399910.1371/journal.pone.0083999 (2014).
Muhsen, K., Pasetti, M. F., Reymann, M. K., Graham, D. Y. & Levine, M. M. Helicobacter pylori infection affects immune responses following vaccination of typhoid-naive US adults with attenuated Salmonella Typhi oral vaccine CVD 908-htrA. J. Infect. Dis. 209, 1452–1458. https://doi.org/10.1093/infdis/jit625 (2014).
Sow, S. O. et al. Randomized, placebo-controlled, double-blind phase 2 trial comparing the reactogenicity and immunogenicity of a single standard dose to those of a high dose of CVD 103-HgR live attenuated oral cholera vaccine, with Shanchol inactivated oral vaccine as an open-label immunologic comparator. Clin. Vaccine Immunol. 24, doi:UNSP e00265–1710.1128/CVI.00265–17 (2017).
Zhang, X. M., Li, J. X., Zhang, G. Y., Li, X. H. & Gu, H. The value of serum pepsinogen levels for the diagnosis of gastric diseases in Chinese Han people in midsouth China. BMC Gastroenterol. 14, 3. https://doi.org/10.1186/1471-230X-14-3 (2014).
Nardone, G. et al. Diagnostic accuracy of the serum profile of gastric mucosa in relation to histological and morphometric diagnosis of atrophy. Aliment. Pharmacol. Ther. 22, 1139–1146. https://doi.org/10.1111/j.1365-2036.2005.02734.x (2005).
Samloff, I. M. Cellular localization of group I pepsinogens in human gastric mucosa by immunofluorescence. Gastroenterology 61, 185–188 (1971).
Samloff, I. M. & Liebman, W. M. Cellular localization of the group II pepsinogens in human stomach and duodenum by immunofluorescence. Gastroenterology 65, 36–42 (1973).
Miki, K. & Urita, Y. Using serum pepsinogens wisely in a clinical practice. J. Dig. Dis. 8, 8–14. https://doi.org/10.1111/j.1443-9573.2007.00278.x (2007).
Kekki, M., Samloff, I. M., Varis, K. & Ihamaki, T. Serum pepsinogen I and serum gastrin in the 438 screening of severe atrophic corpus gastritis. Scand. J. Gastroenterol. 439–440, 109–116 (1991).
Cao, Q., Ran, Z. H. & Xiao, S. D. Screening of atrophic gastritis and gastric cancer by. J. Dig. Dis. 8, 15–22. https://doi.org/10.1111/j.1443-9573.2007.00271.x (2007).
Graham, D. Y. et al. Noninvasive versus histologic detection of gastric atrophy in a Hispanic population in North America. Clin. Gastroenterol. Hepatol. 4, 306–314. https://doi.org/10.1016/j.cgh.2005.11.003 (2006).
Broutet, N. et al. Pepsinogen A, pepsinogen C, and gastrin as markers of atrophic chronic gastritis in European dyspeptics. Br. J. Cancer. 88, 1239–1247. https://doi.org/10.1038/sj.bjc.6600877 (2003).
Muhsen, K. et al. Prevalence and determinants of serological evidence of atrophic gastritis among Arab and Jewish residents of Jerusalem: a cross-sectional study. BMJ Open. 9, e024689. https://doi.org/10.1136/bmjopen-2018-024689 (2019).
Kotloff, K. L. et al. Burden and aetiology of diarrhoeal disease in infants and young children in developing countries (the Global Enteric Multicenter Study, GEMS): a prospective, case-control study. Lancet 382, 209–222. https://doi.org/10.1016/S0140-6736(13)60844-2 (2013).
Kotloff, K. L. et al. The incidence, aetiology, and adverse clinical consequences of less severe diarrhoeal episodes among infants and children residing in low-income and middle-income countries: a 12-month case-control study as a follow-on to the Global Enteric Multicenter Study (GEMS). Lancet Glob. Health. 7, e568–e584. https://doi.org/10.1016/S2214-109X(19)30076-2 (2019).
Livio, S. et al. Shigella isolates from the global enteric multicenter study inform vaccine development. Clin. Infect. Dis. 59, 933–941. https://doi.org/10.1093/cid/ciu468 (2014).
Cohen, D., Block, C., Green, M. S., Lowell, G. & Ofek, I. Immunoglobulin M, A, and G antibody response to lipopolysaccharide O antigen in symptomatic and asymptomatic Shigella infections. J. Clin. Microbiol. 27, 162–167 (1989).
McNutt, L. A., Wu, C., Xue, X. & Hafner, J. P. Estimating the relative risk in cohort studies and clinical trials of common outcomes. Am. J. Epidemiol. 157, 940–943. https://doi.org/10.1093/aje/kwg074 (2003).
McCullagh, P. N (Chapman and Hall, J. Generalized linear models. Second edition. edn, 1983).
Spiegelman, D. & Hertzmark, E. Easy SAS calculations for risk or prevalence ratios and differences. Am. J. Epidemiol. 162, 199–200. https://doi.org/10.1093/aje/kwi188 (2005).
Wang, X. T. et al. The correlation between histological gastritis staging—"OLGA/OLGIM’ and serum pepsinogen test in assessment of gastric atrophy/intestinal metaplasia in China. Scand. J. Gastroenterol. 52, 822–827. https://doi.org/10.1080/00365521.2017.1315739 (2017).
Nam, J. H. et al. OLGA and OLGIM stage distribution according to age and Helicobacter pylori status in the Korean population. Helicobacter. 19, 81–89. https://doi.org/10.1111/hel.12112 (2014).
Kuipers, E. J. et al. Long-term sequelae of Helicobacter pylori gastritis. Lancet 345, 1525–1528. https://doi.org/10.1016/S0140-6736(95)91084-0 (1995).
Ganga-Zandzou, P. S. et al. Natural outcome of Helicobacter pylori infection in asymptomatic children: a two-year follow-up study. Pediatrics 104, 216–221 (1999).
Muhsen, K., Jurban, M., Goren, S. & Cohen, D. Incidence, age of acquisition and risk factors of Helicobacter pylori infection among Israeli Arab infants. J. Trop. Pediatr. 58, 208–213. https://doi.org/10.1093/tropej/fmr068 (2012).
Cover, T. L. & Blaser, M. J. Helicobacter pylori in health and disease. Gastroenterology 136, 1863–1873 (2009).
Smith, S., Fowora, M. & Pellicano, R. Infections with Helicobacter pylori and challenges encountered in Africa. World J. Gastroenterol. 25, 3183–3195. https://doi.org/10.3748/wjg.v25.i25.3183 (2019).
Holcombe, C. Helicobacter pylori: the African enigma. Gut 33, 429–431. https://doi.org/10.1136/gut.33.4.429 (1992).
Nalin, D. R. et al. Cholera, non-vibrio cholera, and stomach acid. Lancet 2, 856–859. https://doi.org/10.1016/s0140-6736(78)91568-4 (1978).
Giannella, R. A., Broitman, S. A. & Zamcheck, N. Influence of gastric acidity on bacterial and parasitic enteric infections. A perspective. Ann. Intern. Med. 78, 271–276 (1973).
Sack, G. H. Jr. et al. Gastric acidity in cholera and noncholera diarrhoea. Bull. World Health Organ. 47, 31–36 (1972).
Schiraldi, O., Benvestito, V., Di Bari, C., Moschetta, R. & Pastore, G. Gastric abnormalities in cholera: epidemiological and clinical considerations. Bull. World Health Organ. 51, 349–352 (1974).
Gitelson, S. Gastrectomy, achlorhydria and cholera. Isr. J. Med. Sci. 7, 663–667 (1971).
Clemens, J. et al. Impact of infection by Helicobacter pylori on the risk and severity of endemic cholera. J. Infect. Dis. 171, 1653–1656 (1995).
Leon-Barua, R. et al. Helicobacter pylori-associated chronic atrophic gastritis involving the gastric body and severe disease by Vibrio cholerae. Trans. R. Soc. Trop. Med. Hyg. 100, 567–572. https://doi.org/10.1016/j.trstmh.2005.09.013 (2006).
Shahinian, M. L. et al. Helicobacter pylori and epidemic Vibrio cholerae O1 infection in Peru. Lancet 355, 377–378 (2000).
Bhan, M. K. et al. Association between Helicobacter pylori infection and increased risk of typhoid fever. J. Infect. Dis. 186, 1857–1860 (2002).
Vollaard, A. M. et al. Helicobacter pylori infection and typhoid fever in Jakarta, Indonesia. Epidemiol. Infect. 134, 163–170. https://doi.org/10.1017/S0950268805004875 (2006).
Mattsson, A., Lonroth, H., Quiding-Jarbrink, M. & Svennerholm, A. M. Induction of B cell responses in the stomach of Helicobacter pylori- infected subjects after oral cholera vaccination. J. Clin. Invest. 102, 51–56. https://doi.org/10.1172/JCI22 (1998).
Taye, B. et al. Association between infection with Helicobacter pylori and atopy in young Ethiopian children: A longitudinal study. Clin. Exp. Allergy. 47, 1299–1308. https://doi.org/10.1111/cea.12995 (2017).
Cohen, D., Shoham, O., Orr, N. & Muhsen, K. An inverse and independent association between Helicobacter pylori infection and the incidence of shigellosis and other diarrheal diseases. Clin. Infec. Dis. 54, e35-42. https://doi.org/10.1093/cid/cir916 (2012).
Rothenbacher, D., Blaser, M. J., Bode, G. & Brenner, H. Inverse relationship between gastric colonization of Helicobacter pylori and diarrheal illnesses in children: results of a population-based cross-sectional study. J. Infect. Dis. 182, 1446–1449. https://doi.org/10.1086/315887 (2000).
Harris, V. et al. Rotavirus vaccine response correlates with the infant gut microbiota composition in Pakistan. Gut Microbes. 9, 93–101. https://doi.org/10.1080/19490976.2017.1376162 (2018).
Harris, V. C. et al. Significant correlation between the infant gut microbiome and rotavirus vaccine response in rural Ghana. J. Infect. Dis. 215, 34–41. https://doi.org/10.1093/infdis/jiw518 (2017).
Harris, V. C. et al. Effect of antibiotic-mediated microbiome modulation on rotavirus vaccine immunogenicity: a human, randomized-control proof-of-Concept trial. Cell Host Microbe. 24, 197. https://doi.org/10.1016/j.chom.2018.07.005 (2018).
Hooi, J. K. Y. et al. Global prevalence of Helicobacter pylori infection: systematic review and meta-analysis. Gastroenterology 153, 420–429. https://doi.org/10.1053/j.gastro.2017.04.022 (2017).
Maiga, M. et al. Stool microbiome reveals diverse bacterial ureases as confounders of oral urea breath testing for Helicobacter pylori and Mycobacterium tuberculosis in Bamako. Mali. J. Breath Res. https://doi.org/10.1088/1752-7155/10/3/036012 (2016).
Acknowledgements
We are very thankful to Professor Guillermo I Perez-Perez and Professor Martin J Blaser from New York University School of Medicine, New York, NY, USA for providing the recombinant CagA antigen. We thank Ms. Gany Beer-Davidson (Tel Aviv University) for her technical assistance in performing the H. pylori serological assays.
Funding
This study was funded by the United States-Israel Binational Science Foundation (BSF) (PIs K.M. and M.M.L.) Grant No. 2015361.
Author information
Authors and Affiliations
Contributions
K.M., S.O.S., W.H.C., M.D.T., M.F.P. and M.M.L. made substantial contributions to the conception and design of the work, and directed its implementation. K.M. and M.M.L. acquired funding. S.O.S., W.H.C., M.D.T., F.C.H., M.R., V.A., M.F.P., K.M. and M.M.L. contributed substantially to acquisition of data, blood samples. K.M. and M.M.L. were responsible for data analysis. All authors made substantial contributions to interpretation of findings. K.M. and M.M.L. drafted the manuscript and all authors contributed to writing and substantive revisions. All authors approved the submitted version of the manuscript and agreed to be personally accountable for the author's own contributions and accuracy of data presented in the manuscript.
Corresponding author
Ethics declarations
Competing interests
Professor Levine is the co-inventor of CVD 103-HgR which is commercialized by Emergent Biosolutions, Gaithersburg, MD as Vaxchora. The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Muhsen, K., Sow, S.O., Tapia, M.D. et al. Pre-existing Helicobacter pylori serum IgG enhances the vibriocidal antibody response to CVD 103-HgR live oral cholera vaccine in Malian adults. Sci Rep 10, 16871 (2020). https://doi.org/10.1038/s41598-020-71754-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-71754-9
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.