Abstract
To describe the 5 years’ trajectories in functionality and pain of patients with hip or knee osteoarthritis and arthroplasty and analyze the association of these with long-term patients survival. Patients with OA receiving total hip or knee arthroplasty were recruited and completed two sets of standardized questionnaires for functionality and pain 6, 12, and 60 months postoperatively. Multivariate mixed models were conducted to assess trajectories over time and the resulting improvement per month during the last time period was included in a landmark-model to estimate adjusted hazard ratios for mortality. In total 809 patients with joint replacement were included (mean age 65.0 years, 62.2% female), 407 patients died (median follow-up 18.4 years). Both instruments of functionality and pain showed extensive improvement during the first 6 months. Baseline and change in functionality (both p < 0.001) and pain (p = 0.02) during the first 6 months were associated with mortality. Better values in functionality corresponded with improved survival whereas the association with the pain scores was inverse. In patients with hip and knee OA, an explicit improvement in function is seen within the first 6 months after arthroplasty. In addition, especially the functionality scores at baseline as well as their improvement showed an association with long-term patient survival.
Similar content being viewed by others
Introduction
Osteoarthritis (OA) is a very common musculoskeletal disorder. Prevalence of OA is increasing with age and OA leads to functional disability and pain in the joints1,2. Arthroplasty is an established treatment in symptomatic patients in order to restore functionality, relief pain, and increase overall quality of life. It prevents disability and also enables a renewed physically active lifestyle, which is an important component of health3.
Overall, patients with OA seem to have no increased all-cause mortality compared to the general population, also previous studies revealed inconsistent results4. A recent meta-analysis which investigated the association of symptomatic or radiological OA and all-cause mortality came to the conclusion that so far no reliable evidence exists for an association of OA with general and all-cause mortality5. We came to a similar conclusion when analyzing the 20 years’ mortality after the first hip or knee joint replacement in our study population6. However, as impaired function and chronic pain associated with OA may result in disability as well as in decreased physical activity, these patients may also have long-term consequences on a variety of health-related endpoints, and finally on long-term survival. However, studies that investigated the trajectories of functionality and pain after arthroplasty and the association with long-term health consequences are scarce yet. Additionally, the difference in association with long-term mortality between generic and osteoarthritis-specific instruments has not been investigated so far.
Therefore, the aim of this investigation was to describe the 5 years’ trajectories in functionality and pain of patients from the Ulm Osteoarthritis Study cohort, who underwent a hip or knee replacement due to osteoarthritis and were characterized with different measurement instruments of pain and functionality. The resulting trajectories have then been analyzed to investigate the association with long-term patient survival after adjustment for multiple covariates.
Methods
Study design and study population
For this prospective cohort study patients for unilateral total hip or knee arthroplasty due to advanced OA were recruited consecutively between January 1995 and December 1996 in four hospitals in the South-West of Germany. The inclusion criteria (i.e. white, age not exceeding 75 years, absence of malignancies, inflammatory diseases, or corticosteroid medication; no previous joint replacement) were fulfilled by N = 809 patients who also gave written informed consent. The initial study (details in7,8), as well as the current follow-up, was approved by the Ethics Committee of Ulm University (No. 164/14). The study was conducted according to the relevant guidelines and regulations and the Declaration of Helsinki.
Study data collection and classification
Among others, detailed information about comorbidities, symptoms, and medical history as well as demographic data, was gathered by standardized interviews. We characterized “secondary OA” by the following reasons: infection, avascular necrosis, and osteochondritis, hemorrhagic diathesis, traumatic events with radiologically and/or surgically confirmed structural joint lesions as well as sequelae of slipped femoral capital epiphysis and acetabular dysplasia in pelvic radiographs. An idiopathic origin of “primary OA” was assumed in the absence of these risk factors. Missing values in secondary OA were handled as separate category “unknown”. Serum cholesterol levels and serum uric acid levels were obtained9,10 in non-fasting serum-samples taken preoperatively by standard venipuncture.
Assessment of functionality and pain
Different assessments were applied for functionality and pain. To measure functionality, the Hannover Functionality Status Questionnaire (FFbH) and the functionality sub-scale of the Western Ontario and McMaster University Osteoarthritis Index (WOMAC) were applied. The basic version of FFbH (including 18 single questions regarding the last seven days) was used to assess general function. WOMAC (including 17 single questions) was used to specifically describe function in the operated joint at the time point of assessment.
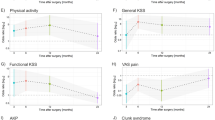
To measure pain, the Visual Analogue Scale (VAS) and the pain sub-scale of the WOMAC were applied. Both measures describe pain in the operated joint at the moment of assessment, the WOMAC pain sub-scale, however, concentrates on typical OA-associated circumstances. For comparability, each score was transformed onto a scale from 0 to 100 with higher values being positive for a patient (better functionality, less pain). The measurements of these instruments were applied at baseline as well as at 6 months, 12 months, and at 60 months. Missing values in assessments occurred due to loss to follow-up of patients or missed follow-up visits during the study course. The exact number of observations is displayed in Fig. 1A–D.
Trajectories of functionality (A,C) and pain (B,D) until the 60 months’ Follow-up. Shown values are means with standard errors. FFbH Hannover Functionality Status Questionnaire, VAS visual analogue scale, WOMAC Western Ontario and McMaster University Osteoarthritis Index, N number of pat. *Due to normalization, high scores equal less pain.
Assessment of mortality
Mortality was assessed during the follow-up time up to 20 years via residents' registration office. In case of death, the exact date of death was obtained from the respective residents' registration office. Information was gathered up until 31st August 2015. Further details can be found elsewhere6.
Statistical analysis
The main characteristics of the study population at baseline were described. The selection of characteristics included in these analyses was based on a previous investigation of the same dataset6. The selected characteristics were age, gender, diabetes, cholesterol, uric acid, heart insufficiency, hypertension, overweight, smoking status, localization of OA, and secondary OA as covariates for overall survival (details of variable selection see6).
Two different approaches were used to analyze both, a functionality value and a pain value in one statistical model. Approach 1 combined the FFbH functionality score with the VAS pain score. Approach 2 combined the two sub-scales for functionality and pain of the WOMAC. To assess the course of functionality and pain, the mean values of all assessments with corresponding standard errors were computed for baseline and follow-up time points. The resulting mean courses of all four assessments were plotted. Correlations between measured baseline values and trajectories (changes within specific time periods) were assessed by Pearson’s correlation coefficients for descriptive purposes.
The statistical analysis was conducted via a landmark Cox model combined with a prior, two-dimensional linear mixed effects model. We excluded observations with missing baseline measurements in pain or functionality for this analysis. The linear mixed effects model was used to estimate the partwise-linear trajectories of pain and functionality in the corresponding landmark dataset. The linear mixed effects model was calculated including no covariates other than time as predictor, using the breakpoints 6 and 12 months after follow-up. Then, the estimated current slopes as well as baseline functionality, pain and other baseline characteristics were included in the landmark Cox model11,12,13. Due to the follow-up times, landmark times were chosen to be 6, 12 and 60 months after follow-up and the previously described Cox model was calculated for each landmark time. For further information concerning the exact statistical methods see the Supplementary Material. Hazard ratios (HR) were estimated for the improvement in functionality or pain. The HRs with 95% confidence intervals (CI) and additional p values are shown for all 6 resulting sub-models (3 time points for 2 approaches). No adjustment for multiple testing was performed. All analyses were performed using SAS 9.4 (SAS Institute Inc., Cary, NC, USA).
Results
In the baseline investigation, 809 patients with OA were included; of these, 389 patients had arthroplasty of the knee, and 420 patients had arthroplasty of the hip, respectively. As displayed in Table 1 median age of patients with knee OA was 5 years older compared to patients with hip OA. Patients with knee OA also exhibited more comorbidities. In the subsets of patients with available assessments of functionality and pain, the described baseline characteristics were comparable to the population without missing values (data not shown). At the end of the 20 years’ follow-up (median observation time 18.4 years), N = 407 (50.3%) patients were deceased and n = 13 (1.6%) patients had been lost to follow-up.
Trajectories of functionality and pain
Score values over time of functionality (FFbH and WOMAC sub-scale functionality) and of pain (VAS and WOMAC sub-scale pain) are displayed in Fig. 1A–D stratified for localization of OA and gender. Patients started at relatively low levels of functionality and with high levels of pain at baseline. They experienced substantial improvements during the first 6 months after arthroplasty, in FFbH as well as in the VAS, and also in both WOMAC sub-scales. While looking at the differences between patients with knee OA and patients with hip OA one must keep in mind that knee-patients were older than hip patients. Further details are provided in Supplementary Table S1. Baseline values and trajectories of the FFbH and VAS-pain scale were only moderately correlated. In contrast, the WOMAC sub-scales were strongly correlated (Supplementary Table S2).
Functionality measured by FFbH was in general lower (i.e. worse functionality) in knee OA compared to hip OA and in females compared to males at baseline (Fig. 1, panel A). It increased substantially until month 6 and thereafter decreased until month 60. In general, patients with hip OA had higher functionality values (i.e. better functionality) than patients with knee OA, this was also the case for WOMAC functionality. Within gender, patients with hip OA had better values than knee OA during follow-up. VAS pain values showed an even stronger increase from point zero to 6 months’ follow-up, and patients with hip OA showed higher (less pain) values (Fig. 1, panel B). Patients with hip OA reached a higher plateau than patients with knee OA and showed no decrease after 12 months.
The WOMAC functionality sub-scale showed a strong increase up to month 6 and less steep to month 12, and was also reaching higher levels in patients with hip OA compared to knee OA (Fig. 1, panel C). Both sites and genders showed no further notable changes after month 12 until month 60. A similar pattern was found for the WOMAC pain sub-scale (Fig. 1, panel D).
Association of functionality and pain with survival-approach 1 (FFbH and VAS)
Higher values of FFbH and therefore better functionality at baseline were associated with lower overall mortality [HR at landmark 6 months 0.98 (95% CI 0.97–0.99) per point increase]. This association remained statistically significant also in landmark times 12 and 60 months (Table 2, upper panel). Even 60 months later better baseline FFbH values are still associated with lower subsequent mortality of patients [HR = 0.98 (95% CI 0.97–0.99)]. Additionally, the improvement in FFbH over the first six months was also associated with lower mortality (HR = 0.80, 95% CI 0.71–0.90). The HRs of the 12 months’ and 60 months’ landmark times tended into the same direction.
The VAS pain baseline values showed no association with mortality. However, more pronounced improvement in pain during the first 6 months was associated with increased mortality [HR = 1.06 (95% CI 1.01–1.12)].
Association of functionality and pain with survival-approach 2 (WOMAC sub-scales)
The analyses using the osteoarthritis-specific WOMAC sub-scales to quantify functionality and pain yielded no associations with overall mortality (Table 2, lower panel). Both baseline variables resulted in HR estimates whose 95% CIs included the null-effect value in all cases.
Discussion
In this cohort study of 809 patients with arthroplasty of hip or knee, we found a clear improvement in both functionality and pain after arthroplasty within the first 6 months which persisted, although less steep, until month 12. Better FFbH function scores at baseline, as well as improvement during the landmark times of 6, 12, and 60 months, were associated with improved survival during 20 years of follow-up. Notably, none of these associations with mortality were evident with the osteoarthritis specific WOMAC sub-scales pain and functionality primarily focusing on OA-specific aspects. Therefore trajectories of pain and function related to factors associated with general health aspects may be more important for long-term survival than joint-specific trajectories within a period of 1 year after arthroplasty.
Previous studies already showed an increase in functionality as well as a relief in pain after hip or knee arthroplasty with more pronounced effect in the hip14,15,16. A study by Lenguerrand et al. found that the main improvement in pain, as well as functionality, takes place in patients with hip and knee arthroplasty during the first three months after arthroplasty17, whereas no further changes were evident in the following nine months. Dowsey, Smith, and Choong tried to model the pain and functionality of patients with knee arthroplasty up to 5 years after operation18. Their measurements were taken once a year and showed an improvement during the first year in all subclasses (except patients with high pain scores) and approximately constant levels in later years. Our results are in line with the findings of these studies and expand them in several important respects.
Looking on specific factors Nüesch et al. reported that mortality in patients with hip or knee OA is linked to walking disability19. Hawker et al. confirmed this observation in patients with hip or knee OA who were followed over 13 years and reported an association of all-cause mortality with the WOMAC function sub-scale and walking disability but not with pain20. Interestingly, in the subgroup which received joint arthroplasty a reduced risk for cardiovascular events and improved patient survival was identified going in line with improved physical function. Joint arthroplasty also reduces chronic pain which may carry itself an increased risk for mortality. In a large cohort study from Denmark, patients with chronic pain had a 39% increased risk of death compared to the general population21. Management of peri- and postoperative pain is an important issue in patients with arthroplasty of the hip or knee. Several studies that investigated the effect of different strategies emphasized the importance of adequate pain management to prevent persistent postoperative pain15,22,23. Dumenci et al.24 estimated that among adults after knee arthroplasty about 18% had persistent pain, poor function, or both after 12 months. Interestingly, a recent review and meta-analysis suggested an overall modest risk of chronic pain in general with high heterogeneity between studies25. This variation was partly attributed to different pain phenotypes included. More recent studies on pain and mortality in adults above 50 years of age indicated that mainly pain which compromises daily life activities is associated with an increased risk of mortality26 and that functional limitation, as well as physical inactivity, may represent relevant mediators27.
Arthroplasty of hip or knee usually improved cardiovascular fitness in patients after hip arthroplasty investigated up to 2 years postoperatively28, an accepted predictor for all-cause mortality and cardiovascular events29. Interestingly, disability but not OA itself has recently been claimed to predict cardiovascular disease in a population-based cohort30.
However, currently there is no good evidence to support the association between joint replacement and increased physical activity. Patient self-reported physical activity seems neither accurate nor reproducible as assessed in a group of patients pre-operatively and 6–8 weeks post-operatively31. A study conducted with sensor-based measurements in 63 patients awaiting hip or knee arthroplasty from Australia showed no change to measurements 6 months later32, also 6 months measurements may still be influenced by post-operative pain and complications. In another study from Australia including 51 patients with total hip arthroplasty also no improvement in sensor-measured 24-h activity profiles at six months was seen33. A review including eight studies with patients with hip or knee arthroplasty and also sensor-based measurements showed negligible changes at 6 months follow-up, but larger changes at 12 months, which were especially evident for hip OA34. Still existing studies are based on relatively small numbers and partly suffer a high risk of bias. Therefore larger and better designed studies are still needed to make firm conclusions.
Our results indicate that long-term mortality of OA patients after joint replacement is more associated with the general health status, physical activity, and comorbidities than with joint-specific impairment35. Therefore, joint replacement should not be performed too late. Further investigations should look especially into the primary determinants and long-term consequences of different functional and pain trajectories especially visible in the first 6 months after OA. It seems plausible that the time shortly after OA is an important time slot for long-term prognosis, still with the possibility to eventually modifying treatment and rehabilitation efforts.
The study has the following strength: the study population with more than 800 patients with OA and arthroplasty of hip and knee was very well characterized at baseline and had a well-defined disease status. In addition, different measurements for functionality and pain were available during follow-up: on the one side a more general assessment of functionality by the FFbH score and of pain by the VAS, on the other side, an OA-specific assessment with the two WOMAC sub-scales.
The advanced landmark analyses used in this investigation extend standard landmark approaches due to the inclusion of a previous mixed model. By prior estimation of the trajectories, we were able to account for missing values occurring over the course of time as well as for a time-dependent bias (immortal time bias). A limitation of this technique is the disregard towards the joint distribution between survival process and trajectory36,37,38,39.
Another advantage is based on the design of landmarking itself. We were able to gain estimators, evaluating the association of the trajectory slopes at certain landmark times with survival. This is important because patients undergo greater changes during the first period after an arthroplasty. This period is therefore much more likely associated with survival than later ones. Another strength is that we were able to mutually adjust for functionality and pain. A limitation in our advanced approach arises due to the created linear dependencies between different estimations in our trajectory. Therefore, we cannot conclude with certainty, that the borderline significant results in a change of functionality included in the 12 months’ model for FFbH are due to an existing association or the dependency to the change at landmark time 6. A landmarking sensitivity analysis without mixed modeling did not find such an effect (results not shown). As an additional limitation, we did not have data from all patients for all the follow-up time points. In addition, we had a limited sample size especially in the subgroups and we were not able to assess the specific cause of death. Furthermore, it has to be considered that especially fitter patients may have benefitted more from arthroplasty and eventually survived longer.
Our final results suggest that in patients with hip and knee OA, arthroplasty leads to a clear improvement in both functionality measurements within the first 6 months, which seems to persist, although less steep, until month 12. The more pronounced improvement of the more generic VAS-pain score at the landmark time of 6 months showed an inverse association with long-term survival, pointing to a higher importance of general health status compared to joint-specific impairment for long-term patient survival.
Data availability
Due to ethical restrictions, the data cannot be made publicly accessible but are available upon reasonable request. The request should be directed to Prof. Rothenbacher (dietrich.rothenbacher@uni-ulm.de).
References
Cross, M. et al. The global burden of hip and knee osteoarthritis: Estimates from the global burden of disease 2010 study. Ann. Rheum. Dis. 73, 1323–1330 (2014).
van Dijk, G. M., Dekker, J., Veenhof, C., van den Ende, C. H. M. & Carpa Study Group. Course of functional status and pain in osteoarthritis of the hip or knee: A systematic review of the literature. Arthritis Rheum. 55, 779–785 (2006).
Piercy, K. L. et al. The physical activity guidelines for Americans. JAMA 320, 2020–2028 (2018).
Liu, R., Huizinga, T. W. & Kloppenburg, M. Mortality in osteoarthritis: A systematic review. Ann. Rheum. Dis. 72, A699 (2014).
Xing, D. et al. Osteoarthritis and all-cause mortality in worldwide populations: Grading the evidence from a meta-analysis. Sci. Rep. 6, 24393 (2016).
Büchele, G. et al. Osteoarthritis-patterns, cardio-metabolic risk factors and risk of all-cause mortality: 20 years follow-up in patients after hip or knee replacement. Sci. Rep. 8, 5253 (2018).
Günther, K. P. et al. Prevalence of generalised osteoarthritis in patients with advanced hip and knee osteoarthritis: The Ulm Osteoarthritis Study. Ann. Rheum. Dis. 57, 717–723 (1998).
Günther, K. P. et al. Incidence of joint-specific risk factors in patients with advanced cox- and gonarthroses in the Ulm Osteoarthrosis Study. Z. Orthop. Ihre Grenzgeb. 137, 468–473 (1999).
Stürmer, T. et al. Serum cholesterol and osteoarthritis. The baseline examination of the Ulm Osteoarthritis Study. J. Rheumatol. 25, 1827–1832 (1998).
Sun, Y. et al. Serum uric acid and patterns of radiographic osteoarthritis—the Ulm Osteoarthritis Study. Scand. J. Rheumatol. 29, 380–386 (2000).
Stürmer, T., Brenner, H., Koenig, W. & Günther, K.-P. Severity and extent of osteoarthritis and low grade systemic inflammation as assessed by high sensitivity C reactive protein. Ann. Rheum. Dis. 63, 200–205 (2004).
Statistisches Bundesamt (Destatis). https://www.destatis.de/DE/Startseite.html.
Houwelingen, H. C. V. Dynamic prediction by landmarking in event history analysis. Scand. J. Stat. 34, 70–85 (2007).
Jones, C. A., Voaklander, D. C., Johnston, D. W. & Suarez-Almazor, M. E. Health related quality of life outcomes after total hip and knee arthroplasties in a community based population. J. Rheumatol. 27, 1745–1752 (2000).
Grosu, I., Lavandhomme, P. M. & Thienpont, E. Pain after knee arthroplasty: An unresolved issue. Knee Surg. Sports Traumatol. Arthrosc. 22, 1744–1758 (2014).
Mandzuk, L. L., McMillan, D. E. & Bohm, E. R. A longitudinal study of quality of life and functional status in total hip and total knee replacement patients. Int. J. Orthop. Trauma Nurs. 19, 102–113 (2015).
Lenguerrand, E. et al. Trajectories of pain and function after primary hip and knee arthroplasty: The ADAPT cohort study. PLoS One 11, e0149306 (2016).
Dowsey, M. M., Smith, A. J. & Choong, P. F. M. Latent Class Growth Analysis predicts long term pain and function trajectories in total knee arthroplasty: A study of 689 patients. Osteoarthr. Cartil. 23, 2141–2149 (2015).
Nüesch, E. et al. All cause and disease specific mortality in patients with knee or hip osteoarthritis: Population based cohort study. BMJ 342, d1165 (2011).
Hawker, G. A. et al. All-cause mortality and serious cardiovascular events in people with hip and knee osteoarthritis: A population based cohort study. PLoS One 9, e91286 (2014).
Ekholm, O., Kurita, G. P., Højsted, J., Juel, K. & Sjøgren, P. Chronic pain, opioid prescriptions, and mortality in Denmark: A population-based cohort study. Pain 155, 2486–2490 (2014).
Lizaur-Utrilla, A., Gonzalez-Parreño, S., Miralles-Muñoz, F. A. & Lopez-Prats, F. A. Ten-year mortality risk predictors after primary total knee arthroplasty for osteoarthritis. Knee Surg. Sports Traumatol. Arthrosc 23, 1848–1855 (2015).
Baratta, J. L., Gandhi, K. & Viscusi, E. R. Perioperative pain management for total knee arthroplasty. J. Surg. Orthop. Adv. 23, 22–36 (2014).
Dumenci, L. et al. Model-based pain and function outcome trajectory types for patients undergoing knee arthroplasty: A secondary analysis from a randomized clinical trial. Osteoarthr. Cartil. 27, 878–884 (2019).
Smith, D., Wilkie, R., Uthman, O., Jordan, J. L. & McBeth, J. Chronic pain and mortality: A systematic review. PLoS One 9, e99048 (2014).
Smith, D., Wilkie, R., Croft, P. & McBeth, J. Pain and mortality in older adults: The influence of pain phenotype. Arthritis Care Res. 70, 236–243 (2018).
Smith, D., Wilkie, R., Croft, P., Parmar, S. & McBeth, J. Pain and mortality: Mechanisms for a relationship. Pain 159, 1112–1118 (2018).
Ries, M. D. et al. Effect of total hip arthroplasty on cardiovascular fitness. J. Arthroplasty 12, 84–90 (1997).
Kodama, S. et al. Cardiorespiratory fitness as a quantitative predictor of all-cause mortality and cardiovascular events in healthy men and women: A meta-analysis. JAMA 301, 2024–2035 (2009).
Hoeven, T. A. et al. Disability and not osteoarthritis predicts cardiovascular disease: A prospective population-based cohort study. Ann. Rheum. Dis. 74, 752–756 (2015).
Vaughn, N. H., Dunklebarger, M. F. & Mason, M. W. Individual patient-reported activity levels before and after joint arthroplasty are neither accurate nor reproducible. Clin. Orthop. 477, 536–544 (2019).
Harding, P., Holland, A. E., Delany, C. & Hinman, R. S. Do activity levels increase after total hip and knee arthroplasty?. Clin. Orthop. 472, 1502–1511 (2014).
Thewlis, D. et al. Objectively measured 24-hour activity profiles before and after total hip arthroplasty. Bone Jt. J. 101-B, 415–425 (2019).
Arnold, J. B., Walters, J. L. & Ferrar, K. E. Does physical activity increase after total hip or knee arthroplasty for osteoarthritis? A systematic review. J. Orthop. Sports Phys. Ther. 46, 431–442 (2016).
Bülow, E. et al. Comorbidity does not predict long-term mortality after total hip arthroplasty. Acta Orthop. 88, 472–477 (2017).
Rizopoulos, D., Molenberghs, G. & Lesaffre, E. M. E. H. Dynamic predictions with time-dependent covariates in survival analysis using joint modeling and landmarking. Biom. J. Biom. Z. 59, 1261–1276 (2017).
Suresh, K., Taylor, J. M. G., Spratt, D. E., Daignault, S. & Tsodikov, A. Comparison of joint modeling and landmarking for dynamic prediction under an illness-death model. Biom. J. Biom. Z. 59, 1277–1300 (2017).
Maziarz, M., Heagerty, P., Cai, T. & Zheng, Y. On longitudinal prediction with time-to-event outcome: Comparison of modeling options. Biometrics 73, 83–93 (2017).
Paige, E. et al. Landmark models for optimizing the use of repeated measurements of risk factors in electronic health records to predict future disease risk. Am. J. Epidemiol. 187, 1530–1538 (2018).
Acknowledgements
The study was supported by a grant from the German Federal Ministry for Research and Technology (BMFT No. 01 EF940/6). The 20-year follow-up was supported by the Deutsche Arthrosehilfe e.V.
Funding
Open Access funding provided by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
H.B., R.E.B., K.P.G., D.R., J.B., S.R., T.S., K.H.: designed research. S.R.: analyzed the data. S.R., G.B., D.R.: wrote the manuscript. All authors: reviewed the manuscript for intellectual contents.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Repky, S., Büchele, G., Günther, KP. et al. Five years’ trajectories of functionality and pain in patients after hip or knee replacement and association with long-term patient survival. Sci Rep 10, 14388 (2020). https://doi.org/10.1038/s41598-020-71277-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-71277-3
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.