Abstract
This study aims to assess the effects of a community-based lifestyle intervention program on the incidence of type 2 diabetes (T2D). For this purpose, three communities in Tehran were chosen; one community received a face-to-face educational session embedded in a long-term community-wide lifestyle intervention aimed at supporting lifestyle changes. We followed up 9,204 participants (control: 5,739, intervention: 3,465) triennially from 1999 to 2015 (Waves 1–5). After a median follow-up of 3.5 years (wave 2), the risk of T2D was 30% lower in the intervention community as compared with two control communities by (Hazard-ratio: 0.70 [95% CI 0.53; 0.91]); however, the difference was not statistically significant in the following waves. After a median follow-up of 11.9 years (wave 5), there was a non-significant 6% reduction in the incidence of T2D in the intervention group as compared to the control group (Hazard-ratio: 0.94 [0.81, 1.08]). Moreover, after 11.9 years of follow-up, the intervention significantly improved the diet quality measured by the Dietary Approaches to Stop Hypertension concordance (DASH) score. Mean difference in DASH score in the intervention group versus control group was 0.2 [95% CI 0.1; 0.3]. In conclusion, the intervention prevented T2D by 30% in the short-term (3.5 years) but not long-term; however, effects on improvement of the diet maintained in the long-term.
Registration: This study is registered at IRCT, a WHO primary registry (https://irct.ir). The registration date 39 is 2008-10-29 and the IRCT registration number is IRCT138705301058N1.
Similar content being viewed by others
Introduction
The burden of type 2 diabetes (T2D) is high and increasing in Low- and Middle-Income Countries (LMICs) like Iran1. Iranians have a high risk of developing T2D with an incidence rate of the disease being 11 per 1,000 person-years2. Given the high burden of T2D in Iran, there is an urgent need for effective prevention programs for T2D that can be implemented nationally.
Community-wide strategies are vital to have a major impact on trends in raising the T2D epidemic3,4,5. Several studies have assessed the effects of community-wide lifestyle interventions on the prevention of T2D. For this aim, community-wide interventions were delivered to a community living within a certain geographic area and their outcomes were compared with other similar communities in distinct geographic areas6,7,8. Previous community-wide lifestyle intervention studies showed a reduction in risk factors of T2D including significant beneficial effects on poor diet habits9,10,11,12,13, obesity9,14,15,16,17, low physical activity9,13,18, and smoking9,10,11,12,13,16,19,20,21,22,23,24,25,26,27,28. However, only a few of them assessed the effect of their program on the incidence of T2D14,29. Moreover, none of the previous studies evaluated the maintenance of the effects of community-wide lifestyle interventions after a decade. Most community-wide lifestyle intervention studies have been conducted in high-income countries and there are only a few studies from LMICs6,7,8. Therefore, there is a pressing need for robust evidence on the long-term effects of community-wide lifestyle interventions on the incidence of T2D and related risk factors, especially in LMICs where the burden of T2D is high and increasing1.
The Tehran Lipid and Glucose Study (TLGS) is a long-term community-based lifestyle intervention program aimed at preventing non-communicable diseases and their risk factors30. Previously, we showed that the lifestyle intervention in the TLGS reduced T2D incidence and its risk factors including obesity, dyslipidemia, and dysglycemia short-term (after 3 years)17. The current study evaluates the long-term effectiveness of the TLGS intervention on the incidence of T2D and its risk factors.
Methods
Study design and participants
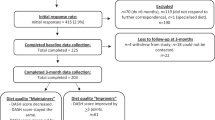
The TLGS was designed and implemented at two main junctures: (i) a cross-sectional study of the prevalence of NCDs and their risk factors implemented from 1999 to 200130 and (ii) a prospective follow-up study along with lifestyle interventions and triennial data recollection. The protocol of TLGS has been published previously30. Briefly, three areas in District 13 of Tehran were selected for the study. One district was assigned to receive lifestyle intervention, and two other communities, far from the intervention area, were allocated to the control group. Of the total population living in the three areas (total population: 27,551: intervention area: 10,761, control areas: 7,858 + 8,932), 10,368 individuals who aged ≥ 20 years provided informed consent. Of these individuals, 1,164 had T2D at baseline and were excluded. As a result, 9,204 eligible participants were left for this study (5,739 participants in the control group and 3,465 participants in the intervention group). We used information of all eligible participants in the primary analysis of this study after imputing the missing values. In the sensitivity analysis, however, of the 9,204 eligible participants for this study, we excluded 2,158 participants who were absent at follow-up (23%), 178 participants with missing status for T2D in their follow-ups (2%), and 910 participants with missing values for confounders and blood glucose at baseline (10%). Eventually, the data of the remaining 5,958 participants (3,906 participants in the control group and 2052 in the intervention group) were used in the sensitivity analysis.
Clinical and laboratory measurements
The details of clinical and laboratory measurements have been reported previously30. Briefly, all participants were examined at the TLGS Clinic between February 1999 and August 2001 (wave 1) and were followed up through four times: wave 2: Oct 2001–Sep 2005; wave 3: Apr 2005–Sep 2008; wave 4: Jul 2008–Oct 2011; and wave 5: Sep 2011–Jan 2015. In each wave, data on demographics, socioeconomic status, past medical history, physical activity, and smoking status were collected by completing a 110-item questionnaire. The Lipid Research Clinic (LRC) questionnaire in the baseline examination (wave 1) and the Modifiable Activity Questionnaire (MAQ) in waves 2–5 were used to assess the physical activity level30.
Dietary intake was collected using a validated 168-item food frequency questionnaire (FFQ)31,32 in waves 3–5. The FFQ was used to collect information on 17 food groups including whole grains, refined grains, dairy products, vegetables, fruits, legumes, meats, poultry, fish, nuts, seeds, dry beans, fat, oil, tea, coffee, salt, and simple sugars31,32. In our previous studies, we showed that the FFQ was reliable and valid for assessing the intake of different food groups in the TLGS population31,32. Furthermore, in another TLGS sub-study, dietary intake data of 578 randomly selected participants in the control group and the intervention group were collected at the baseline (wave 1) using the FFQ. The results showed that there was no difference between intervention and control group33.
Anthropometric and blood pressure measurements were taken according to standard protocols30. A blood sample was drawn after 12–14 h of overnight fasting to measure fasting plasma glucose (FPG), 2 h-postprandial plasma glucose (2 h-PG), high-density lipoprotein cholesterol (HDL-C), triglycerides, and total cholesterol. For the oral glucose tolerance test, 75 g anhydrous glucose was administered orally30. All the measurements were taken in both the intervention and control groups.
Definition of terms
Current smoking was ascertained in participants who smoked cigarettes at least once a day or those who smoked cigarettes occasionally. Low physical activity was defined as having less than 3 days of performing sports or heavy physical activity per week in wave 1 of study (based on the LRC questionnaire) and as having less than 600 metabolic equivalents of task (MET) per week in waves 2–5 (based on MAQ questionnaire)30.
The quality of participants’ diets was assessed according to Dietary Approaches to Stop Hypertension (DASH) dietary plan34. To this end, the cut-offs defined by the DASH diet concordance score (DASH score) was used34.
We discarded measurements collected after contamination. Contamination occurred if a participant assigned to the intervention group moved out from the intervention community or a participant assigned to the control group moved into the intervention community in one of the follow-up waves. A total of 267, 357, and 108 participants in the intervention group moved out from the intervention community in waves 3, 4, and 5, respectively. Also, 15, 11, and 11 participants in the control group moved into the intervention community in waves 3, 4, and 5, respectively. The data collected after contamination were discarded and the data before the contamination were used as the last available follow-up.
Outcomes
The primary outcome was the incidence of T2D. T2D was ascertained as FPG ≥ 7.0 mmol/L or 2 h-PG ≥ 11.1 mmol/L and/or taking glucose-lowering medication35. The event date was considered as the half-time between the first date that T2D was diagnosed and the last known disease-free date.
Secondary outcomes were the difference between the study groups in physical activity, smoking status, energy intake, quality of diet, body mass index (BMI), waist circumference (WC), FPG, 2 h-PG, triglycerides, High-Density Lipoproteins (HDL) cholesterol, and total cholesterol in the follow-up waves. The difference in change from baseline was also assessed for physical activity, smoking status, BMI, WC, FPG, 2 h-PG, triglycerides, HDL, and total cholesterol in the follow-up waves. The difference in change from baseline was not assessed for energy intake and quality of diet because these measurements were not collected at the baseline.
Description of lifestyle intervention
Details of the lifestyle intervention have been reported previously17,30,36,37,38; briefly, the lifestyle intervention design was adapted from the North Karelia project39,40 and using American Heart Association guidelines. For this purpose, findings of the need assessments and Knowledge, Attitude, and Practice (KAP) studies in the TLGS communities were also used41,42. The lifestyle intervention was performed to prevent non-communicable diseases and improve risk factors of the subject through improving diet, increasing physical activity, and encouraging smoking cessation. The interventions had three components: family-based, school-based, and community-wide interventions. On the other hand, the control group received routine health care.
Family-based lifestyle intervention
The families in the intervention area were invited to receive a single face-to-face lifestyle intervention educational session between waves 1 and 2 of the study (between 1999 and 2001). The session was initiated with individual consultation and a 2-h educational class in small groups. The session included structured advice about lifestyle changes related to improving dietary patterns, increasing physical activity, and smoking cessation using slide and video presentations. All smokers were invited to take part in a motivational consult and then referred to a cessation clinic.
Residents from the intervention community received health newsletters named “Courier of Health” every three months (between 2001 and 2011). The newsletters contained information about health topics including the food pyramid guide, weight management, health hazards of smoking, smoking-cessation techniques, the importance of daily walking, and regular physical activity, and specific exercise recommendations. Moreover, they contained summarized findings of the TLGS, including the prevalence of risk factors in their community. Pamphlets and booklets on specific topics related to lifestyle management were also distributed 2–4 times per year among the residents of the intervention community. TLGS staff collected information on how many families read the pamphlets and booklets in each wave through telephone surveys. Telephone surveys showed that 50% of households had received and paid attention to the educational pamphlets and health newsletters37.
Community-wide intervention
Participants in the intervention area were also encouraged to participate in public education in 2–4 community gatherings annually for 1.5 to 3 h between 2001 and 2011. The gatherings included social events, seminars, and religious ceremonies, particularly at mosques in the holy month of Ramadan. Public events on occasions such as World Tobacco Day and World Diabetes Day were also held. Community health projects such as sports competitions, developing sports facilities in the community, providing subsidies for local gyms and pools, and health promotion advertisements (billboards) were also established in the intervention community between 2001 and 2011. More than 80% of the households participated in at least one of public gatherings for national or religious holidays between every two examinations38.
School-based intervention
A total of 12 schools across the intervention community implemented an ongoing school-based intervention that directly targeted students, parents, teachers, staff, and the school environment36. Briefly, since 2001, a total of 12 healthy lifestyle sessions (45 min each) were held for the 1st-grade students, followed with three sessions for students of grades 2 and 3, in each school year. Sessions included educational courses for students including “living tobacco-free” classes. The intervention also included forming the school’s “health team” by students with the aim of peer education38 and labelling snacks sold at the school’s shop regarding their healthiness.
For parents, three educational sessions (60 min each) were conducted for each grade in addition to a group discussion each year36. For teachers, 2-day seminars and 45-min class focusing on the knowledge and skills regarding healthy behaviours were held annually36. Moreover, smoking was prohibited for all the schoolchildren, teachers, and employees inside the school.
Statistical analysis
Baseline characteristics were summarized using mean (± SD) values for continuous and frequencies (%) for categorical variables in the control and intervention groups. Since triglycerides had a skewed distribution, it was summarized by the median (interquartile range).
Cox proportional hazard models were fitted to compare the incidence rate of the T2D in the study groups accounting for baseline value of potential confounders (i.e., age, sex, area of residence, education level, family history of diabetes, smoking, low physical activity, WC, BMI, systolic blood pressure, diastolic blood pressure, FPG, 2 h-PG, total cholesterol, triglycerides, and HDL-C, and self-reported drug consumption for hypertension, and dyslipidemia) and clustered nature of data for families (i.e., using robust standard errors). Also, the effect of the intervention in each wave was estimated by restricting the Cox proportional hazard models to the data collected until that particular wave. For example, to estimate the effect of the intervention until the end of wave 3, we only used the data collected from waves 1–3 and discarded the data collected in waves 4 and 5.
To compare the risk factor levels between the study groups in different waves, generalized estimating equations (GEE) were fitted in a long-form dataset including data from waves 2–543. In each model, the level of risk factor was defined as the outcome and the predictors were defined to be baseline level of risk factor, time-point variable (i.e., waves 2–5), interventions status (control and intervention), an interaction term between intervention status and time-point variable, and potential confounders (i.e., age, sex, area of residence, education level, family history of diabetes, smoking, low physical activity, WC, BMI, systolic blood pressure, diastolic blood pressure, FPG, 2 h-PG, total cholesterol, triglycerides, and HDL-C, and self-reported drug consumption for hypertension, and dyslipidemia). The model also accounted for the clustered nature of data due to repeated measures using an auto-regressive correlation matrix (the autoregressive process of order 1). An autoregressive correlation matrix was chosen since measurements taken further apart were less correlated than those taken closer together44. Logit link function for binary outcomes and identity link function for continuous outcomes were used in the GEE models.
To compare the change from baseline for the risk factor levels between the study groups in different waves, GEE models with similar link functions (as described above) and autoregressive correlation matrix were fitted in a long-form dataset including data from waves 1–543. In each model, the level of risk factor was defined as the outcome and the predictors were defined to be time-point variable (i.e., waves 1–5), intervention status (control and intervention), the interaction term between intervention status and time-point variable, and potential confounders (as listed above). The estimated coefficient for interaction terms between intervention status and time-point variable were used to compare study groups in change in risk factor levels from baseline to different waves of study43.
In the primary analysis for primary outcome (incidence of T2D), we imputed the baseline missing values of BMI (n = 230), WC (n = 269), family history of T2D (n = 394), low-physical activity (n = 163), education level (n = 10), smoking status (n = 158), systolic/diastolic blood pressure (n = 209), FPG (n = 299), 2 h-PG (n = 880), total cholesterol (n = 297), triglycerides (n = 300), HDL (n = 307)m T2D status at the end of follow-up (n = 2,270), and time-to-event (n = 2,305). Ice package in Stata was used to produce 10 imputed datasets using linear regression models for imputing continuous variables, logistic regression for binary variables, and ordinal regression models for ordinal variables45,46,47. We imputed the time-to-event variable as described in ice package documentations and previous studies45,46,47. To analyze the secondary outcomes, we also imputed data of risk factors in follow-up waves (waves 2–5) using similar methods45,46,47. For each analysis, estimates from imputed datasets were combined using Rubin’s rule45,46,47. In the complete-case analysis, similar models were fitted in those with complete data (n = 5,958).
To account for multiple comparisons in the secondary aim of the study, the corrected p-value threshold was calculated and reported using the Bonferroni48 formula. Estimates with p-values less than Bonferroni threshold were considered as statistically significant. Analyses were performed using the Stata statistical software (version 14 SE).
Research ethics
The ethics committee of the Research Institute for Endocrine Sciences, Shahid Beheshti University of Medical Sciences confirmed the design of the TLGS study. Methods were carried out following the relevant guidelines and regulations. All participants provided written informed consent.
Results
Of 9,204 included participants, 5,285 ones were female (57.4%) with mean (± SD) age and BMI of 41.1 ± 14.52 years and 26.5 ± 4.7 kg/m2, respectively (Table 1). As compared to participants in the intervention group, participants in the control group had significantly higher physical activity (25% vs. 22%), education, smoking prevalence (14% vs. 11%), and FPG (4.99 vs. 4.96 mmol/L) and lower WC (86.8 vs. 87.4 cm) at baseline (Table 1).
After a median follow-up of 3.5 years (IQR 2.7–4.2) (wave 2), 4.5% (95% CI 3.7%; 5.2%) of participants in the control group and 3.8% (95% CI 3.1%; 4.5%) participants in the intervention group developed T2D. It resulted in incidence rates of 14.4 and 9.2 per 1,000 person-years in the control and the intervention groups, respectively. The hazard of incident T2D was significantly 30% lower in the intervention group compared to the control group (IRR 0.70 [0.53; 0.91], p-value: 0.009). This difference, however, disappeared in the following waves (Table 2). After a median follow-up of 11.9 years (IQR 6.6–13.3) (wave 5), 14.1% (95% CI 13.2%; 15.1%) of participants in the control group and 11.1% (95% CI 10.1%; 12.6%) of participants in the intervention group were diagnosed with T2D with an incidence rate of 12.9 and 11.9 per 1,000 person-years in the control and intervention groups, respectively. There was a non-significant 6% reduction in the incidence rate of T2D in the intervention group compared to the control group [Hazard ratio: 0.94 (0.81, 1.08)]. Findings from complete case analyses were similar to those from the primary analysis (Table 2).
Table 3 compares the change in the lifestyle risk factors of T2D. Based on the Bonferroni method, the corrected p-value threshold was 0.00058 for the secondary aim of the study. Adjusting for the differences between study groups at baseline, at wave 2 of TLGS, the intervention group indicates a significantly lower FPG (by 0.1 mmol/L; p-value < 0.0001) and a significantly higher HDL (by 0.03 mmol/L; p-value < 0.0001). Similar findings were observed when comparing the changes from baseline to wave 2 for each risk factor. In the final wave (wave 5), the intervention group had significantly higher levels of DASH score (0.2; p-value < 0.0001). Generally, similar results were observed in complete case analysis (data not shown).
Discussion
This research is one of the few studies reporting the long-term effects of a community-wide lifestyle intervention on T2D prevention in an LMIC. Although the intervention reduced the risk of T2D by 30% short-term (wave 2: 3.5 years of follow-up), this effect was not maintained until the end of the study (wave 5) with a non-significant 6% reduction in the risk of T2D after 11.9 years of follow-up. Nevertheless, the effect of lifestyle intervention on the improvement of diet quality maintained after 11.9 years.
Our findings are in line with those of a recent study in the TLGS that showed that lifestyle intervention prevented metabolic syndrome short-term (waves 2 and 3). However, this effect was not maintained in the long run (wave 4 and wave 5)37. Moreover, our recent study in the adolescent participants of the TLGS, showed that the lifestyle intervention prevented metabolic syndrome in a short time (wave 2) but not in long-term (wave 4)36. There is limited evidence about the long-term effects of a community-wide lifestyle intervention program on the incidence of T2D or the prevalence of its risk factors. Repeated surveys in the Isfahan Healthy Heart Program, a multi-component community-wide lifestyle intervention, showed a non-significant (0.8%) reduction in the prevalence of T2D in the intervention group compared to the controls after 7 years of follow-up29. Similarly, studies conducted in high-income countries showed no significant reduction in the incidence of T2D in the long-term14,49,50. Regarding changes in the risk factors of T2D, several studies showed that the community-wide lifestyle intervention programs had significant long-term effects on the reduction of T2D risk factors6,7,8,51. In a community-wide lifestyle intervention in the Coalfields district of New South Wales, Australia52, a significant reduction in poor dietary habits and BMI was observed after 10 years of follow-up.
Our research demonstrates that a low-cost and pragmatic intervention consisting of a face-to-face educational session embedded in a community-wide intervention can reduce the incidence of T2D short-term and improve the quality of diet in the long-term. Therefore, if scaled up, this program can prevent a considerable number of new cases of T2D as well as other non-communicable diseases in Iran. However, we also showed that the intervention was not effective in the long term. Underscoring this issue needs more attention to ensure lifestyle intervention effectiveness in the long-term. There is limited evidence regarding the factors contributing to the maintenance of long-term success of community-wide lifestyle intervention programs especially beyond a period of 24 months53. Previous studies suggested that the lack of maintenance in the effects of lifestyle interventions may be due to the inability of participants in maintaining healthy eating and exercise behaviours over time53,54 and long-term maintenance may increase by removing the barriers in lifestyle modification55. Based on previous studies56,57,58,59,60,61, the most important barriers to healthy nutrition and physical activity were interpersonal/cultural effects, lack of access to healthy foods, food preferences, media advertisements, nutrition transition, lack of time, motivation, and prioritizing other activities over sports and high costs of the facilities. Moreover, a booster face-to-face educational session every 3 years might help maintain the effectiveness of the lifestyle intervention for a longer period.
This study has several strengths including a large sample size and more than a decade-long follow-up. Moreover, the team and the methods for data collection had minimal changes throughout the study. This is one of the few community trials that has collected and compared the dietary patterns in detail between study groups. The findings of this study, however, should be interpreted in light of several limitations of which, such as the non-randomized design of the study. As another limitation, 35% of participants had at least one missing value in their variables of interest. Moreover, TLGS did not collect data on T2D knowledge. An increase in T2D knowledge is one of the main goals of community-wide lifestyle intervention programs for T2D prevention as it can result in the gradual development of healthy beliefs/attitudes and a meaningful change in behaviour. Lack of T2D knowledge data averted further investigations on potential causes for lack of long-term effectiveness. For example, T2D knowledge data could have helped distinguish whether the lack of long-term effectiveness is mainly due to external and internal barriers that prevent participants to apply their knowledge in practice or it was mainly due to a decrease in T2D knowledge of TLGS participants.
In conclusion, the lifestyle intervention reduced the risk of T2D by 30% after 3.5 years of follow-up (wave 2 of study), a change that was not maintained in the following waves with a non-significant 6% reduction in T2D risk after 11.9 years of follow-up. Nevertheless, the effect of lifestyle intervention on the quality of diet maintained even after 11.9 years of follow-up.
Data availability
Data are available upon request.
References
1International Diabetes Federation. (2017).
Harati, H., Hadaegh, F., Saadat, N. & Azizi, F. Population-based incidence of Type 2 diabetes and its associated risk factors: results from a six-year cohort study in Iran. BMC Public Health 9, 186. https://doi.org/10.1186/1471-2458-9-186 (2009).
Shaw, J. E. Prediabetes: lifestyle, pharmacotherapy or regulation?. Ther. Adv. Endocrinol. Metab. 10, 2042018819863020. https://doi.org/10.1177/2042018819863020 (2019).
Shaw, J. E. & Chisholm, D. J. 1: epidemiology and prevention of type 2 diabetes and the metabolic syndrome. Med. J. Aust. 179, 379–383. https://doi.org/10.5694/j.1326-5377.2003.tb05599.x (2003).
Albright, A. L. & Gregg, E. W. Preventing type 2 diabetes in communities across the U.S.: the National Diabetes Prevention Program. Am. J. Prev. Med. 44, S346-351. https://doi.org/10.1016/j.amepre.2012.12.009 (2013).
Satterfield, D. W. et al. Community-based lifestyle interventions to prevent type 2 diabetes. Diabetes Care 26, 2643–2652. https://doi.org/10.2337/diacare.26.9.2643 (2003).
Pennant, M. et al. Community programs for the prevention of cardiovascular disease: a systematic review. Am. J. Epidemiol. 172, 501–516. https://doi.org/10.1093/aje/kwq171 (2010).
Sellers, D. E., Crawford, S. L., Bullock, K. & McKinlay, J. B. Understanding the variability in the effectiveness of community heart health programs: a meta-analysis. Soc. Sci. Med. 44, 1325–1339. https://doi.org/10.1016/s0277-9536(96)00263-8 (1997).
Lupton, B. S., Fonnebo, V., Sogaard, A. J. & Langfeldt, E. The Finnmark intervention study. Better health for the fishery population in an Arctic village in North Norway. Scand. J. Prim. Health Care 20, 213–218. https://doi.org/10.1080/028134302321004863 (2002).
Baxter, T. et al. A cost effective, community based heart health promotion project in England: prospective comparative study. BMJ 315, 582–585. https://doi.org/10.1136/bmj.315.7108.582 (1997).
Kottke, T. E. et al. CardioVision 2020: program acceptance and progress after 4 years. Am. J. Prev. Med. 30, 137–143. https://doi.org/10.1016/j.amepre.2005.10.017 (2006).
Sarrafzadegan, N. et al. Do lifestyle interventions work in developing countries? Findings from the Isfahan Healthy Heart Program in the Islamic Republic of Iran. Bull. World Health Organ 87, 39–50. https://doi.org/10.2471/blt.07.049841 (2009).
Huang, S. et al. The positive effect of an intervention program on the hypertension knowledge and lifestyles of rural residents over the age of 35 years in an area of China. Hypertens. Res. 34, 503–508. https://doi.org/10.1038/hr.2010.265 (2011).
Schuit, A. J. et al. Effect of 5-year community intervention Hartslag Limburg on cardiovascular risk factors. Am. J. Prev. Med. 30, 237–242. https://doi.org/10.1016/j.amepre.2005.10.020 (2006).
Domenighetti, G., Casabianca, A., Wietlisbach, V. & Gutzwiller, F. Prevention of cardiovascular diseases is effective Initial program evaluation of the canton Tessin (1984–1989). Hygie 11, 24–31 (1992).
Rossouw, J. E. et al. Community-based intervention: the Coronary Risk Factor Study (CORIS). Int. J. Epidemiol. 22, 428–438. https://doi.org/10.1093/ije/22.3.428 (1993).
Harati, H. et al. Reduction in incidence of type 2 diabetes by lifestyle intervention in a middle eastern community. Am. J. Prev. Med. 38, 628–636. https://doi.org/10.1016/j.amepre.2010.03.003 (2010).
Brownson, R. C. et al. Preventing cardiovascular disease through community-based risk reduction: the Bootheel Heart Health Project. Am. J. Public Health 86, 206–213. https://doi.org/10.2105/ajph.86.2.206 (1996).
Goodman, R. M., Wheeler, F. C. & Lee, P. R. Evaluation of the Heart To Heart Project: lessons from a community-based chronic disease prevention project. Am. J. Health Promot. 9, 443–455. https://doi.org/10.4278/0890-1171-9.6.443 (1995).
Nafziger, A. N., Erb, T. A., Jenkins, P. L., Lewis, C. & Pearson, T. A. The Otsego-Schoharie healthy heart program: prevention of cardiovascular disease in the rural US. Scand. J. Public Health Suppl 56, 21–32. https://doi.org/10.1177/14034948010290021501 (2001).
Hoffmeister, H. et al. Reduction of coronary heart disease risk factors in the German cardiovascular prevention study. Prev. Med. 25, 135–145. https://doi.org/10.1006/pmed.1996.0039 (1996).
Egger, G. et al. Results of large scale media antismoking campaign in Australia: North Coast “Quit for Life” programme. Br. Med. J. (Clin. Res. Ed.) 287, 1125–1128. https://doi.org/10.1136/bmj.287.6399.1125 (1983).
Puska, P. et al. Change in risk factors for coronary heart disease during 10 years of a community intervention programme (North Karelia project). Br. Med. J. (Clin. Res. Ed.) 287, 1840–1844. https://doi.org/10.1136/bmj.287.6408.1840 (1983).
Gutzwiller, F., Nater, B. & Martin, J. Community-based primary prevention of cardiovascular disease in Switzerland: methods and results of the National Research Program (NRP 1A). Prev. Med. 14, 482–491. https://doi.org/10.1016/0091-7435(85)90008-8 (1985).
Winkleby, M. A., Taylor, C. B., Jatulis, D. & Fortmann, S. P. The long-term effects of a cardiovascular disease prevention trial: the Stanford Five-City Project. Am. J. Public Health 86, 1773–1779. https://doi.org/10.2105/ajph.86.12.1773 (1996).
Farquhar, J. W. et al. Community education for cardiovascular health. Lancet 1, 1192–1195. https://doi.org/10.1016/s0140-6736(77)92727-1 (1977).
Chen, J., Wu, X. & Gu, D. Hypertension and cardiovascular diseases intervention in the capital steel and iron company and Beijing Fangshan community. Obes. Rev. 9(Suppl 1), 142–145. https://doi.org/10.1111/j.1467-789X.2007.00456.x (2008).
Huot, I., Paradis, G., Ledoux, M. & Quebec Heart Health Demonstration Project Research Group. Effects of the Quebec Heart Health Demonstration Project on adult dietary behaviours. Prev. Med. 38, 137–148. https://doi.org/10.1016/j.ypmed.2003.09.019 (2004).
Khosravi, A. et al. The impact of a 6-year comprehensive community trial on the awareness, treatment and control rates of hypertension in Iran: experiences from the Isfahan healthy heart program. BMC Cardiovasc. Disord. 10, 61. https://doi.org/10.1186/1471-2261-10-61 (2010).
Azizi, F. et al. Prevention of non-communicable disease in a population in nutrition transition: Tehran Lipid and Glucose Study phase II. Trials 10, 5. https://doi.org/10.1186/1745-6215-10-5 (2009).
Asghari, G. et al. Reliability, comparative validity and stability of dietary patterns derived from an FFQ in the Tehran Lipid and Glucose Study. Br. J. Nutr. 108, 1109–1117. https://doi.org/10.1017/S0007114511006313 (2012).
Esfahani, F. H., Asghari, G., Mirmiran, P. & Azizi, F. Reproducibility and relative validity of food group intake in a food frequency questionnaire developed for the Tehran Lipid and Glucose Study. J. Epidemiol. 20, 150–158. https://doi.org/10.2188/jea.je20090083 (2010).
Mirmiran, P., Ramezankhani, A., Hekmatdoost, A. & Azizi, F. Effect of nutrition intervention on non-communicable disease risk factors among Tehranian adults: Tehran Lipid and Glucose Study. Ann. Nutr. Metab. 52, 91–95. https://doi.org/10.1159/000121364 (2008).
Campbell, A. P. DASH eating plan: an eating pattern for diabetes management. Diabetes Spectr. 30, 76–81. https://doi.org/10.2337/ds16-0084 (2017).
Gavin, J. R. III., Alberti, K. G. M. M., Davidson, M. B. & DeFronzo, R. A. Report of the expert committee on the diagnosis and classification of diabetes mellitus. Diabetes Care 20, 1183–1197. https://doi.org/10.2337/diacare.20.7.1183 (1997).
Amiri, P. et al. The effects of a community-based lifestyle intervention on metabolic syndrome and its components in adolescents: findings of a decade follow-up. Metab. Syndr. Relat. Disord. 16, 215–223. https://doi.org/10.1089/met.2017.0055 (2018).
Khalili, D. et al. Long-term effectiveness of a lifestyle intervention: a pragmatic community trial to prevent metabolic syndrome. Am. J. Prev. Med. 56, 437–446. https://doi.org/10.1016/j.amepre.2018.10.029 (2019).
Khalili, D. et al. Outcomes of a longitudinal population-based cohort study and pragmatic community trial: findings from 20 years of the tehran lipid and glucose study. Int. J. Endocrinol. Metab. 16, e84748. https://doi.org/10.5812/ijem.84748 (2018).
McAlister, A., Puska, P., Salonen, J. T., Tuomilehto, J. & Koskela, K. Theory and action for health promotion illustrations from the North Karelia Project. Am. J. Public Health 72, 43–50. https://doi.org/10.2105/ajph.72.1.43 (1982).
Puska, P., Vartiainen, E., Nissinen, A., Laatikainen, T. & Jousilahti, P. Background, principles, implementation, and general experiences of the North Karelia Project. Glob Heart 11, 173–178. https://doi.org/10.1016/j.gheart.2016.04.010 (2016).
Mirmiran, P. et al. Nutritional knowledge, attitude and practice of Tehranian adults and their relation to serum lipid and lipoproteins: Tehran lipid and glucose study. Ann. Nutr. Metab. 56, 233–240. https://doi.org/10.1159/000288313 (2010).
Mirmiran, P., Azadbakht, L. & Azizi, F. Dietary behaviour of Tehranian adolescents does not accord with their nutritional knowledge. Public Health Nutr. 10, 897–901. https://doi.org/10.1017/S1368980007246701 (2007).
Achy-Brou, A. C., Frangakis, C. E. & Griswold, M. Estimating treatment effects of longitudinal designs using regression models on propensity scores. Biometrics 66, 824–833. https://doi.org/10.1111/j.1541-0420.2009.01334.x (2010).
Zeger, S. L., Liang, K. Y. & Albert, P. S. Models for longitudinal data: a generalized estimating equation approach. Biometrics https://doi.org/10.2307/2531734 (1988).
Royston, P. An informal tutorial on the ice command for chained equations imputation in Stata. (Stata Users Group, 2007).
Royston, P. Multiple imputation of missing values: further update of ice, with an emphasis on categorical variables. Stat J. 9, 466–477 (2009).
Royston, P. & White, I. R. Multiple imputation by chained equations (MICE): implementation in Stata. Stat. J. 45, 1–20 (2011).
Bland, J. M. & Altman, D. G. Multiple significance tests: the Bonferroni method. BMJ 310, 170. https://doi.org/10.1136/bmj.310.6973.170 (1995).
Daniel, M. et al. Effectiveness of community-directed diabetes prevention and control in a rural Aboriginal population in British Columbia, Canada. Soc. Sci. Med. 48, 815–832. https://doi.org/10.1016/s0277-9536(98)00403-1 (1999).
Rowley, K. G. et al. Reduced prevalence of impaired glucose tolerance and no change in prevalence of diabetes despite increasing BMI among Aboriginal people from a group of remote homeland communities. Diabetes Care 23, 898–904. https://doi.org/10.2337/diacare.23.7.898 (2000).
van de Vijver, S., Oti, S., Addo, J., de Graft-Aikins, A. & Agyemang, C. Review of community-based interventions for prevention of cardiovascular diseases in low- and middle-income countries. Ethnic Health 17, 651–676. https://doi.org/10.1080/13557858.2012.754409 (2012).
Higginbotham, N., Heading, G., McElduff, P., Dobson, A. & Heller, R. Reducing coronary heart disease in the Australian Coalfields: evaluation of a 10-year community intervention. Soc. Sci. Med. 48, 683–692. https://doi.org/10.1016/s0277-9536(98)00384-0 (1999).
Dombrowski, S. U., Knittle, K., Avenell, A., Araujo-Soares, V. & Sniehotta, F. F. Long term maintenance of weight loss with non-surgical interventions in obese adults: systematic review and meta-analyses of randomised controlled trials. BMJ 348, g2646. https://doi.org/10.1136/bmj.g2646 (2014).
Wing, R. R. & Phelan, S. Long-term weight loss maintenance. Am. J. Clin. Nutr. 82, 222S-225S. https://doi.org/10.1093/ajcn/82.1.222S (2005).
Yu, E., Malik, V. S. & Hu, F. B. Cardiovascular disease prevention by diet modification: JACC health promotion series. J. Am. Coll. Cardiol. 72, 914–926. https://doi.org/10.1016/j.jacc.2018.02.085 (2018).
Abedini Sedigheh, S., Morowatisharifabad Mohammadali, M., Enjezab Behnaz, B., Fallahzade Hosin, H. & Barkhordari Abolfazl, A. Perceived barriers to physical activity among nurses in Bandar Abbas, Iran: A qualitative approach. Schol. J. Educ. (2014).
Enjezab, B., Farajzadegan, Z., Taleghani, F. & Aflatoonian, A. Internal motivations and barriers effective on the healthy lifestyle of middle-aged women: a qualitative approach. Iran J. Nurs. Midwifery Res. 17, 390–398 (2012).
Momenan, A. A., Delshad, M., Mirmiran, P., Ghanbarian, A. & Azizi, F. Leisure time physical activity and its determinants among adults in Tehran: Tehran Lipid and Glucose Study. Int. J. Prev. Med. 2, 243–251 (2011).
Kelishadi, R. et al. Barriers to physical activity in a population-based sample of children and adolescents in Isfahan, Iran. Int. J. Prev. Med. 1, 131–137 (2010).
Farahmand, M. et al. What are the main barriers to healthy eating among families? A qualitative exploration of perceptions and experiences of Tehranian men. Appetite 89, 291–297. https://doi.org/10.1016/j.appet.2015.02.025 (2015).
Farahmand, M., Tehrani, F. R., Amiri, P. & Azizi, F. Barriers to healthy nutrition: perceptions and experiences of Iranian women. BMC Public Health 12, 1064. https://doi.org/10.1186/1471-2458-12-1064 (2012).
Funding
The Tehran Lipid and Glucose Study (TLGS) was supported by the National Research Council of the Islamic Republic of Iran [grant numbers 121]. The current study was conducted within the framework of the TLGS, despite not receiving any specific funding source.
Author information
Authors and Affiliations
Contributions
M.L., D.K., and F.H.: study conception and design; F.A., F.H., and D.K.: acquisition of the data; M.L.: writing the first draft; M.L., M.A.M., and D.K.: analysis and interpretation of data; M.L., M.A.M., F.A., F.H., N.Z., A.G., P.M., B.O., and D.K.: critical revision; M.A.M., F.A., B.O., D.K., and F.H.: supervision. All authors have approved the final article.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lotfaliany, M., Mansournia, M.A., Azizi, F. et al. Long-term effectiveness of a lifestyle intervention on the prevention of type 2 diabetes in a middle-income country. Sci Rep 10, 14173 (2020). https://doi.org/10.1038/s41598-020-71119-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-71119-2
This article is cited by
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.