Abstract
While food insecurity is a persistent public health challenge, its long-term association with depression at a national level is unknown. We investigated the spatial heterogeneity of food insecurity and its association with depression in South Africa (SA), using nationally-representative panel data from the South African National Income Dynamics Study (years 2008–2015). Geographical clusters (“hotpots”) of food insecurity were identified using Kulldorff spatial scan statistic in SaTScan. Regression models were fitted to assess association between residing in food insecure hotspot communities and depression. Surprisingly, we found food insecurity hotspots (p < 0.001) in high-suitability agricultural crop and livestock production areas with reliable rainfall and fertile soils. At baseline (N = 15,630), we found greater likelihood of depression in individuals residing in food insecure hotspot communities [adjusted relative risk (aRR) = 1.13, 95% CI:1.01–1.27] using a generalized linear regression model. When the panel analysis was limited to 8,801 participants who were depression free at baseline, residing in a food insecure hotspot community was significantly associated with higher subsequent incidence of depression (aRR = 1.11, 95% CI:1.01–1.22) using a generalized estimating equation regression model. The association persisted even after controlling for multiple socioeconomic factors and household food insecurity. We identified spatial heterogeneity of food insecurity at a national scale in SA, with a demonstrated greater risk of incident depression in hotspots. More importantly, our finding points to the “Food Security Paradox”, food insecurity in areas with high food-producing potential. There is a need for place-based policy interventions that target communities vulnerable to food insecurity, to reduce the burden of depression.
Similar content being viewed by others
Introduction
Despite two decades of political advancement since liberation from the apartheid regime and the advent of democracy in 1994, South Africa continues to face intractable poverty1, income inequality2, and unemployment3, that results in many citizens struggling to meet their basic household needs. Consistent with recent global trends4, there has also been a disconcerting decline in South African food security, a concept defined internationally as having enough food at all times for an active, healthy life5. Since 2011, there has been a growing number of individuals living below the food poverty line (25.2% in 2015 versus 21.4% in 20111), where approximately a quarter of households are exposed to food insecurity in South Africa (which ranged from 21.5% to 23.9% between the years 2010–20156).
Depression, our study outcome of this current investigation, is also a serious health condition that affects 9.8% of South Africans in their lifetime7. As a leading cause of disability globally8, depression is understood to have the highest negative impact on productivity among all medical conditions9,10. Evidence based on financial modelling strongly underpins the assertion that untreated depression can be considered both a health and development challenge for many low- and middle-income countries11. In South Africa, workplace-related economic loss from depression is estimated to be 4.9% of gross domestic product (GDP)12, a major impediment to economic development for a developing nation, which is further compounded by an additional GDP loss of 5% due to high rates of malnutrition13.
Food insecurity and depression are dual public health challenges that are often closely linked. Several systematic reviews confirm a link between food insecurity and mental health14,15, with likely mechanisms including both biological processes related to nutritional deficiencies and the psychological stress of having insufficient food16,17,18. Consumption of several nutrients, including vitamin B12 and antioxidants, appear important to prevent depression19,20. As a self-reported construct, food insecurity at household- or individual-level also encapsulates an important psychological aspect (i.e. anxiety about restricted food supplies) that is central to the experience of living with food insecurity21.
Achieving food security, as part of the United Nation’s Sustainable Development Goal (SDG) 2.122, and in terms of Section 27(1)(b) of the South African constitution23, as well as preventing depression onset (SDG 3.424), remain monumental challenges in the light of budgetary limitations to address multiple development priorities. This dilemma warrants targeted strategies to first identify food-vulnerable geographical locations, so as to inform prioritized interventions for the most affected areas (which may have mental health implications, yet to be examined). With some exceptions from Nigeria25 and Ethiopia26, there are few recent national-level studies from sub-Saharan African (SSA) countries27 on the spatial variability of household food insecurity. In this current study, we will use of novel spatial statistical methods to first identify geographical clusters (“hotpots”) of food insecurity, and assess its association with depression, based on panel data from the South African National Income Dynamics Study (SA-NIDS), a unique nationally-representative sample of South Africans, with geographical coordinates for each household. As alluded to previously, the association between food insecurity and depression is well-established at the individual-level28,29,30. Second, we aimed to identify risk of depression onset between individuals living in/outside food insecure hotspot communities over and above the individual effect of household-level food insecurity.
Methods
Data from the South African National Income Dynamics Study (SA-NIDS) wave 1 (year 2008), wave 2 (2010), wave 3 (2012), and wave 4 (2015) were utilized. As the first panel survey of a nationally representative sample of households in South Africa, the SA-NIDS provides unique insights into population trends in living conditions and well-being that is rarely observed in SSA. The SA-NIDS employs a stratified, two-stage cluster sample design to attain a nationally representative sample of households. In the first stage, 400 of the 3,000 Primary Sampling Units (PSUs) from Statistics South Africa’s Master Sample were selected for inclusion and proportionally allocated, based on the 53 district councils in South Africa. In the second stage, clusters of dwelling units were systematically drawn within each PSU, with two clusters of 12 dwelling units being selected from each. All consenting adult resident household members (≥ age 15) at the selected dwelling units were administered the SA-NIDS questionnaire, its details being described in a published methodological report31. For study participants between the ages of 15 and 17, the SA-NIDS obtained written informed consent from a parent and or legal guardian. In minor cases where there were no parents or legal guardians, written informed consent was obtained from caregivers, consistent with South African National Department of Health Guidelines for ethics in health research32.
Our study constructed an incident cohort based on similar methods utilized in previous studies33,34, to better isolate the effect of exposure to food insecurity (i.e. residing in food insecurity hotspot communities) at baseline on subsequent depression onset; thus, reducing the likelihood of reverse causation. The purpose of constructing the incident cohort was to ensure that the observed study participants were free of depression initially; and then to track the risk of depression onset over time between individuals exposed and unexposed to food insecurity. Household food insecurity information was only available for wave 1 (baseline) in the SA-NIDS. Therefore, the incident cohort of our current study consisted of wave 1 participants who screened negative for depression in wave 1 (baseline) and for whom there was a further depression rating score available in any of waves 2–4 (thus participants who screened positive for depression in wave 1 were excluded). We right censored the data, either at the earliest observation at which a participant subsequently screened positive, or at the last observation if the participant did not subsequently screen positive for depression. The SA-NIDS study, approved by the Ethics Committee of the University of Cape Town, obtained written informed consent for all study participants. Our use of SA-NIDS data was approved by the University of KwaZulu-Natal Biomedical Research Ethics Committee (BE 111/14).
Measures
Depression
Depression was the main study outcome. Information on depression, based on the ten-item abridged version of the Center for Epidemiologic Studies Depression Scale (CES-D), were obtained from the SA-NIDS Adult questionnaire. The CES-D is a commonly-used psychometric valid/reliable instrument35,36 that captures self-reported depression-associated symptoms during the past week. Each of the items has four possible responses in a Likert format, ranging from 0 = rarely/none of the time (less than 1 day) to 3 = almost/all of the time (5–7 days). Depression symptomatology is based on a composite score of the 10 items (Cronbach’s α = 0.75), with a total score of ≥ 10 being classified as a cutoff to signify significant depressive symptoms, consistent with a previous study37. Importantly, in this study we use this cutoff to define ‘depression’ as a presentation characterized by significant depressive symptomatology, although this cannot be considered equivalent to a clinical diagnosis of major depressive disorder.
Household food insecurity
The information on household food insecurity was obtained from wave 1 (2008) of the SA-NIDS Household questionnaire and captured the adequacy of household food needs over the last month. The measure was based on a three-point Likert scale on the adequacy of the food needs, ranging from 1 = less than adequate for household’s needs, to 3 = more than adequate. We generated a final household food insecurity measure (where food adequate/more than adequate = 0 and less than adequate = 1) to be used for the regression analysis (and for generating geographical clustering described immediately below).
Geographical clusters (“hotpots”) of food insecurity
Geographical clusters (“hotpots”) of food insecurity were identified using Kulldorff spatial scan statistic38 implemented in SaTScan software39,40. The space permutation model was utilized to identify spatial clusters of households with food insecurity, which were unlikely to have arisen by chance, by testing whether they were significantly adjacent in space. The scan statistical analysis imposed a circular window with varying radii continuously for each global positioning system (GPS) coordinate of the SA-NIDs households located throughout South Africa. The analysis identified a number of distinct potential clusters of affected households with the statistical significance of each being tested using a likelihood ratio test. After a food insecurity hotspot was identified (p < 0.05), its strength within compared with outside the hotspot was estimated using relative risk (RR). Individuals were subsequently either classified as exposed to a food insecurity hotspot (i.e. residing in a household located within a hotspot) or unexposed to a food insecurity hotspot (i.e. residing in a household located outside the hotspots). The SA-NIDS household GPS coordinates were accessed (with permission) from the DataFirst’s Secure Data Centre at the University of Cape Town.
Statistical analysis
First, a descriptive analysis of the sociodemographic details of the incident cohort was conducted. Second, geographical clusters of food insecurity (i.e. hotspots) were identified (based on the method described above) and the socio-demographic correlates of these ‘hotspot populations’ assessed. Socio-demographic disparities between the hotspot exposed and unexposed were tested using the second-order correction method for survey design41 and subsequently converted into F statistics. Third, we investigated the baseline association between residing in food insecure hotspot communities and the likelihood of depression by fitting a generalized linear model42 (GLM) based on the prevalence cohort (labelled Model 1). The prevalence cohort, as opposed to incident cohort, included all adults (i.e. 15,630 adults) regardless of depression status at baseline. This analysis was conducted to supplement the results from the above-mentioned second analysis, and to quantify the ‘immediate effect’ of residing in food insecurity hotspot on depression at baseline. Lastly, for the primary focus of our study, we investigated the long-term risk of depression onset due to exposure to hotspots over time based on the incident cohort who were depression-free at baseline. For this final analysis, given the repeated measurements of the SA-NID data structure, we fitted two generalized estimating equation43 (GEE) regression models. The first (labelled Model 2a) is a model based on variables included in Model 1. The second (labelled Model 2b) is our full model with household food insecurity variable nested within Model 2a. The significance of the nested model that added household food insecurity was tested using Wald test. All regression models were adjusted for sociodemographic variables (e.g. gender, race, age, educational attainment, employment status, income, and urban/rural). Given the nature of the complex survey design in the SA-NIDS, all the analyses involving proportion and regressions were adjusted by post-stratification weight to allow our results to better represent the South African population. The construction of post-stratification weight by SA-NIDS is documented in the published report44. All methods were performed in accordance with the relevant guidelines and regulations.
Results
Sociodemographic characteristics
Our incident cohort consisted of 8,801 participants who were depression-free at baseline (i.e. year 2008), with the socio-demographic characteristics (Table 1) of the incident cohort indicating that 55.3% (n = 5,169) were female, most were Black African (n = 6,771; 78.6%), and were unemployed (n = 5,300; 56.8%). The largest under-35-age group was 15 to 19 (n = 1,886; 19.9%). The prevalence of food insecurity among the incident cohort was 35.1% (n = 3,284). The number of depression cases among the incident cohort (i.e. depression free at baseline) during the subsequent waves 2–4 were 2,008, 1,330 and 659, respectively.
Geographical clusters of food insecurity community and its association with baseline depression
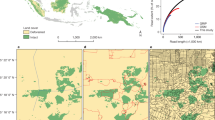
Spatio-temporal scan statistics analysis identified three significant clusters of food insecurity (p < 0.05) in South Africa (Fig. 1 and Table 2). There were two clusters in KwaZulu-Natal (KZN) Province and one overlapping both KZN and Eastern Cape. Relative risk of food insecurity within these clusters ranged from 1.34 to 2.21. Among 1,279 individuals residing in food insecure hotspot communities [hereafter refer to as hotspot or hotspot community], 844 reported food insecurity (64.8%). This is in stark contrast to only 2,440 (32.7%) among 7,503 individuals residing outside hotspots reporting food insecurity (F(1, 1,061) = 54.86, p < 0.01). The significant socio-demographic correlates of residing within a hotspot included: race, being young, having low educational attainment/income, being unemployed, and residing within a rural area (Table 3). We found significantly greater likelihood of depression in individuals residing in hotspot communities [adjusted relative risk (aRR) = 1.13, 95% CI:1.01–1.27] at baseline (Table 4 Model 1) after adjusting for sociodemographic variables, namely gender, race, age, educational attainment, employment status, income, and urban/rural.
Food insecurity hotspot map of South Africa. Information regarding each cluster number are described in Table 2. Spatial clustering of food insecurity was derived from the SA-NIDS household GPS coordinates accessed (with permission) from the DataFirst’s Secure Data Centre using SaTScan. The map was created using ArcGIS software by Esri version 10.3.
Geographical clusters of food insecurity community and its association on incident depression
The results of the adjusted regression analysis (Table 4 Model 2a) indicated that residing in a hotspot community was significantly associated with higher subsequent incidence of depression (aRR = 1.15, 95% CI: 1.05–1.26). Lastly, the results based on the full model (Table 4 Model 2b) indicated that residing in a hotspot community was significantly associated with higher subsequent incidence of depression (aRR = 1.11, 95% CI: 1.01–1.22). The association persisted even after controlling for multiple socioeconomic factors such as household income (aRR = 0.68, 95% CI: 0.57–0.81) and household food insecurity (aRR = 1.13, 95% CI: 1.03–1.23) under the full model. The addition of household food insecurity to Model 2b was significant using the Wald test (χ = 7.26, df = 1, p < 0.01), suggesting the depression is likely to be caused by household food insecurity and/or residing in a food insecure hotspot community.
Discussion
Our study investigated the spatial heterogeneity of food insecurity, and its association with incident depression in South Africa, and yielded two significant findings. First, we found a significantly greater incident depression for those residing in a hotspot that had high levels of food insecurity over and above the individual effect of household food insecurity based on incident cohort. This finding points to the likelihood that depression can be associated with either household food insecurity or residing in hotspot communities or both. Second, we found significant differences in the study participant profile, pointing to social vulnerabilities (e.g.[low] household income, employment, and educational attainment) of individuals residing in food insecure hotspot communities. While alleviating depression is often assumed to require psychotherapeutic and pharmacotherapeutic approaches45 in low-resource setting, addressing the underlying social causes (e.g. poverty and hunger in the community) may well be called for. Our findings highlight the need to go beyond biomedical approach, and address broader social determinants of depression in many under-resourced communities in South Africa.
To the best of our knowledge, this is the first study in South Africa that has identified the spatial variability of food insecurity at a national scale, with greater risk of incident depression among individuals residing in food insecure hotspot communities. Our findings on the spatial patterns of “hotpots” provide evidence supporting the “Food Security Paradox”; i.e. food insecurity in areas with a high food producing potential46. This paradox poses nuanced challenges in devising place-based policy interventions tailored to vulnerable communities. South Africa in general, being regarded as a food secure nation with the means to produce enough staple foods for all individuals47, is nonetheless plagued with widespread chronic household food insecurity; this “Food Security Paradox” phenomenon being particularly evident in KwaZulu-Natal Province (KZN) and its border area with the Eastern Cape Province. KZN’s fertile soils are suitable for commercial and small-scale/subsistence farming, being the best-watered province48 and home to many large agri-business firms49. The province has the country’s highest proportion of agricultural households (23.0%)50, with the hotspot communities being located within municipalities with the highest percentage of subsistence-based livelihoods (South African census51).
In the 1970s, viewing hunger as a social rather than a technical problem, Moore and colleagues in Food first: Beyond the myth of scarcity52, documented how the Sahel zone of North Africa exported food to Europe/North America and wealthy African clientele, the amount exceeding that of provided by international food relief in the midst of the famine. The “Food Security Paradox” is also a South African legacy, with apartheid policies replacing adequate and self-sufficient subsistence farming systems with commercial farming, where black South Africans were labor pools, reliant on cash from employment as a basis for attaining food security47.
Weaver and Hadley suggest three pathways from food insecurity to mental health problems such as depression namely: nutritional deficiencies with neurobiological consequences; stress generated by “uncertainty in the household ecology”; and perhaps most pertinent to the current South African context, the negative psychological consequences of relative social comparisons of wellbeing within and between communities14. Food has significant social functions53, and food insecurity may “amplify or magnify relative differences in wellbeing”, being a “particularly honest signal” of relative wealth/income and wellbeing14, both between households within and between different communities. There is substantial evidence showing the negative mental health effects of social comparisons in relation to household income inequality54. In the context of contemporary South Africa, a country characterised by one of the highest indexes of income inequality globally, households and communities experiencing relative food insecurity (in comparison with their neighbouring households and communities) are likely to experience feelings of inadequacy, shame and ‘social defeat’—all highly correlated with depressive symptoms and disorders in particular54.
The question remains regarding what equity policies can address food insecurity that is also closely linked to improved mental health outcomes for socioeconomically vulnerable populations. While market-based policies for improving food security are necessary, there is also a case to be made for well-planned government policies and interventions, particularly when food security is viewed as a public good55. Access to food is also a right guaranteed under Section 27(1)(b) of the Constitution of the Republic of South Africa23. There is also a case for reducing negative market externality, given that agriculture was the major driver of habitat loss in KZN56. Several government options are worth noting57, as they have cross-cutting food security and human well-being implications, such as mental health. Acknowledging that it is plausible that government interventions may give rise to unintended consequences that threaten food security, it is also important to explore the provision and restoration of land/property rights of (previously) disenfranchised individuals for subsistence farming. This seems obvious if ending hunger is to be achieved through the production of sufficient and nutritious amounts of food where it is most needed, and not just through social protection mechanisms such as cash transfers/social grants. Currently, the focus of the South African government policy is not on supporting subsistence farmers, but on transitioning them to semi-commercial farming58. A land/property rights-based approach to food security may be less dependent on market forces that determine agricultural commodity and individual purchasing power; and may relate more to the restoration of dignity and psychological liberation [given that black South Africans were forcibly removed from their ancestral (fertile) land for whites as part of the Natives Land Act #27 of 191359]. While the discussion of implementation choices in the provision and restoration of land/property rights, with or without compensation, is outside the purview of this current study, it is important to contextualize this research within the socioeconomic and political debate around food, land, and social justice in contemporary South Africa. Finally, we urge prioritized interventions focused on food security and its mental health impacts for individuals residing in hotspot communities in South Africa, and in particular throughout KwaZulu-Natal province and its bordering area with the Eastern Cape. These are the communities that the data suggest are most affected by the “Food Security Paradox” and, therefore, most in need of comprehensive and integrated interventions that deal, not only with food insecurity per se, but also the consequent negative impacts on human wellbeing, as well as the human rights of dignity and equality.
The major limitation of this investigation is the lack of clinical data that would allow for a diagnosis of depressive disorder; and we have therefore utilized a measure of significant depressive symptomatology as a ‘depression’ outcome. Second, food insecurity status was based on self-report, with limited longitudinal measures. Although we assumed the spatial-temporality of food insecure hotspots, we argued, as indicated in the Introduction section, that household food insecurity, although high, remains consistent over time. Notwithstanding these limitations, for the first time, we identified spatial variability of food insecurity at a national scale, with greater risk of incident depression among individuals residing in food insecure hotspot communities, linked directly to a decline in human wellbeing detectable at the population level. The strength of our investigation rests on spatially analyzing GPS data to identify food insecurity patterns, and linking this to the onset of depression at a national-scale; this, to our knowledge, not having been reported previously in studies from SSA. Furthermore, by constructing an incident cohort, we are better able to establish directionality and a causal path from exposure to food insecurity hotspot communities to onset of depression.
Our study highlights cross-cutting SDGs challenges (i.e. 2.1 and 3.4) and comes at a critical juncture when South Africa is grappling with highly contentious land reform issues to address chronic racial inequality60 – an issue that is further complicated by climate change61. As we acknowledge the important role of food insecurity in mental health outcomes, hunger in the community is also an emotional and ‘distributive justice’ social issue that is linked to the basic human dignity of South Africans previously dispossessed of their land. Addressing symptoms or manifested mental health challenges will require recognition of this deep-rooted (economic) land injustice that undermined human dignity. Our study underscores the need for place-based policy and prioritized interventions that target communities vulnerable to food insecurity to prevent depression and its associated damaging impact on social development in South Africa.
References
Statistics South Africa. Poverty trends in South Africa: An examination of absolute poverty between 2006 and 2015. https://www.statssa.gov.za/publications/report-03-10-06/report-03-10-062015.pdf (2017).
World Bank. Overcoming poverty and inequality in South Africa: An assessment of drivers, constraints and opportunities. https://documents.worldbank.org/curated/en/530481521735906534/pdf/124521-rev-ouo-south-africa-poverty-and-inequality-assessment-report-2018-final-web.pdf (2018).
Statistics South Africa. Quarterly Labour Force Survey Quarter 3: 2018. https://www.statssa.gov.za/publications/p0211/p02113rdquarter2018.pdf (2018).
United Nations. The Sustainable Development Goals Report 2018. https://unstats.un.org/sdgs/files/report/2018/thesustainabledevelopmentgoalsreport2018-en.pdf (2018).
World Bank. Poverty and Hunger: Issues and Options for Food Security in Developing Countries. (World Bank, Washington DC, 1986).
Statistics South Africa. General household survey 2016. https://www.statssa.gov.za/publications/report-03-10-06/report-03-10-062015.pdf (2017).
Herman, A. A. et al. The South African Stress and Health (SASH) study: 12-month and lifetime prevalence of common mental disorders. S. Afr. Med. J.99, 339–344 (2009).
Murray, C. J. L. et al. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet380, 2197–2223 (2012).
Burton, W. N., Pransky, G., Conti, D. J., Chen, C. Y. & Edington, D. W. The association of medical conditions and presenteeism. J. Occup. Environ. Med.46, S38-45 (2004).
Henderson, M., Harvey, S. B., Overland, S., Mykletun, A. & Hotopf, M. Work and common psychiatric disorders. J. R. Soc. Med.104, 198–207 (2011).
Chisholm, D. et al. Scaling-up treatment of depression and anxiety: A global return on investment analysis. Lancet. Psychiatry3, 415–424 (2016).
Evans-Lacko, S. & Knapp, M. Global patterns of workplace productivity for people with depression: Absenteeism and presenteeism costs across eight diverse countries. Soc. Psychiatry Psychiatr. Epidemiol.51, 1525–1537 (2016).
Food and Agriculture Organization of the United Nations. The state of food and agriculture 2013: Food systems for better nutrition. https://www.fao.org/docrep/018/i3300e/i3300e.pdf (2013).
Weaver, L. J. & Hadley, C. Moving beyond hunger and nutrition: A systematic review of the evidence linking food insecurity and mental health in developing countries. Ecol. Food Nutr.48, 263–284 (2009).
Jones, A. D. Food insecurity and mental health status: A global analysis of 149 countries. Am. J. Prev. Med.53, 264–273 (2017).
Firth, J. et al. Nutritional deficiencies and clinical correlates in first-episode psychosis: A systematic review and meta-analysis. Schizophr. Bull.44, 1275–1292 (2017).
Firth, J. et al. The effects of vitamin and mineral supplementation on symptoms of schizophrenia: A systematic review and meta-analysis. Psychol. Med.47, 1515–1527 (2017).
Li, Y. et al. Dietary patterns and depression risk: A meta-analysis. Psychiatry Res.253, 373–382 (2017).
Coppen, A. & Bolander-Gouaille, C. Treatment of depression: Time to consider folic acid and vitamin B12. J. Psychopharmacol.19, 59–65 (2005).
Liu, X., Yan, Y., Li, F. & Zhang, D. Fruit and vegetable consumption and the risk of depression: A meta-analysis. Nutrition32, 296–302 (2016).
Campbell, C. C. Food Insecurity: A Nutritional outcome or a predictor variable?. J. Nutr.121, 408–415 (1991).
United Nations. Goal 2: Zero Hunger. https://www.un.org/sustainabledevelopment/hunger/ (2019).
Republic of South Africa. Constitution of the Republic of South Africa. https://www.justice.gov.za/legislation/constitution/saconstitution-web-eng.pdf (1996).
World Health Organization. GOAL 3. Target 3.4. https://iris.wpro.who.int/bitstream/handle/10665.1/12876/sdg_poster_goal3_3.4_eng.pdf (2018).
Tolulope, T. A., Olubukola, O. B. & Olukemi, S. F. Spatial pattern of household food insecurity and childhood malnutrition in Akinyele local government area, Nigeria. Int. J. Health Sci.3, 235–250 (2015).
Alemu, Z. A., Ahmed, A. A., Yalew, A. W. & Simanie, B. Spatial variations of household food insecurity in East Gojjam Zone, Amhara Region, Ethiopia: Implications for agroecosystem-based interventions. Agric. Food Secur.6, 36 (2017).
Liu, J. et al. A spatially explicit assessment of current and future hotspots of hunger in Sub-Saharan Africa in the context of global change. Glob. Planet Change64, 222–235 (2008).
Hadley, C. et al. Food insecurity, stressful life events and symptoms of anxiety and depression in east Africa: Evidence from the Gilgel Gibe growth and development study. J. Epidemiol. Commun. Health62, 980 (2008).
Tomita, A. et al. Major depression and household food insecurity among individuals with multidrug-resistant tuberculosis (MDR-TB) in South Africa. Soc. Psychiatry Psychiatr. Epidemiol.54, 387–393 (2019).
Maharaj, V., Tomita, A., Thela, L., Mhlongo, M. & Burns, J. K. Food insecurity and risk of depression among refugees and immigrants in South Africa. J. Immigr. Minor Health19, 631–637 (2017).
Leibbrandt, M., Woolard, I. & de Villiers, L. Methodology: Report on NIDS Wave 1 (University of Cape Town, Cape Town, 2009).
South African National Department of Health. Ethics in health research principles, processes and structures (2015).
Tomita, A. et al. Green environment and incident depression in South Africa: A geospatial analysis and mental health implications in a resource-limited setting. Lancet Planet Health1, e152–e162 (2017).
Tomita, A. & Manuel, J. I. Evidence on the association between cigarette smoking and incident depression from the South African national income dynamics study 2008–2015: Mental health implications for a resource-limited setting. Nicotine Tob. Res. (2018).
Bjorgvinsson, T., Kertz, S. J., Bigda-Peyton, J. S., McCoy, K. L. & Aderka, I. M. Psychometric properties of the CES-D-10 in a psychiatric sample. Assessment20, 429–436 (2013).
Cole, J. C., Rabin, A. S., Smith, T. L. & Kaufman, A. S. Development and validation of a Rasch-derived CES-D short form. Psychol. Assess.16, 360–372 (2004).
Andresen, E. M., Malmgren, J. A., Carter, W. B. & Patrick, D. L. Screening for depression in well older adults: Evaluation of a short form of the CES-D (Center for Epidemiologic Studies Depression Scale). Am. J. Prev. Med.10, 77–84 (1994).
Kulldorff, M. A spatial scan statistic. Commun. Stat. Theory Methods26, 1481–1496 (1997).
Kulldorff, M., Heffernan, R., Hartman, J., Assuncao, R. & Mostashari, F. A space-time permutation scan statistic for disease outbreak detection. PLoS Med.2, e59 (2005).
Kulldorff, M. SaTScan v9.0: Software for the Spatial and Space-Time Statistics. (National Cancer Institute, 2010).
Rao, J. N. K. & Scott, A. J. On Chi-squared tests for multiway contingency tables with cell proportions estimated from survey data. Ann. Stat.12, 46–60 (1984).
McCullagh, P. & Nelder, J. A. Generalized Linear Models 2nd edn. (Chapman & Hall/CRC, London, 1989).
Zeger, S. L., Liang, K. Y. & Albert, P. S. Models for longitudinal data: A generalized estimating equation approach. Biometrics44, 1049–1060 (1988).
Wittenberg, M. Weights: Report on NIDS Wave 1. (University of Cape Town, 2009).
Thase, M. E. et al. Treatment of major depression with psychotherapy or psychotherapy-pharmacotherapy combinations. Arch. Gen. Psychiatry54, 1009–1015 (1997).
Wall, R.S., Maseland, J., Rochel, L.K., & Spaliviero, M. The State of African Cities 2018: The Geography of African Investment. United Nations Human Settlements Programme.
Hwenha, S. The South African food security paradox: Lessons and opportunities for CSI. First Rand. https://www.firstrand.co.za/csi/research/the%20south%20african%20food%20security%20paradox%20-%20lessons%20and%20opportunities%20for%20csi.pdf (2014).
South African Weather Service. Historical rain maps. https://www.weathersa.co.za/climate/historical-rain-maps
Deloitte. KZN agri outlook 2016: The KZN agri-industry building value chains into Africa. https://www2.deloitte.com/content/dam/deloitte/za/documents/process-and-operations/za_kzn%20agri%20outlook_2016.pdf (2016).
Statistics South Africa. Community Survey 2016 Agricultural Households. https://www.statssa.gov.za/publications/03-01-05/03-01-052016.pdf (2016).
Statistics South Africa. Presentation on Community Survey 2016 Agricultural Households. https://www.statssa.gov.za/publications/03-01-05/Presentation_CS2016_Agricultural_Households.pdf (2016).
Lappé, F.M., Collins, J. & Fowler, C. Food First: Beyond the Myth of Scarcity. (Ballantine Books, 1979).
Mintz, S., & Du Bois, C.M. The anthropology of food and eating. Annu. Rev. Anthropol.31, 99–119 (2002).
Patel, V. et al. Income inequality and depression: A systematic review and meta-analysis of the association and a scoping review of mechanisms. World Psychiatry17, 76–89 (2018).
Rocha, C. Food insecurity as market failure: A contribution from economics. J. Hunger Environ. Nutr.1, 5–22 (2007).
Jewitt, D., Goodman, P. S., Erasmus, B. F. N., O’Connor, T. G. & Witkowski, E. T. F. Systematic land-cover change in KwaZulu-Natal, South Africa: Implications for biodiversity. S. Afr. J. Sci.111, 01–09 (2015).
Landell-Mills, N. & Porras, I.T. Silver bullet or fools’ gold? A global review of markets for forest environmental services and their impact on the poor. International Institute for Environment and Development. https://pubs.iied.org/pdfs/9066IIED.pdf (2002).
Mabhaudhi, T. et al. Mainstreaming underutilized indigenous and traditional crops into food systems: A South African perspective. Sustainability11, 172 (2018).
Union of South Africa. Natives Land Act, Act No 27 of 1913. https://www.disa.ukzn.ac.za/sites/default/files/pdf_files/leg19130619.028.020.027.pdf (1913).
Dlamini, S. & Ogunnubi, O. Land reform in South Africa: Contending issues. J. Public Admin.53, 339–360 (2018).
Masipa, T. S. The impact of climate change on food security in South Africa: Current realities and challenges ahead. Jamba9, a411 (2017).
Statistics South Africa. Concept and definitions. https://www.statssa.gov.za/census/census_2001/concepts_definitions/concepts_definitions.doc (2004).
Brown, K. Coloured and black relations in South Africa: The burden of racialized hierarchy. Macalester Int.9, 13 (2000).
Acknowledgements
Our study utilized data from SA-NIDS. Waves 1-4 Data: Southern Africa Labour and Development Research Unit. National Income Dynamics Study 2008–2015, Cape Town: Southern Africa Labour and Development Research Unit [producer], 2016. Cape Town: DataFirst [distributor], 2016. Pretoria: Department of Planning Monitoring and Evaluation [commissioner], 2014. We thank Lynn Woolfrey at DataFirst at the University of Cape Town. Andrew Tomita was supported by SA MRC Flagship grant (MRC-RFAUFSP-01-2013/UKZN HIVEPI) with funds from the South African National Treasury under its Economic Competitiveness and Support Package. TM, BS, BPN, ADD, ATM, and RS were part of the Sustainable and Healthy Food Systems (SHEFS) programme supported by the Wellcome Trust’s Our Planet, Our Health programme [grant number: 205200/Z/16/Z]. The content is solely the responsibility of the authors and does not necessarily represent the official views of the South Africa Medical Research Council, South African National Treasury, or the Wellcome Trust. No conflict of interest reported.
Author information
Authors and Affiliations
Contributions
A.T. developed the conceptual approach. A.T. and D.F.C. analyzed the data and generated figures. A.T. wrote the first draft of the report. A.T., D.F.C., T.M., B.S., B.P.N., A.D.D., F.T., A.T.M., R.S. and J.K.B. contributed to the data interpretation and to the revision of the final report.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Tomita, A., Cuadros, D.F., Mabhaudhi, T. et al. Spatial clustering of food insecurity and its association with depression: a geospatial analysis of nationally representative South African data, 2008–2015. Sci Rep 10, 13771 (2020). https://doi.org/10.1038/s41598-020-70647-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-70647-1
This article is cited by
-
The spatial modification effect of predictors on household level food insecurity in Ethiopia
Scientific Reports (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.