Abstract
We hypothesized that Ventilator-Associated Event (VAE) within 28 days upon admission to medical intensive care units (ICUs) can be a predictor for poor outcomes in sepsis patients. We aimed to determine the risk factors and associated outcomes of VAE. A total of 453 consecutive mechanically ventilated (MV) sepsis patients were enrolled. Of them, 136 patients had immune profile study. Early VAE (< 7-day MV, n = 33) was associated with a higher mortality (90 days: 81.8% vs. 23.0% [non-VAE], P < 0.01), while late VAE (developed between 7 and 28 days, n = 85) was associated with longer MV day (43.8 days vs. 23.3 days [non-VAE], P < 0.05). The 90-day Kaplan–Meier survival curves showed three lines that separate the groups (non-VAE, early VAE, and late VAE). Cox regression models with time-varying coefficient covariates (adjusted for the number of days from intubation to VAE development) confirmed that VAE which occurred within 28 days upon admission to the medical ICUs can be associated with higher 90-day mortality. The risk factors for VAE development include impaired immune response (lower human leukocyte antigen D-related expression, higher interleukin-10 expression) and sepsis progression with elevated SOFA score (especially in coagulation sub-score).
Similar content being viewed by others
Introduction
Ventilator-associated event (VAE)1,2 was proposed to overcome the limitations of only focusing on ventilator-associated pneumonia (VAP)3 surveillance in mechanically ventilated (MV) patients in the context of surveying quality improvement. The limitations of previous VAP surveillance, which is proven to be neither sensitive nor specific4, hindered its application in quality improvement programs5. Although VAE surveillance was a promising early warning tool for VAP prevention6, VAP prevention bundle compliance was not associated with a reduced risk of VAE7. VAEs are defined as respiratory deterioration after a period of improved or stable gas exchange. The definition of VAE shifted the focus of surveillance from pneumonia to all conditions caused by mechanical ventilation including infectious or noninfectious conditions. The purpose was to expand the scope of surveillance to include multiple serious complications in ventilated patients, not just pneumonia, as well as to make surveillance more objective, efficient, and suitable for electronic implementation.
Sepsis patients developed life-threatening organ dysfunctions (e.g., acute respiratory failure) caused by dysregulated host immune response to infection8,9,10. An increase in sequential organ failure assessment (SOFA) score (including respiratory and other five sub-scores) has prognostic accuracy for in-hospital mortality in sepsis patients in the intensive care units (ICUs)11. Since mechanical ventilator support and aggressive fluid resuscitation are usually performed as sepsis management, sepsis patients are vulnerable to VAE development due to fluid overload12, ventilator-associated lung injury, VAP, and multiple organ dysfunction. The association between sepsis and VAE is complicated. Although several studies have tested the prognostic accuracy of VAE13,14,15 in the medical and surgical ICUs such as for trauma patients, only a few studies have been conducted among sepsis patients. Whether the presence of early VAE or late VAE influences the outcomes of sepsis patients remains unclear.
We hypothesize that VAE can be a predictor for poor outcomes (90-day mortality as the main outcome) in sepsis patients and is associated with impaired immune profile and abnormal values in serial SOFA sub-scores. The early onset of VAE (within 7 days upon ICU admission) may reflect the progression of sepsis in the first week, and late VAE (developed between day 7 and day 28) may indicate poor recovery from sepsis. The characteristics and outcomes of non-VAE, early VAE, and late VAE may be different. This study aimed to determine whether sepsis patients who develop VAEs within 28 days had poorer outcomes, regardless of early or late onset. It also aimed to investigate the predictors for early and late VAEs.
Methods
Setting
The study was conducted in three medical ICUs (total 34 beds) from August 2013 to January 2016 at Kaohsiung Chang Gung Memorial Hospital, a 2,700-bed tertiary hospital in Southern Taiwan.
Study design
The retrospective analysis study is a part of integrated research programs, consisting of prospective observational study (immune profile study) and retrospective medical record review (e.g., consecutive mechanically ventilated sepsis patients), that investigate the clinical factors, biomarkers, and immune response in predicting outcomes in sepsis patients10,16,17,18. All patients who met the Sepsis-3 criteria8 and admitted to the medical ICUs with invasive mechanical ventilation support were screened. The enrolled patients with sepsis were admitted to the ICU before development of VAE. Patients receiving noninvasive mechanical ventilation or extracorporeal membrane oxygenation use were excluded. To meet the VAE criteria, we also excluded those patients who never achieved stable ventilator setting after intubation or died within 3 days of mechanical ventilation initiation.
The study was approved by the Institutional Review Board of Chang Gung Memorial Hospital. We confirmed that all methods were performed in accordance with the relevant guidelines and regulations. For the patients who prospectively participated in immune profiling and cytokine analysis, patients or their surrogates had signed the written informed consent. The requirements to obtain informed consent for the retrospective analysis part of the study were waived by Institutional Review Board.
Definition and criteria for VAE: early VAE and late VAE
The following three categories of VAE were identified: (1) ventilator-associated condition (VAC), (2) infection-related ventilator-associated complication (IVAC), and (3) possible VAP19. VAC is defined as an increase of at least 3 cmH2O in daily minimum positive end expiratory pressure (PEEP) or an increase of at least 20 points in daily minimum fraction of inspired oxygen (FiO2) over baseline for at least 2 days, after at least 2 days of stable or decreasing PEEP or FiO2 20. IVAC belongs to the subset of VAC that may be infection related. VAP was defined as the presence of purulent secretions or positive pulmonary cultures. The culture specimens utilized for the testing of pneumonia organisms include sputum, tracheal aspirate, bronchoalveolar lavage fluid, pleural effusion, blood, and urine for Legionellae antigen test or Streptococcus pneumoniae antigen test21. Early VAE (within 7 days) and late VAE (between day 7 and day 28) were defined as the period from the initiation of mechanical ventilation to the onset of VAC. Patients who had an early VAE were not included in the late VAE model. Long-term ventilator dependence was defined as the need for mechanical ventilation for more than 6 h per day for more than 21 days22.
Data collection
Clinical data were retrieved from the medical records including SOFA score11,23,24, Acute Physiology and Chronic Health Evaluation II (APACHE II) score25,26, Charlson Comorbidity Index, and underlying comorbidities and other clinical factors that were possibly related to the occurrence of the condition. The factors for possible VAP were utilized for VAE surveillance1,27,28. Moreover, 136 patients had been enrolled in immune status and cytokine study with blood sampling tests performed based on the protocol on days 1, 3, and 7 during ICU admission (Fig. 1).
Immune status and cytokine study
Plasma and peripheral blood mononuclear cell preparation, measurements of human leukocyte antigen D-related (HLA-DR) monocyte expression, and cytokine levels have been described in our previous studies9, 10.
Statistical methods
Patient demographics, clinical characteristics, and outcomes were expressed using frequency and percentage for categorical variables and mean ± standard deviation or median (interquartile range, IQR) for continuous variables (Table 1). The differences between the non-VAE group and VAE group were analyzed using the Student’s t-test or Mann–Whitney U test, as appropriate, for continuous variables or the chi-square test for categorical variables. Comparison analyses among the non-VAE, early VAE, and late VAE groups were performed using the Pearson chi-square and one-way analysis of variance as appropriate. Pairwise comparisons were conducted using the analysis of variance (ANOVA) with adjustment for multiple comparisons utilizing Tukey's range test for post hoc comparisons (Table 2). Kruskal–Wallis test was used as a non-parametric alternative to the ANOVA for non-normally distributed continuous variables. Clinical parameters [e.g., baseline characteristics, SOFA sub-scores, laboratory data, oxygenation index, lung mechanics, and input/output (I/O) fluid balance on days 1, 3, and 7; details in Table 1 or e-Tables 1, and 2(a, b)] thought to be predictors of VAE development (early VAE and late VAE, respectively) were analyzed using a univariable regression analysis. The factors that were found to be statistically significant (P < 0.1) in the univariable regression analysis were then retained and included in the multivariable logistic regression model using backward elimination of logistic regression analysis to determine whether they remained predictive for early VAE (Table 3) or late VAE (Table 4) development. Patients who have been on invasive ventilation for at least 7 days are at risk for late VAE. The analytical population for late VAE was limited to those with at least 7 days of mechanical ventilation and was included in the multivariable logistic regression model. To assess the survival outcome between groups, Kaplan–Meier survival curves were constructed; comparison between groups was performed using the log-rank test. The mortality hazard ratios between groups were also compared using Cox regression models with time-varying coefficient or fixed (non-time-dependent) covariates. The number of days from intubation to VAE development was then adjusted. Statistical significance was set at a two-sided P value of < 0.05. All data were analyzed using the Statistical Package for the Social Sciences software version 22.0 (IBM Corp., Armonk, NY, USA).
Ethics approval and consent to participate
The study was approved by the Institutional Review Board of Chang Gung Memorial Hospital. We confirmed that all methods were performed in accordance with the relevant guidelines and regulations. For the patients who prospectively participated in immune profiling and cytokine analysis, patients or their surrogates had signed the written informed consent. The requirements to obtain informed consent for the retrospective analysis part of the study were waived by Institutional Review Board.
Results
A total of 453 sepsis patients were enrolled for analysis. Of them, 136 patients had immune profile study (Fig. 1). A total of 118 sepsis patients (26%) developed VAE after initial respiratory stabilization following sepsis treatment (Table 1). There were no notable differences between the VAE group and non-VAE group in terms of age, gender, body mass index, APACHE II score, and site of suspected infection. Their pneumonia severity scores21 (PSI and CURB65) were also comparable. Although more patients with VAE had cancer (VAE vs. non-VAE = 36% vs. 17%, P < 0.001) and higher Charlson Comorbidity Index (3.2 ± 2.2 vs. 2.4 ± 1.7, P = 0.001), the phenomenon disappeared in the multivariable analysis.
Sepsis patients who developed VAEs with poorer outcomes
Patients in the VAE group (compared to non-VAE) have a longer ICU length of stay (LOS) (20.1 ± 13.7 days vs. 12.6 ± 7.5 days, P < 0.001); longer duration of mechanical ventilation (36.4 ± 46.8 days vs. 23.3 ± 63.0 days, P = 0.040); higher 7-day, 14-day, 28-day, and 90-day ICU and hospital mortality (Table 2, e-Fig. 1); and higher ventilator dependence (57% vs. 22.7%, P < 0.001) (Table 2).
Different outcomes and serial clinical variables among the non-VAE, early VAE, and late VAE groups
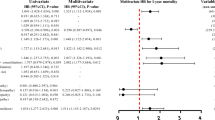
The incidence of all VAEs in our study was 26%; patients developed the VAE within a median of 13 days (IQR 7–24) (Table 2). Patients developed the early VAE within a median of 5 days (IQR 4–6) and the late VAE within a median of 17 days (IQR 12–28). The outcomes of the late VAE group were poorer than those of the early VAE group in terms of ventilator dependence, total ventilation days, LOS, and hospital LOS (Table 2). However, early VAE was a good predictor of poorer 7-day, 14-day, 28-day, and ICU mortality than late VAE. The 90-day mortality and hospital mortality were comparable between early VAE and late VAE (Table 2). Kaplan–Meier survival curves showed three lines that separates the non-VAE, early VAE, and late VAE groups (Fig. 2). However, the early VAE and late VAE group showed comparable mortality hazard ratios in the 90-day Cox regression model with time-varying coefficient (time to VAE development after intubation).
Ninety-day survival curves of the non-VAE, early VAE, and VAE groups. Kaplan–Meier estimates of 90-day survival according to stratification of the three groups. Hazard ratios between groups using Cox regression models with time-varying coefficient were shown. The number of days from intubation to VAE development was adjusted.
E-Table 2(a) and (b) illustrates the clinical characteristics of the non-VAE, early VAE, and late VAE groups in different time points (day 1, day 3, and day 7).
Predictor for early VAE
No statistically significant differences were observed between the VAE group and non-VAE group in terms of demographic characteristics except for the presence of underlying cancer and poorer Charlson Comorbidity Index in the VAE group (e-Table 1). The fluid balance of the VAE group on day 1 was not significantly different compared with that of the non-VAE group (e-Table 2(a)). However, cumulative positive fluid balance was noted in the early VAE group (e-Table 3). From the analysis on the serial SOFA sub-scores and laboratory data, we found that patients who developed early VAE had poorer coagulation sub-score on day 1 and elevated serum lactate level and SOFA score (including coagulation, liver, and cardiovascular [CV] sub-scores) on day 3 (e-Table 2(a), (b)). Logistical regression yields that the coagulation sub-score on day 3 can predict the development of early VAE (Table 3). The SOFA score has been shown to decrease over time in the non-VAE group (e-Table 4).
Predictors for late VAE
The presence of underlying cancer and poorer Charlson Comorbidity Index were significantly different between the late VAE group and non-VAE group (e-Table 1). E-Table 2(a) and (b) shows the different variables between patients with late VAE and those without VAE. Cumulative positive fluid balance was noted in the late VAE group (e-Table 3). Table 4 presents some of the characteristics of the late VAE. Multivariable logistic regression yielded that poor coagulation sub-score on day 3, poor CV sub-score on day 7, and increased airway resistance on day 7 were predictors of late VAE development. On the contrary, respiration sub-score on day 3 and red blood cell (RBC) count on day 7 were negative predictors of late VAE.
Immune status and cytokine expression characteristics of patients with early VAE and late VAE
No difference was observed in the 90-day mortality between patients who had immune data for this analysis and those who did not have the data. They had similar survival curves regardless of VAE status (e-Fig. 2).
In this subpopulation with immune status and cytokine studies (Table 5), the early VAE group had lower HLA-DR expression (76.6 ± 21.1% vs. 87.3 ± 15.0%, P = 0.051) on day 1, while the late VAE group had lower HLA-DR expression (80.8 ± 20.6% vs. 94.3 ± 8.0%, P < 0.05) on day 7. The late VAE group had significantly higher anti-inflammatory cytokine (interleukin-10 [IL-10]) on day 1 and day 7 compared with the non-VAE group. This finding suggests that the patients were immunosuppressed prior to the appearance of VAE. However, the late VAE group showed increased in granulocyte-colony stimulating factor (G-CSF), interleukin-6 (IL-6), and tumor necrosis factor alpha (TNF-α) on day 3. On day 7, the IL-6 concentration in the late VAE group remained high compared with that in the non-VAE group. There were differences in the immune profiles of VAE and non-VAE groups.
Discussion
Our study shows that VAE within 28 days of ICU admission can be a simple predictor of poorer outcomes (mortality and ventilator dependency) for sepsis patients with initially stable respiratory condition after treatment. The notion of “early VAE” vs “late VAE” is novel since it is a concept borrowed from VAP and not hitherto applied to VAE. The interaction between sepsis and VAE before day 7 may be more complicated. Many sepsis studies considered 28-day all-cause mortality as the primary outcome measure. We suggested that VAE that developed after day 28 was less likely to interact with sepsis. Therefore, late VAE was considered respiratory deterioration developed between day 7 and day 28. The patients who did not develop VAE within 28 days were stratified as non-VAE. The characteristics and outcomes of non-VAE, early VAE, and late VAE were different.
VAE development might be related either with worsening of the initial episode of sepsis or a with a new episode. The development of VAE is associated with patients’ impaired immune profile during sepsis. Before the patients developed VAE, bigger positive cumulative fluid balance, abnormal SOFA score and sub-scores, and other risk factors have already been identified. Changes in SOFA sub-scores vary by VAE status (e-Table 4 [see Additional file 1]). We also demonstrated the different effects of early and late VAE on sepsis patients’ outcomes.
VAP is associated with a longer ICU length of stay, longer duration of mechanical ventilation, and higher mortality29. Therefore, VAP surveillance was initiated, and VAP prevention bundle care was encouraged. To enhance the quality improvement programs, a VAE definition was proposed. However, VAE surveillance is insensitive for identifying VAP30. A recent study confirmed that there was poor agreement between VAE and VAP31. Therefore, the outcomes of patients with VAE may be different from those with VAP. In addition, some other conditions during mechanical ventilation also cause the deterioration in gas exchange, such as pulmonary edema, acute respiratory distress syndrome, and lung atelectasis. Sepsis is also among the risk factors for the abovementioned syndromes. Therefore, the rate of VAE (118/453 [26.0%]) in our series was higher than those reported in other studies32. Our VAE cases include 23 (19.4%) VACs, 47 (39.8%) IVACs, and 48 (40.6%) possible VAPs. The three categories of VAE may have specific impact on outcomes; however, that is beyond the scope of this study. VACs, IVACs, and possible VAPs had been combined into one category owing to the small number of samples with VAEs. The distributions of VAE types (i.e., VAC, IVAC, and possible VAP) between the early and late VAE groups were similar (e-Table 5).
Many factors affect the outcomes of sepsis patients33. The severity scores (APACHE II and SOFA scores) on day 1 were comparable. Therefore, the poor outcomes in VAE group were not due to the baseline sepsis severity. Sepsis patients were admitted to the ICU primarily due to pneumonia. We tested the severity score of pneumonia, and results showed that VAE and non-VAE were comparable. The higher Charlson Comorbidity Index in the VAE group was due to the higher percentage of patients with cancer. As in our previous study, sepsis patients with underlying active cancer had higher baseline levels of plasma IL-109. Although IL-10 levels were higher in the late VAE group than in the non-VAE group on day 1 and day 7, whether cancer patients were at risk of developing VAE for this reason needs further investigation. Anyway, the presence of cancer did not remain predictive for early VAE or late VAE development using multivariable logistic regression model.
Sepsis patients experience life-threatening organ dysfunction, which can be reflected on their SOFA score. The SOFA score assesses the severity of organ dysfunction in six organ systems: respiration, coagulation, liver, CV, central nervous system (CNS), and renal34. It can be applied to improve our understanding of the history of organ dysfunction and the interrelation between the failure of various organs35. Coagulation abnormalities contribute to sepsis-associated organ failure and uncontrolled inflammations36,37. Coagulopathy is associated with an increased incidence of early and late VAE in our study. The similar phenomenon was also observed in burn patients38. An elevated serum lactate concentration is a biomarker of tissue hypoperfusion during sepsis37,38,39. The elevated lactate level was noted on day 3 in the early VAE group and day 7 in the late VAE group, suggesting the relationship between tissue hypoperfusion and VAE development. The need for more fluid resuscitation, resulting in bigger positive cumulative fluid balance before the patients developed VAE, can be partially due to patients’ tissue hypoperfusion. Meanwhile, lung compliance can decrease because of pulmonary edema either due to fluid overload or sepsis progression. Furthermore, adequate oxygen delivery to peripheral tissue involves the integration of the various organs. Clear central nerve system drives the respiratory muscle to inspire air into the lung where oxygen exchange happens, and RBC takes the oxygen to the peripheral tissue. The impact of an elevated SOFA-score, coagulation disorders, and increasing lactate levels on adverse outcome is very clear. However, the relationship of the above factors with the development of VAE is less clear. Any impairment of the above organ can contribute to the development of late VAE and can be considered a risk factor (Table 4). An elevated RBC count has an inverse association with late VAE. Patients’ respiratory sub-scores will become poorer once they develop early VAE, as those who developed early VAE were excluded from the group with late VAE. This condition may explain why there was an inverse association between respiratory sub-score and late VAE development.
In addition to the above clinical data, one unique strength of our study is the performance of subpopulation analysis with immune status and cytokine study. Our results demonstrated serial immune status (HLA-DR; the levels indicate the percentage of activated serum monocyte with decreased number in immune suppression), proinflammatory cytokines (G-CSF, IL-6, TNF-α), and anti-inflammatory cytokine (IL-10) levels, which are important in patients with sepsis (Table 5). Our data showed that VAE development was associated with immune suppression (HLA-DR decreased, IL-10 elevated). Those immune dysfunctions in sepsis patients were associated with poor prognosis10. There were different trends by VAE status in the changes in cytokine levels (e-Table 6). Although the limited number of VAE patients enrolled in the immune study precludes further analysis, the study brings new insight into this field. The connection of VAE to VAP may include a compromised immune response40. By adding this phenomenon to the clinical factors, we can improve the detection of VAP.
The limitations of the study include the moderate number of patients and possible time-dependent confounding in the analyses of 28-day prognosis among the early VAE, late VAE, and non-VAE patients. We are interested in determining the influence of VAE on this episode of sepsis, which occurred upon ICU admission. However, the patients must have survived and been on the ventilator long enough to get the VAE. Therefore, the 90-day Kaplan–Meier survival curves with time zero were provided upon ICU admission. To account for immortal person time, we calculated the mortality hazard ratios between groups using Cox regression models with time-varying coefficient covariates. The number of days from intubation to VAE development was then adjusted. The Cox regression models with fixed (non-time-dependent) were also provided for reference (e-Table 7). Those models drew the same conclusion that VAE that occurred within 28 days of admission to the medical ICUs can be a predictor for poor outcomes in sepsis patients. We excluded patients who never had a period of stable or decreasing oxygenation. For those patient group, an immune dysfunction score can be used to predict the 28-day mortality10. In treating sepsis, strategies to reduce nosocomial infections are important39. In addition to predicting VAP, VAE surveillance could be used as another marker for mortality and prolonged mechanical ventilation prediction.
Conclusions
In MV sepsis patients, after a period of improved or stable gas exchange, VAE was associated with a higher mortality, and patients with late VAE were prone to ventilation dependency. The risk factors include impaired immune response and sepsis progression with elevated SOFA score (especially in coagulation sub-score).
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Klompas, M. et al. The preventability of ventilator-associated events. The CDC prevention epicenters wake up and breathe collaborative. Am. J. Respir. Crit. Care Med. 191, 292–301. https://doi.org/10.1164/rccm.201407-1394OC (2015).
Klompas, M. Potential strategies to prevent ventilator-associated events. Am. J. Respir. Crit. Care Med. 192, 1420–1430. https://doi.org/10.1164/rccm.201506-1161CI (2015).
O’Grady, N. P., Murray, P. R. & Ames, N. Preventing ventilator-associated pneumonia: Does the evidence support the practice?. JAMA 307, 2534–2539. https://doi.org/10.1001/jama.2012.6445 (2012).
Canadian Critical Care Trials, G. A randomized trial of diagnostic techniques for ventilator-associated pneumonia. N. Engl. J. Med. 355, 2619–2630. https://doi.org/10.1056/NEJMoa052904 (2006).
Raoof, S., Baumann, M. H. & Critical Care Societies Collaborative, c. o. t. l. o. t. A. A. o. C.-C. N. t. A. C. o. C. P. t. A. T. S. & the Society of Critical Care, M. Ventilator-associated events: The new definition. Am. J. Crit. Care 23, 7–9. https://doi.org/10.4037/ajcc2014469 (2014).
Klompas, M. & Berra, L. Should ventilator-associated events become a quality indicator for ICUs?. Respir. Care 61, 723–736. https://doi.org/10.4187/respcare.04548 (2016).
Harris, B. D., Thomas, G. A., Greene, M. H., Spires, S. S. & Talbot, T. R. Ventilator bundle compliance and risk of ventilator-associated events. Infect Control Hosp. Epidemiol. 39, 637–643. https://doi.org/10.1017/ice.2018.30 (2018).
Singer, M. et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA 315, 801–810. https://doi.org/10.1001/jama.2016.0287 (2016).
Fang, W. F. et al. Immune profiles and clinical outcomes between sepsis patients with or without active cancer requiring admission to intensive care units. PLoS ONE 12, e0179749. https://doi.org/10.1371/journal.pone.0179749 (2017).
Fang, W. F. et al. Development and validation of immune dysfunction score to predict 28-day mortality of sepsis patients. PLoS ONE 12, e0187088. https://doi.org/10.1371/journal.pone.0187088 (2017).
Raith, E. P. et al. Prognostic accuracy of the SOFA score, SIRS criteria, and qSOFA score for in-hospital mortality among adults with suspected infection admitted to the intensive care unit. JAMA 317, 290–300. https://doi.org/10.1001/jama.2016.20328 (2017).
Lewis, S. C., Li, L., Murphy, M. V., Klompas, M. & Epicenters, C. D. C. P. Risk factors for ventilator-associated events: A case–control multivariable analysis. Crit Care Med. 42, 1839–1848. https://doi.org/10.1097/CCM.0000000000000338 (2014).
Younan, D., Griffin, R., Zaky, A., Pittet, J. F. & Camins, B. A comparison of outcomes of trauma patients with ventilator- associated events by diagnostic criteria set. Shock https://doi.org/10.1097/SHK.0000000000001214 (2018).
Boyer, A. F. et al. A prospective evaluation of ventilator-associated conditions and infection-related ventilator-associated conditions. Chest 147, 68–81. https://doi.org/10.1378/chest.14-0544 (2015).
Klompas, M., Kleinman, K. & Murphy, M. V. Descriptive epidemiology and attributable morbidity of ventilator-associated events. Infect Control Hosp. Epidemiol. 35, 502–510. https://doi.org/10.1086/675834 (2014).
Fang, W. F. et al. Application of dynamic pulse pressure and vasopressor tools for predicting outcomes in patients with sepsis in intensive care units. J. Crit. Care 52, 156–162. https://doi.org/10.1016/j.jcrc.2019.05.003 (2019).
Chang, Y. C. et al. The effect of do-not-resuscitate orders on patients with sepsis in the medical intensive care unit: A retrospective, observational and propensity scorematched study in a tertiary referral hospital in Taiwan. BMJ Open 9, e029041. https://doi.org/10.1136/bmjopen-2019-029041 (2019).
Fang, W. F. et al. Incorporation of dynamic segmented neutrophil-to-monocyte ratio with leukocyte count for sepsis risk stratification. Sci. Rep. 9, 19756. https://doi.org/10.1038/s41598-019-56368-0 (2019).
Levy, M. M. A new definition of ventilator-associated pneumonia: Far from perfect, better than before. Ann. Am. Thorac. Soc. 10, 644–645. https://doi.org/10.1513/AnnalsATS.201310-361ED (2013).
Magill, S. S. et al. Developing a new, national approach to surveillance for ventilator-associated events: Executive summary. Chest 144, 1448–1452. https://doi.org/10.1378/chest.13-1640 (2013).
Fang, W. F. et al. Application and comparison of scoring indices to predict outcomes in patients with healthcare-associated pneumonia. Crit. Care 15, R32. https://doi.org/10.1186/cc9979 (2011).
Chang, Y. C. et al. Ventilator dependence risk score for the prediction of prolonged mechanical ventilation in patients who survive sepsis/septic shock with respiratory failure. Sci. Rep. 8, 5650. https://doi.org/10.1038/s41598-018-24028-4 (2018).
Seymour, C. W. et al. Assessment of Clinical Criteria for Sepsis: For the Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA 315, 762–774. https://doi.org/10.1001/jama.2016.0288 (2016).
Schuler, A. et al. The impact of acute organ dysfunction on long-term survival in sepsis. Crit. Care Med. 46, 843–849. https://doi.org/10.1097/CCM.0000000000003023 (2018).
Lee, H. et al. Efficacy of the APACHE II score at ICU discharge in predicting post-ICU mortality and ICU readmission in critically ill surgical patients. Anaesth. Intensive Care 43, 175–186. https://doi.org/10.1177/0310057X1504300206 (2015).
Knapik, P., Krzych, L. J., Weigl, W., Adamski, J. & Hultstom, M. Mortality rate in Polish intensive care units is lower than predicted according to the APACHE II scoring system. Intensive Care Med. 43, 1745–1746. https://doi.org/10.1007/s00134-017-4883-0 (2017).
Waters, B. & Muscedere, J. A 2015 update on ventilator-associated pneumonia: new insights on its prevention, diagnosis, and treatment. Curr. Infect. Disease Rep. 17, 496. https://doi.org/10.1007/s11908-015-0496-3 (2015).
Mann, T. et al. Building and validating a computerized algorithm for surveillance of ventilator-associated events. Infect Control Hosp. Epidemiol. 36, 999–1003. https://doi.org/10.1017/ice.2015.127 (2015).
Muscedere, J. G., Martin, C. M. & Heyland, D. K. The impact of ventilator-associated pneumonia on the Canadian health care system. J. Crit. Care 23, 5–10. https://doi.org/10.1016/j.jcrc.2007.11.012 (2008).
Zhang, C., Berra, L. & Klompas, M. Should aerosolized antibiotics be used to treat ventilator-associated pneumonia?. Respir. Care 61, 737–748. https://doi.org/10.4187/respcare.04748 (2016).
Pouly, O. et al. Accuracy of ventilator-associated events for the diagnosis of ventilator-associated lower respiratory tract infections. Ann. Intensive Care 10, 6. https://doi.org/10.1186/s13613-020-0624-6 (2020).
He, S. et al. Ventilator-associated events after cardiac surgery: evidence from 1,709 patients. J. Thorac. Disease 10, 776–783. https://doi.org/10.21037/jtd.2018.01.49 (2018).
Hung, K. Y. et al. Insufficient nutrition and mortality risk in septic patients admitted to ICU with a focus on immune dysfunction. Nutrients 11, 367. https://doi.org/10.3390/nu11020367 (2019).
Jones, A. E., Trzeciak, S. & Kline, J. A. The Sequential Organ Failure Assessment score for predicting outcome in patients with severe sepsis and evidence of hypoperfusion at the time of emergency department presentation. Crit. Care Med. 37, 1649–1654. https://doi.org/10.1097/CCM.0b013e31819def97 (2009).
Vincent, J. L. et al. The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Intensive Care Med. 22, 707–710 (1996).
Fang, W. F. et al. Histone deacetylase 2 (HDAC2) attenuates lipopolysaccharide (LPS)-induced inflammation by regulating PAI-1 expression. J. Inflamm. (London, England) 15, 3. https://doi.org/10.1186/s12950-018-0179-6 (2018).
Abraham, E. Do coagulation abnormalities contribute to sepsis associated organ failure?. Crit. Care Med. 34, 1842–1844. https://doi.org/10.1097/01.CCM.0000220051.19432.05 (2006).
Younan, D. et al. Early coagulopathy is associated with increased incidence of ventilator-associated events among burn patients. Shock 47, 107–110. https://doi.org/10.1097/SHK.0000000000000738 (2017).
Gotts, J. E. & Matthay, M. A. Sepsis: Pathophysiology and clinical management. BMJ 353, i1585. https://doi.org/10.1136/bmj.i1585 (2016).
Almansa, R. et al. Transcriptomic depression of immunological synapse as a signature of ventilator-associated pneumonia. Ann. Transl. Med. 6, 415. https://doi.org/10.21037/atm.2018.05.12 (2018).
Acknowledgements
We would like to thank all the staff and clinicians in the ICU who participated in this study and for their support. We also thank the Biostatistics Center, Kaohsiung Chang Gung Memorial Hospital, for their statistical assistance. The work is supported in part by Grants from the Chang Gung Memorial Hospital Grant (CMRPG8B1063, CMRPG8F1331, CMRPG8H1171, CMRPG8J0421, and CMRPG8J0422) to WF Fang, CMRPG8B1073 to YH Wang, and CMRPG8B1083 to CC Wang.
Author information
Authors and Affiliations
Contributions
Conception or design of the work: W.-F.F., Y.-T.F., C.-C.W., and M.-C.L. Acquisition, analysis, or interpretation of data for the work: C.-H.H., Y.-T.F., Y.-M.C., Y.-C.C., C.-Y.L., K.-Y.H., Y.-T.C., H.-C.C., K.-T.H., H.-C.C., Y.-C.C., Y.-H.W., C.-C.W., M.-C.L., and W.-F.F. Drafting the work and revising it critically for important intellectual content: C.-H.H. and W.-F.F.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Fang, WF., Fang, YT., Huang, CH. et al. Risk factors and associated outcomes of ventilator-associated events developed in 28 days among sepsis patients admitted to intensive care unit. Sci Rep 10, 12702 (2020). https://doi.org/10.1038/s41598-020-69731-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-69731-3
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.