Abstract
The apolipoprotein E (APOE) e4 allele is the most common genetic variant associated with Alzheimer’s disease (AD). We sought to investigate the distribution of APOE genotypes across the full clinical AD spectrum including AD, late-stage amnestic mild cognitive impairment (L-aMCI), early-stage aMCI (E-aMCI), subjective memory impairment (SMI), and controls. We prospectively recruited 713 AD patients, 735 aMCI patients, 575 SMI patients, and 8,260 individuals as controls. The frequency of the APOE e4 allele revealed an ordered fashion in the AD (30.8%), L-aMCI (24.0%), E-aMCI (15.1%), SMI (11.7%), and control (9.1%) groups. APOE e3/e4 and e4/e4 genotype frequencies also appeared in an ordered fashion in the AD group (39.1% of e3/e4 and 10.9% of e4/e4), as well as the L-aMCI (28.3% and 9.4%), E-aMCI (22.3% and 3.7%), SMI (18.3% and 1.9%), and control (15.1% and 0.8%) groups. In the comparisons of APOE e3/e3 vs. e3/e4 genotypes, all patient groups had a higher frequency of APOE e3/e4 relative to the control group. Relative to the SMI and E-aMCI groups, the AD and L-aMCI groups had higher frequency of the APOE e3/e4 genotype, and the AD group had a higher frequency relative to the L-aMCI group. However, there was no significant difference between the E-aMCI and SMI groups. In our longitudinal data, APOE e4 carrier showed a steeper incline slope in a clinical dementia rating sum of boxes (CDR-SB) score than APOE e4 non-carrier in SMI (B = 0.0066, p = 0.0104), E-aMCI (B = 0.0313, p < 0.0001), and L-aMCI (B = 0.0178, p = 0.0007). APOE e4 carrier showed a steeper decline slope in the CDR-SB than APOE e4 non-carrier in AD (B = − 0.0309, p = 0.0003). These findings suggest that E-aMCI and SMI are associated with a similarly increased frequency of the APOE e4 allele compared to controls, suggesting a greater genetic risk for AD and the importance of monitoring the allele more closely.
Similar content being viewed by others
Introduction
The apolipoprotein E (APOE) e4 allele is the most common genetic variant associated with Alzheimer’s disease (AD), with the presence of an allele increasing the risk of developing AD1,2,3,4. Several studies have reported that the prevalence of APOE e4 is higher among patients with mild cognitive impairment (MCI) compared to the general population, at 36.5%5 and 27.9%6 in Western countries, and 21.4%7 in Asia.
Although the most commonly accepted prodromal AD stage is amnestic MCI (aMCI), recent studies (ADNI GO, ADNI 2) have described two forms based on severity: early aMCI (E-aMCI) and late aMCI (L-aMCI). L-aMCI refers to the original definition (with test performance of 1.5 SD below the normative mean), while E-aMCI is defined as between 1.0 and 1.5 SD below the normative mean on a memory test8. Furthermore, to define an even earlier point in time for disease detection, subjective memory impairment (SMI) is sometimes considered to be the first clinical indicator of AD even prior to aMCI. SMI is defined by subjective reports of memory decline with no evidence of cognitive impairment on formal testing9. Epidemiologic studies have reported more rapid progression in cognitive decline and the development of AD in E-aMCI6 and SMI patients10,11,12,13. Some studies have investigated the frequency of the APOE e4 allele in E-MCI in Western countries (NC:E-MCI = 24.4%:40.7%)14, (NC:E-MCI = 18.9%:17.5%)6 and SMI (NC:SMI = 21%:29%)15, (NC:SMI = 15%:22%)5, (NC:SMI = 22.2%:26.8%)16, as well as China (NC:SMI = 7.3%:14.7%)7. However, the results have been inconsistent, which could be due to the relatively small and varying sample sizes.
A greater understanding of the preclinical stages of AD is critical to determine the future development of AD. The aim of this study was to evaluate the distribution of the APOE e4 genotype in AD, L-aMCI, E-aMCI, SMI, and control groups in a relatively large cohort of patients across the full clinical AD spectrum, and to compare the frequency of the genotype between the different diagnostic categories. Furthermore, we determined whether APOE e4 genotype might affect clinical progression measured by a clinical dementia rating sum of boxes (CDR-SB) score in AD, L-aMCI, E-aMCI, and SMI.
Results
Demographic characteristics
The demographic characteristics of the study participants are listed in Table 1. The age at the initial visit recorded at the memory clinic was higher in the AD, L-aMCI, E-aMCI, and SMI groups compared to the control group. The gender distribution was distinct between the control and AD, L-aMCI, E-aMCI, and SMI groups. Mean MMSE scores were also lower in the AD group than in the other groups.
APOE genotypes and alleles
The distribution of the APOE allele differed between the diagnostic groups (Table 2). APOE e4 allele frequency had an ordered fashion in the AD, L-aMCI, E-aMCI, SMI, and control groups (30.8%, 24.0%, 15.1%, 11.7% and 9.1%, respectively).
APOE e3/e3 vs. e3/e4 genotyping was statistically significant between the diagnostic groups (Table 3). Relative to the control group, all patient groups had a higher frequency of the APOE e3/e4 allele. Relative to the SMI and E-aMCI groups, the AD and L-aMCI groups had a higher frequency of the APOE e3/e4 genotype, while the AD group had a higher frequency relative to the L-aMCI group. However, no statistical significance was observed between the E-aMCI and SMI groups.
Comparison of the APOE e3/e3 vs. e4/e4 genotypes or APOE e4 carrier vs. APOE e4 non-carriers showed a similar pattern to comparisons of the APOE e3/e3 vs. e3/e4 genotypes (Table 3).
Longitudinal cognitive change according to APOE e4 genotypes
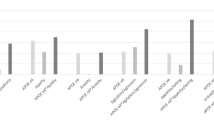
Supplementary Table S2 summarizes the characteristics of the subjects included in the longitudinal study. APOE e4 carrier showed a steeper incline slope in a clinical dementia rating sum of boxes (CDR-SB) score than APOE e4 non-carriers in SMI (B = 0.0066, p = 0.0104), E-aMCI (B = 0.0313, p < 0.0001), and L-aMCI (B = 0.0178, p = 0.0007) (Figure). APOE e4 carrier showed a steeper decline slope in the CDR-SB than APOE e4 non-carriers in AD (B = -0.0309, p = 0.0003) (Fig. 1).
Cognitive changes in the follow-up duration according to APOE e4 genotypes. APOE e4 carrier showed a steeper incline slope in CDR-SB score than APOE e4 non-carriers in SMI, E-aMCI, and L-aMCI. However, in AD, APOE e4 non-carrier showed a steeper inline slope in the CDR-SB than APOE e4 carriers. APOE apolipoprotein E, CDR-SB clinical dementia rating sum of boxes, AD Alzheimer’s disease, E-aMCI early-stage amnestic mild cognitive impairment, L-aMCI late-aMCI, SMI subjective memory impairment.
Methods
Subjects
We prospectively recruited 713 AD patients, 735 aMCI patients, and 575 SMI patients, with all diagnosed at Samsung Medical Center (Seoul, Republic of Korea) from August 2006 until June 2012. Eligible patients were required to meet the criteria for probable AD as described by NINCDS-ADRDA (National Institute of Neurological and Communicative Disorders and Stroke and the Alzheimer’s Disease and Related Disorders Association)17. All aMCI cases met the criteria described by Petersen et al.18, including: (1) subjective memory complaint by patients or caregivers; (2) normal general cognitive function as defined by scores on the Korean version of the Mini-Mental State Examination (MMSE) ≥ − 1.0 standard deviation (SD) of the norms for age- and education-matched normal participants; (3) normal activities of daily living (ADL), as judged both clinically and on the ADL scale described later; (4) objective memory decline below the sixteenth percentile (− 1.0 SD) on either verbal or visual memory tests; and (5) without dementia. The aMCI subjects were classified in accordance with the baseline results of their memory test. Abnormal memory function was classified when recall scores were delayed on either the SVLT or RCFT at lower than − 1.0 SD relative to age-, gender-, and education- matched norms. Patients with scores that were between − 1.5 and − 1.0 SD of age-, gender-, and education-matched norms received an E-aMCI classification, while scores lower than − 1.5 SD resulted in an L-aMCI classification. From the 735 patients with aMCI, we excluded 86 subjects with incomplete data from the neuropsychological tests. Finally, 649 patients with aMCI were further classified E-aMCI (215) and L-aMCI (434) groups. SMI was determined if the memory clinic received a referral for subjects for the reason of memory impairment and by the standard question: “Do you feel like your memory is becoming worse?” with the answer “Yes, this worries me”. Subjects were excluded if they selected either of the other options: “no” or “yes, but this does not worry me”. To support the validity of memory impairment, only those subjects whose memory worsening was confirmed by others, including their spouses or close relatives (often accompanying the patient to the memory clinic). SMI was defined by subjective memory complaint from patients or caregivers, as well as normal cognitive function as defined by objective neuropsychological test results, normal ADL, and without mild cognitive impairment. Cognitive function was considered normal when all cognitive tests were higher than − 1.0 SD of the age-, gender-, and education- matched norms.
After obtaining informed consent, all patients were required to undertake comprehensive interviews, a neurological exam, and a series of neuropsychological tests [Seoul Neuropsychological Screening Battery (SNSB)]19,20,21, brain MRI scans, and APOE e4 genotyping. Patients were excluded from the study if they presented with other structural lesions detected on brain MRI, including territorial infarction, brain tumor, intracranial hemorrhage, hydrocephalus or severe white matter hyperintensities (WMH). The possibility of alternative causes of cognitive deficits was eliminated by laboratory testing for complete blood count, blood chemistry, folate, vitamin B12, syphilis serology and thyroid function tests. The study protocol was approved by Samsung Medical Center’s Institutional Review Board. All methods in this study were performed in accordance with applicable guidelines.
APOE genotyping
The Wizard Genomic DNA Purification kit was used to extract genomic DNA from peripheral blood leukocytes, following the manufacturer’s instructions (Promega, Madison, WI, USA). Within the APOE gene, the single nucleotide polymorphisms (rs429358 in codon 112 and rs7412 in codon 158) were genotyped with a TaqManSNP Genotyping Assay (Applied Biosystems, Foster City, CA, USA) using a 7500 Fast Real-Time PCR System (Applied Biosystems) according to the manufacturer’s instructions.
In order to compare the APOE genotype and allele frequencies of AD, MCI, and SMI groups with a control population, an extensive dataset including 8,260 individuals who underwent routine health exams between 1995 and 2002 at Samsung Medical Center’s Health Promotion Center was used.
Neuropsychological testing
The patients were required to undergo neuropsychological testing using the Seoul Neuropsychological Screening Battery (SNSB)19,20,21. The battery is comprised of quantitative tests, including the Korean version of the Boston Naming Test (K-BNT)22, digit span (forward and backward), Rey-Osterrieth Complex Figure Test (copying, immediate, 20-min delayed recall, and recognition), phonemic and semantic Controlled Oral Word Association Test (COWAT), Seoul Verbal Learning Test (SVLT; three learning-free recall trials of 12 words, a 20-min delayed recall trial for these 12 items, and a recognition test), and a Stroop Test (word/color reading of listed items over a 2-min period).
Clinical follow-up
We collected CDR-SB scores from 455 patients (82 SMI, 61 E-aMCI, 169 L-aMCI, and 143 AD) who were followed up more than three times to obtain CDR-SB scores at the Samsung Medical Center. Their clinical follow-up was performed until 2015. The study subjects were examined for 2.4 ± 2.2 years from baseline. Although the follow-up times and durations varied among participants, their mean duration was 29.2 months while the follow-up tests were conducted 4.0 times on average.
Statistical analysis
Chi-square test was applied to assess the APOE genotype and allele frequencies among the AD, L-aMCI, E-aMCI, SMI and control groups. Statistical significance was defined at p < 0.05, corrected for the false discovery rate (FDR).
Longitudinal statistical analyses were conducted with linear mixed effect model and adjusted for age, sex, education years, follow-up duration and presence of an APOE e4 (PROC MIXED; SAS version 9.4, SAS Institute).
Discussion
Few studies have investigated the frequency of APOE e4 alleles in the continuum of NC and AD in Asia7, although some similar studies in Western countries have been reported5,6. In the present study, an ordered trend in the frequency of the APOE e4 allele was observed: AD (30.8%), L-aMCI (24.0%), E-aMCI (15.1%), SMI (11.7%), and control (9.1%) groups, suggesting that there is an increasing trend in the frequency of APOE e4 alleles in the AD spectrum. Furthermore, APOE e4 carrier showed more rapid cognitive decline than APOE e4 non-carrier from SMI to L-aMCI while in AD, APOE e4 non-carrier showed more rapid cognitive decline than APOE e4 carrier. Therefore, our findings replicated that APOE e4 genotype is a prognostic factor of AD as well as important risk factor.
We investigated the distribution of APOE genotypes in AD, L-aMCI, E-aMCI, SMI, and control groups in Korea. Across all groups, we observed increasing frequency of the APOE e4 allele in an ordered fashion, with the highest risk in AD (30.8%) followed by L-aMCI (24.0%), E-aMCI (15.1%), SMI (11.7%), and control (9.1%) groups (Table 2). This finding shows that frequency of APOE e4 allele increases as impairment increases. The incidence of the APOE ε4 allele in patients with AD was consistent with the findings of previous studies in Korea which reported 44.3%23, 22.3%24, and 41.6%25. The frequency of the APOE e4 with NC was also comparable to that found in normal Korean subjects (9.1%) in another study24. Previous studies have demonstrated consistent results with the frequency of the APOE e4 allele in L-aMCI being significantly higher compared with the general population: 36.5%5 and 27.9%6 in Western countries, and 21.4% in China7. In addition, several reports have demonstrated that the APOE e4 genotype is associated with a more rapid progression from L-aMCI to AD26,27,28, implying that the presence of APOE e4 is a genetic risk factor for the future development of AD.
We have found that APOE e4 frequency in ethnic Koreans is lower than that reported in Western studies for controls as well as AD and MCI patients. Previous studies have consistently shown that patients of Asian ethnicity have lower APOE e4 frequency than their Western counterparts with AD and MCI29,30 and in the general population29,31. In a recent meta-analysis32, the frequency of APOE e4 carriers was 68.9% vs 52.1% in AD, 52.5% vs 33.3% in MCI, and 35.3% vs 22.5% in control subjects (northern Europe vs Asia)32. They demonstrated that APOE e4 prevalence in Asia was statistically lower than in northern Europe and North America. However, because the number of Asians in the study was relatively small (around 100 per group), it was necessary to assess the frequency of APOE e4 in an additional larger cohort. Our results suggest that the frequency of APOE e4 can be dependent on racial and regional differences, which should be considered in clinical research and during the selection of patients for AD treatment.
We observed that the frequency of the APOE e3/e4 genotype is higher in E-aMCI and SMI as well as AD and L-aMCI, relative to the controls (Table 3). There have been previous reports on the frequency of APOE e4 compared to normal controls in E-MCI (NC:E-MCI = 24.4%:40.7%)14, (NC:E-MCI = 18.9%:17.5%)6 and SMI (NC:SMI = 21%:29%)15, (NC:SMI = 15%:22%)5, (NC:SMI = 22.2%:26.8%)16 in Western countries, and in China (NC:SMI = 7.3%:14.7%)7. However, the results have been inconsistent, possibly due to the relatively small and varying sample sizes. In the present study, we confirmed that the frequency of the APOE e3/e4 genotype in the E-aMCI and SMI groups was significantly higher than in normal controls, indicating that people with an early stage of objective memory impairment or with subjective memory complaints may be at increased risk for AD.
AD prevalence increases exponentially as age increases, so dementia factors have a high age distribution, while the controls belong to a lower age group that is not yet at risk of dementia, so it may seem that the control groups have lower APOE e4 prevalence. As outlined in previous studies, various methods have been used for the application of age distribution, including Bayesian probabilities and Gompertz Law33,34,35. Therefore, for the association between APOE genotype and disease stage, taking into account the confounding effect of age distribution within the disease stage groups in our study, we stratified the data by age group and applied the Cochran–Mantel–Haenszel (CMH) test (Supplemental Table S1). Following this (Supplemental Table S1), we found almost consistent outcomes with the previous results without consideration for age (Table 3) other than the comparison of the APOE e3/e3 and e3/e4 genotypes between E-aMCI and controls.
Interestingly, we found no significant difference in the frequency of the APOE e3/e3 vs. e3/e4 genotypes between the E-aMCI and SMI groups (Table 3). To our knowledge, only one study has reported on the comparison of the APOE e4 frequency between patients with early MCI (17.5%) and SMI (19.8%)6. This study found that the two groups did not differ in the frequency of the APOE e4, which is consistent with our results. However, this previous study had some limitations, as they focused on an AD biomarker using neuroimaging and neuropsychological tests, rather than a genetic test, and as they partially enrolled participants for the study of APOE e4, the sample size was smaller than for our study. There were no significant differences in the frequency of the APOE e4 allele even in the early MCI (17.5%) or SMI (19.8%) groups, compared with the control group (18.9%).
Exactly why there is no significant difference in the APOE e4 genotype between E-aMCI and SMI remains unclear. A previous study suggests that clinically diagnosed aMCI patients might be pathologically heterogeneous36, and it is also known that the presence of anxiety or depression may negatively impact memory performance37. It is possible that E-aMCI group included patients other than the early stage of AD, and therefore the subjects with E-aMCI performing between 1.0 SD and 1.5 SD below the norm on memory tests have no additional effect on the frequency of the APOE e4 genotype in our data. Furthermore, we cannot exclude the possibility that a categorical definition of E-aMCI as a minimal impairment is unsuitable to detect individuals at the earliest AD stages. Based on our results, it remains unclear whether SMI and E-aMCI can be clearly separated, and thus these two groups could be considered to be a continuum in the middle stage between normal cognition and MCI.
Nevertheless, our finding may have important clinical implications. The results of the frequency of APOE e4 is comparable among patients with E-aMCI and SMI suggesting that subjective complaints, even in the absence of objective impairment, may be a precise indicator of early disease-related changes as much as a single time point measurement of minimal memory impairment. Our suggestion is supported by a previous study showing that SMI and E-aMCI are associated with a similarly increased risk of AD dementia6. Previous studies have also suggested that subjective complaints are associated with the future development of dementia10,11,12,13,38. Overall, our data strengthens the importance of the subjective experience of memory impairment in dementia prediction.
Another major finding was that APOE e4 genotyping is one of the most predictive factors of cognitive decline from SMI to L-aMCI while once patients progress to clinically manifest AD, the effects of APOE e4 genotyping disappeared. Our findings were consistent with previous studies showing that APOE e4 genotype is the most important genetic risk factor for developing AD39. However, after patients progress to clinically manifest dementia, the effects of APOE e4 genotype are less clear40. Furthermore, a previous study showed that APOE e4 non-carriers with AD dementia have more amyloid burdens than carriers41 although many studies have shown that APOE e4 carriers more amyloid burdens than non-carriers in participants with normal cognition and MCI42. Our findings of the APOE e4 non-carriers on more rapid cognitive decline in AD might be explained by APOE e4 carriers having less brain reserve. That is, since pathology in APOE e4 non-carriers is more severe than in APOE e4 carriers after AD has developed, there is much less substrate remaining to function as a reserve43,44. Therefore, the insufficient reserve in APOE e4 non-carriers contributes towards accelerated deterioration of AD45,46,47.
We note some limitations to our findings. Our patients were selected from a single center, which may limit the generalizability of the findings, and we used a cross-sectional study design. In addition, the study lacks CSF, blood biomarker and imaging data. Further longitudinal and multi-center prospective studies are needed to better understand the actual risk of developing AD and the rate of disease progression in the AD spectrum for participants with or without APOE e4.
In conclusion, we found that E-aMCI and SMI are associated with a similarly increased frequency of the APOE e4 allele, suggesting a greater genetic risk for AD and the importance of monitoring the allele more closely.
Data availability
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy restriction.
References
Corder, E. H. et al. Gene dose of apolipoprotein E type 4 allele and the risk of Alzheimer’s disease in late onset families. Science261, 921–923 (1993).
Bertram, L., Lill, C. M. & Tanzi, R. E. The genetics of Alzheimer disease: Back to the future. Neuron68, 270–281 (2010).
Strittmatter, W. J. et al. Apolipoprotein E: High-avidity binding to beta-amyloid and increased frequency of type 4 allele in late-onset familial Alzheimer disease. Proc. Natl. Acad. Sci. USA90, 1977–1981 (1993).
Rocchi, A., Pellegrini, S., Siciliano, G. & Murri, L. Causative and susceptibility genes for Alzheimer’s disease: A review. Brain Res. Bull.61, 1–24 (2003).
van der Flier, W. M. et al. Distribution of APOE genotypes in a memory clinic cohort. Dement. Geriatr. Cogn. Disord.25, 433–438 (2008).
Jessen, F. et al. AD dementia risk in late MCI, in early MCI, and in subjective memory impairment. Alzheimers Dement.10, 76–83 (2014).
Wang, X., Wang, H., Li, H., Li, T. & Yu, X. Frequency of the apolipoprotein E epsilon4 allele in a memory clinic cohort in Beijing: A naturalistic descriptive study. PLoS One9, e99130 (2014).
Aisen, P. S. et al. Clinical core of the Alzheimer’s disease neuroimaging initiative: Progress and plans. Alzheimers Dement.6, 239–246 (2010).
Stewart, R. Subjective cognitive impairment. Curr. Opin. Psychiatry25, 445–450 (2012).
Jonker, C., Geerlings, M. I. & Schmand, B. Are memory complaints predictive for dementia? A review of clinical and population-based studies. Int. J. Geriatr. Psychiatry15, 983–991 (2000).
Geerlings, M. I., Jonker, C., Bouter, L. M., Ader, H. J. & Schmand, B. Association between memory complaints and incident Alzheimer’s disease in elderly people with normal baseline cognition. Am. J. Psychiatry156, 531–537 (1999).
Jessen, F. et al. Prediction of dementia by subjective memory impairment: Effects of severity and temporal association with cognitive impairment. Arch. Gen. Psychiatry67, 414–422 (2010).
Reisberg, B., Shulman, M. B., Torossian, C., Leng, L. & Zhu, W. Outcome over seven years of healthy adults with and without subjective cognitive impairment. Alzheimers Dement.6, 11–24 (2010).
Risacher, S. L. et al. The role of apolipoprotein E (APOE) genotype in early mild cognitive impairment (E-MCI). Front. Aging Neurosci.5, 11 (2013).
Peter, J. et al. Gray matter atrophy pattern in elderly with subjective memory impairment. Alzheimers Dement.10, 99–108 (2014).
Striepens, N. et al. Interaction effects of subjective memory impairment and ApoE4 genotype on episodic memory and hippocampal volume. Psychol. Med.41, 1997–2006 (2011).
McKhann, G. et al. Clinical diagnosis of Alzheimer’s disease: Report of the NINCDS-ADRDA Work Group under the auspices of Department of Health and Human Services Task Force on Alzheimer’s Disease. Neurology34, 939–944 (1984).
Petersen, R. C. et al. Mild cognitive impairment: Clinical characterization and outcome. Arch Neurol. 56, 303–308 (1999).
Kang, Y. & Na, D. L. Seoul Neuropsychological Screening Battery (SNSB) (Human Brain Research & Consulting Co., Seoul, 2003).
Ahn, H. J. et al. Seoul Neuropsychological Screening Battery-dementia version (SNSB-D): A useful tool for assessing and monitoring cognitive impairments in dementia patients. J. Korean Med. Sci.25, 1071–1076 (2010).
Kang, S. H. et al. The cortical neuroanatomy related to specific neuropsychological deficits in Alzheimer’s Continuum. Dement Neurocogn Disord.18, 77–95. https://doi.org/10.12779/dnd.12019.12718.12773.12777 (2019) ((Epub 12019 Oct 12772)).
Kim, H. & Na, D. L. Normative data on the Korean version of the Boston Naming Test. J. Clin. Exp. Neuropsychol.21, 127–133 (1999).
Hong, Y. J. et al. APOE epsilon4 allele status in korean dementia patients with severe white matter hyperintensities. J. Alzheimers Dis.24, 519–524. https://doi.org/10.3233/JAD-2011-101611 (2011).
Kim, K. W. et al. Association between apolipoprotein E polymorphism and Alzheimer’s disease in Koreans. Neurosci. Lett.277, 145–148 (1999).
Park, H. K. et al. Clinical characteristics of a nationwide hospital-based registry of mild-to-moderate Alzheimer’s disease patients in Korea: A CREDOS (Clinical Research Center for Dementia of South Korea) study. J. Korean Med. Sci.26, 1219–1226 (2011).
Wang, P. N., Hong, C. J., Lin, K. N., Liu, H. C. & Chen, W. T. APOE epsilon4 increases the risk of progression from amnestic mild cognitive impairment to Alzheimer’s disease among ethnic Chinese in Taiwan. J. Neurol. Neurosurg. Psychiatry82, 165–169 (2011).
Herukka, S. K. et al. CSF Abeta42, Tau and phosphorylated Tau, APOE epsilon4 allele and MCI type in progressive MCI. Neurobiol. Aging28, 507–514 (2007).
Blom, E. S. et al. Rapid progression from mild cognitive impairment to Alzheimer’s disease in subjects with elevated levels of tau in cerebrospinal fluid and the APOE epsilon4/epsilon4 genotype. Dement. Geriatr. Cogn. Disord.27, 458–464 (2009).
Norberg, J. et al. Regional differences in effects of APOE epsilon4 on cognitive impairment in non-demented subjects. Dement. Geriatr. Cogn. Disord.32, 135–142 (2011).
Ward, A. et al. Prevalence of apolipoprotein E4 genotype and homozygotes (APOE e4/4) among patients diagnosed with Alzheimer’s disease: A systematic review and meta-analysis. Neuroepidemiology38, 1–17 (2012).
Corbo, R. M. & Scacchi, R. Apolipoprotein E (APOE) allele distribution in the world. Is APOE*4 a “thrifty” allele?. Ann. Human Genet.63, 301–310 (1999).
Mattsson, N. et al. Prevalence of the apolipoprotein E epsilon4 allele in amyloid beta positive subjects across the spectrum of Alzheimer’s disease. Alzheimers Dement.14, 913–924. https://doi.org/10.1016/j.jalz.2018.1002.1009 (2018) ((Epub 2018 Mar 1028)).
Yesavage, J. A. et al. Modeling the prevalence and incidence of Alzheimer’s disease and mild cognitive impairment. J. Psychiatr. Res.36, 281–286. https://doi.org/10.1016/s0022-3956(1002)00020-00021 (2002).
Jorm, A. F. & Jolley, D. The incidence of dementia: A meta-analysis. Neurology51, 728–733. https://doi.org/10.1212/wnl.1251.1213.1728 (1998).
Raber, J., Huang, Y. & Ashford, J. W. ApoE genotype accounts for the vast majority of AD risk and AD pathology. Neurobiol. Aging25, 641–650 (2004).
Petersen, R. C. Mild cognitive impairment as a diagnostic entity. J. Intern. Med.256, 183–194 (2004).
Kizilbash, A. H., Vanderploeg, R. D. & Curtiss, G. The effects of depression and anxiety on memory performance. Arch. Clin. Neuropsychol.17, 57–67 (2002).
St John, P. & Montgomery, P. Are cognitively intact seniors with subjective memory loss more likely to develop dementia?. Int. J. Geriatr. Psychiatry17, 814–820 (2002).
Farrer, L. A. et al. Effects of age, sex, and ethnicity on the association between apolipoprotein E genotype and Alzheimer disease—a meta-analysis. J. Am. Med. Assoc.278, 1349–1356 (1997).
Cosentino, S. et al. APOE epsilon 4 allele predicts faster cognitive decline in mild Alzheimer disease. Neurology70, 1842–1849 (2008).
Ossenkoppele, R. et al. Differential effect of APOE genotype on amyloid load and glucose metabolism in AD dementia. Neurology80, 359–365 (2013).
Jansen, W. J. et al. Prevalence of cerebral amyloid pathology in persons without dementia: A meta-analysis. JAMA313, 1924–1938 (2015).
Stern, Y. Cognitive reserve in ageing and Alzheimer’s disease. Lancet Neurol.11, 1006–1012 (2012).
Stern, Y. Cognitive reserve. Neuropsychologia47, 2015–2028 (2009).
Wilson, R. S. et al. Premorbid reading activity and patterns of cognitive decline in Alzheimer disease. Arch. Neurol.57, 1718–1723 (2000).
Stern, Y., Albert, S., Tang, M. X. & Tsai, W. Y. Rate of memory decline in AD is related to education and occupation: Cognitive reserve?. Neurology53, 1942–1947 (1999).
Scarmeas, N., Albert, S. M., Manly, J. J. & Stern, Y. Education and rates of cognitive decline in incident Alzheimer’s disease. J. Neurol. Neurosurg. Psychiatry77, 308–316 (2006).
Acknowledgements
This research was supported by the Brain Research Program of the National Research Foundation (NRF) funded by the Ministry of Science & ICT (NRF-2018M3C7A1056512), the National Research Council of Science & Technology (NST) grant by the Korea government (MSIP) (No. CRC-15-04-KIST), and a fund (2018-ER6203-02) by Research of Korea Centers for Disease Control and Prevention, a grant of the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI) funded by the Ministry of Health & Welfare, Republic of Korea (grant number: HI18C1159), and funded by the Ministry of Education (NRF-2018R1D1A1B07049386).
Author information
Authors and Affiliations
Contributions
The first co-authors, H.C. and Y.-E.K. have made contribution to design of the article, interpretation of genetic data, analysis of clinical information and co-writing the article. Co-authors, W.C., K.W.K., H.J.K., J.-W.K., and D.L.N. contributed to enrollment of patients and provided help gathering clinical and laboratory information. Corresponding authors, S.W.S. and C.-S.K. have contributed to supervise all process of the research and revised the article.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Cho, H., Kim, YE., Chae, W. et al. Distribution and clinical impact of apolipoprotein E4 in subjective memory impairment and early mild cognitive impairment. Sci Rep 10, 13365 (2020). https://doi.org/10.1038/s41598-020-69603-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-69603-w
This article is cited by
-
Recent Advances Towards Diagnosis and Therapeutic Fingerprinting for Alzheimer’s Disease
Journal of Molecular Neuroscience (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.