Abstract
Vancomycin-resistant Staphylococcus aureus (VRSA), Vancomycin-intermediate S. aureus (VISA) and heterogeneous VISA (hVISA) are subject to vancomycin treatment failure. The aim of the present study was to determine their precise prevalence and investigate prevalence variability depending on different years and locations. Several international databases including Medline (PubMed), Embase and Web of Sciences were searched (data from 1997 to 2019) to identify studies that addressed the prevalence of VRSA, VISA and hVISA among human clinical isolates around the world. Subgroup analyses and meta-regression were conducted to indicate potential source of variation. Publication bias was assessed using Egger’s test. Statistical analyses were conducted using STATA software (version 14.0). Data analysis showed that VRSA, VISA and hVISA isolates were reported in 23, 50 and 82 studies, with an overall prevalence of 1.5% among 5855 S. aureus isolates, 1.7% among 22,277 strains and 4.6% among 47,721 strains, respectively. The overall prevalence of VRSA, VISA, and hVISA before 2010 was 1.2%, 1.2%, and 4%, respectively, while their prevalence after this year has reached 2.4%, 4.3%, and 5.3%. The results of this study showed that the frequency of VRSA, VISA and hVISA after 2010 represent a 2.0, 3.6 and 1.3-fold increase over prior years. In a subgroup analysis of different strain origins, the highest frequency of VRSA (3.6%) and hVISA (5.2%) was encountered in the USA while VISA (2.1%) was more prevalent in Asia. Meta-regression analysis showed significant increasing of VISA prevalence in recent years (p value ≤ 0.05). Based on the results of case reports (which were not included in the calculations mentioned above), the numbers of VRSA, VISA and hVISA isolates were 12, 24 and 14, respectively, among different continents. Since the prevalence of VRSA, VISA and hVISA has been increasing in recent years (especially in the Asian and American continents), rigorous monitoring of vancomycin treatment, it’s the therapeutic response and the definition of appropriate control guidelines depending on geographical regions is highly recommended and essential to prevent the further spread of vancomycin-resistant S. aureus.
Similar content being viewed by others
Introduction
Staphylococcus aureus is a common pathogen that causes various community and hospital-acquired diseases, including endocarditis, wound abscesses, osteomyelitis, skin and soft tissue infections, pneumonia and toxin-mediated syndromes in both healthy people and those with underlying illnesses1,2. Over the past 20 years, this bacterial species has developed resistance to many antibiotics, beta-lactams in particular3,4. During the seventies of the previous century, reports indicated that in the USA there was a significant increase in the morbidity and health care-associated costs, caused by methicillin-resistant S. aureus (MRSA)4. Currently, MRSA is endemic in hospitals around the world and the emergence of community-associated (CA) MRSA has added another serious concern5. Vancomycin, the first glycopeptide antibiotic to be discovered, provides one of the empiric therapies and still is a mainstay for treatment of MRSA infections2. In 1997, the first Vancomycin Intermediate S. aureus (VISA) with Minimum Inhibitory Concentration (MIC) of 8 μg/ml, was reported from Japan6. In 2002, the first case of Vancomycin-resistant S. aureus (VRSA) was reported in a diabetic patient in the USA7. Previously, in vitro studies suggested the existence of various mechanisms for vancomycin resistance in MRSA, the main one being the decreased permeability and the increased thickness of the cell wall and hence a decreased availability of vancomycin for intracellular target molecules. Another type of resistance was caused by plasmid-mediated vancomycin resistance genes (vanA, vanB, vanD, vanE, vanF, and vanG) which may have been transferred from enterococcal species6,8,9,10. Besides, a recent study has shown that VISA growth rate is lower and that the cells harbor a thicker cell wall than those fully susceptible.9,11. Heterogeneous VISA (hVISA) show MICs in the susceptible range (≤ 2 μg/mL), but they contain a sub-population that expresses a resistant phenotype12,13. Infections caused by VISA and hVISA lead to higher rates of vancomycin treatment failure and are associated with extended hospitalization, higher risk of persistent infection, and elevated treatment costs13,14. Despite a published systematic review and meta-analysis study on the prevalence VISA and hVISA15 5 years ago, there has not been published a comprehensive study on the prevalence VRSA, VISA and hVISA worldwide, yet. In the present systematic review and meta-analysis, we pooled published studies that reported the prevalence of VRSA, VISA and hVISA. The findings of the current study will more precisely define the current epidemiology of VRSA, VISA and hVISA and may help to develop more appropriate antibiotic stewardship policies to combat vancomycin resistance.
Methods
Search strategy
A comprehensive systematic literature search was performed in Medline (via PubMed), Embase, and Web of Science databases for original research articles published from 1997 until September 2019. The following terms were applied in our search strategy: Staphylococcus aureus, S. aureus, Vancomycin Resistant Staphylococcus aureus, Vancomycin Resistant S. aureus, VRSA, Vancomycin Intermediate Staphylococcus aureus, Vancomycin Intermediate S. aureus, VISA, heterogeneous Vancomycin Intermediate Staphylococcus aureus, heterogeneous Vancomycin Intermediate S. aureus and hVISA. We also searched the bibliographies of relevant articles to identify additional studies.
Inclusion and exclusion criteria
All original human studies on the prevalence of VRSA, VISA and hVISA among clinical S. aureus isolates that reported sufficient data (including prevalence, evaluation methods, and country of origin) were assessed5,12,13,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96,97,98,99,100,101,102,103,104,105,106,107,108,109,110,111,112,113,114,115,116,117,118,119,120,121,122,123,124,125,126,127,128,129,130,131,132,133,134,135,136,137,138,139,140,141,142,143,144,145,146,147,148,149,150,151,152,153,154,155,156,157,158,159,160,161,162,163,164,165,166,167,168,169,170,171,172,173,174,175,176,177,178,179,180,181,182,183,184,185,186,187,188,189,190,191,192,193,194,195,196,197. Titles, abstracts and full texts of the recorded studies were checked based on the inclusion and exclusion criteria. The exclusion criteria were: (1) animal research only, (2) studies considering vancomycin-resistant bacteria beyond S. aureus, (3) reviews, (4) abstracts presented in conferences, and (5) duplicate studies. Two of the authors (AS and MT) evaluated all studies based on inclusion and exclusion criteria and selected the appropriate papers.
Data extraction and definitions
The following items were extracted from each included study: the last name of the first author, study years, time of publication, country, number of VRSA, VISA and hVISA, number of patients with staphylococcal infection, phenotypic methods used, genotypic identification methods applied and the sample source. Data were collected by two independent examiners and verified by another researcher. According to the CLSI, the definition of VRSA, VISA and hVISA in S. aureus isolates with reduced susceptibility to vancomycin is MIC ≥ 16 μg/mL, MIC of 4–8 μg/mL; and MIC of 1–2 μg/mL, respectively. Furthermore, articles before 2006 used the old definition of VRSA and VISA (VRSA, MIC ≥ 32 μg/mL; VISA, MIC of 8–16 μg/mL)198.
Quality assessment
All reviewed articles were evaluated for quality (according to guidelines developed by the Joanna Briggs Institute), and only high-quality articles that met those rules were included199.
Meta-analysis
Statistical analysis was conducted with STATA software, version 14.0 (Stata Corporation, College Station, Texas, USA) to report the global prevalence of VRSA, VISA and hVISA isolated from human clinical samples. The data were pooled using the fixed-effects (FEM)200 and the random-effects model (REM). Subgroup analyses were conducted based on the type of isolates, publication year and geographic areas (continent/countries). Statistical heterogeneity was evaluated using the Q-test and the I2 statistical methods201. P value < 0.1 was regarded as statistically-significant202. To assess possible publication bias, we calculated the Egger’s test.
Meta-regression analysis
We evaluated whether the prevalence of VRSA, VISA and hVISA changed over time by performing restricted maximum likelihood (REML) random effect meta-regression analysis based on publication year as the moderator. A p value less than 0.05 (p value ≤ 0.05) was considered statistically significant.
Results
Characteristics of included studies
In total, 3200 citations were recorded in the initial database searches. Since we collected data from three databases, many duplicate studies were included. After removing 975 duplicates, titles and abstracts of 2225 articles were checked and 1418 irrelevant studies not meeting the Briggs Institute rules were excluded from our review. In the next screening, 477 non-relevant studies were removed upon reading the full text. In the end, 155 articles were included in the final analysis (Fig. 1 shows a flow chart).
The prevalence of VRSA, VISA and hVISA isolates among human clinical isolates
Out of 155 articles that reported the prevalence of VRSA, VISA and hVISA, 89 studies were from Asia, 22 from Europe, 31 from America, 9 from Africa and 4 from Oceania (Table 1). Data analysis showed that VRSA, VISA and hVISA isolates were reported in 23, 50 and 82 studies, with an overall prevalence of 1.5% [(95% CI) 1.0–2.0] among 5855 S. aureus isolates, 1.7% [(95% CI) 1.3–2.0] among 22,277 strains and 4.6% [(95% CI) 4.1–5.1] among 47,721 strains, respectively (Table 2).
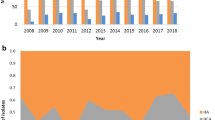
The prevalence of VRSA, VISA and hVISA in two study periods
To analyze the trends for changes in the prevalence of VRSA, VISA and hVISA in more recent years, we performed a subgroup analysis for two periods (before 2010 and 2010–2019) (Table 2, Fig. 2). The prevalence of VRSA, VISA and hVISA gradually increased. Before 2010, the prevalence was 1.2% (95% CI 0.5–1.8) among 2444 S. aureus isolates, 1.2% (95% CI 0.9–1.5) among 18,469 isolates and 4.0 (95% CI 2.9–5.0) among 41,190 S. aureus, respectively. Prevalence reached 2.4% (95% CI 1.4–3.5) among 3411 S. aureus isolates, 4.3% (95% CI 3.0–5.7) among 3808 isolates and 5.3% (95% CI 1.8–4.1) among 6531 isolates in 2010–2019, respectively. The changes in VRSA, VISA and hVISA prevalence between periods are presented in Table 2. The results of this review indicate that the frequency of VRSA, VISA and hVISA after 2010 represent a 2.0, 3.6 and 1.3-fold increase over the prior years (Fig. 2).
The prevalence of VRSA, VISA and hVISA on different continents
The prevalence of VRSA was 1.2% (95% CI 0.7–1.8) among 5043 S. aureus isolates in Asia, 1.1% (95% CI 0.0–2.7) among 179 isolates in Europe, 3.6% (95% CI 0.5–6.6) among 140 isolates in America and 2.5% (95% CI 0.1–4.8) among 493 isolates in Africa. There has been no report of VRSA from Oceania (Figs. 3, 4, 5, 6). The results of this review showed that the prevalence of VISA isolates was 2.1% (95% CI 1.6–2.6) among 13,449 S. aureus isolates, 1.8% (95% CI 0.8–2.8) among 2198 isolates, 1.0% (95% CI 0.5–1.4) among 5040 isolates, 1.8% (95% CI 0.1–3.4) among 1072 isolates and 0.6% (95% CI 0.0–1.3) among 518 isolates from Asia, Europe, America, Africa and Oceania, respectively (Figs. 3, 4, 5, 6). Moreover, the prevalence of hVISA in Asia, Europe, America, Africa and Oceania were 4.7% (95% CI 3.9–5.4) among 16,955 S. aureus isolates, 4.4% (95% CI 3.2–5.5) among 14,680 isolates, 5.2% (95% CI 4.3–6.1) among 15,532 isolates, 4.0% (95% CI 0.2–7.8) among 100 isolates and 11.2% (95% CI 8.3–14.1) among 454 isolates, respectively (Figs. 3, 4, 5, 6).
The prevalence of VRSA, VISA and hVISA on different continents based on case reporting
After the meta-analysis of the prevalence of VRSA, VISA and hVISA among human clinical isolates in different continents, we evaluated the frequency of these three types of S. aureus isolates based on case reports published in the mentioned electronic databases. Based on the results of case reports (Supplementry information Table S2) (which were not taken into account during the analyses already mentioned above), the numbers of VRSA, VISA and hVISA isolates were 12, 24 and 14 among different continents. However, most reports have been from Asia and America continents. There has been no report of VRSA isolates in Europe and Oceania. Oceania was the only continent from which there were no case reports on VISA (Figs. 7 and 8).
Meta-regression analysis
The results of meta-regression showed that the prevalence of VISA was significantly increase by increasing published year (p value < 0.05, Supplementry information figure S1). The results of this analysis indicated that by increasing the published year of study, the prevalence of VRSA and hVISA increased, but this increase was statistically non-significant (p value > 0.05; Table 3 and Supplementry information Figure S1).
Discussion
Frequent use of vancomycin as the drug of choice for treatment of infections caused by multidrug-resistant MRSA has putatively led to selection of the is isolates with reduced susceptibility to vancomycin15,203. In this study we report the prevalence of VRSA, VISA and hVISA around the world. The global prevalence of VRSA, VISA and hVISA isolates was 1.5%, 1.7%, and 4.6%, respectively.
In studies mentioned in Supplementry information Table S1, presence of vanA in VRSA strains by PCR showed that 69% (55/79) of the VRSA strains were vanA positive. This elevated rate of vanA in these bacteria indicates that the resistance determinant was possibly acquired from a vancomycin-resistant Enterococcus species or from one of the other vanA positive organisms living in the human gastro-intestinal tract. Absence of vanA in the other isolates suggests that cell wall thickening and possibly vancomycin affinity trapping may be responsible for the development of vancomycin resistance in these isolates19. Furthermore, many studies reported a failure to detect the vanB gene.
Regarding VISA and hVISA strains, although, there is no clear overall genetic explanation for these phenotypes15, the main mechanisms of reduced susceptibility to vancomycin among VISA strains are mutations in cell wall-associated genes (thickened cell wall with an increased number of peptidoglycan layers)204,205, and/or in the ribosomal gene rpoB203. The prolonged usage of vancomycin can lead to changes in cell wall patterning or reduced expression of penicillin-binding proteins. This may accumulate from heterogeneous to selected homogeneous VISA-type resistance203,206. Noteworthy, when the cell wall gets thicker, the vancomycin MIC level increases207,208. Because of enhanced selective pressure, evolution of hVISA/VISA strains is more rapid in the hospital setting than in the community and therefore VISA is considered a more significant clinical problem than VRSA209. Furthermore, the results of meta-regression results showed the prevalence of the VISA was significantly increase over the time compare to the VRSA and hVISA. It seems that the real incidence of hVISA/ VISA strains is much higher than the present reports and hence there is a clear need for the development of new diagnostic methods for detecting hVISA/VISA. This also includes the development for new antimicrobial susceptibility tests (AST). For instance, in several studies, the PAP-AUC gold standard AST method was not used due to its time-consumption and technical difficulty. Other methods such as Disk Diffusion testing are unable to detect and distinguish these strains9. In overall, all studies used the culture-based methods such as E-test, PAP-AUC, broth dilution, and agar dilution. Moreover, some studies beside the culture-based methods, used PCR for detection of resistant-related gene. Since global scale sort of the same type and frequency of methods was used, the differences between developed and developing countries cannot be hypothetically addressed towards the use of different AST systems.
VRSA and/or VISA with resistance to multiple other antibiotics, including β-lactams, have been isolated from livestock animals that highlights the abuse of antibiotic in that sector and the suspected use of antibiotics as a food supplement210,211. The potential reasons for the emergence or detecting more resistant strains during recent years include: more frequent use of vancomycin for treatment of MRSA infections, better use of diagnostics, inadequate surveillance for drug-resistant strains and a possible change in the vancomycin-resistance breakpoints since 2006212,213.
The prevalence of VRSA in Asia, Europe, America and Africa was 1.2%, 1.1%, 3.6% and 2.5%, respectively. By the way, 65 strains of VRSA were found in Asia versus only 5 VRSA in America. The prevalence of VISA in Asia was higher than on the other continents. It should be noted that 67% (327/485) of vancomycin-resistant strains were reported from Iran and India. Therefore, our data shows that the Asian data are biased towards two countries but also that the emergence of VRSA in India and Iran warrants active microbiological surveillance and careful monitoring of vancomycin therapy. There are several factors involved in the higher number of VRSA and a higher prevalence of VISA in Asia, in comparison to Europe/America countries. Most of the Asian countries are developing countries with lower public hygiene standards and different attitudes towards antimicrobial treatments. Furthermore, population density can lead to more MRSA infections through enhanced microbial transmission. Higher vancomycin use for the treatment of infections can play a role as well15.
Previous studies have helped to identify risk factors that may contribute to VISA emergence such as previous MRSA colonization, hemodialysis dependence, long-term use of vancomycin, hospitalization in ICU and use of indwelling devices. There is no clarity on the precise clinical consequences of vancomycin non-susceptibility among S. aureus strains. Although some meta-analyses have addressed the association between elevated vancomycin MICs and worse clinical outcomes214,215, a recent prospective cohort study suggested exactly the opposite216. Previous studies have also demonstrated a correlation between increased vancomycin MICs and daptomycin resistance in VISA isolates217,218. Furthermore, decreased vancomycin susceptibility is associated with increased susceptibility to beta-lactams. Therefore, the combination of vancomycin and beta-lactams can be a good option for treatment of hVISA or VISA infections198,219. On the other hand, those correlated resistances can lead to problems in elucidating the role of the individual resistance marker in disease severity. Since there is an emerging and increasing rate of resistance to vancomycin, thorough monitoring of the success of vancomycin treatment is essential.220. The majority of VRSA strains belonged to same clonal complex (CC) such as CC5 in the USA. Interestingly, there is high prevalence of the CC5 in healthcare settings. Unlike VRSA, hVISA/VISA has been associated with many clones such as CC5, CC8, CC30, and CC45221.
Antibiotics such as trimethoprim-sulfamethoxazole, tetracyclines, fluoroquinolones, and clindamycin are alternative treatment choices for community-acquired MRSA infections. New drugs such as linezolid, daptomycin, tigecycline, and sodium fusidate are suggested for isolates with a vancomycin MIC of greater than 2 μg/mL198. Finally, in order to control the spread of vancomycin resistant staphylococci, contact precautions, disinfection of care equipment and the environment, plus adequate antimicrobial stewardship are highly recommended222,223,224.
References
Abbasian, S. et al. Genotypic characterization of Staphylococcus aureus isolated from a burn centre by using agr, spa and SCCmec typing methods. New Microbes New Infect. 26, 15–19 (2018).
Bamigboye, B. T., Olowe, O. A. & Taiwo, S. S. Phenotypic and molecular identification of vancomycin resistance in clinical Staphylococcus aureus isolates in Osogbo, Nigeria. Eur. J. Microbiol. Immunol. 8, 25–30 (2018).
Shanson, D., Kensit, J. & Duke, R. Outbreak of hospital infection with a strain of Staphylococcus aureus resistant to gentamicin and methicillin. The Lancet 308, 1347–1348 (1976).
Haley, R. W. et al. The emergence of methicillin-resistant Staphylococcus aureus infections in United States hospitals: possible role of the house staff-patient transfer circuit. Ann. Internal Med. 97, 297–308 (1982).
Kim, M.-N., Hwang, S. H., Pyo, Y.-J., Mun, H.-M. & Pai, C. H. Clonal spread of Staphylococcus aureus heterogeneously resistant to vancomycin in a university hospital in Korea. J. Clin. Microbiol. 40, 1376–1380 (2002).
Hiramatsu, K. et al. Methicillin-resistant Staphylococcus aureus clinical strain with reduced vancomycin susceptibility. J. Antimicrob. Chemother 40, 135–136 (1997).
Goldrick, B. First reported case of VRSA in the United States: an alarming development in microbial resistance. Am. J. Nurs. 102, 17 (2002).
Francia, M. V. & Clewell, D. B. Transfer origins in the conjugative Enterococcus faecalis plasmids pAD1 and pAM373: identification of the pAD1 nic site, a specific relaxase and a possible TraG-like protein. Mol. Microbiol. 45, 375–395 (2002).
Tenover, F. C., Biddle, J. W. & Lancaster, M. V. Increasing resistance to vancomycin and other glycopeptides in Staphylococcus aureus. Emerg. Infect. Dis. 7, 327 (2001).
Woodford, N. Epidemiology of the genetic elements responsible for acquired glycopeptide resistance in enterococci. Microbial. Drug Res. 7, 229–236 (2001).
Al-Daghistani, H. I., Shquirat, W., Al-Kharabsha, M. & Al-Latif, S. M. A. Asymptomatic colonization of Staphylococcus aureus with intermediate resistance to vancomycin harboring vanb resistance gene. Asian J. Pharm. Clin. Res. 10, 349–356 (2017).
Chen, H., Liu, Y., Sun, W., Chen, M. & Wang, H. The incidence of heterogeneous vancomycin-intermediate Staphylococcus aureus correlated with increase of vancomycin MIC. Diagn. Microbiol. Infect. Dis. 71, 301–303 (2011).
Charles, P. G., Ward, P. B., Johnson, P. D., Howden, B. P. & Grayson, M. L. Clinical features associated with bacteremia due to heterogeneous vancomycin-intermediate Staphylococcus aureus. Clin. Infect. Dis. 38, 448–451 (2004).
Maor, Y. et al. Clinical features of heteroresistant vancomycin-intermediate Staphylococcus aureus bacteremia versus those of methicillin-resistant S. aureus bacteremia. J. Infect. Dis. 199, 619–624 (2009).
Zhang, S., Sun, X., Chang, W., Dai, Y. & Ma, X. Systematic review and meta-analysis of the epidemiology of vancomycin-intermediate and heterogeneous vancomycin-intermediate Staphylococcus aureus isolates. PLoS ONE 10, e0136082 (2015).
Abdel-Maksoud, M. et al. Methicillin-resistant Staphylococcus aureus recovered from healthcare- and community-associated infections in Egypt. Int. J. Bacteriol. 2016, 5751785. https://doi.org/10.1155/2016/5751785 (2016).
AbdEl-Mongy, M., Awad, E. T. & Mosaed, F. Vancomycin resistance among methicillin resistant Staphylococcus aureus Isolates from neonatal sepsis attending intensive care unit in Shibin El-Kom teaching hospital Egypt. J. Pure Appl. Microbiol. 12, 1093–1100 (2018).
Adam, H. J. et al. Detection and characterization of heterogeneous vancomycin-intermediate Staphylococcus aureus isolates in Canada: results from the Canadian Nosocomial Infection Surveillance Program, 1995–2006. Antimicrob. Agents Chemother. 54, 945–949. https://doi.org/10.1128/aac.01316-09 (2010).
Aligholi, M. et al. Emergence of high-level vancomycin-resistant Staphylococcus aureus in the Imam Khomeini Hospital in Tehran. Med. Principles Pract. 17, 432–434 (2008).
Al-Obeid, S., Haddad, Q., Cherkaoui, A., Schrenzel, J. & Francois, P. First detection of an invasive Staphylococcus aureus strain (D958) with reduced susceptibility to glycopeptides in Saudi Arabia. J. Clin. Microbiol. 48, 2199–2204 (2010).
Alzolibani, A. A. et al. Documentation of vancomycin-resistant Staphylococcus aureus (VRSA) among children with atopic dermatitis in the Qassim region, Saudi Arabia. Acta Dermatovenerol Alp Pannonica Adriat 21, 51–53 (2012).
Amod, F. et al. Ventriculitis due to a hetero strain of vancomycin intermediate Staphylococcus aureus (hVISA): successful treatment with linezolid in combination with intraventricular vancomycin. J. Infect. 50, 252–257 (2005).
Andrade-Baiocchi, S., Tognim, M. C. B., Baiocchi, O. C. & Sader, H. S. Endocarditis due to glycopeptide-intermediate Staphylococcus aureus: case report and strain characterization. Diagn. Microbiol. Infect. Dis. 45, 149–152 (2003).
Anvari, M., Ranji, N. & Khoshmaslak, F. Antibacterial susceptibility of three vancomycin-resistant Staphylococcus aureus Strain Isolated from Nor thern Part of Iran. J. Pure Appl. Microbiol. 6, 671–675 (2012).
Ariza, J. & Pujol, M. Vancomycin in surgical infections due to meticillin-resistant Staphylococcus aureus with heterogeneous resistance to vancomycin. The Lancet 353, 1587–1588 (1999).
Asadpour, L. & Ghazanfari, N. Detection of vancomycin nonsusceptible strains in clinical isolates of Staphylococcus aureus in northern Iran. Int. Microbiol. 22, 411 (2019).
Avery, L. M., Steed, M. E., Woodruff, A. E., Hasan, M. & Rybak, M. J. Daptomycin-nonsusceptible vancomycin-intermediate Staphylococcus aureus vertebral osteomyelitis cases complicated by bacteremia treated with high-dose daptomycin and trimethoprim-sulfamethoxazole. Antimicrob. Agents Chemother. 56, 5990–5993 (2012).
Azimian, A. et al. Genetic characterization of a vancomycin-resistant Staphylococcus aureus isolate from the respiratory tract of a patient in a university hospital in northeastern Iran. J. Clin. Microbiol. 50, 3581–3585 (2012).
Backo, M., Gaenger, E., Burkart, A., Chai, Y. L. & Bayer, A. S. Treatment of experimental staphylococcal endocarditis due to a strain with reduced susceptibility in vitro to vancomycin: efficacy of ampicillin-sulbactam. Antimicrob. Agents Chemother. 43, 2565–2568 (1999).
Bakthavatchalam, Y. D., Ralph, R., Veeraraghavan, B., Babu, P. & Munusamy, E. Evidence from an In Vitro Study: Is Oxacillin Plus Vancomycin a Better Choice for Heteroresistant Vancomycin-Intermediate Staphylococcus aureus?. Infect. Dis. Ther. 8, 51–62. https://doi.org/10.1007/s40121-018-0224-z (2019).
Balkhair, A., Al Muharrmi, Z., Darwish, L., Farhan, H. & Sallam, M. Treatment of vancomycin-intermediate Staphylococcus aureus (VISA) endocarditis with linezolid. Int. J. Infect. Dis 14, e227–e229 (2010).
Bamigboye, B. T., Olowe, O. A. & Taiwo, S. S. Phenotypic and molecular identification of vancomycin resistance in clinical Staphylococcus aureus isolates in Osogbo Nigeria. Eur. J. Microbiol. Immunol. (Bp) 8, 25–30. https://doi.org/10.1556/1886.2018.00003 (2018).
Banerjee, T. & Anupurba, S. Colonization with vancomycin-intermediate Staphylococcus aureus strains containing the vanA resistance gene in a tertiary-care center in north India. J. Clin. Microbiol. 50, 1730–1732. https://doi.org/10.1128/jcm.06208-11 (2012).
Bataineh, H. A. Resistance of staphyiococcus aureus to vancomycin in Zarqa Jordan. Pak. J. Med. Sci. 22, 144 (2006).
Baxi, S. M., Chan, D. & Jain, V. Daptomycin non-susceptible, vancomycin-intermediate Staphylococcus aureus endocarditis treated with ceftaroline and daptomycin: case report and brief review of the literature. Infection 43, 751–754 (2015).
Bert, F. et al. Prevalence, molecular epidemiology, and clinical significance of heterogeneous glycopeptide-intermediate Staphylococcus aureus in liver transplant recipients. J. Clin. Microbiol. 41, 5147–5152 (2003).
Beydoun, K. & Wenzel, R. Left ventricular assist device endocarditis caused by vancomycin-intermediate Staphylococcus aureus successfully treated with ceftaroline: a review of the clinical case and overview of vancomycin resistance in Staphylococcus aureus. Clin. Microb.Newslett. 35, 171–176 (2013).
Bhowmick, T., Liu, C., Imp, B., Sharma, R. & Boruchoff, S. E. Ceftaroline as salvage therapy for complicated MRSA bacteremia: case series and analysis. Infection 47(4), 629–635 (2019).
Bierbaum, G., Fuchs, K., Lenz, W., Szekat, C. & Sahl, H.-G. Presence of Staphylococcus aureus with reduced susceptibility to vancomycin in Germany. Eur. J. Clin. Microbiol. Infect. Dis. 18, 691–696 (1999).
Bobin-Dubreux, S. et al. Clinical isolate of Vancomycin-heterointermediatestaphylococcus aureus susceptible to methicillin and in vitro selection of a vancomycin-resistant derivative. Antimicrob. Agents Chemother. 45, 349–352 (2001).
Cafiso, V. et al. Methicillin resistance and vancomycin heteroresistance in Staphylococcus aureus in cystic fibrosis patients. Eur. J. Clin. Microbiol. Infect. Dis. 29, 1277–1285. https://doi.org/10.1007/s10096-010-1000-5 (2010).
Campanile, F. et al. Heteroresistance to glycopeptides in Italian meticillin-resistant Staphylococcus aureus (MRSA) isolates. Int. J. Antimicrob. Agents 36, 415–419. https://doi.org/10.1016/j.ijantimicag.2010.06.044 (2010).
Cartolano, G. L., Cheron, M., Benabid, D., Leneveu, M. & Boisivon, A. Methicillin-resistant Staphylococcus aureus (MRSA) with reduced susceptibility to glycopeptides (GISA) in 63 French general hospitals. Clin. Microbiol. Infect. 10, 448–451. https://doi.org/10.1111/j.1469-0691.2004.00830.x (2004).
Casapao, A. M. et al. Evaluation of vancomycin population susceptibility analysis profile as a predictor of outcomes for patients with infective endocarditis due to methicillin-resistant Staphylococcus aureus. Antimicrob. Agents Chemother. 58, 4636–4641. https://doi.org/10.1128/aac.02820-13 (2014).
Cha, H. Y., Kim, H. O., Jin, J. S. & Lee, J. C. Emergence of vancomycin-intermediate Staphylococcus aureus from predominant methicillin-resistant S. aureus clones in a Korean hospital. J. Microbiol. 48, 533–535 (2010).
Chaiwongkarjohn, S. et al. The first case of vancomycin-intermediate Staphylococcus aureus in Hawai’i. Hawaii Med. J. 68, 189 (2009).
Chaiwongkarjohn, S. et al. A report on the first case of vancomycin-intermediate Staphylococcus aureus (VISA) in Hawai ‘i. Hawaii Med. J. 70, 233 (2011).
Chang, S. et al. Infection with vancomycin-resistant Staphylococcus aureus containing the vanA resistance gene. N. Engl. J. Med. 348, 1342–1347 (2003).
Chaudhari, C. et al. Heterogeneous vancomycin-intermediate among methicillin resistant Staphylococcus aureus. Med. J. Armed Forces India 71, 15–18 (2015).
Chaudhary, M. & Payasi, A. Prevalence of heterogeneous glycopeptide intermediate resistance in Methicillin-Resistant Staphylococcus aureus. Am. J. Infect. Dis. 9, 63 (2013).
Chaudhary, M. & Payasi, A. Vancoplus kinetic study in vancomycin resistant Staphylococcus aureus. Int. J. Pharm. Sci. Rev. Res. 31, 135–142 (2015).
Chen, C.-J., Lin, M.-H., Shu, J.-C. & Lu, J.-J. Reduced susceptibility to vancomycin in isogenic Staphylococcus aureus strains of sequence type 59: tracking evolution and identifying mutations by whole-genome sequencing. J. Antimicrob. Chemother. 69, 349–354 (2013).
Chua, T. et al. Molecular epidemiology of methicillin-resistant Staphylococcus aureus bloodstream isolates in urban Detroit. J. Clin. Microbiol. 46, 2345–2352. https://doi.org/10.1128/jcm.00154-08 (2008).
Chung, D. R. et al. Genotype-specific prevalence of heterogeneous vancomycin-intermediate Staphylococcus aureus in Asian countries. Int. J. Antimicrob. Agents 46, 338–341. https://doi.org/10.1016/j.ijantimicag.2015.03.009 (2015).
Chung, G. et al. Nationwide surveillance study of vancomycin intermediate Staphylococcus aureus strains in Korean hospitals from 2001 to 2006. J. Microbiol. Biotechnol. 20, 637–642 (2010).
Claeys, K. C. et al. 2016 Pneumonia caused by methicillin-resistant Staphylococcus aureus: does vancomycin heteroresistance matter? Antimicrob. Agents Chemother. 60, 1708–1716 (2016).
da Costa, T. M. et al. Clinical and microbiological characteristics of heteroresistant and vancomycin-intermediate Staphylococcus aureus from bloodstream infections in a Brazilian teaching hospital. PLoS ONE 11, e0160506. https://doi.org/10.1371/journal.pone.0160506 (2016).
Dedania, V. S., Hale, B. P. & Bhatnagar, P. Endogenous endophthalmitis due to clinically vancomycin-resistant Staphylococcus aureus. Retinal Cases Brief Rep. 9, 59–60 (2015).
Denis, O., Deplano, A., De Ryck, R., Nonhoff, C. & Struelens, M. J. Emergence and spread of gentamicin-susceptible strains of methicillin-resistant Staphylococcus aureus in Belgian hospitals. Microb. Drug. Resist. 9, 61–71. https://doi.org/10.1089/107662903764736355 (2003).
Denis, O. et al. Emergence of vancomycin-intermediate Staphylococcus aureus in a Belgian hospital: microbiological and clinical features. J. Antimicrob. Chemother. 50, 383–391. https://doi.org/10.1093/jac/dkf142 (2002).
Dezfulian, A. et al. Identification and characterization of a high vancomycin-resistant Staphylococcus aureus harboring VanA gene cluster isolated from diabetic foot ulcer. Iran. J. Basic Med. Sci. 15, 803 (2012).
Di Gregorio, S. et al. Clinical, microbiological, and genetic characteristics of heteroresistant vancomycin-intermediate Staphylococcus aureus bacteremia in a teaching hospital. Microb. Drug. Resist. 21, 25–34. https://doi.org/10.1089/mdr.2014.0190 (2015).
Dubey, D. et al. Surveillance of infection status of drug resistant Staphylococcus aureus in an Indian teaching hospital. Asian Pac. J. Trop. Dis. 3, 133–142 (2013).
El Ayoubi, M.-D., Hamze, M., Mallat, H., Achkar, M. & Dabboussi, F. Glycopeptide intermediate Staphylococcus aureus and prevalence of the luk-PV gene in clinical isolates Northern Lebanon. Médecine et Maladies Infectieuses 44, 223–228 (2014).
El-Aziz, N. K. A., El-Hamid, M. I. A., Bendary, M. M., El-Azazy, A. A. & Ammar, A. M. Existence of vancomycin resistance among methicillin resistant S. aureus recovered from animal and human sources in Egypt. Vet. Med. Health Econ. 55, 221 (2018).
ElSayed, N., Ashour, M. & Amine, A. E. K. Vancomycin resistance among Staphylococcus aureus isolates in a rural setting Egypt. Germs 8, 134 (2018).
Fasihi, Y., Kiaei, S. & Kalantar-Neyestanaki, D. Characterization of SCCmec and spa types of methicillin-resistant Staphylococcus aureus isolates from health-care and community-acquired infections in Kerman Iran. J Epidemiol Glob Health 7, 263–267. https://doi.org/10.1016/j.jegh.2017.08.004 (2017).
Fasihi, Y., Saffari, F., Mansouri, S. & Kalantar-Neyestanaki, D. The emergence of vancomycin-resistant Staphylococcus aureus in an intensive care unit in Kerman Iran. Wien Med. Wochenschr. 168, 85–88. https://doi.org/10.1007/s10354-017-0562-6 (2018).
Finks, J. et al. Vancomycin-resistant Staphylococcus aureus, Michigan, USA, 2007. Emerg. Infect. Dis. 15, 943 (2009).
Fitzgibbon, M. M., Rossney, A. S. & O’Connell, B. Investigation of reduced susceptibility to glycopeptides among methicillin-resistant Staphylococcus aureus isolates from patients in Ireland and evaluation of agar screening methods for detection of heterogeneously glycopeptide-intermediate S. aureus. J. Clin. Microbiol. 45, 3263–3269. https://doi.org/10.1128/jcm.00836-07 (2007).
Fong, R. K., Low, J., Koh, T. H. & Kurup, A. Clinical features and treatment outcomes of vancomycin-intermediate Staphylococcus aureus (VISA) and heteroresistant vancomycin-intermediate Staphylococcus aureus (hVISA) in a tertiary care institution in Singapore. Eur. J. Clin. Microbiol. Infect. Dis. 28, 983–987. https://doi.org/10.1007/s10096-009-0741-5 (2009).
Gagliotti, C. et al. Staphylococcus aureus in a northern Italian region: phenotypic and molecular characterization. Scand. J. Infect. Dis. 44, 24–28 (2012).
Gallon, O. et al. Antimicrobial susceptibility profiles of Staphylococcus aureus isolated in 2007 from French patients with bloodstream infections: goodbye hVISA, welcome Geraldine?. J. Antimicrob. Chemother. 65, 1297–1299 (2010).
Gardete, S., Aires-De-Sousa, M., Faustino, A., Ludovice, A. & de Lencastre, H. Identification of the first vancomycin intermediate-resistant Staphylococcus aureus (VISA) isolate from a hospital in Portugal. Microbial. Drug Res. 14, 1–6 (2008).
Garnier, F. et al. A 1 year surveillance study of glycopeptide-intermediate Staphylococcus aureus strains in a French hospital. J Antimicrob. Chemother. 57, 146–149. https://doi.org/10.1093/jac/dki413 (2006).
Gecgel, A. S. K. Vancomycin minimum inhibitory concentration (MIC) creep and its effect on mortality in adult cardiac patients who developed sepsis caused by Staphylococcus aureus and coagulase-negative Staphylococcus. Med. Sci. Tech. 58, 49–55 (2017).
Ghahremani, M., Jazani, N. H. & Sharifi, Y. Emergence of vancomycin-intermediate and -resistant Staphylococcus aureus among methicillin-resistant S. aureus isolated from clinical specimens in the northwest of Iran. J. Glob. Antimicrob. Resist. 14, 4–9. https://doi.org/10.1016/j.jgar.2018.01.017 (2018).
Goud, R. et al. Community prevalence of methicillin and vancomycin resistant Staphylococcus aureus in and around Bangalore, southern India. Rev. Soc. Bras. Med. Trop. 44, 309–312. https://doi.org/10.1590/s0037-86822011005000035 (2011).
Gowrishankar, S., Thenmozhi, R., Balaji, K. & Pandian, S. K. Emergence of methicillin-resistant, vancomycin-intermediate Staphylococcus aureus among patients associated with group a Streptococcal pharyngitis infection in southern India. Infect. Genet. Evol. 14, 383–389. https://doi.org/10.1016/j.meegid.2013.01.002 (2013).
Hafer, C., Lin, Y., Kornblum, J., Lowy, F. D. & Uhlemann, A. C. Contribution of selected gene mutations to resistance in clinical isolates of vancomycin-intermediate Staphylococcus aureus. Antimicrob. Agents Chemother. 56, 5845–5851. https://doi.org/10.1128/aac.01139-12 (2012).
Hageman, J. C. et al. Occurrence of a USA300 vancomycin-intermediate Staphylococcus aureus. Diagn. Microbiol. Infect. Dis. 62, 440–442 (2008).
Hageman, J. C. et al. Vancomycin-intermediate Staphylococcus aureus in a home health-care patient. Emerg. Infect. Dis. 7, 1023 (2001).
Hakim, S., Arshed, S., Iqbal, M. & Javaid, S. Vancomycin sensitivity of Staphylococcus aureus isolates from hospital patients in Karachi Pakistan. Libyan J. Med. 2, 176–179 (2007).
Al-Daghistani, H. I., Atwa, D. S., Al-kharabsha, M. U. & AL-Latif, S. M. Asymptomatic colonization of Staphylococcus aureus with intermediate resistance to vancomycin harboring vanB resistance gene. Pharm. Clin. Res Asian J https://doi.org/10.22159/ajpcr.2017.v10i5.17285 (2017).
Hanaki, H. et al. Antibiotic susceptibility survey of blood-borne MRSA isolates in Japan from 2008 through 2011. J. Infect. Chemother. 20, 527–534. https://doi.org/10.1016/j.jiac.2014.06.012 (2014).
Hanaki, H. et al. Occurrence of vancomycin-intermediate-resistant Staphylococcus aureus in Japan. J. Infect. Chemother. 13, 118–121. https://doi.org/10.1007/s10156-006-0498-z (2007).
Hasan, R., Acharjee, M. & Noor, R. Prevalence of vancomycin resistant Staphylococcus aureus (VRSA) in methicillin resistant S. aureus (MRSA) strains isolated from burn wound infections. Ci Ji Yi Xue Za Zhi 28, 49–53. https://doi.org/10.1016/j.tcmj.2016.03.002 (2016).
Havaei, S. A. et al. Genetic characterization of methicillin resistant and sensitive, vancomycin intermediate Staphylococcus aureus strains isolated from different Iranian Hospitals. ISRN Microbiol. https://doi.org/10.5402/2012/215275 (2012).
Ho, C. M. et al. Prevalence and accessory gene regulator (agr) analysis of vancomycin-intermediate Staphylococcus aureus among methicillin-resistant isolates in Taiwan–SMART program, 2003. Eur. J. Clin. Microbiol. Infect. Dis. 29, 383–389. https://doi.org/10.1007/s10096-009-0868-4 (2010).
Hong, K. H., Park, J. S. & Kim, E.-C. Two cases of vancomycin-intermediate Staphylococcus aureus isolated from joint tissue or wound. Kor. J. Lab. Med. 28, 444–448 (2008).
Horne, K. C. et al. Prospective comparison of the clinical impacts of heterogeneous vancomycin-intermediate methicillin-resistant Staphylococcus aureus (MRSA) and vancomycin-susceptible MRSA. Antimicrob. Agents Chemother. 53, 3447–3452 (2009).
Hsueh, P. R., Lee, S. Y., Perng, C. L., Chang, T. Y. & Lu, J. J. Clonal dissemination of meticillin-resistant and vancomycin-intermediate Staphylococcus aureus in a Taiwanese hospital. Int. J. Antimicrob. Agents 36, 307–312. https://doi.org/10.1016/j.ijantimicag.2010.06.035 (2010).
Hu, J. et al. Reduced vancomycin susceptibility found in methicillin-resistant and methicillin-sensitive Staphylococcus aureus clinical isolates in Northeast China. PLoS ONE 8, e73300. https://doi.org/10.1371/journal.pone.0073300 (2013).
Huang, S. H. et al. Prevalence of vancomycin-intermediate Staphylococcus aureus (VISA) and heterogeneous VISA among methicillin-resistant S. aureus with high vancomycin minimal inhibitory concentrations in Taiwan: a multicenter surveillance study, 2012–2013. J. Microbiol. Immunol. Infect. 49, 701–707. https://doi.org/10.1016/j.jmii.2015.07.003 (2016).
Hubert, S. K. et al. Glycopeptide-intermediate Staphylococcus aureus: evaluation of a novel screening method and results of a survey of selected US hospitals. J. Clin. Microbiol. 37, 3590–3593 (1999).
Islam, T. A. B. & Shamsuzzaman, S. Prevalence and antimicrobial susceptibility pattern of methicillin-resistant, vancomycin-resistant, and Panton-Valentine leukocidin positive Staphylococcus aureus in a tertiary care hospital Dhaka Bangladesh. Tzu Chi. Med. J. 27, 10–14 (2015).
Jahanshahi, A., Zeighami, H. & Haghi, F. Molecular characterization of methicillin and vancomycin resistant Staphylococcus aureus strains isolated from hospitalized patients. Microb. Drug. Resist. https://doi.org/10.1089/mdr.2018.0069 (2018).
Julian, K. et al. Characterization of a daptomycin-nonsusceptible vancomycin-intermediate Staphylococcus aureus strain in a patient with endocarditis. Antimicrob. Agents Chemother. 51, 3445–3448 (2007).
Kang, Y. R. et al. Decreasing prevalence of heterogeneous vancomycin-intermediate Staphylococcus aureus among blood isolates in Korean hospitals. Diagn. Microbiol. Infect. Dis. 86, 464–466. https://doi.org/10.1016/j.diagmicrobio.2016.09.015 (2016).
Khatib, R. et al. Relevance of vancomycin-intermediate susceptibility and heteroresistance in methicillin-resistant Staphylococcus aureus bacteraemia. J. Antimicrob. Chemother. 66, 1594–1599. https://doi.org/10.1093/jac/dkr169 (2011).
Khatib, R. et al. Decreasing prevalence of isolates with vancomycin heteroresistance and vancomycin minimum inhibitory concentrations >/=2 mg/L in methicillin-resistant Staphylococcus aureus over 11 years: potential impact of vancomycin treatment guidelines. Diagn. Microbiol. Infect. Dis. 82, 245–248. https://doi.org/10.1016/j.diagmicrobio.2015.03.014 (2015).
Khosrovaneh, A. et al. Frequency of reduced vancomycin susceptibility and heterogeneous subpopulation in persistent or recurrent methicillin-resistant Staphylococcus aureus bacteremia. Clin. Infect. Dis. 38, 1328–1330 (2004).
Kim, E. S. et al. Clinical and Molecular Characterization of Invasive Heteroresistant Vancomycin-Intermediate Staphylococcus aureus Infections in Korean Hospitals. J. Clin. Microbiol. 54, 760–763. https://doi.org/10.1128/jcm.02595-15 (2016).
Kim, M.-N., Pai, C. H., Woo, J. H., Ryu, J. S. & Hiramatsu, K. Vancomycin-intermediate Staphylococcus aureus in Korea. J. Clin. Microbiol. 38, 3879–3881 (2000).
Kim, T. et al. Phenotypic changes of methicillin-resistant Staphylococcus aureus during vancomycin therapy for persistent bacteraemia and related clinical outcome. Eur. J. Clin. Microbiol. Infect. Dis. 36, 1473–1481. https://doi.org/10.1007/s10096-017-2956-1 (2017).
Kino, H. et al. Central nervous system infection caused by vancomycin-intermediate Staphylococcus aureus (SCCmec type IV, ST8). J. Infect. Chemother. 20, 643–646 (2014).
Kirby, A. et al. Staphylococcus aureus with reduced glycopeptide susceptibility in Liverpool UK. J. Antimicrob. Chemother. 65, 721–724. https://doi.org/10.1093/jac/dkq009 (2010).
Koh, Y. R., Kim, K. H., Chang, C. L. & Yi, J. Prevalence and clinical impact of heterogeneous vancomycin-intermediate Staphylococcus aureus isolated from hospitalized patients. Ann. Lab. Med. 36, 235–243. https://doi.org/10.3343/alm.2016.36.3.235 (2016).
Kosowska-Shick, K. et al. Incidence and characteristics of vancomycin nonsusceptible strains of methicillin-resistant Staphylococcus aureus at Hershey Medical Center. Antimicrob. Agents Chemother. 52, 4510–4513 (2008).
Krzyszton-Russjan, J., Gniadkowski, M., Polowniak-Pracka, H., Hagmajer, E. & Hryniewicz, W. The first Staphylococcus aureus isolates with reduced susceptibility to vancomycin in Poland. J. Antimicrob. Chemother. 50, 1065–1069. https://doi.org/10.1093/jac/dkf252 (2002).
Kumar, M. Multidrug-resistant Staphylococcus aureus, India, 2013–2015. Emerg. Infect. Dis. 22, 1666–1667. https://doi.org/10.3201/eid2209.160044 (2016).
Lee, H.-W. et al. Detection of MecA gene in clinical isolates of Staphylococcus aureus by multiplex-PCR, and antimicrobial susceptibility of MRSA. J. Microbiol. Biotechnol. 13, 354–359 (2003).
Liaqat, F. et al. Isolation identification and control of vancomycin resistant Staphylococcus aureus. Pak. J. Pharm. Sci. 28, 997–1004 (2015).
Limbago, B. M. et al. Report of the 13th vancomycin-resistant Staphylococcus aureus isolate from the United States. J. Clin. Microbiol. 52, 998–1002 (2014).
Lin, S. Y. et al. Molecular epidemiology and clinical characteristics of hetero-resistant vancomycin intermediate Staphylococcus aureus bacteremia in a Taiwan Medical Center. J. Microbiol. Immunol. Infect. 45, 435–441. https://doi.org/10.1016/j.jmii.2012.05.004 (2012).
Liu, C. et al. Molecular characteristics and virulence factors in methicillin-susceptible, resistant, and heterogeneous vancomycin-intermediate Staphylococcus aureus from central-southern China. J. Microbiol. Immunol. Infect. 48, 490–496. https://doi.org/10.1016/j.jmii.2014.03.003 (2015).
Lulitanond, A. et al. The first vancomycin-intermediate Staphylococcus aureus strains isolated from patients in Thailand. J. Clin. Microbiol. 47, 2311–2316 (2009).
Mabed, M. & Marouf, S. Vancomycin-resistant Staphylococcus aureus in a bone marrow transplantation unit. Ann. Hematol. 84, 133–135 (2005).
Maor, Y. et al. Prevalence and characteristics of heteroresistant vancomycin-intermediate Staphylococcus aureus bacteremia in a tertiary care center. J. Clin. Microbiol. 45, 1511–1514. https://doi.org/10.1128/jcm.01262-06 (2007).
Marchese, A., Balistreri, G., Tonoli, E., Debbia, E. & Schito, G. Heterogeneous Vancomycin Resistance in Methicillin-ResistantStaphylococcus aureus Strains Isolated in a Large Italian Hospital. J. Clin. Microbiol. 38, 866–869 (2000).
Martirosov, D. M. et al. Relationship between day 1 and day 2 Vancomycin area under the curve values and emergence of heterogeneous Vancomycin-intermediate Staphylococcus aureus (hVISA) by Etest(R) macromethod among patients with MRSA bloodstream infections: a pilot study. BMC Infect. Dis. 17, 534. https://doi.org/10.1186/s12879-017-2609-0 (2017).
Melo, G. B. et al. Analysis of the genetic diversity of vancomycin-resistant Staphylococcus aureus. Braz. J. Microbiol. 36, 126–130 (2005).
Melo-Cristino, J., Resina, C., Manuel, V., Lito, L. & Ramirez, M. First case of infection with vancomycin-resistant Staphylococcus aureus in Europe. The Lancet 382, 205 (2013).
Mendem, S. K., Alasthimannahalli Gangadhara, T., Shivannavar, C. T. & Gaddad, S. M. Antibiotic resistance patterns of Staphylococcus aureus: A multi center study from India. Microb. Pathog. 98, 167–170. https://doi.org/10.1016/j.micpath.2016.07.010 (2016).
Mirani, Z. A. & Jamil, N. Characterization of a vancomycin intermediate-resistant Staphylococcus aureus isolated from a hospital. J. Coll. Phys. Surg. Pak. 20, 558–559 (2010).
Mirza, H. C., Sancak, B. & Gur, D. The prevalence of vancomycin-intermediate Staphylococcus aureus and heterogeneous VISA among methicillin-resistant strains isolated from pediatric population in a Turkish University Hospital. Microb. Drug. Resist. 21, 537–544. https://doi.org/10.1089/mdr.2015.0048 (2015).
Mlynarczyk, A., Mlynarczyk, G. & Luczak, M. Searching for Staphylococcus aureus strains with reduced susceptibility to glycopeptides among clinical isolates obtained during the year of 2002. Med. Dosw. Mikrobiol. 55, 209–217 (2003).
Monaco, M., Sanchini, A., Grundmann, H. & Pantosti, A. Vancomycin-heteroresistant phenotype in invasive methicillin-resistant Staphylococcus aureus isolates belonging to spa type 041. Eur. J. Clin. Microbiol. Infect. Dis. 29, 771–777. https://doi.org/10.1007/s10096-010-0922-2 (2010).
Muneeri, S. S., Mobaiyen, H. & Mirzaie, H. Study on Vancomycin-resistant Staphylococcus aureus and identification of VanA gene in these strains isolated from Tabriz Shuhada Hospital using e-test and PCR methods. Life Sci. J. 10, 748–752 (2013).
Musta, A. C. et al. Vancomycin MIC plus heteroresistance and outcome of methicillin-resistant Staphylococcus aureus bacteremia: trends over 11 years. J. Clin. Microbiol. 47, 1640–1644. https://doi.org/10.1128/jcm.02135-08 (2009).
Naimi, T. S. et al. Vancomycin-intermediate Staphylococcus aureus with phenotypic susceptibility to methicillin in a patient with recurrent bacteremia. Clin. Infect. Dis. 36, 1609–1612 (2003).
Najar-Peerayeh, S., Mirzaee, M. & Behmanesh, M. Molecular characterization of vancomycin-intermediate Staphylococcus aureus isolates from Tehran. Asian Pac. J. Trop. Dis. 6, 726–731 (2016).
Neetu, T. J. P. & Murugan, S. Genotyping of methicillin resistant Staphylococcus aureus from tertiary care hospitals in Coimbatore, South India. J. Glob. Infect. Dis. 8, 68 (2016).
Neoh, H.-M. et al. Impact of reduced vancomycin susceptibility on the therapeutic outcome of MRSA bloodstream infections. Ann. Clin. Microbiol. Antimicrob. 6, 13 (2007).
Nonhoff, C., Denis, O. & Struelens, M. Low prevalence of methicillin-resistant Staphylococcus aureus with reduced susceptibility to glycopeptides in Belgian hospitals. Clin. Microbiol. Infect. 11, 214–220 (2005).
Norazah, A., Law, N. L., Kamel, A. G. & Salbiah, N. The presence of heterogeneous vancomycin-lntermediate Staphylococcus aureus (heteroVISA) in a major Malaysian hospital. Med. J. Malaysia 67, 269–273 (2012).
Oguz, V. A., Kose, H., Yapar, N., Karatosun, V. & Gulay, Z. Heteroresistant vancomycin intermediate S. aureus (h-VISA) isolated from a patient with orthopedic implant infection treated with glycopeptides: a case report. J. Exp. Clin. Med. 34, 149–154 (2017).
Okada, N. et al. A case report of postoperative VRSA enteritis: Effective management of rifampicin for vancomycin resistant Staphylococcus aureus enteritis after esophagectomy and colon reconstruction. Int. J. Surg. Case Rep. 52, 75–78 (2018).
Oksuz, L. et al. The high diversity of MRSA clones detected in a university hospital in Istanbul. Int. J. Med. Sci. 10, 1740 (2013).
Oliveira, G. A. et al. Isolation in Brazil of nosocomial Staphylococcus aureus with reduced susceptibility to vancomycin. Infect. Control Hosp. Epidemiol. 22, 443–448 (2001).
Olufunmiso, O., Tolulope, I. & Roger, C. Multidrug and vancomycin resistance among clinical isolates of Staphylococcus aureus from different teaching hospitals in Nigeria. Afr. Health Sci. 17, 797–807 (2017).
Othman, H. B., Halim, R. M. A., Gomaa, F. A. M. & Amer, M. Z. Vancomycin MIC distribution among methicillin-resistant Staphylococcus aureus. Is reduced vancomycin susceptibility related to MIC creep?. Open Access Maced J. Med. Sci. 7, 12–18. https://doi.org/10.3889/oamjms.2019.009 (2019).
Ouko, T. T. et al. Oxacillin resistant Staphylococcus aureus among HIV infected and non-infected Kenyan patients. East Afr. Med. J. 87, 179–186 (2010).
Panesso, D. et al. Methicillin-susceptible, vancomycin-resistant Staphylococcus aureus Brazil. Emerg. Infect. Dis. 21, 1844 (2015).
Parer, S. et al. An outbreak of heterogeneous glycopeptide-intermediate Staphylococcus aureus related to a device source in an intensive care unit. Infect. Control Hosp. Epidemiol. 33, 167–174. https://doi.org/10.1086/663703 (2012).
Park, K. H. et al. Comparison of the clinical features, bacterial genotypes and outcomes of patients with bacteraemia due to heteroresistant vancomycin-intermediate Staphylococcus aureus and vancomycin-susceptible S. aureus. J. Antimicrob. Chemother. 67, 1843–1849. https://doi.org/10.1093/jac/dks131 (2012).
Park, M. J. et al. Accessory gene regulator polymorphism and vancomycin minimum inhibitory concentration in Methicillin-Resistant Staphylococcus aureus. Ann. Lab. Med. 35, 399–403. https://doi.org/10.3343/alm.2015.35.4.399 (2015).
Phongsamart, W. et al. The first pediatric case of Staphylococcus aureus with heterogenous resistant to vancomycin endocarditis in Thailand. J. Med. Assoc. Thai 88, S264-268 (2005).
Pierard, D., Vandenbussche, H., Verschraegen, I. & Lauwers, S. Screening for Staphylococcus aureus with a reduced susceptibility to vancomycin in a Belgian hospital. Pathol. Biol. (Paris) 52, 486–488. https://doi.org/10.1016/j.patbio.2004.07.016 (2004).
Pitz, A. M. et al. Vancomycin susceptibility trends and prevalence of heterogeneous vancomycin-intermediate Staphylococcus aureus in clinical methicillin-resistant S. aureus isolates. J. Clin. Microbiol. 49, 269–274. https://doi.org/10.1128/jcm.00914-10 (2011).
Ramli, S. R., Neoh, H. M., Aziz, M. N. & Hussin, S. Screening and detection of heterogenous vancomycin intermediate Staphylococcus aureus in Hospital Kuala Lumpur Malaysia, using the glycopeptide resistance detection Etest and population analysis profiling. Infect. Dis. Rep. 4, e20. https://doi.org/10.4081/idr.2012.e20 (2012).
Rebiahi, S., Abdelouahid, D., Rahmoun, M., Abdelali, S. & Azzaoui, H. Emergence of vancomycin-resistant Staphylococcus aureus identified in the Tlemcen university hospital (North-West Algeria). Médecine et maladies infectieuses 41, 646–651 (2011).
Reverdy, M. et al. Incidence of Staphylococcus aureus with reduced susceptibility to glycopeptides in two French hospitals. Clin. Microbiol. Infect. 7, 267–272 (2001).
Richter, S. S. et al. Activities of vancomycin, ceftaroline, and mupirocin against Staphylococcus aureus isolates collected in a 2011 national surveillance study in the United States. Antimicrob. Agents Chemother. 58, 740–745 (2014).
Richter, S. S. et al. Detection of Staphylococcus aureus isolates with heterogeneous intermediate-level resistance to vancomycin in the United States. J. Clin. Microbiol. 49, 4203–4207. https://doi.org/10.1128/jcm.01152-11 (2011).
Riederer, K. et al. Detection of intermediately vancomycin-susceptible and heterogeneous Staphylococcus aureus isolates: comparison of Etest and Agar screening methods. J. Clin. Microbiol. 49, 2147–2150. https://doi.org/10.1128/jcm.01435-10 (2011).
Robert, J., Bismuth, R. & Jarlier, V. Decreased susceptibility to glycopeptides in methicillin-resistant Staphylococcus aureus: a 20 year study in a large French teaching hospital, 1983–2002. J. Antimicrob. Chemother. 57, 506–510. https://doi.org/10.1093/jac/dki486 (2006).
Rossi, F. et al. Transferable vancomycin resistance in a community-associated MRSA lineage. N. Engl. J. Med. 370, 1524–1531 (2014).
Rybak, M. J. et al. Characterization of vancomycin-heteroresistant Staphylococcus aureus from the metropolitan area of Detroit, Michigan, over a 22-year period (1986 to 2007). J. Clin. Microbiol. 46, 2950–2954. https://doi.org/10.1128/jcm.00582-08 (2008).
Sader, H. S., Jones, R. N., Rossi, K. L. & Rybak, M. J. Occurrence of vancomycin-tolerant and heterogeneous vancomycin-intermediate strains (hVISA) among Staphylococcus aureus causing bloodstream infections in nine USA hospitals. J. Antimicrob. Chemother. 64, 1024–1028. https://doi.org/10.1093/jac/dkp319 (2009).
Sambandam, S. N., Rohinikumar, G. J., Gul, A. & Mounasamy, V. Intramuscular injection abscess due to VRSA: a new health care challenge. Arch. Bone Joint Surg. 4, 277 (2016).
Sancak, B., Ercis, S., Menemenlioglu, D., Colakoglu, S. & Hascelik, G. Methicillin-resistant Staphylococcus aureus heterogeneously resistant to vancomycin in a Turkish university hospital. J. Antimicrob. Chemother. 56, 519–523. https://doi.org/10.1093/jac/dki272 (2005).
Sancak, B. et al. Vancomycin and daptomycin minimum inhibitory concentration distribution and occurrence of heteroresistance among methicillin-resistant Staphylococcus aureus blood isolates in Turkey. BMC Infect. Dis. 13, 583. https://doi.org/10.1186/1471-2334-13-583 (2013).
Shekarabi, M., Hajikhani, B., Chirani, A. S., Fazeli, M. & Goudarzi, M. Molecular characterization of vancomycin-resistant Staphylococcus aureus strains isolated from clinical samples: a three year study in Tehran Iran. PLoS ONE 12, e0183607 (2017).
Silveira, A. C. et al. Is prediffusion test an alternative to improve accuracy in screening hVISA strains and to detect susceptibility to glycopeptides/lipopeptides?. Diagn. Microbiol. Infect. Dis. 79, 401–404. https://doi.org/10.1016/j.diagmicrobio.2014.04.008 (2014).
Singh, A. et al. Increasing trend of heterogeneous vancomycin intermediate Staphylococcus aureus in a tertiary care center of Northern India. Microb. Drug Resist. 21, 545–550. https://doi.org/10.1089/mdr.2015.0004 (2015).
Sivakumar, B., Vijaysegaran, P., Chaudhuri, A., Crawford, S. & Ottley, M. Daptomycin resistance in prosthetic joint infections. Orthopedics 35, e603–e606 (2012).
Sng, L.-H. et al. Heterogeneous vancomycin-resistant Staphylococcus aureus (hetero-VISA) in Singapore. Int. J. Antimicrob. Agents 25, 177–179 (2005).
Sola, C. et al. Heterogeneous vancomycin-intermediate susceptibility in a community-associated methicillin-resistant Staphylococcus aureus epidemic clone, in a case of Infective Endocarditis in Argentina. Ann. Clin. Microbiol. Antimicrob. 10, 15 (2011).
Song, J. H. et al. Emergence in Asian countries of Staphylococcus aureus with reduced susceptibility to vancomycin. Antimicrob. Agents Chemother. 48, 4926–4928. https://doi.org/10.1128/aac.48.12.4926-4928.2004 (2004).
Stroh, E. M. Quinupristin/dalfopristin in vancomycin-resistant Staphylococcus aureus endophthalmitis. Arch. Ophthalmol. 130, 1323–1324 (2012).
Sumon, Z. E. et al. Successful cure of daptomycin-non-susceptible, vancomycin-intermediate Staphylococcus aureus prosthetic aortic valve endocarditis directed by synergistic in vitro time-kill study. Infect. Dis. 51, 287–292 (2019).
Sun, W. et al. Prevalence and characterization of heterogeneous vancomycin-intermediate Staphylococcus aureus isolates from 14 cities in China. Antimicrob. Agents Chemother. 53, 3642–3649. https://doi.org/10.1128/aac.00206-09 (2009).
Swartz, T. et al. Heart transplantation in a patient with heteroresistant vancomycin-intermediate S taphylococcus aureus ventricular assist device mediastinitis and bacteremia. Transplant. Infect. Dis. 15, E177–E181 (2013).
Taha, A., Badr, M., El-Morsy, F. & Hammad, E. Report of β-lactam antibiotic–induced vancomycin-resistant Staphylococcus aureus from a university hospital in Egypt. New Microb. new Infect. 29, 100507 (2019).
Takata, T. et al. Presence of both heterogeneous vancomycin-intermediate resistance and β-lactam antibiotic-induced vancomycin resistance phenotypes is associated with the outcome in methicillin-resistant Staphylococcus aureus bloodstream infection. Scand. J. Infect. Dis. 45, 203–212 (2013).
Tallent, S. M. et al. Vancomycin susceptibility of oxacillin-resistant Staphylococcus aureus isolates causing nosocomial bloodstream infections. J. Clin. Microbiol. 40, 2249–2250. https://doi.org/10.1128/jcm.40.6.2249-2250.2002 (2002).
Tascini, C. et al. Case report of a successful treatment of methicillin-resistant Staphylococcus aureus (MRSA) bacteremia and MRSA/vancomycin-resistant enterococcus faecium cholecystitis by daptomycin. Antimicrob. Agents Chemother. 55, 2458–2459 (2011).
Thati, V., Shivannavar, C. T. & Gaddad, S. M. Vancomycin resistance among methicillin resistant Staphylococcus aureus isolates from intensive care units of tertiary care hospitals in Hyderabad. Indian J. Med. Res. 134, 704 (2011).
Thirat, S. Methicillin-resistant Staphylococcus aureus with reduced susceptibility to vancomycin in Sanprasitthiprasong Hospital. J. Med. Assoc. Thai 97, S1 (2014).
Tiwari, H. K. & Sen, M. R. Emergence of vancomycin resistant Staphylococcus aureus (VRSA) from a tertiary care hospital from northern part of India. BMC Infect. Dis. 6, 156 (2006).
Tóth, Á et al. First report of heterogeneously vancomycin-intermediate Staphylococcus aureus (hVISA) causing fatal infection in Hungary. J. Chemother. 20, 655–656 (2008).
Trakulsomboon, S. et al. First Report of Methicillin-ResistantStaphylococcus aureus with Reduced Susceptibility to Vancomycin in Thailand. J. Clin. Microbiol. 39, 591–595 (2001).
Tsakris, A., Papadimitriou, E., Douboyas, J., Stylianopoulou, F. & Manolis, E. Emergence of vancomycin-intermediate Staphylococcus aureus and S. sciuri Greece. Emerg. Infect. Dis. 8, 536 (2002).
Ullah, A. et al. High frequency of methicillin-resistant Staphylococcus aureus in Peshawar Region of Pakistan. Springerplus 5, 600. https://doi.org/10.1186/s40064-016-2277-3 (2016).
van Hal, S. J., Jones, M., Gosbell, I. B. & Paterson, D. L. Vancomycin heteroresistance is associated with reduced mortality in ST239 methicillin-resistant Staphylococcus aureus blood stream infections. PLoS ONE 6, e21217. https://doi.org/10.1371/journal.pone.0021217 (2011).
Varona-Barquín, A., Iglesias-Losada, J. J., Ezpeleta, G., Eraso, E. & Quindós, G. Vancomycin heteroresistant community associated methicillin-resistant Staphylococcus aureus ST72-SCCmecIVa strain colonizing the nostrils of a five-year-old Spanish girl. Enfermedades infecciosas y microbiologia clinica (English ed.) 35, 148–152 (2017).
Vellappally, S. et al. Occurrence of vancomycin-resistant Staphylococcus aureus in the oral cavity of patients with dental caries. Acta Microbiol. Immunol. Hung. 64, 343–351 (2017).
Wang, J. L. et al. High vancomycin minimum inhibitory concentrations with heteroresistant vancomycin-intermediate Staphylococcus aureus in meticillin-resistant S. aureus bacteraemia patients. Int. J. Antimicrob. Agents 42, 390–394. https://doi.org/10.1016/j.ijantimicag.2013.07.010 (2013).
Whitener, C. J. et al. Vancomycin-resistant Staphylococcus aureus in the absence of vancomycin exposure. Clin. Infect. Dis. 38, 1049–1055 (2004).
Wong, S.S.-Y. et al. Bacteremia due to Staphylococcus aureus with reduced susceptibility to vancomycin. Diagn. Microbiol. Infect. Dis. 36, 261–268 (2000).
Yamakawa, J. et al. Heterogeneously vancomycin-intermediate Staphylococcus aureus (hVISA) emerged before the clinical introduction of vancomycin in Japan: a retrospective study. J. Infect. Chemother. 18, 406–409. https://doi.org/10.1007/s10156-011-0330-2 (2012).
Yoon, J. Vancomycin resistance of Staphylococcus aureus in Korean primary hospitals. J. Bacteriol. Virol. 44, 305–310 (2014).
Yousefi, M. et al. Identification of tigecycline- and vancomycin-resistant Staphylococcus aureus strains among patients with urinary tract infection in Iran. New Microb. New Infect. 19, 8–12. https://doi.org/10.1016/j.nmni.2017.05.009 (2017).
Zeller, V., Kitzis, M.-D., Graff, W., Mamoudy, P. & Desplaces, N. Hip arthroplasty infection with heterogeneous vancomycin-resistant Staphylococcus aureus. Scand. J. Infect. Dis. 38, 934–938 (2006).
Zhang, X. et al. First report of a sequence type 239 vancomycin-intermediate Staphylococcus aureus isolate in Mainland China. Diagn. Microbiol. Infect. Dis. 77, 64–68 (2013).
Zhu, X. et al. Vancomycin intermediate-resistant Staphylococcus aureus (VISA) isolated from a patient who never received vancomycin treatment. Int. J. Infect. Dis. 33, 185–190 (2015).
Lin, C.-Y., Wang, J.-H., Lin, K.-H., Ho, Y.-L. & Ho, C.-M. Methicillin-resistant Staphylococcus aureus with reduced vancomycin susceptibility in Taiwan. Tzu-Chi Med. J. 30, 135 (2018).
Institute, J. B. Joanna Briggs Institute reviewers’ manual 2014th edn. (The Joanna Briggs Institute, Australia, 2014).
Mantel, N. & Haenszel, W. Statistical aspects of the analysis of data from retrospective studies of disease. J. Natl. Cancer Inst. 22, 719–748 (1959).
DerSimonian, R. & Laird, N. Meta-analysis in clinical trials. Control. Clin. Trials 7, 177–188 (1986).
Higgins, J. P., Thompson, S. G., Deeks, J. J. & Altman, D. G. Measuring inconsistency in meta-analyses. BMJ 327, 557–560 (2003).
Gardete, S. & Tomasz, A. Mechanisms of vancomycin resistance in Staphylococcus aureus. J. Clin. Investig. 124, 2836–2840 (2014).
Cosgrove, S., Carroll, K. C. & Perl, T. Staphylococcus aureus with reduced susceptibility to vancomycin. Clin. Infect. Dis. 39, 539–545 (2004).
Howden, B. P., Davies, J. K., Johnson, P. D., Stinear, T. P. & Grayson, M. L. Reduced vancomycin susceptibility in Staphylococcus aureus, including vancomycin-intermediate and heterogeneous vancomycin-intermediate strains: resistance mechanisms, laboratory detection, and clinical implications. Clin. Microbiol. Rev. 23, 99–139 (2010).
Walsh, T. R. & Howe, R. A. The prevalence and mechanisms of vancomycin resistance in Staphylococcus aureus. Ann. Rev. Microbiol. 56, 657–675 (2002).
Smith, T. L. et al. Emergence of vancomycin resistance in Staphylococcus aureus. N. Engl. J. Med. 340, 493–501 (1999).
Cui, L. et al. Cell wall thickening is a common feature of vancomycin resistance in Staphylococcus aureus. J. Clin. Microbiol. 41, 5–14 (2003).
Fridkin, S. K. et al. Epidemiological and microbiological characterization of infections caused by Staphylococcus aureus with reduced susceptibility to vancomycin, United States, 1997–2001. Clin. Infect. Dis. 36, 429–439 (2003).
Bhattacharyya, D. et al. First report on vancomycin-resistant Staphylococcus aureus in bovine and caprine milk. Microbial. Drug. Res. 22, 675–681 (2016).
Moreno, L. Z. et al. Vancomycin-intermediate livestock-associated methicillin-resistant Staphylococcus aureus ST398/t9538 from swine in Brazil. Mem. Inst. Oswaldo Cruz 111, 659–661 (2016).
Ho, P.-L. et al. Vancomycin MIC creep in MRSA isolates from 1997 to 2008 in a healthcare region in Hong Kong. J. Infect. 60, 140–145 (2010).
Chang, W. et al. Vancomycin MIC creep in methicillin-resistant Staphylococcus aureus (MRSA) isolates from 2006 to 2010 in a hospital in China. Indian J. Med. Microbiol. 33, 262 (2015).
Jacob, J. T. & DiazGranados, C. A. High vancomycin minimum inhibitory concentration and clinical outcomes in adults with methicillin-resistant Staphylococcus aureus infections: a meta-analysis. Int. J. Infect. Dis. 17, e93–e100 (2013).
Van Hal, S., Lodise, T. P. & Paterson, D. L. The clinical significance of vancomycin minimum inhibitory concentration in Staphylococcus aureus infections: a systematic review and meta-analysis. Clin. Infect. Dis. 54, 755–771 (2012).
Kim, T. et al. Clinical and microbiological factors associated with early patient mortality from methicillin-resistant Staphylococcus aureus bacteremia. Kor. J. Internal Med. 34, 184 (2019).
Kelley, P. G., Gao, W., Ward, P. B. & Howden, B. P. Daptomycin non-susceptibility in vancomycin-intermediate Staphylococcus aureus (VISA) and heterogeneous-VISA (hVISA): implications for therapy after vancomycin treatment failure. J. Antimicrob. Chemother. 66, 1057–1060 (2011).
Cui, L., Tominaga, E., Neoh, H.-M. & Hiramatsu, K. Correlation between reduced daptomycin susceptibility and vancomycin resistance in vancomycin-intermediate Staphylococcus aureus. Antimicrob. Agents Chemother. 50, 1079–1082 (2006).
Sieradzki, K., Roberts, R. B., Haber, S. W. & Tomasz, A. The development of vancomycin resistance in a patient with methicillin-resistant Staphylococcus aureus infection. N. Engl. J. Med. 340, 517–523 (1999).
Hageman, J. C. et al. Management of persistent bacteremia caused by methicillin-resistant Staphylococcus aureus: a survey of infectious diseases consultants. Clin. Infect. Dis. 43, e42–e45 (2006).
McGuinness, W. A., Malachowa, N. & DeLeo, F. R. Vancomycin Resistance in Staphylococcus aureus. Yale J. Biol. Med. 90, 269–281 (2017).
Siegel, J. Healthcare Infection Control Practices Advisory Committee 2007 Guideline for isolation precautions: preventing transmission of infectious agents in healthcare settings. https://www.cdc.gov/ncidod/dhqp/gl_isolation.html (2007).
Ayliffe, G. et al. Revised guidelines for the control of methicillin-resistant Staphylococcus aureus infection in hospitals: report of a combined working party of the British Society for Antimicrobial Chemotherapy, the Hospital Infection Society and the Infection Control Nurses Association. J. Hosp. Infect. 39, 253–290 (1998).
Luzar, M. A. et al. Staphylococcus aureus nasal carriage and infection in patients on continuous ambulatory peritoneal dialysis. N. Engl. J. Med. 322, 505–509 (1990).
Author information
Authors and Affiliations
Contributions
D.D.-S. and M.D. conceived and designed the study. A.S. and M.T.M. contributed in comprehensive research and data extraction. M.D. analyzed all the data. M.D. and S.Y. designed the Figures. D.D.-S., M.D. and A.S. wrote the paper. A.B. and D.D.-S. participated in critical manuscript editing.
Corresponding authors
Ethics declarations
Competing interests
Alex van Belkum is a bioMerieux employee. bioMerieux is a company that design, develops and sells diagnostics in the field on infectious diseases. The company had no direct influence on the design and execution of the present study. Rest of the authors declare to have no competing interest.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Shariati, A., Dadashi, M., Moghadam, M.T. et al. Global prevalence and distribution of vancomycin resistant, vancomycin intermediate and heterogeneously vancomycin intermediate Staphylococcus aureus clinical isolates: a systematic review and meta-analysis. Sci Rep 10, 12689 (2020). https://doi.org/10.1038/s41598-020-69058-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-69058-z
This article is cited by
-
Genetic diversity of macrolides resistant Staphylococcus aureus clinical isolates and the potential synergistic effect of vitamins, C and K3
BMC Microbiology (2024)
-
Optimization of fermentation conditions and medium components for chrysomycin a production by Streptomyces sp. 891-B6
BMC Microbiology (2024)
-
Optimization of the media components for increased production of vancomycin by Amycolatopsis orientalis
Biomass Conversion and Biorefinery (2024)
-
Genetic characterization of tetracycline-resistant Staphylococcus aureus with reduced vancomycin susceptibility using whole-genome sequencing
Archives of Microbiology (2024)
-
Engineered phage enzymes against drug-resistant pathogens: a review on advances and applications
Bioprocess and Biosystems Engineering (2024)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.