Abstract
This study aimed to investigate the association of maternal sleep before and during pregnancy with preterm birth, infant sleep and temperament at 1 month of age. We used the data of the Japan Environment and Children’s Study, a cohort study in Japan, which registered 103,099 pregnancies between 2011 and 2014. Participants were asked about their sleep before and during pregnancy, and the sleep and temperament of their newborns at 1 month of age. Preterm birth data were collected from medical records. Maternal sleep was not associated with preterm birth, but subjective sleep quality during pregnancy was associated with late preterm birth (birth at 34–36 weeks of gestation). For example, participants with extremely light subjective depth of sleep were more likely to experience preterm birth (RR = 1.19; 95% confidence interval [CI] = 1.04–1.35). Maternal sleep both before and during pregnancy seemed to be associated with infant sleep and temperament at 1 month of age. Infants, whose mothers slept for less than 6 hours before pregnancy, tended to cry intensely (RR = 1.15; 95% CI = 1.09–1.20). Maternal sleep problems before and during pregnancy were associated with preterm birth and child sleep problems and temperament.
Similar content being viewed by others
Introduction
In Japan, the average sleep duration is shorter than in other countries1, and it has become even shorter in recent years2. At the same time, the rate of preterm birth in Japan has increased3, as has the incidence of developmental disorders4.
Maternal short sleep duration and sleep-disordered breathing (SDB) are associated with increased preterm birth rates5,6. Furthermore, maternal SDB and apnea during pregnancy affects offspring’s development, manifesting as disrupted social skills and low reading test scores7,8.
However, no large-scale study has examined potential associations between sleep during pregnancy and offspring’s development. Additionally, the importance of maternal sleep during various periods of pregnancy remains unclear. Maternal short sleep and SDB increase inflammatory cytokine levels9,10, and maternal inflammation can cause preterm birth11,12 and developmental disorder13,14. Maternal obesity also increases inflammatory cytokines15,16, and a study reported that maternal pre-pregnancy body mass index (BMI) affects maternal inflammatory markers to a greater extent than does late pregnancy BMI17. Similarly, maternal sleep before pregnancy may also be more important for obstetric outcomes and offspring development than sleep during pregnancy.
In cases of neurodevelopmental disorders, including autism spectrum disorder (ASD), abnormalities of neurodevelopment, sleep, and temperament are observed in early infancy, such as a 1–4-month-old18,19. This study aimed to investigate the association of maternal sleep before and during pregnancy with preterm birth, infant sleep, and temperament at 1 month of age.
Results
The baseline characteristics of participants, along with available data on sleep duration before and during pregnancy, are shown in Table 1. The most commonly reported sleep duration was 7–8 h both before and during pregnancy.
Maternal sleep and preterm birth
Sleep duration and bedtime before and during pregnancy were not associated with preterm birth in this study (Table 2). However, very light sleep and very bad feeling when waking up during pregnancy were associated with late preterm birth in a multivariable model (RR for very light sleep vs. normal = 1.19, 95% CI = 1.04–1.35; RR for very bad feeling vs. normal = 1.31, 95% CI = 1.02–1.67) (Table 3).
Maternal sleep and infant sleep
Sleep duration and bed time before pregnancy were not associated with ≥ 5 nocturnal awakenings. However, both sleep duration and bed time were likely to be related with an infant’s tendency to sleep longer during the day than at night (Table 4).
In the M-T2, waking up ≥ 5 times during the night was associated with maternal light sleep and feeling bad at awakening during pregnancy. Sleeping longer during the day than at night was related not only to maternal short sleep duration but also to late bed time and feeling bad at awakening (Table 5).
In the subanalysis of participants who slept 7–9 h before pregnancy, maternal short sleep and bed time after midnight were associated with longer day sleeps. Similarly, in the group of participants who slept 7–9 h during pregnancy, maternal short sleep before pregnancy was associated with more awakenings during the night and longer day-time sleep durations (Table S1).
Maternal sleep and infant temperament
In the M-T1, sleeping < 7 h and going to bed after midnight were associated with infants with bad mood, frequent crying for long periods, and intense crying (Table 6).
In the M-T2, we observed a relationship between bad mood and maternal short sleep, late bed time, light sleep, and feeling bad on awakening. Frequent crying for long periods was likely to be associated with short sleep, late bed time, light sleep, and feeling bad on awakening. Intense crying was also related to short sleep, late bed time, light sleep, and feeling bad on awakening (Table 7).
In the subanalysis of participants who slept 7–9 h before pregnancy, maternal short sleep during pregnancy was associated with bad mood in infants. Similarly, in the group of participants who slept 7–9 h during pregnancy, maternal late bed time before pregnancy was associated with bad mood in infants (Table S2).
Discussion
This study investigated whether maternal sleep before and during pregnancy was associated with preterm birth, infants sleep and temperament at 1 month of age, using data from a nationwide large-scale cohort study.
In this study, preterm birth was only associated with the quality of maternal sleep during pregnancy. Previous studies reported an association between preterm birth and subjective maternal sleep quality9,20. Subjective sleep depth and mood on awakening may reflect maternal SDB or depression21,22, both of which are known to increase preterm birth rates6,20. Interventions to improve sleep depth and mood on awakening could reduce preterm birth rates.
Contrary to a previous meta-analysis in 20185, we found no association of sleep duration with preterm birth. One conceivable reason for this difference is the lower rate of preterm birth in Japan compared to other countries23,24.
This study also revealed an association of maternal sleep before and during pregnancy with infant sleep and temperament at 1 month of age. To our knowledge, no studies have previously reported similar findings. However, infant sleep disorders and temperament have been reported to increase maternal stress25 and relate to maternal anxiety disorder and depression26. As a result, it may lead to parenting abandonment and child abuse27. If maternal sleep before and during pregnancy could be addressed to improve infant sleep and temperament, maternal postpartum mental disease and child abuse could also be reduced.
Maternal sleep before pregnancy also seemed to be associated with some features of infant temperament and frequent night awakenings in the group of participants with adequate sleep duration (7–9 h) during pregnancy. The Centers for Disease Control and Prevention and the World Health Organization recently issued statements on the importance of preconception care28, without emphasising maternal sleep. We should probably pay more attention to maternal sleep not only during pregnancy but also before pregnancy.
This study had four major limitations. First, maternal obesity and depression may be confounding factors: both are associated with sleeping problems and can cause maternal inflammation29,30. Some epidemiological studies have also reported that maternal obesity and depression are associated with preterm birth and developmental disorders20,31. In this study, we showed an association between maternal sleep and preterm birth, infant sleeping problems, and temperament after adjustment for pre-pregnancy BMI and postpartum depressive symptoms. Maternal sleep may affect these outcomes. However, adjustment for maternal depression could be insufficient because depressive symptoms were investigated postpartum.
Second, information about maternal and infant sleeping problems and infant temperament were collected using a questionnaire.
Third, because of the observational study design, we were not able to demonstrate how maternal sleep affected outcomes. Evidence suggests that inflammatory response plays a role, due to maternal sleep disruption during pregnancy causing preterm birth and aberrant development of offspring; short maternal sleep duration and SDB increases inflammatory cytokine levels9,10. It is believed that maternal inflammation can cause preterm birth11,12 and developmental disorders, such as ASD13,14. However, this study did not analyse inflammatory markers.
Fourth, the large sample size might show a statistically significant difference even when the difference is small. Since there have been no similar reports to this work, further investigations of relationships between maternal sleep and offspring’s outcome are necessary.
In conclusion, maternal sleep problems before and during pregnancy were associated with preterm birth and infant sleep problems and temperament.
Methods
Research ethics
The study protocol was approved by the Ministry of Environment’s Institutional Review Board on Epidemiological Studies and by the Ethics Committee of all participating institutions: the National Institute for Environmental Studies that leads the JECS, the National Center for Child Health and Development, Hokkaido University, Sapporo Medical University, Asahikawa Medical College, Japanese Red Cross Hokkaido College of Nursing, Tohoku University, Fukushima Medical University, Chiba University, Yokohama City University, University of Yamanashi, Shinshu University, University of Toyama, Nagoya City University, Kyoto University, Doshisha University, Osaka University, Osaka Medical Center and Research Institute for Maternal and Child Health, Hyogo College of Medicine, Tottori University, Kochi University, University of Occupational and Environmental Health, Kyushu University, Kumamoto University, University of Miyazaki, and University of Ryukyu.. Written informed consent, which also included the follow-up study of children after birth, was obtained from all participants. All methods were performed in accordance with approved guidelines.
Study participants
Data used in this study were obtained from the Japan Environment and Children’s Study (JECS), an ongoing large-scale cohort study. The JECS elucidated environmental factors that affected children’s health and development and was designed to follow-up pregnant women until their newborns grow up to 13 years old. The participants were recruited between 2011 and 2014 in 15 regions throughout Japan, and the follow-up is carried out mainly by a self-administered questionnaire. The detailed protocol has been reported elsewhere32. The baseline profile of participants in the JECS was reported previously33. Participants answered a questionnaire about lifestyle and behaviour twice during pregnancy: at recruitment (early pregnancy, M-T1) and later during mid- and late-pregnancy (M-T2). Participants also answered a questionnaire about their newborns at 1 month after delivery (M-1m).
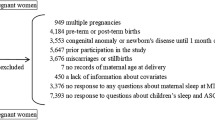
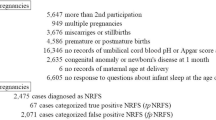
Of all 103,099 pregnancies, we excluded 14,845 pregnancies due to the following reasons: no delivery records (n = 2,321), prior participation in the study (n = 5,608), multiple pregnancy (n = 947), miscarriage or stillbirth (n = 1,427), congenital anomaly identified by 1 month old (n = 3,554), missing information on maternal age at delivery (n = 5), and no response to the questions related to sleep at both M-T1 and M-T2 (n = 983). The remaining 88,254 participants (87,106 with M-T1 data and 86,358 with M-T2 data) were included in the analysis of the association between maternal sleep and preterm birth. Then, we further excluded preterm or post-term deliveries (n = 4,113) and participants who did not respond to the questions related to the children’s sleep and temperament at M-1m (n = 1,307). (Fig. 1) Finally, 81,821 participants with M-T1 data and 82,038 participants with M-T2 data were included in the analysis of the association between maternal sleep and infant sleep and temperament.
Maternal sleep
In the M-T1 questionnaire, participants were asked about their sleep duration and bed time before pregnancy. We divided participants into six groups by sleep time: < 6 h, 6–7 h, 7–8 h, 8–9 h, 9–10 h, and > 10 h. Participants were also divided by bedtime: 9:00 p.m. to midnight, midnight to 3 a.m., and others.
In the M-T2 questionnaire, participants were asked about their sleep duration and bed time during pregnancy. The participants were divided into groups as described above for the M-T1. In addition, the M-T2 questionnaire included two more questions about sleep quality. One was, “How would you rate your average depth of sleep during the past month?” The other one was, “How would you rate your overall feeling when waking up in the morning during past month?” The answers to both questions were scored 1, 2, 3, 4, and 5, representing very light (bad), relatively light (bad), normal, relatively deep (good), and very deep (good), respectively.
Preterm birth
Information on gestational age at delivery was transferred from medical records. Preterm birth was defined as birth before 37 completed weeks of gestation. In the present study, 3,903 (4.4%) pregnant women had preterm births. We divided these women into two groups: the early preterm birth group (birth before 34 completed weeks of gestation) and the late preterm birth group (birth after 34 gestational weeks). There were 759 (0.9%) women in the early preterm birth group and 3,144 (3.6%) women in the late preterm birth group. In the analysis of association between maternal sleep during pregnancy and preterm birth, we selected only late preterm birth as an outcome because some participants in the early preterm birth group did not answer M-T2 questionnaire between 22 and 28 weeks gestational age. So, the available number of participants in the early preterm group was too small to analyse.
Outcome (infant sleep and temperament)
At 1 month after delivery, we assessed infant sleep and temperature using a parents-reported questionnaire (M-1m questionnaire). For infant sleep, participants were asked about sleep and wake times during a 24-h period for their newborns. In this analysis, we focused on two points. First, we analysed the number of nocturnal awakenings. We defined ≥ 5 awakenings as too many because a previous study reported that the average number of awakenings during the night (20:00 – 7:59) is 2.95 (range: 1.0–5.0) for 2-week-old infants34. Second, we analysed whether the infants slept longer during the day (08:00–19:59) or at night (20:00–7:59). We regarded longer sleeping times during the day than at night as unusual.
Also, the M-1m questionnaire included three questions about infant temperament. The first question was, “When you hold your baby, how often do you feel difficulty to hold your baby due to his/her fretting, crying, or throwing his/her head back?”; the answer options were “often,” “sometimes”, “seldom,” and “none.” Those who answered “often” were categorised as “bad mood.” The second question was, “How often and for how long does your baby cry?”; the answer options were “quite often and for long periods,” “sometimes and for short periods,” and “seldom and almost never.” Those who answered as “quite often and long” were categorised as “frequent crying, for long periods.” The third question was “Does your baby cry very hard sometimes no matter what you do to stop him/her?”; the answer options were “yes” and “no,” and those who answered “yes” were categorised as “intense crying”. These categories are the same as those in our previous study35.
Covariates
Information about maternal age at delivery, smoking habits, alcohol consumption, pre-pregnancy body mass index (BMI), parity, current history of diabetes, gestational diabetes, hypertensive disorder in pregnancy and intrauterine infection, history of preterm birth, gestational age at birth, infertility treatment, infant sex, type of delivery, small for gestational age and postpartum depressive symptoms were collected via self-administered questionnaires and/or medical records. Postpartum depressive symptoms were assessed using the Edinburgh Postnatal Depression Scale (EPDS), including in the questionnaire at 1 month after delivery36. According to previous studies37, participants with a score of 9 or more were categorized as having depressive symptoms.
Statistical analyses
We used the Poisson regression model with a robust error variance38 to explore the association of maternal sleep before and during pregnancy with each outcome and to estimate the relative risks (RRs) of each outcome and 95% confidence intervals (CIs). We initially adjusted for maternal age at delivery, and then further adjusted as follows. In the analysis of the association between maternal sleep and preterm birth, we adjusted for smoking habits (never-smokers, ex-smokers who quit before pregnancy, smokers during early pregnancy), alcohol consumption (never-drinkers, ex-drinkers who quit before pregnancy, drinkers during early pregnancy), pre-pregnancy BMI (< 18·5, 18·5–24·9, ≥ 25·0 kg m2), current history of diabetes or gestational diabetes (yes, no), hypertensive disorders in pregnancy (yes, no) and intrauterine infection (yes, no), parity (0, ≥ 1), history of preterm birth (yes, no) and infertility treatment (yes, no).
In the analysis of the association between maternal sleep and infant sleep or temperament, we adjusted for smoking habits, alcohol consumption, pre-pregnancy BMI, gestational age at birth (37, 38, 39, 40, and 41 weeks of gestation), infant sex (boys, girls), parity, infertility treatment, type of delivery (vaginal, caesarean section), small for gestational age infants (yes, no), and postpartum depressive symptoms (yes, no).
We performed a subanalysis of infant sleep or temperament in the participant groups that reported adequate sleep durations of 7–9 h both at M-T1 and M-T2 to evaluate how maternal sleep before and during pregnancy impacts the outcome of these parameters.
The dataset used for statistical analyses was the jecs-ag-20160424 dataset, which was released in June 2016, and revised in October 2016, along with the supplementary dataset jecs-ag-20160424-sp1. Stata version 14 (StataCorp LP, College Station, Texas, USA) was used for all analyses.
References
Organization for Economic Co-operation and Development (OECD). Special focus: measuring leisure in OECD countries 19. https://www.oecd.org/berlin/42675407.pdf (2009).
Statistics Bureau, Ministry of Internal Affairs and Communications, Japan. Survey on time use and leisure activities in 2016: summary of results (QuestionnaireA) time use. https://www.stat.go.jp/english/data/shakai/2016/pdf/timeuse-a2016.pdf (2016).
Ministry of Health, Labour and Welfare, Japan. Vital Statistics of Japan 2017. https://www.mhlw.go.jp/english/database/db-hw/dl/81-1a2en.pdf (2017).
Ministry of Education, Culture, Sports, Science and Technology, Japan. Number of students taking special classes in 2014 (in Japanese). https://www.mext.go.jp/a_menu/shotou/tokubetu/material/__icsFiles/afieldfile/2015/03/27/1356210.pdf (2015)
Warland, J., Dorrian, J., Morrison, J. L. & O’Brien, L. M. Maternal sleep during pregnancy and poor fetal outcomes: a scoping review of the literature with meta-analysis. Sleep Med. Rev. 41, 197–219. https://doi.org/10.1016/j.smrv.2018.03.004 (2018).
Brown, N. T., Turner, J. M. & Kumar, S. The intrapartum and perinatal risks of sleep-disordered breathing in pregnancy: a systematic review and metaanalysis. Am. J. Obstet. Gynecol. 219(2), 147-161.e1. https://doi.org/10.1016/j.ajog.2018.02.004 (2018).
Bassan, H. et al. The effect of maternal sleep-disordered breathing on the infant’s neurodevelopment. Am. J. Obstet. Gynecol. 212(5), 656.e1-656.e7. https://doi.org/10.1016/j.ajog.2015.01.001 (2015).
Sun, Y., Hons, B., Cistulli, P. A. & Hons, M. Childhood health and educational outcomes associated with maternal sleep apnea: a population record-linkage study. Sleep 40(11), zsx158. https://doi.org/10.1093/sleep/zsx158 (2017).
Blair, L. M., Porter, K., Leblebicioglu, B. & Christian, L. M. Poor sleep quality and associated inflammation predict preterm birth: heightened risk among African Americans. Sleep 38(8), 1259–1267. https://doi.org/10.5665/sleep.4904 (2015).
Okun, M. L., Luther, J. F., Wisniewski, S. R. & Wisner, K. L. Disturbed sleep and inflammatory cytokines in depressed and nondepressed pregnant women. Psychosom Med. 75(7), 670–681. https://doi.org/10.1097/psy.0b013e31829cc3e7 (2013).
Cappelletti, M., Della Bella, S., Ferrazzi, E., Divanovic, S. & Mavilio, D. Inflammation and preterm birth. J. Leukoc. Biol. 99(1), 67–78. https://doi.org/10.1189/jlb.3mr0615-272rr (2015).
Kwak-Kim, J. et al. Inflammation induced preterm labor and birth. J. Reprod. Immunol. 129, 53–58. https://doi.org/10.1016/j.jri.2018.06.029 (2018).
Schobel, S. A. et al. Maternal immune activation and abnormal brain development across CNS disorders. Nat. Rev. Neurol. 10(11), 643–660. https://doi.org/10.1038/nrneurol.2014.187 (2014).
Estes, M. L. & McAllister, A. K. Maternal immune activation: implications for neuropsychiatric disorders. Science 353(6301), 772–777. https://doi.org/10.1126/science.aag3194 (2016).
Stewart, F. M., Freeman, D. J. & Ramsay, J. E. Longitudinal assessment of maternal endothelial function and markers of inflammation and placental function throughout pregnancy in lean and obese mothers. J. Clin. Endocrinol. Metab. 92, 969–975. https://doi.org/10.1210/jc.2006-2083 (2007).
Christian, L. M. & Porter, K. Longitudinal changes in serum proinflammatory markers across pregnancy and postpartum: effects of maternal body mass index. Cytokine 70, 134–140. https://doi.org/10.1016/j.cyto.2014.06.018 (2014).
McDade, T. W., Borja, J. B., Largado, F., Adair, L. S. & Kuzawa, C. W. Adiposity and chronic inflammation in young women predict inflammation during normal pregnancy in the Philippines. J. Nutr. 146(2), 353–357. https://doi.org/10.3945/jn.115.224279 (2016).
Karmel, B. Z. et al. Early medical and behavioral characteristics of NICU infants later classified with ASD. Pediatrics 126(3), 457–467. https://doi.org/10.1542/peds.2009-2680 (2010).
Saenz, J., Yaugher, A. & Alexander, G. M. Sleep in infancy predicts gender specific social-emotional problems in toddlers. Front. Pediatr. 3, 1–6. https://doi.org/10.3389/fped.2015.00042 (2015).
Straub, H., Adams, M., Kim, J. J. & Silver, R. K. Antenatal depressive symptoms increase the likelihood of preterm birth. Am. J. Obstet. Gynecol. 207(4), 329.e1-329.e4. https://doi.org/10.1016/j.ajog.2012.06.033 (2012).
Pamidi, S. & Kimoff, R. J. Maternal sleep-disordered breathing. Chest 153(4), 1052–1066. https://doi.org/10.1016/j.chest.2017.10.011 (2018).
Chong, Y.-S. et al. Associations between poor subjective prenatal sleep quality and postnatal depression and anxiety symptoms. J. Affect. Disord. 202, 91–94. https://doi.org/10.1016/j.jad.2016.05.028 (2016).
Blencowe, H. et al. National, regional, and worldwide estimates of preterm birth rates in the year 2010 with time trends since 1990 for selected countries: a systematic analysis and implications. Lancet 379(9832), 2162–2172. https://doi.org/10.1016/S0140-6736(12)60820-4 (2012).
Purisch, S. E. & Gyamfi-Bannerman, C. Epidemiology of preterm birth. Semin. Perinatol. 41(7), 387–391. https://doi.org/10.1053/j.semperi.2017.07.009 (2017).
Moe, V., von Soest, T., Fredriksen, E., Olafsen, K. S. & Smith, L. The multiple determinants of maternal parenting stress 12 months after birth: The contribution of antenatal attachment style, adverse childhood experiences, and infant temperament. Front. Psychol. 9, 1987. https://doi.org/10.3389/fpsyg.2018.01987 (2018).
Britton, J. R. Infant temperament and maternal anxiety and depressed mood in the early postpartum period. Women Health. 51(1), 55–71. https://doi.org/10.1080/03630242.2011.540741 (2011).
Zahra, E. D. et al. Maternal child abuse and its association with maternal anxiety in the socio-cultural context of Iran. Oman Med. J. 28(6), 404–409. https://doi.org/10.5001/omj.2013.116 (2013).
World Health Organization. Preconception care policy brief (1). 1–8. doi:10.1016/S1002-0721(09)60023-5 (2013).
Huang, E. et al. Maternal prenatal depression predicts infant negative affect via maternal inflammatory cytokine levels. Brain Behav. Immun. 73, 470–481. https://doi.org/10.1016/j.bbi.2018.06.011 (2018).
van der Burg, J. W. et al. The role of systemic inflammation linking maternal BMI to neurodevelopment in children. Pediatr. Res. 79(1), 3–12. https://doi.org/10.1038/pr.2015.179 (2016).
Chu, S. Maternal obesity and risk of preterm delivery. JAMA 309(22), 2362–2370. https://doi.org/10.1001/jama.2013.6295 (2013).
Kawamoto, T. et al. Rationale and study design of the Japan environment and children’s study (JECS). BMC Public Health https://doi.org/10.1186/1471-2458-14-25 (2014).
Michikawa, T. et al. Baseline profile of participants in the Japan Environment and Children’s Study (JECS). J. Epidemiol. 28(2), 99–104. https://doi.org/10.2188/jea.JE20170018 (2018).
Figueiredo, B., Dias, C. C., Pinto, T. M. & Field, T. Infant sleep-wake behaviors at two weeks, three and six months. Infant. Behav. Dev. 44, 169–178. https://doi.org/10.1016/j.infbeh.2016.06.011 (2016).
Morokuma, S. et al. Non-reassuring foetal status and neonatal irritability in the Japan Environment and Children’s Study: a cohort study. Sci. Rep. 8(1), 15853. https://doi.org/10.1038/s41598-018-34231-y (2018).
Cox, J. L., Holden, J. M. & Sagovsky, R. Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. Br. J. Psychiatry 150, 782–786 (1987).
Yamashita, H. & Yoshida, K. Screening and intervention for depressive mothers of new-born infants. Seishin Shinkeigaku Zasshi. 105(9), 1129–1135 (2003).
Guangyong, Z. A modified poisson regression approach to prospective studies with binary data. Am. J. Epidemiol. 159, 702–706. https://doi.org/10.1093/aje/kwh090 (2004).
Acknowledgements
We would like to express our gratitude to all the participants in this study and all the individuals involved in data collection. The Japan Environment and Children's Study was funded by the Ministry of the Environment, Japan. The findings and conclusions of this article are solely the responsibility of the authors and do not represent the official views of the Ministry of the Environment.
Author information
Authors and Affiliations
Consortia
Contributions
Study concept and design: S.M. Statistical analyses: T.M. Drafting of the manuscript and approval of the final content: K.N., S.M. and T.M. Critical revision of the manuscript for important intellectual content: all authors. Manuscript review: all authors.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The Study Group members are listed at the end of this article.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Nakahara, K., Michikawa, T., Morokuma, S. et al. Association of maternal sleep before and during pregnancy with preterm birth and early infant sleep and temperament. Sci Rep 10, 11084 (2020). https://doi.org/10.1038/s41598-020-67852-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-67852-3
This article is cited by
-
Sleep pattern and disorders among pregnant women in Ibadan, Southwest Nigeria
BMC Women's Health (2024)
-
Influence of mothers’ nighttime responses on the sleep–wake rhythm of 1-month-old infants
Scientific Reports (2021)
-
Influence of physical activity before and during pregnancy on infant’s sleep and neurodevelopment at 1-year-old
Scientific Reports (2021)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.