Abstract
The outcome of periampullary adenocarcinomas remains poor with few treatment options. Podocalyxin-like protein (PODXL) is an anti-adhesive protein, the high expression of which has been shown to confer a poor prognosis in numerous malignancies. A correlation and adverse prognostic synergy between PODXL and the epidermal growth factor receptor (EGFR) has been observed in colorectal cancer. Here, we investigated whether this also applies to periampullary adenocarcinomas. We analyzed the immunohistochemical expression of PODXL and EGFR in tissue microarrays with tumors from two patient cohorts; (Cohort 1, n = 175) and (Cohort 2, n = 189). The effect of TGF-β-induced expression and siRNA-mediated knockdown of PODXL and EGFR, were investigated in pancreatic cancer cells (PANC-1) in vitro. We found a correlation between PODXL and EGFR in these cancers, and a synergistic adverse effect on survival. Furthermore, silencing PODXL in pancreatic cancer cells resulted in the down-regulation of EGFR, but not vice versa. Consequently, these findings suggest a functional link between PODXL and EGFR, and the potential combined utility as biomarkers possibly improving patient stratification. Further studies examining the mechanistic basis underlying these observations may open new avenues of targeted treatment options for subsets of patients affected by these particularly aggressive cancers.
Similar content being viewed by others
Introduction
The periampullary region includes the head of the pancreas, the distal bile duct, the ampulla of Vater and the periampullary duodenum. Adenocarcinomas developing in this region represent a heterogeneous group of tumors, wherein morphology appear to provide more prognostic information than the tumor origin, in that pancreatobiliary type (PB-type) differentiation is associated with a significantly shorter survival than intestinal type (I-type)1,2. Pancreatic cancer, the most common type of periampullary adenocarcinomas, has a 5-year overall survival of merely 7%3, the dismal prognosis partly due to a high rate of advanced tumor stages at the time of diagnosis4.
Podocalyxin-like protein (PODXL) is a member of the CD34 family of transmembrane glycoproteins consisting of a mucin-like extracellular domain and a cytoplasmic tail. PODXL is expressed on podocytes and the apical surface of glomerular epithelial cells of the kidney5, where it plays an important role in maintaining adequate filtration6, due to its anti-adhesive properties. Moreover, PODXL is involved in the regulation of cell adhesion and is expressed for instance on vascular endothelia7 and hematopoietic progenitor cells8,9. Aside from these normal conditions, PODXL has been found to be upregulated in various malignancies, and its strong expression, particularly in the cell membrane, associates with a more aggressive tumor phenotype and a poor prognosis in periampullary10, breast11, colorectal12,13,14,15 ovarian16, and bladder cancers17, as well as in glioblastoma18. The role of PODXL in tumorigenesis is unclear, but evidence suggests that PODXL is involved in epithelial-mesenchymal transition (EMT), a process by which epithelial cells acquire invasive and migratory properties and make them resistant to apoptosis19. EMT is regulated by various differentiation and growth factors, most importantly transforming growth factor β (TGF-β). When TGF-β is added to epithelial cells in culture, EMT will be induced20.
The epidermal growth factor receptor (EGFR) is a glycoprotein and a tyrosine kinase receptor, which belongs to the human epidermal growth factor receptor (HER) family. EGFR activation induces intracellular signaling-cascades important for growth, differentiation and cell survival21, all essential for tumor development. EGFR overexpression is common in several malignancies including cancers of the breast, ovary, bladder, kidney, lung and brain21. In pancreatic cancer, EGFR has been found to be overexpressed in 30–95% of the cases22,23 and associated with a poor prognosis24. Previous work has shown that high expression of PODXL and EGFR impair survival in colorectal cancer in a synergistic way25. This study thus aimed to investigate the relationship between the expression of PODXL and EGFR in periampullary adenocarcinomas, including pancreatic cancer, with focus on morphological subtypes. We also examined the functional interplay between PODXL and EGFR in pancreatic cancer cells in vitro.
Methods
Patients
Cohort 1
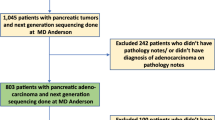
Cohort 1 is a previously described retrospective consecutive cohort of 175 patients with primary periampullary adenocarcinomas who were surgically treated with pancreaticoduodenectomy at the University hospitals of Lund and Malmö, Sweden, from 1 January 2001 through 31 December 201110,26,27,28,29. Morphologically, 110 cases were classified as PB-type and 65 cases as I-type adenocarcinomas. Fortysix of these 175 patients presented with pancreatic ductal adenocarcinoma. Data on survival were gathered from the Swedish National Civil Register and clinical data was obtained retrospectively from medical records. Follow-up began on the date of surgery and ended upon death or upon the final update in March 2017. Patients were identified through broad searches in the pathology database, and all haematoxylin and eosin (H&E) stained slides were re-evaluated by one pathologist (JEL), blinded to the original report and outcome, with the decision on tumor origin and morphological type being based on several criteria, as previously described26. The Ethics Committee of Lund University (ref no. 445/07) approved the study, whereby the committee waived the need for consent other than by opting out. Methods were carried out in accordance with relevant guidelines and regulations.
Cohort 2
Cohort 2 is a previously described retrospective cohort of 189 consecutive patients with pancreatic ductal adenocarcinoma undergoing surgery at the Department of Surgery, Helsinki University Hospital in Finland from 1 January 2000 through 31 December 201130,31. A majority of the tumors were of periampullary origin, however a small number of the tumors originated in cauda pancreatis. Patients who received neoadjuvant chemotherapy (n = 21) were excluded from the study. Data on survival and cause of death were gathered from medical records, Statistics Finland, and the Finnish Population Registry. The Surgical Ethics Committee of Helsinki University Central Hospital (Dnro HUS 226/E6/06, extension TMK02 §66 17.4.2013) approved the study. Permission to use tissue samples without individual informed consent was granted by the National Supervisory Authority of Health and Welfare (Valvira Dnro 10041/06.01.03.01/2012). Methods were carried out in accordance with relevant guidelines and regulations.
Tissue microarray construction
As previously described for Cohort 110, a semi-automated arraying device (TMArrayer, Pathology Devices, Westminister, MD, USA) was used for the construction of tissue microarrays (TMAs). Three tissue cores of 1 mm were sampled from each of the 175 primary tumors and from lymph node metastases from 105 of the cases. In addition, two tissue cores (1 mm) were obtained from adjacent benign-appearing pancreatic tissue in 50 cases with duodenal or ampullary cancer.
For Cohort 2, TMAs were constructed using a semiautomatic tissue microarrayer (Tissue Arrayer 1, Beecher Instruments Inc., Silver Spring, MD, USA). Two 1-mm cores were taken from representative areas of each of the 168 tumors. Fifteen cases were excluded from analysis due to inadequate or missing cores. All samples were re-evaluated by two experienced pathologists. Histological images of the tumor tissues from both cohorts were published elsewhere10,28,30.
Immunohistochemistry and staining evaluation
For immunohistochemical analysis of PODXL expression in Cohort 1, TMA sections of 4 μm were automatically pre-treated using the PT Link system, and then stained in an Autostainer Plus (DAKO; Glostrup, Copenhagen, Denmark) with a polyclonal anti-PODXL antibody (HPA2110, Atlas Antibodies AB, Stockholm, Sweden, diluted to 1: 250), as described elsewhere10. The expression of PODXL was recorded as negative (0), weak cytoplasmic positivity in any proportion of cells (1), moderate cytoplasmic positivity in any proportion of cells (2), distinct membranous positivity in ≤50% of cells (3) and distinct membranous positivity in>50% of cells (4)10,12,13,14,17, and dichotomized into low (0–2) or high (3–4). Staining evaluation was performed by two independent observers (MH and KJ), who were blinded to the clinical and outcome data.
Immunohistochemical technique and PODXL staining evaluation in Cohort 2 were described elsewhere30. The same polyclonal antibody (HPA 2110, Atlas Antibodies, Stockholm, Sweden) was used as that in Cohort 1.
For immunohistochemical analysis of EGFR in both cohorts, 4 μm TMA-sections were pre-treated using the PT-link system (Dako), and subsequently stained with a monoclonal anti-EGFR antibody (31G7, Zymed Laboratories Inc, San Francisco, CA, USA, diluted to 1:25) using the Autostainer Plus (Dako, Glostrup, Denmark). The evaluation of the EGFR protein expression in Cohort 1 was described elsewhere28 but was now performed on Cohort 2. The evaluation was performed using the recommended protocol for HER2 testing in gastric and gastroesophageal junction cancer biopsies32, taking complete, basolateral, or lateral membranous reactivity in a minimum of five clustered positive cancer cells into account. The intensity recorded was rated as 0, 1+, 2+ or 3+. Protein expression was grouped into low (0–2+) or high (3+) expression, as described elsewhere28. Cytoplasmic staining was grouped as 1+ in the statistical analyses. Staining evaluation was performed by three independent observers (MH, AL and KJ). Any inter-observer discrepancies were discussed in order to reach consensus. In Cohort 2, 10 cases were excluded from the analyses due to staining or interpretation problems with the EGFR antibody.
Cell culture
Human pancreatic cancer cell lines PANC-1 and human foetal foreskin fibroblasts (HFFF2) were purchased from Sigma-Aldrich and the growth medium, foetal bovine serum (FBS) and antibiotics were obtained from Nordic Biolabs. The cells were maintained in an RPMI1640 or DMEM medium supplemented with 10% FBS and antibiotics (100 U/ml penicillin and 100 μg/ml streptomycin) in a humidified 5% CO2 atmosphere at 37°C. All in vitro reagents were purchased from ThermoFisher Scientific unless stated otherwise. All in vitro experiments were repeated at least three times.
siRNA transfection
Pancreatic cancer cells were seeded in T-25 flasks (5×105 cells) and incubated for 72 hours in 37°C for siRNA transfection. Subsequently, the cells were washed twice with phosphate buffered saline (PBS) and received the medium without FBS, together with lipofectamine 2000 and the negative control, anti-PODXL (s10770 + s10771) or anti-EGFR (s563 + s565) siRNA in OptiMEM to a final siRNA concentration of 25 nM. After 4.5 hours, the transfection was stopped, and the medium changed to a full-growth medium. The cells were then left to recover overnight, and the next day, cells were harvested and spun down to pellets. The pellets were either resuspended in Trizol and stored at −20°C for qPCR, or fixated, dehydrated and embedded in paraffin for immunohistochemistry.
TGF- β incubation
For TGF-β incubation, pancreatic cancer cells were seeded in T-25 flasks (5×105 cells), incubated for 72 hours at 37°C, and then incubated with TGF-β (10 ng/ml) for 48 hours. Following this, the cells were harvested and spun down to pellets. The pellets were either resuspended in Trizol and stored at −20°C for qPCR, or fixated, dehydrated and embedded in paraffin for immunohistochemistry.
Organotypic assay
The method of designing an organotypic assay was described elsewhere33. Twenty-four hours after siRNA transfection or TGF-β incubation, the 3D organotypic model was prepared according to Moutasim et al. and Froeling et al.34,35. Prior to making the gel (7 parts Collagen I, 1 part DMEM 10×, 1 part FBS and 1 part regular DMEM growth medium), inserts (3 μm pores) in a 24-wells plate were coated with collagen. The gel was made from 3.5 parts Collagen I, 3.5 parts Matrigel, 1 part DMEM 10×, 1 part FBS and 1 part cell suspension (containing 2.5×104 HFFF2 cells) and added to each collagen-coated insert. The gels were left to incubate for 1 hour at 37 C, and following gel polymerization, the cancer cells (5×104) were harvested and mixed with HFFF2 (2.5×104) and seeded on top of the gels. Subsequently, the medium was added to the wells and the organotypic model was incubated overnight at 37 C. After overnight incubation, the medium was removed from the wells and inserts and the medium was added to the well up to the bottom of the insert to create an air-liquid interface. Every two to three days, the medium was changed, and after incubation for seven days, the gels were fixated in 4% paraformaldehyde and paraffin embedded. Sections (3-μm-thick) of the gels were stained with H&E for the visualization of cancer cell invasion. For TGF-β incubated cells prior to the model, gel sections were also stained for PODXL or EGFR using the same antibodies as those used for tissue samples. Representative pictures of one out of three individual repeats were taken with cellSens dimension software at 20x magnification. The rate of invasion in the gel was based on estimates of the observed number of cells entering the gel, and not formally quantified.
Immunohistochemistry
TMAs were constructed from the paraffin-embedded cell pellets, and the staining of PODXL and EGFR was performed in the same manner as the tissue samples. The cell pellets were used to visualize protein expression under the different conditions tested in vitro.
qPCR
The method of qPCR has been described elsewhere33. To remove the cell debris, the cell samples were thawed and spun down. According to the manufacturer’s instructions, RNA purification was performed using Trizol with phasemaker tubes. Thereafter, RNA cleanup was performed using the RNeasy minelute kit (QIAGEN) and the RNA concentration was determined using Qubit with the RNA HS kit. cDNA reverse transcription was performed using the high-capacity cDNA reverse transcription kit, prior to qPCR, and the total cDNA concentration was determined using Qubit with the DNA HS kit. Ten ng per reaction of each sample was used to run qPCR with the PODXL or EGFR TaqMan gene expression assay (Assay ID Hs01574644_m1 and Hs01076090_m1, respectively), with samples run in triplicates. 18 S served as the endogenous control (Assay ID Hs039288985_g1).
Statistical analysis
In Cohort 1, three patients were excluded from the survival analyses; two with I-type adenocarcinomas who died within one month of surgery due to complications and one with PB-type adenocarcinoma who emigrated five months after surgery. Another two patients with PB-type adenocarcinomas who had received neoadjuvant chemotherapy were excluded from the survival analyses since the treatment might have affected the expression of PODXL. The Kaplan Meier analysis and log-rank test were applied to illustrate differences in overall survival (OS) with respect to PODXL and EGFR expression. The p-value was based on a pairwise comparison. Cox regression proportional hazard models were used to estimate hazard ratios (HRs) for death in both univariable and multivariable analysis, adjusted for tumor grade, T-stage (T1–2 vs. T3–4), N-stage (N0 vs. N1), perineural growth, blood vessel invasion, lymphatic invasion, the invasion of peripancreatic fat, adjuvant treatment, and for morphological type in Cohort 1, and adjusted for tumor grade, T-stage (T1–2 vs. T3–4), N-stage (N0 vs. N1), perineural growth, blood vessel invasion, and adjuvant treatment in Cohort 2. The proportional hazard (PH) assumption was tested graphically by using log-minus-log plots. The PH assumption was also evaluated using the Cox regression analysis with a time-dependent covariate analysis, whereby the PH assumption was considered to be satisfied when the factor-by-time interaction was not significant. All statistical analyses were performed using IBM SPSS Statistics version 22.0 (SPSS Inc., Chicago, IL, USA). All tests were two-sided and we considered p-values <0.05 significant.
Results
PODXL and EGFR expression
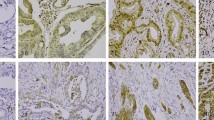
A significant correlation between the expression of PODXL and EGFR was identified in both cohorts, as well as in the stratified analysis according to morphological subtype (Fig. 1). The associations of clinicopathological factors with PODXL and EGFR expressions in Cohort 110,28 and with PODXL in Cohort 230 were described elsewhere.
Correlations between the immunohistochemical expression of PODXL and EGFR. Bar charts visualizing the correlations between low vs. high (0 vs. 1) PODXL and low vs. high (0 vs. 1) EGFR. The top row shows the correlations for Cohort 1, for the entire cohort and divided into morphological subtypes. The bottom row shows the correlations for Cohort 2.
Clinical outcome related to the combined strata of PODXL and EGFR expression
Cohort 1
As Fig. 2 shows, the Kaplan-Meier analysis revealed that patients with tumors displaying high levels of both PODXL and EGFR exhibited the shortest OS in the entire cohort and in tumors with an I-type morphology. This was, however, not seen in PB-type tumors. As shown in Table 1, the high PODXL expression served as an independent predictor of a diminished OS across the entire cohort, among both patients with low EGFR tumors (HR 1.84; 95% CI 1.09–3.12), and among patients with high EGFR tumors (HR 1.78; 95% CI 1.03–3.07). The highest risk of death was observed among patients with I-type tumors displaying a high expression of both PODXL and EGFR (unadjusted HR 2.90; 95% CI 1.03–8.18), and this association remained significant in the adjusted analysis (HR 4.77; 95% CI 1.02–22.33). We considered the PH assumption satisfied using the graphic evaluation of log-minus-log plots (data not shown). Moreover, the time-dependent covariate was not significant for PODXL and EFGR, and therefore, the factor x time interaction term was dropped from the model.
Overall survival according to PODXL and EGFR expressions in Cohort 1. Kaplan-Meier estimates for the overall survival according to the combined strata of low and high PODXL and EGFR expression in Cohort 1, shown for the entire cohort, for PB-type and I-type tumors. The p-value was based on a pairwise comparison with PODXL-/EGFR- and PODXL+/EGFR+.
Cohort 2
As demonstrated in Fig. 3, the Kaplan-Meier analysis found that a high PODXL expression, in combination with a high EGFR expression, correlated with a significantly reduced overall survival (p = 0.017) compared to patients without the overexpression of the two proteins. These results mirror those in Cohort 1. However, as shown in Table 2, a high PODXL expression did not associate with a reduced overall survival, irrespective of EGFR expression.
Overall survival according to PODXL and EGFR expressions in Cohort 2. Kaplan-Meier estimates for the overall survival in pancreatic ductal adenocarcinoma according to the combined strata of low and high expression of PODXL and EGFR in Cohort 2. The p-value was based on a pairwise comparison with PODXL-/EGFR- and PODXL+/EGFR+.
Effects of TGF-β incubation and the siRNA-mediated silencing of PODXL and EGFR in pancreatic cancer cells in vitro
In addition to the results found in both cohorts, functional studies were performed in vitro using PANC-1 pancreatic cancer cells either transfected with siRNA against PODXL (siPODXL) or EGFR (siEGFR), or incubated with TGF-β. Figure 4A displays the protein expression under different conditions in the 3D organotypic model and cell pellets. In the top row, where cells were incubated with TGF-β alone, we found an increasing invasion following TGF-β incubation. This was visualized in the H&E staining by the greater number of cells entering the gel compared to the control. In addition, the expression of PODXL was more prominent along the invasive front, however, the protein expression of EGFR was fairly unchanged (second and third row; inserts show immunocytochemistry on the cell pellets). Furthermore, the mRNA levels of PODXL and EGFR were successfully transiently knocked down in PANC-1 cells by siRNA (Fig. 4B). Here, the siPODXL-transfected cells were reduced in both PODXL and EGFR, whereas the siEGFR-transfected cells alone appeared reduced in EGFR. Following TGF-β incubation, the PODXL mRNA levels showed a fourfold increase and EGFR was somewhat reduced (Fig. 4C). To examine the combined effect of TGF-β and siRNA on PODXL and EGFR expression, PANC-1 cells were incubated with TGF-β following siRNA transfection (bottom two rows of Fig. 4A, and Fig. 4D). As shown in Fig. 4A, EGFR expression disappeared following the combination of siPODXL and TGF-β, whereas PODXL expression increased after the combination of siEGFR and TGF-β. This was also visible at the mRNA level, where the combination of siPODXL and TGF-β incubation resulted in a reduction in EGFR, and siEGFR together with TGF-β greatly enhanced the PODXL expression (Fig. 4D). This confirms that PODXL appears to influence EGFR expression but not vice versa and, furthermore, that PODXL suppression can prevent the overexpression induced by TGF-β.
Effects of TGF-β incubation and siRNA-mediated silencing of PODXL and EGFR in pancreatic cancer cells. (A) 3D organotypic model of the PANC-1 cell line on gel sections, as visualized in an H&E stain (top row), without (left column) and after (right column) incubation with TGF-β. As shown in the second row, the expression of PODXL increases upon incubation with TGF-β, particularly along the invasive front (inserts show the immunocytochemistry on cell pellets). The third row shows that the expression of EGFR does not markedly change upon incubation with TGF-β. The fourth row shows the EGFR protein expression in siPODXL silenced PANC-1 cells and the bottom panel shows PODXL protein expression in siEGFR silenced PANC-1 cells. (B) qPCR demonstrating the mRNA levels of PODXL and EGFR in siPODXL and siEGFR PANC-1 cell line. (C) qPCR demonstrating the mRNA levels of PODXL and EGFR in TGF-β incubated PANC-1 cell line. (D) qPCR demonstrating mRNA levels of PODXL and EGFR where PANC-1 cells were incubated with TGF-β following siRNA transfection.
Discussion
The prognosis for patients with pancreatic and other periampullary adenocarcinomas remains poor with few treatment options. Thus, identifying biomarkers to better understand and define this group of tumors in a clinically relevant context is important. In this translational study we investigated PODXL and EGFR and demonstrated a significant relationship between the overexpression of these proteins in pancreatic and other periampullary adenocarcinomas. In the cohort comprising the full range of periampullary cancers, this association was particularly evident in I-type tumors, whereas in PB-type tumors, all patients exhibited a similarly poor prognosis. However, in Cohort 2, which comprised only ductal pancreatic cancer, patients with tumors overexpressing both PODXL and EGFR exhibited a significantly shorter overall survival. The association between the overexpression of PODXL and EGFR seen in I-type periampullary tumors was not confirmed in PB-type tumors or in pancreatic cancer in Cohort 2 in the Cox regression analysis, further indicating that I-type tumors resemble and should be treated as colorectal cancer25.
The results from the tumor analyses were further verified through the in vitro data. Incubation with TGF-β rendered pancreatic cancer cells seemingly more invasive, leading to an increased expression of PODXL, particularly at the invasive front. This confirms that PODXL is markedly increased during TGF-β-induced EMT, a process associated with cell migration and increased invasion, as previously described by e.g. Meng et al.19 and Fröse et al.36. In addition, TGF-β has been associated with EMT in pancreatic cancer37, representing a central pathway in the development of pancreatic cancer38,39,40. The influence of TGF-β on PODXL and tumor aggressiveness might provide an explanation of the mechanism indicative of the association between high PODXL and reduced survival among patients. For instance, a study by Javle et al.41 demonstrated that a high plasma level of TGF-β1 was associated with diminished survival among patients with advanced pancreatic cancer. Notably in our study, while the knockdown of PODXL reduced EGFR expression, PODXL levels were not affected by the knockdown of EGFR. This was further confirmed in the presence of TGF-β, where siPODXL prevented an increase in PODXL and EGFR but siEGFR played no effect on protein expression. This agrees with our findings in both cohorts, where high PODXL expressing tumors were also more likely to display high levels of EGFR. Furthermore, EGFR signaling has been shown to take part in cancer progression, in that EGFR overexpression leads to enhanced invasiveness through the loss of E-cadherin42. Accordingly, inhibiting EGFR may affect EMT and inhibit cancer cell migration, although the association between EGFR and EMT is not as apparent as it is for PODXL. Moreover, the relationship between PODXL and EGFR is not fully understood, but previous in vitro studies have demonstrated a possible interaction through the Na+/H+ Exchanger Regulatory Factor (NHERF) proteins. Expression of PODXL leads to the induction of the NHERF proteins to the surface of the epithelial cell43. On the cell surface, NHERF-1 has been demonstrated to stabilize EGFR, thus restricting receptor downregulation, leading to enhanced EGFR signaling44.
The response to EGFR inhibitors in e.g. non-small cell lung cancer depends upon specific EGFR mutations45, which are rare in pancreatic cancer22. Furthermore, in a phase III trial among patients with locally advanced or metastatic pancreatic cancer, the EGFR expression did not predict the response to the EGFR tyrosine kinase inhibitor erlotinib, when added to gemcitabine46. In addition, a study by Izumchenko et al.47 demonstrated a mechanism of how resistance to erlotinib may develop. During TGF-β-mediated EMT the microRNAs 200 (miR200) family was inhibited and the expression of the mitogen-inducible gene 6 (MIG6), which is a negative regulator of EGFR, was upregulated, thus leading to resistance to erlotinib. The interaction between PODXL and EGFR and the potential role of PODXL in upregulating EGFR found in the present study is noteworthy, and it would be of interest to explore if PODXL expression affects the response to anti-EGFR directed therapy.
Since periampullary cancers encompass several different tumor origins, a pancreatic cancer cell line was chosen for the in vitro portion of this study. This decision was made based on the fact that pancreatic cancer represented the largest subset of cancers among the periampullary tumors in Cohort 1, whereby Cohort 2 only includes ductal pancreatic cancers. The cell line, PANC-1, used here was obtained from a ductal pancreatic carcinoma from a 56-year old Caucasian male48. The tumor cells are TP53- and KRAS- mutated, but SMAD-4 wild type. Mutations in the tumor suppressor gene TP53 and the proto-oncogene KRAS lead to cell cycle deregulation, inhibition of apoptosis, cell invasion, metastasis and poor treatment response, all essential in tumor development. Other cell lines currently used to study pancreatic carcinogenesis include MIA PaCa-2 and BxPC-3. When designing this study, these other cell lines were considered. However, the MIA PaCa-2 cell line has an impaired TGF-βR2 status, thus rendering it unsuitable for the experimental setting with TGF-β stimulation used herein, and BxPC-3 is KRAS wild-type48. Since KRAS mutations occur in almost all primary tumors of pancreatic cancer, and appear early in the progression of the disease, this cell line was also deemed unsuitable49.
One strength of this study stems from its use of two well-characterized, consecutive, and comparatively large patient cohorts with periampullary adenocarcinomas, including pancreatic cancer, both spanning over the same period of time. The cohorts were kept separate whereby the use of two different cohorts can be considered a validation of the results. Furthermore, given the fact that differentiation of tumor origin can be difficult in the clinical setting, using the morphological type in treatment decisions is crucial. All histological samples were re-evaluated by experienced pathologists, and clinical follow-up and survival data were reliable and up-to-date.
A potential limitation to this study lies in the use of TMA, since this technique, although being a well-validated method50, may not reflect heterogeneous biomarker expression. However, the analysis of one whole tissue section will also merely reflect a small portion of the tumor, and sampling of tissue cores from multiple donor blocks, carried out in this study, may provide a more representative picture of the entire tumor.
We have previously demonstrated that patients with I-type, but not PB-type, tumors displaying high expression of PODXL benefitted from adjuvant chemotherapy10. Furthermore, in patients with PB-type tumors receiving adjuvant gemcitabine, high expression of EGFR was significantly associated with a shorter overall survival and recurrence free survival, with a significant treatment interaction in relation to OS28. These findings suggest that adjuvant treatment has a limited or no effect on survival in patients with PB-type tumors with a high EGFR and PODXL expression. Speculatively, the inhibition of EGFR might serve as an alternative treatment option for these patients.
References
Westgaard, A. et al. Pancreatobiliary versus intestinal histologic type of differentiation is an independent prognostic factor in resected periampullary adenocarcinoma. BMC cancer 8, 170, https://doi.org/10.1186/1471-2407-8-170 (2008).
Bronsert, P. et al. Intestinal-type of differentiation predicts favourable overall survival: confirmatory clinicopathological analysis of 198 periampullary adenocarcinomas of pancreatic, biliary, ampullary and duodenal origin. BMC cancer 13, 428, https://doi.org/10.1186/1471-2407-13-428 (2013).
Siegel, R. L., Miller, K. D. & Jemal, A. Cancer statistics, 2016. CA: a cancer journal for clinicians 66, 7–30, https://doi.org/10.3322/caac.21332 (2016).
Herreros-Villanueva, M., Hijona, E., Cosme, A. & Bujanda, L. Adjuvant and neoadjuvant treatment in pancreatic cancer. World journal of gastroenterology 18, 1565–1572, https://doi.org/10.3748/wjg.v18.i14.1565 (2012).
Kerjaschki, D., Sharkey, D. J. & Farquhar, M. G. Identification and characterization of podocalyxin–the major sialoprotein of the renal glomerular epithelial cell. The Journal of cell biology 98, 1591–1596 (1984).
Doyonnas, R. et al. Anuria, omphalocele, and perinatal lethality in mice lacking the CD34-related protein podocalyxin. The Journal of experimental medicine 194, 13–27 (2001).
Horvat, R., Hovorka, A., Dekan, G., Poczewski, H. & Kerjaschki, D. Endothelial cell membranes contain podocalyxin–the major sialoprotein of visceral glomerular epithelial cells. The Journal of cell biology 102, 484–491 (1986).
Doyonnas, R. et al. Podocalyxin is a CD34-related marker of murine hematopoietic stem cells and embryonic erythroid cells. Blood 105, 4170–4178, https://doi.org/10.1182/blood-2004-10-4077 (2005).
McNagny, K. M. et al. Thrombomucin, a novel cell surface protein that defines thrombocytes and multipotent hematopoietic progenitors. The Journal of cell biology 138, 1395–1407 (1997).
Heby, M., Elebro, J., Nodin, B., Jirstrom, K. & Eberhard, J. Prognostic and predictive significance of podocalyxin-like protein expression in pancreatic and periampullary adenocarcinoma. BMC clinical pathology 15, 10, https://doi.org/10.1186/s12907-015-0009-1 (2015).
Somasiri, A. et al. Overexpression of the anti-adhesin podocalyxin is an independent predictor of breast cancer progression. Cancer research 64, 5068–5073, https://doi.org/10.1158/0008-5472.CAN-04-0240 (2004).
Larsson, A. et al. Overexpression of podocalyxin-like protein is an independent factor of poor prognosis in colorectal cancer. British journal of cancer 105, 666–672, https://doi.org/10.1038/bjc.2011.295 (2011).
Larsson, A. H. et al. Validation of podocalyxin-like protein as a biomarker of poor prognosis in colorectal cancer. BMC Cancer 12, 282, https://doi.org/10.1186/1471-2407-12-282 (2012).
Larsson, A. H. et al. Podocalyxin-like protein expression in primary colorectal cancer and synchronous lymph node metastases. Diagnostic pathology 8, 109, https://doi.org/10.1186/1746-1596-8-109 (2013).
Kaprio, T. et al. Podocalyxin is a marker of poor prognosis in colorectal cancer. BMC Cancer 14, 493, https://doi.org/10.1186/1471-2407-14-493 (2014).
Cipollone, J. A. et al. The anti-adhesive mucin podocalyxin may help initiate the transperitoneal metastasis of high grade serous ovarian carcinoma. Clinical & experimental metastasis 29, 239–252, https://doi.org/10.1007/s10585-011-9446-0 (2012).
Boman, K. et al. Membranous expression of podocalyxin-like protein is an independent factor of poor prognosis in urothelial bladder cancer. British journal of cancer 108, 2321–2328, https://doi.org/10.1038/bjc.2013.215 (2013).
Binder, Z. A. et al. Podocalyxin-like protein is expressed in glioblastoma multiforme stem-like cells and is associated with poor outcome. PloS one 8, e75945, https://doi.org/10.1371/journal.pone.0075945 (2013).
Meng, X., Ezzati, P. & Wilkins, J. A. Requirement of podocalyxin in TGF-beta induced epithelial mesenchymal transition. PloS one 6, e18715, https://doi.org/10.1371/journal.pone.0018715 (2011).
Miettinen, P. J., Ebner, R., Lopez, A. R. & Derynck, R. TGF-beta induced transdifferentiation of mammary epithelial cells to mesenchymal cells: involvement of type I receptors. The Journal of cell biology 127, 2021–2036, https://doi.org/10.1083/jcb.127.6.2021 (1994).
Arteaga, C. L. The epidermal growth factor receptor: from mutant oncogene in nonhuman cancers to therapeutic target in human neoplasia. Journal of clinical oncology: official journal of the American Society of Clinical Oncology 19, 32S–40S (2001).
Oliveira-Cunha, M., Newman, W. G. & Siriwardena, A. K. Epidermal growth factor receptor in pancreatic cancer. Cancers 3, 1513–1526, https://doi.org/10.3390/cancers3021513 (2011).
Xiong, H. Q. & Abbruzzese, J. L. Epidermal growth factor receptor-targeted therapy for pancreatic cancer. Seminars in oncology 29, 31–37, https://doi.org/10.1053/sonc.2002.35645 (2002).
Ueda, S. et al. The correlation between cytoplasmic overexpression of epidermal growth factor receptor and tumor aggressiveness: poor prognosis in patients with pancreatic ductal adenocarcinoma. Pancreas 29, e1–8 (2004).
Larsson, A. H. et al. Significant association and synergistic adverse prognostic effect of podocalyxin-like protein and epidermal growth factor receptor expression in colorectal cancer. Journal of translational medicine 14, 128, https://doi.org/10.1186/s12967-016-0882-0 (2016).
Elebro, J. & Jirstrom, K. Use of a standardized diagnostic approach improves the prognostic information of histopathologic factors in pancreatic and periampullary adenocarcinoma. Diagnostic Pathology 9, 80, https://doi.org/10.1186/1746-1596-9-80 (2014).
Fristedt, R. et al. Reduced expression of the polymeric immunoglobulin receptor in pancreatic and periampullary adenocarcinoma signifies tumour progression and poor prognosis. PloS one 9, e112728, https://doi.org/10.1371/journal.pone.0112728 (2014).
Elebro, J. et al. Expression and Prognostic Significance of Human Epidermal Growth Factor Receptors 1, 2 and 3 in Periampullary Adenocarcinoma. PloS one 11, e0153533, https://doi.org/10.1371/journal.pone.0153533 (2016).
Elebro, J. et al. Prognostic and treatment predictive significance of SATB1 and SATB2 expression in pancreatic and periampullary adenocarcinoma. Journal of translational medicine 12, 289, https://doi.org/10.1186/s12967-014-0289-8 (2014).
Saukkonen, K. et al. Podocalyxin Is a Marker of Poor Prognosis in Pancreatic Ductal Adenocarcinoma. PloS one 10, e0129012, https://doi.org/10.1371/journal.pone.0129012 (2015).
Saukkonen, K. et al. PROX1 and beta-catenin are prognostic markers in pancreatic ductal adenocarcinoma. BMC cancer 16, 472, https://doi.org/10.1186/s12885-016-2497-5 (2016).
Ruschoff, J. et al. HER2 testing in gastric cancer: a practical approach. Modern pathology: an official journal of the United States and Canadian Academy of Pathology, Inc 25, 637–650, https://doi.org/10.1038/modpathol.2011.198 (2012).
Karnevi, E. et al. Translational study reveals a two-faced role of RBM3 in pancreatic cancer and suggests its potential value as a biomarker for improved patient stratification. Oncotarget 9, 6188–6200, https://doi.org/10.18632/oncotarget.23486 (2018).
Moutasim, K. A., Nystrom, M. L. & Thomas, G. J. Cell migration and invasion assays. Methods Mol Biol 731, 333–343, https://doi.org/10.1007/978-1-61779-080-5_27 (2011).
Froeling, F. E., Marshall, J. F. & Kocher, H. M. Pancreatic cancer organotypic cultures. Journal of biotechnology 148, 16–23, https://doi.org/10.1016/j.jbiotec.2010.01.008 (2010).
Frose, J. et al. Epithelial-Mesenchymal Transition Induces Podocalyxin to Promote Extravasation via Ezrin Signaling. Cell reports 24, 962–972, https://doi.org/10.1016/j.celrep.2018.06.092 (2018).
Nakajima, S. et al. N-cadherin expression and epithelial-mesenchymal transition in pancreatic carcinoma. Clinical cancer research: an official journal of the American Association for Cancer Research 10, 4125–4133, https://doi.org/10.1158/1078-0432.CCR-0578-03 (2004).
Pickup, M., Novitskiy, S. & Moses, H. L. The roles of TGFbeta in the tumour microenvironment. Nature reviews. Cancer 13, 788–799, https://doi.org/10.1038/nrc3603 (2013).
Derynck, R., Akhurst, R. J. & Balmain, A. TGF-beta signaling in tumor suppression and cancer progression. Nature genetics 29, 117–129, https://doi.org/10.1038/ng1001-117 (2001).
Hahn, S. A. et al. DPC4, a candidate tumor suppressor gene at human chromosome 18q21.1. Science 271, 350–353, https://doi.org/10.1126/science.271.5247.350 (1996).
Javle, M. et al. Biomarkers of TGF-beta signaling pathway and prognosis of pancreatic cancer. PloS one 9, e85942, https://doi.org/10.1371/journal.pone.0085942 (2014).
Barr, S. et al. Bypassing cellular EGF receptor dependence through epithelial-to-mesenchymal-like transitions. Clinical & experimental metastasis 25, 685–693, https://doi.org/10.1007/s10585-007-9121-7 (2008).
Li, Y., Li, J., Straight, S. W. & Kershaw, D. B. PDZ domain-mediated interaction of rabbit podocalyxin and Na(+)/H(+) exchange regulatory factor-2. American journal of physiology. Renal physiology 282, F1129–1139, https://doi.org/10.1152/ajprenal.00131.2001 (2002).
Lazar, C. S., Cresson, C. M., Lauffenburger, D. A. & Gill, G. N. The Na+/H+ exchanger regulatory factor stabilizes epidermal growth factor receptors at the cell surface. Molecular biology of the cell 15, 5470–5480, https://doi.org/10.1091/mbc.E04-03-0239 (2004).
Lynch, T. J. et al. Activating mutations in the epidermal growth factor receptor underlying responsiveness of non-small-cell lung cancer to gefitinib. The New England journal of medicine 350, 2129–2139, https://doi.org/10.1056/NEJMoa040938 (2004).
Moore, M. J. et al. Erlotinib plus gemcitabine compared with gemcitabine alone in patients with advanced pancreatic cancer: a phase III trial of the National Cancer Institute of Canada Clinical Trials Group. Journal of clinical oncology: official journal of the American Society of Clinical Oncology 25, 1960–1966, https://doi.org/10.1200/JCO.2006.07.9525 (2007).
Izumchenko, E. et al. The TGFbeta-miR200-MIG6 pathway orchestrates the EMT-associated kinase switch that induces resistance to EGFR inhibitors. Cancer research 74, 3995–4005, https://doi.org/10.1158/0008-5472.CAN-14-0110 (2014).
Deer, E. L. et al. Phenotype and genotype of pancreatic cancer cell lines. Pancreas 39, 425–435, https://doi.org/10.1097/MPA.0b013e3181c15963 (2010).
Luttges, J. et al. The K-ras mutation pattern in pancreatic ductal adenocarcinoma usually is identical to that in associated normal, hyperplastic, and metaplastic ductal epithelium. Cancer 85, 1703–1710 (1999).
Torhorst, J. et al. Tissue microarrays for rapid linking of molecular changes to clinical endpoints. The American journal of pathology 159, 2249–2256, https://doi.org/10.1016/S0002-9440(10)63075-1 (2001).
Acknowledgements
This study was supported by grants from the Swedish Research Council, the Swedish Cancer Society, the Mrs Berta Kamprad Foundation, Region Skåne Regional research grants, Governmental Funding for Clinical Research within the National Health Service (ALF), Lund University Faculty of Medicine, Skåne University Hospital Funds and Donations, Helsinki University Hospital Research Grants and the Sigrid Jusélius Foundation. Open access funding provided by Lund University.
Author information
Authors and Affiliations
Contributions
M.H. collected the clinical data, annotated the immunohistochemical staining, performed the statistical analyses and drafted the manuscript. E.K. performed experiments, analyzed the data and contributed reagents, materials and analytical tools. J.E.L. collected clinicopathological data, assisted with TMA construction, evaluated immunohistochemical stainings and performed statistical analyses. B.N. constructed the tissue microarrays and performed the IHC stainings. J.E.B. collected the clinical data and conceived the study. K.S. performed experiments, analyzed the data and contributed reagents, materials and analytical tools. J.H. performed experiments and contributed reagents, materials and analytical tools. H.M. analyzed the data and contributed reagents, materials and analytical tools. H.S. contributed reagents, materials and analytical tools. C.H. conceived and designed the experiments. K.J. supervised the project, evaluated the immunohistochemical stainings and helped draft the manuscript. A.L. designed the experiments, evaluated the immunohistochemical staining and helped draft the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Heby, M., Karnevi, E., Elebro, J. et al. Additive clinical impact of epidermal growth factor receptor and podocalyxin-like protein expression in pancreatic and periampullary adenocarcinomas. Sci Rep 10, 10373 (2020). https://doi.org/10.1038/s41598-020-67187-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-67187-z
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.