Abstract
Abnormal gut-brain interactions are common in irritable bowel syndrome (IBS), but the associations between neurophysiological measures and their relation to gastrointestinal (GI) symptoms are poorly understood. Our aim was to explore these relationships and define the most relevant neurophysiology measures for GI symptom severity in IBS. IBS patients underwent small intestinal motility (manometry; fasted and fed contraction frequency, phase III time) and secretion (transmural potential difference), rectal sensorimotor (barostat; sensory thresholds, tone response, compliance), autonomic nervous system (baroreceptor sensitivity and effectiveness), and colonic motor function (transit time) examinations. GI symptom severity (GSRS-IBS), and anxiety and depression (HAD) as a proxy measure of central nervous system (CNS) dysfunction, were assessed. In total 281 IBS patients (Rome II criteria) were included (74% females, median age 36 [interquartile range 28–50] years). Significant correlations between neurophysiology measures were stronger within, rather than between, different neurophysiological examinations. The strongest neurophysiology-symptom correlations occurred between a combination of CNS and visceral sensitivity parameters, and GSRS-IBS total score and pain domain (ρ = 0.40, p < 0.001, and ρ = 0.38, p < 0.001). Associations between GI symptoms in IBS and individual and combinations of neurophysiological factors occurred, primarily in CNS and visceral sensitivity measures, providing new insights into the clinical presentation of IBS.
Similar content being viewed by others
Introduction
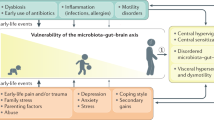
Irritable bowel syndrome (IBS) is a common and complex functional gastrointestinal (GI) disorder where gut-brain interactions1,2, and alterations in the gut microenvironment3 are considered to be central in the pathophysiology. Abdominal pain, related to defecation and associated with changes in stool form or frequency, are the characteristic clinical features of this female predominant disease1 with 5–10% prevalence worldwide4,5,6. The disease leads to high costs for society, due to increased use of health care services7, as well as lowered work productivity and higher absenteeism from work8,9.
Different abnormalities involved in gut-brain interactions are present in IBS, leading to a complex clinical presentation, but to date the pathophysiology is not completely understood. Various pathophysiological factors have been brought forward as important for symptom generation in IBS, but none of these is present in all patients with IBS. IBS patients have been reported to have increased psychological distress10,11, visceral hypersensitivity12, altered colonic motility13, aberrant autonomic nervous system (ANS) function14,15, rectal sensorimotor dysfunction16,17, and dysfunction of motility18,19,20 and secretion21 of the small intestine, in comparison with healthy controls. Although these abnormalities have been described individually in IBS, the associations among these aberrant measures, and the interactions between these parameters and the patient reported IBS symptom severity, have to this date not been thoroughly studied. Associations between overall IBS symptom severity and psychiatric comorbidities22,23 or visceral hypersensitivity12,17,24,25,26 have been previously demonstrated. The link between overall IBS symptom severity and altered colonic motility is less obvious, as associations with abnormal bowel habits, but not other GI symptoms, have been the most commonly reported finding13,27. However, for the other neurophysiological factors, the association with symptom severity in IBS is even less clear.
Since the interaction among the different neurophysiological alterations demonstrated in IBS is incompletely understood, achieving a better understanding of the interactions between the reported symptoms and the complex clinical presentation of IBS is of importance to improve the clinical management of these patients. In line with the concept that IBS is a disorder of gut-brain interactions1,2, associations between the patient reported GI symptom severity and individual neurophysiological factors involved in gut-brain interactions were assessed. Specifically, we included psychological distress as a proxy measure for CNS dysfunction11,28, rectal sensorimotor function, small intestinal motility, small intestinal secretion, colonic motility, and baroreceptor (BR) sensitivity as a proxy for ANS function15,29, or combinations thereof, in a large group of well-characterized IBS patients in multivariable analyses. The aim of this study was to explore the relationships among these factors and to extract the most important variables for symptom generation in IBS, in order to expand our understanding of the complex clinical presentation of IBS.
Results
Descriptives
The total cohort of IBS patients (N = 281) consisted of 74% females, and had a median age of 36 years, as shown in Table 1. IBS-D was the most common IBS subtype (43%), followed by IBS-A (32%) and IBS-C (25%). The median anxiety and depression levels of the patient cohort were in the normal range30 and did not differ between subgroups, and the median scores of the GSRS-IBS domains were mostly in the range of moderate symptom severity31. The median values of the 16 neurophysiological factors used in this study are presented in Table 2. Only few and predominantly expected differences were seen between IBS subgroups; severity of diarrhoea and constipation, colonic transit time, total phase III time in the small bowel, and the mean value of the transmural potential difference in the small intestine. Hence, no division of patients into IBS subgroups were made for further analyses.
Correlations among neurophysiological factors and IBS symptoms
Correlations were calculated among the neurophysiological factors and IBS symptoms in the whole cohort (N = 281), as can be seen in Fig. 1. The strongest correlations were mainly seen between different measures within the same neurophysiological examinations, e.g. factors of rectal tone (ρ = 0.68), small intestinal secretion (ρ = 0.54), visceral sensitivity (ρ = 0.52) and rectal compliance (ρ = 0.46). Weaker, but significant (p < 0.05), correlations were noted between some of the different neurophysiological measurements with ρ-values in the range of 0.2 to 0.3. The measures with the highest number of associations were the GSRS-IBS bloating domain, the rectal pain threshold and psychological distress.
Correlations between the neurophysiological factors from the overall cohort of IBS patients (N = 281). Significant correlations between neurophysiological factors are shown in the figure (p < 0.05, two-tailed, unadjusted for multiple comparisons). Numbers represent Spearman´s rho. Green edges show positive correlations, whereas red edges show negative correlations. BR: Baroreceptor; GSRS-IBS: Gastrointestinal Symptom Rating Scale, IBS version; HAD: Hospital Anxiety and Depression scale; SI: Small intestine/intestinal.
Regarding associations between GI symptom severity and individual neurophysiological measures, significant (p < 0.05) correlations were seen mainly with psychological distress and rectal sensitivity variables. No significant (p < 0.05) correlations were detected between GI symptoms and small intestinal motility, small intestinal secretion, rectal tone response or ANS function. The strongest correlations were seen between rectal sensitivity and GSRS-IBS pain and GSRS-IBS diarrhoea (ρ = 0.30 and ρ = 0.26, respectively), and colonic transit time and GSRS-IBS constipation and GSRS-IBS diarrhoea (ρ = 0.27 and ρ = −0.27, respectively). Psychological distress demonstrated modest associations with all GSRS-IBS domains, whereas moderately strong associations were seen between the different GSRS-IBS domains (ρ = 0.23–0.48).
Multivariate analyses
All study participants who had completed GSRS-IBS, i.e. the dependent variables, were included in the multivariate analyses (N = 193). The 16 neurophysiological factors were first processed to form the overall neurophysiology score. The Lasso scores for the domains and total score of GSRS-IBS, respectively, were then calculated through a summation of the Lasso-extracted combination of variables from the overall neurophysiology score, as can be seen in Table 3.
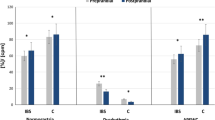
A correlation heatmap was created to visualize the correlations between the GSRS-IBS total and domain scores of GSRS-IBS, and the single neurophysiological factors, as well as the overall neurophysiology score or Lasso scores (Fig. 2). The correlation coefficients and p values of the heatmap are presented in Supplementary Table 1. In general, most of the GSRS-IBS scores (total score and domain scores) had stronger correlations with the Lasso scores than with the overall neurophysiology score, although only moderately strong associations were detected (Fig. 3). The strongest correlation was found between GSRS-IBS total score and the corresponding Lasso score (ρ = 0.40, p < 0.001), which consisted of HAD and the rectal pain threshold (Table 3). The second strongest correlation was seen between GSRS-IBS pain and the corresponding Lasso score (ρ = 0.38, p < 0.001), which consisted of the same neurophysiological factors as the Lasso score of GSRS-IBS total score. GSRS-IBS diarrhoea and GSRS-IBS satiety also showed significant (p < 0.05), but modest, correlations with their respective Lasso scores. After the false discovery rate (FDR) correction, a small number of correlations lost their significance. These associations were evenly distributed among the different neurophysiological examinations, as seen in Supplementary Table 1.
Heatmap of correlations in the overall cohort of IBS patients (N = 281), between GSRS-IBS total score and domain scores of GSRS-IBS, and single neurophysiological factors, the overall neurophysiology scores, or the Lasso scores, respectively. The specified correlation coefficients and p values are available in Supplementary Table 1. BR: baroreceptor; GSRS-IBS: Gastrointestinal Symptom Rating Scale, IBS version; HAD: Hospital Anxiety and Depression scale; Lasso: Least Absolute Selection and Shrinkage Operator regression; overall: Neurophysiology scores derived from all 16 neurophysiological factors; PD; potential difference; SI: small intestine/intestinal.
Comparisons of correlations between neurophysiology scores (overall neurophysiology score or Lasso scores) and GSRS-IBS total score and domain scores of GSRS-IBS in the overall cohort of IBS patients (N = 281). All correlations are significant (p < 0.05, two-tailed, false discovery rate adjusted for multiple comparisons), with the exceptions of Constipation - overall, Constipation – Lasso, Diarrhoea - overall and Satiety - overall. For specified p values, see Supplementary Table 1. GSRS-IBS: Gastrointestinal Symptom Rating Scale, IBS version; Lasso: Least Absolute Selection and Shrinkage Operator regression-derived neurophysiology scores; overall: Neurophysiology scores derived from all 16 neurophysiological factors.
Discussion
In this study, the correlations among IBS symptoms and a wide range of neurophysiological factors were explored to gain knowledge of the associations between symptoms and the complex pathophysiology of IBS and to extract the most relevant neurophysiology measures for GI symptom severity in IBS. Modest associations were seen among some of the different neurophysiological factors, and between some of the neurophysiological factors and GI symptoms. The associations between combinations of neurophysiological factors and GI symptoms were stronger, but the benefit of this approach relative to assessing the neurophysiological factors individually was modest, further highlighting the complexity of symptom generation in IBS.
In previous studies, some individual neurophysiological factors used in this study have been linked to elevated symptom severity, although to the best of our knowledge, GI motility, secretion, sensitivity and ANS and CNS function have not been analysed simultaneously in IBS patients before. Therefore, the associations among these factors are largely unknown, even though some previous studies have presented links between some of these factors. Rectal sensitivity has been found to be associated with rectal compliance32, the rectal tone response after meal intake33 and with baroreceptor sensitivity34. There is also a study that has demonstrated a link between rectal compliance and colonic transit time in IBS patients with urgency35. Therefore, due to the relative paucity of comprehensive and detailed neurophysiology assessment in IBS patients in the literature, the first set of analyses in this study explored associations between the different individual neurophysiological factors, as well as their association with IBS symptoms. The overall finding from these analyses showed associations between different measures within the same neurophysiological examination, e.g. between rectal sensory thresholds during balloon distensions, even though significant (p < 0.05), but weaker, associations were seen between measures from different neurophysiological measurements. When assessing the association with IBS symptom severity, modest associations between individual neurophysiology measures and symptom severity were noted, mainly confirming previous findings with associations between symptoms and visceral hypersensitivity, colonic transit and psychological distress in IBS12,13,24,36. Furthermore, the absence of associations with small intestinal motility and secretory measures, as well as rectal tone response and ANS variables, is noteworthy. The analysis approach used in this study is limited by the inability to articulate on the cause and effect between the different neurophysiological aberrancies and the severity of GI symptoms seen in the patient cohort, although it is well suited for the exploration of associations between measures.
Our hypothesis for the creation of the neurophysiology scores was that the neurophysiological factors could influence symptoms through different, but complimentary mechanisms, and therefore have additive effects on IBS symptoms. Furthermore, we hypothesized that even slight changes in the neurophysiological factors could lead to symptom generation through interactions. Based on these assumptions, we included all values deviating from the mean into the conjunct neurophysiology score in the analysis, creating a score where a value close to zero would indicate a normally functioning gut, including its interactions with ANS and CNS, and a high score would reflect many or high aberrant values in neurophysiological examinations as a proxy indicator of an abnormal gut-brain interaction. In previous studies from our group assessing individual neurophysiological factors included in this study, IBS patients have shown abnormalities in all of these factors relative to healthy controls, namely small intestinal motility20 small intestinal secretion21, ANS function37 colonic transit time13, rectal sensorimotor function12,33 and psychological distress38. For some, but not all of these, modest associations with IBS symptom severity were noted.
The variable reduced neurophysiology scores (Lasso scores) were found to correlate stronger with GI symptoms than the scores originating from all factors combined, i.e. the overall neurophysiology score. However, the gain was modest. There are several potential explanations for this. The limited range of the scales of the outcome measures (GSRS-IBS) might limit the level of detail in the results. The variable selection technique, Lasso regression, was chosen in accordance with previous studies39,40 to achieve an automatic variable selection. If the characteristics of the training set and the test set in the regression analysis are divergent, the variable selection might result in a suboptimal association with the whole cohort, i.e. the training and test sets combined. Furthermore, the Lasso regression has been described to occasionally choose the next-to-best combination of variables41 if there are more than one combination of variables with high predictive value. Lastly, as IBS has been proposed to consist of several diseases or subgroups with similar symptoms due to its heterogeneity42,43, a clearer association between GI symptoms and neurophysiological factors might arise when studying more homogenous subgroups of patients44. This way of extracting important factors for symptom generation in IBS, might be useful in future identification of new IBS subgroups, rather than subgrouping IBS patients solely based on the predominant bowel habit.
Two of the neurophysiological factors were present in every variable reduced neurophysiology score; the proxy measure of CNS function, i.e. psychological distress, and visceral sensitivity parameters, which implicate that they were the most important factors for the GI symptom pattern in this patient cohort. These two parameters were also seen to be central in the network analysis seen in Fig. 1, as they had the largest number of associations to other measures. The neurophysiology scores for GSRS-IBS total score and GSRS-IBS pain consisted of only these two factors, which is in accordance with previous studies, where these two pathophysiological factors have been shown to be of importance for symptom severity in IBS12,24,38. With this study, we have strengthened the view on psychological distress and visceral hypersensitivity as central factors for symptom generation in IBS. This is also in agreement with the findings from a recent publication from our group36, where a proportion of the subjects from this study was included (n = 137), in addition to patients from two other large patient cohorts. In that study, the focus was on visceral hypersensitivity, psychological distress and colonic transit, whereas the present study included a larger number of neurophysiological factors, albeit in a smaller cohort.
To provide a comprehensive model of the gut-brain axis, i.e. the bidirectional communication between the CNS, ANS and the enteric nervous system45, proxy measures of the function of the CNS and ANS were included among the neurophysiological variables, which may be viewed as a limitation. As the function of the ANS is only assessable through indirect measures such as heart rate variability37,46 or BR function, the BR sensitivity (BRS) was used in this study as a proxy measure of ANS function14,15,34, together with the BR effectiveness index, as it has been suggested to provide complementary information to the BRS47. The HAD scale is a widely used questionnaire assessing psychological distress, which has previously been used as a proxy measure for CNS function48,49, as we did in this study. Although it is widely used, it provides an incomplete measure of the whole function of the CNS.
To increase the validity or accuracy of the neurophysiology score, replacement or addition of certain neurophysiological factors could be discussed. The assessment of CNS dysfunction could be improved with addition of brain imaging, which could provide both structural50 and functional information about the CNS51. Furthermore, including heart rate variability and other ANS measures could strengthen the assessment of the ANS function52. Moreover, more detailed assessment of GI motor, sensory and secretory function at different levels in the GI tract could be considered. Lastly, addition of measures of gut microbiota composition and GI immune and barrier function3 to the most important factors for GI symptoms demonstrated in this study, could further broaden the pathophysiological assessment, potentially leading to a more precise prediction of GI symptoms in IBS patients. Although an addition of more variables would increase the risk of noise in the model, a computerized reduction of variables, such as the Lasso method used in this study, would nonetheless extract the relevant measures for GI symptom severity.
Another limitation of this study might be the choice of analysis methods, as association analyses are well suited for the exploration of correlations between measures, but is unfit for unravelling cause and effect between the different neurophysiological aberrancies and the severity of GI symptoms seen in the patient cohort.
To conclude, modest associations between GI symptoms, and individual as well as combinations of neurophysiological factors were seen in this study. The results from this study provides new insights into the complex interactions between symptom severity and neurophysiological measures in IBS. Further studies with an expanded range of neurophysiological variables of importance for symptom generation in IBS can be considered. However, inclusion of other factors putatively involved in the pathophysiology of IBS, such as the microbiome and GI immune and barrier function, in addition to the most important factors for symptom generation found in this study, might provide an even more complete picture of the associations between pathophysiological factors and GI symptoms in IBS.
Methods
Study participants
IBS patients, 18–65 years old, with IBS according to Rome II criteria53, were included for participation in a study assessing the relevance of various pathophysiological factors for IBS symptoms between the years of 2002–2007 in our outpatient clinic specialized in functional GI disorders at Sahlgrenska University hospital, Gothenburg, Sweden12,13,33. This study is a retrospective assessment of all the neurophysiology measures and GI symptom data available from this patient cohort. This cohort has been included in previous publications from our group, but with different research questions and/or focus on only a proportion of all the neurophysiology measurements included in the analyses in this study12,13,21,24,33,36,37. Most of the patients were referred to our unit from primary care. The diagnosis of IBS was confirmed by an experienced gastroenterologist (MS), and if considered necessary, additional investigations to rule out organic GI disorders were performed. Any medication with known effects on the GI system was discontinued prior to the investigations. The patients were subdivided into IBS subgroups, i.e. constipation-predominant IBS (IBS-C), diarrhoea-predominant IBS (IBS-D) or alternating IBS (IBS-A)53. Exclusion criteria were other gastrointestinal diseases explaining the abdominal symptoms, severe physical or psychiatric disease, or pregnancy. The Regional Ethical Review Board at the University of Gothenburg approved the study (Approval number S489-02) and all patients received oral and written information about the study and provided informed consent prior to inclusion. The study was carried out in accordance with the guidelines and regulations of the Declaration of Helsinki.
Questionnaires
The patients completed the Gastrointestinal Symptom Rating Scale, IBS version (GSRS-IBS)31 for assessment of GI symptom severity. The Hospital Anxiety and Depression scale (HAD)30, which is a measure of psychological distress, e.g. anxiety and depression, in non-psychiatric patients, was also completed by the patients and in this study used as a proxy for CNS dysfunction. For details, see Supplementary material.
Neurophysiology measures
Rectal sensorimotor function
Rectal sensitivity, and compliance, as well as the rectal tone response after meal intake were assessed during a rectal balloon distension protocol by using an electronic barostat (Dual Drive Barostat, Distender Series II; G&J Electronics). The pressure thresholds for the first sensation and pain during the balloon distensions in the fasting state were used in this study as measures of visceral sensitivity12. After the first sequence of distensions, the patients ingested a standardized meal, and the early (0–25 minutes) and late (25–50 minutes) rectal tone responses were calculated from the average change in percent in the rectal balloon volume at the operating pressure. The rectal static and dynamic compliance of the rectum were calculated from the pressure-volume curve during first five distension steps of the balloon distension sequence33. The details about this protocol can be found as Supplementary material.
Small bowel motility and secretion
After an overnight fast, the patients were transnasally intubated with a 8-channel multilumen polyvinyl tube (Arndorfer Inc., Greendale, WI, USA). The motility and secretion of the small bowel were examined with a jejunal manometry catheter, with saline liquid infusion acting as a flowing electrode, during a 3 h fasting recording and 1 h after ingestion of a standardized meal, as described in detail in the Supplementary material. The mean fasted and fed contraction frequencies from the motility recordings were used in the analyses, as well as the total phase III time, consisting of the total time with phase III activity in seconds during the three hours long examination period during fasting. Furthermore, the mean and maximum transmural potential difference, as well as the rate of rise of the potential difference were calculated, as measures of reactivity of secretomotor neurons (small intestinal secretion)21.
Autonomic nervous system function
The BR function, in this study used as a measure for ANS function54, was assessed through a simultaneous electrocardiography, arterial blood pressure and heart rate recording. The baroreceptor sensitivity and baroreceptor effectiveness index29, as described in detail in the Supplementary material, were used in the analysis of this study.
Colonic motility
Colonic transit time was used as an indirect measure of colonic motility and was measured using a technique with radio-opaque markers, as described in the Supplementary material. In this study, the overall colonic transit time in days was used for the analysis13.
Data analysis and statistics
Descriptives
Demographic factors derived from the whole IBS cohort are described by medians with interquartile range in continuous variables, and numbers with percentages in categorical variables. The calculations were made in R (version 3.5.1 - “Feather Spray”). Chi squared tests or Kruskal-Wallis tests with two-tailed p-values were performed to compare medians between IBS subgroups. A p-value <0.05 was considered significant.
Correlations among neurophysiological factors and IBS symptoms
Analyses of correlations between the GSRS-IBS total score and the domain scores of GSRS-IBS (pain, bloating, constipation, diarrhoea and satiety), and the neurophysiological factors (rectal sensorimotor function, small bowel motility and secretion, ANS and CNS function, and colonic motility) were calculated with Spearman’s correlation. For this we used the cor function in the stats package in R. The analyses were visualized, uncorrected for multiple comparisons, through a correlation network made by the qgraph function in the qgraph package in R. Two-tailed p-values for the correlations were calculated through the corr.test function in the psych package in R. A p-value <0.05 was considered significant.
Multivariate analyses
Multivariate analyses were performed in order to determine if a combination of neurophysiological factors (neurophysiology score) would show stronger associations with the GI symptom severity than the individual neurophysiological factors. As presented below, two different processes, one with variable selection and one without, were used for calculation of neurophysiology scores, which were then analysed regarding their associations with IBS symptom severity.
Preprocessing of data
The patients who had completed the outcome variables GSRS-IBS were included in the multivariate analyses. The missing values of the dataset were imputed by multiple imputation, as implemented in missForest package in R.
Overall neurophysiology score
A neurophysiology score was created, using all of the 16 different neurophysiologic factors (overall neurophysiology score) in each patient. The neurophysiologic factors were first standardized by the mean (z-scores) and then individually processed. The aim of the processing step was to create a neurophysiology score where a normally functioning gut would be reflected with a score close to zero, whereas many or high aberrancies would give a high total score. All values that were different from the mean in each parameter added to or subtracted from the overall neurophysiology score, as seen in Table 4. Specifically, values considered as abnormal, e.g. a low pain threshold, increased the overall neurophysiology score, whereas values, which were considered normal, e.g. a low value of psychological distress or a high rectal pain threshold, decreased the overall neurophysiology score. After the processing step, the processed values of all of the neurophysiological factors were added up in each patient, resulting in an overall neurophysiology score.
Neurophysiology score using variable selection
In addition to the overall neurophysiology score described above, scores consisting of selected variables were also calculated for each of the GSRS-IBS domains and the total score, in order to see if this is process would lead to stronger associations with the GI symptom severity measures. The Least Absolute Selection and Shrinkage Operator regression model (Lasso) was used as the variable selection method39,40. The six neurophysiology scores consisting of selected measures for each of the GI symptom severity measures (GSRS-IBS total score and the five GSRS-IBS domain scores) are called ‘Lasso scores’ throughout this manuscript. The Lasso regression analysis is described in detail in the Supplementary material.
Correlations between neurophysiology scores and IBS symptoms
As the last step, Spearman’s correlations were calculated between the domains and total score of GSRS-IBS, and all single neurophysiological factors, and the neurophysiology scores (i.e. the overall neurophysiology score and the Lasso scores). The correlations were done with the cor function in the stats package and were illustrated as a heatmap, made by the heatmap.2 function in the gplots package in R, and a barplot. Two-tailed p-values for the correlations (p < 0.05) were calculated by the cor.test function in the stats package, and were adjusted for multiple comparisons with false discovery rate (FDR) adjustment. The heatmap illustrated the correlations between the domains and total score of GSRS-IBS, and the single neurophysiological factors, the overall neurophysiology score and the Lasso scores. The barplot compared the correlations between the domains and total score of GSRS-IBS and the overall neurophysiology score vs. the Lasso scores.
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author upon request.
References
Lacy, B. E. et al. Bowel Disorders. Gastroenterology. 150, 1393–1407 (2016).
Drossman, D. A. & Hasler, W. L. Rome IV—Functional GI Disorders: Disorders of Gut-Brain Interaction. Gastroenterology 150, 1257–1261 (2016).
Öhman, L., Törnblom, H. & Simrén, M. Crosstalk at the mucosal border: Importance of the gut microenvironment in IBS. Nature Reviews Gastroenterology and Hepatology 12, 36–49 (2015).
Palsson, O. S. et al. Development and validation of the Rome IV diagnostic questionnaire for adults. Gastroenterology 150, 1481–1491 (2016).
Lovell, R. M. & Ford, A. C. Global Prevalence of and Risk Factors for Irritable Bowel Syndrome: A Meta-analysis. Clinical Gastroenterology and Hepatology 10, 712–721.e4 (2012).
Enck, P. et al. Irritable bowel syndrome. Supplementary information. Nat. Rev. Dis. Prim. 2, 16014 (2016).
Canavan, C., West, J. & Card, T. Review article: The economic impact of the irritable bowel syndrome. Aliment. Pharmacol. Ther. 40, 1023–1034 (2014).
Zacker, C., Chawla, A. J., Wang, S. & Albers, L. A. Absenteeism among employees with irritable bowel syndrome. Manag. Care Interface 17, 28–32 (2004).
Frändemark, Å., Törnblom, H., Jakobsson, S. & Simrén, M. Work Productivity and Activity Impairment in Irritable Bowel Syndrome (IBS): A Multifaceted Problem. Am. J. Gastroenterol. 113, 1540–1549 (2018).
Fond, G. et al. Anxiety and depression comorbidities in irritable bowel syndrome (IBS): a systematic review and meta-analysis. Eur. Arch. Psychiatry Clin. Neurosci. 264, 651–60 (2014).
Roohafza, H. et al. Anxiety, depression and distress among irritable bowel syndrome and their subtypes: An epidemiological population based study. Adv. Biomed. Res. 5, 183 (2016).
Posserud, I. et al. Altered Rectal Perception in Irritable Bowel Syndrome Is Associated With Symptom Severity. Gastroenterology 133, 1113–1123 (2007).
Törnblom, H. et al. Colonic transit time and IBS symptoms: What’s the link? Am. J. Gastroenterol. 107, 754–760 (2012).
van der Veek, P. P. J. et al. Viscerosensory-cardiovascular reflexes: altered baroreflex sensitivity in irritable bowel syndrome. Am. J. Physiol. Integr. Comp. Physiol. 289, R970–R976 (2005).
Davydov, D. M., Naliboff, B., Shahabi, L. & Shapiro, D. Baroreflex mechanisms in Irritable Bowel Syndrome: Part I. Traditional indices. Physiol. Behav. 157, 102–108 (2016).
Steens, J., Van Der Schaar, P. J., Penning, C., Brussee, J. & Masclee, A. A. M. Compliance, tone and sensitivity of the rectum in different subtypes of irritable bowel syndrome. Neurogastroenterol. Motil. 14, 241–247 (2002).
Van der Veek, P. P. J., Van Rood, Y. R. & Masclee, A. A. M. Symptom Severity but Not Psychopathology Predicts Visceral Hypersensitivity in Irritable Bowel Syndrome. Clin. Gastroenterol. Hepatol. 6, 321–328 (2008).
Kellow, J. E. & Phillips, S. F. Altered small bowel motility in irritable bowel syndrome is correlated with symptoms. Gastroenterology 92, 1885–1893 (1987).
Kellow, J. E., Phillips, S. F., Miller, L. J. & Zinsmeister, A. R. Dysmotility of the small intestine in irritable bowel syndrome. Gut 1236–1243 (1988).
Simrén, M., Castedal, M., Svedlund, J., Abrahamsson, H. & Björnsson, E. Abnormal propagation pattern of duodenal pressure waves in the irritable bowel syndrome (IBS). Dig. Dis. Sci. 45, 2151–2161 (2000).
Larsson, M. H. et al. Elevated motility-related transmucosal potential difference in the upper small intestine in the irritable bowel syndrome. Neurogastroenterol. Motil. 19, 812–820 (2007).
Cho, H. S. et al. Anxiety, depression and quality of life in patients with irritable bowel syndrome. Gut Liver 5, 29–36 (2011).
Thijssen, A. Y. et al. Dysfunctional Cognitions, Anxiety and Depression in Irritable Bowel Syndrome. J. Clin. Gastroenterol. 44, e236–e241 (2010).
Simrén, M. et al. Visceral hypersensitivity is associated with GI symptom severity in functional GI disorders: consistent findings from five different patient cohorts. Gut 67, 255–262 (2018).
Kanazawa, M. et al. Contributions of pain sensitivity and colonic motility to IBS symptom severity and predominant bowel habits. Am. J. Gastroenterol. 103, 2550–2561 (2008).
Le Nevé, B. et al. Lactulose Challenge Determines Visceral Sensitivity and Severity of Symptoms in Patients With Irritable Bowel Syndrome. Clin. Gastroenterol. Hepatol. 14, 226–233.e3 (2015).
Sadik, R., Björnsson, E. & Simrén, M. The relationship between symptoms, body mass index, gastrointestinal transit and stool frequency in patients with irritable bowel syndrome. Eur. J. Gastroenterol. Hepatol. 22, 102–108 (2010).
Elsenbruch, S. et al. Affective disturbances modulate the neural processing of visceral pain stimuli in irritable bowel syndrome: An fMRI study. Gut 59, 489–495 (2010).
Johansson, M. et al. Baroreflex effectiveness index and baroreflex sensitivity predict all-cause mortality and sudden death in hypertensive patients with chronic renal failure. J. Hypertens. 25, 163–168 (2007).
Zigmond, A. S. & Snaith, R. P. The hospital anxiety and depression scale. Acta Psychiatr. Scand. 67, 361–70 (1983).
Wiklund, I. et al. An Irritable Bowel Syndrome-Specific Symptom Questionnaire: Development and Validation. Scand. J. Gastroenterol. 38, 947–954 (2003).
Lee, K. J., Kim, J. H. & Cho, S. W. Relationship of underlying abnormalities in rectal sensitivity and compliance to distension with symptoms in irritable bowel syndrome. Digestion 73, 133–141 (2006).
Törnblom, H., Van Oudenhove, L., Tack, J. & Simrén, M. Interaction between preprandial and postprandial rectal sensory and motor abnormalities in IBS. Gut 63, 1441–1449 (2014).
Spaziani, R. et al. Vagal dysfunction in irritable bowel syndrome assessed by rectal distension and baroreceptor sensitivity. Neurogastroenterol. Motil. 20, 336–342 (2008).
Basilisco, G., De Marco, E., Tomba, C. & Cesana, B. M. Bowel Urgency in Patients With Irritable Bowel Syndrome. Gastroenterology 132, 38–44 (2007).
Simrén, M. et al. Cumulative Effects of Psychologic Distress, Visceral Hypersensitivity, and Abnormal Transit on Patient-reported Outcomes in Irritable Bowel Syndrome. Gastroenterology 157, 391–402.e2 (2019).
Polster, A. et al. Heart rate variability characteristics of patients with irritable bowel syndrome and associations with symptoms. Neurogastroenterol. Motil. 30, e13320 (2018).
Jerndal, P. et al. Gastrointestinal-specific anxiety: An important factor for severity of GI symptoms and quality of life in IBS. Neurogastroenterol. Motil. 22, 646–654 (2010).
Tap, J. et al. Identification of an Intestinal Microbiota Signature Associated With Severity of Irritable Bowel Syndrome. Gastroenterology 152, 111–123.e8 (2017).
Zeller, G. et al. Potential of fecal microbiota for early-stage detection of colorectal cancer. Mol. Syst. Biol. 10, 766–766 (2014).
Lund, K. V. The Instability of Cross-Validated Lasso. (2013).
Whitehead, W. E., Palsson, O. & Jones, K. R. Systematic review of the comorbidity of irritable bowel syndrome with other disorders: What are the causes and implications? Gastroenterology 122, 1140–1156 (2002).
Camilleri, M. Irritable bowel syndrome: how useful is the term and the ‘diagnosis’? Therap. Adv. Gastroenterol. 5, 381–386 (2012).
Polster, A. et al. Mixture model analysis identifies irritable bowel syndrome subgroups characterised by specific profiles of gastrointestinal, extraintestinal somatic and psychological symptoms. Aliment. Pharmacol. Ther. 46, 529–539 (2017).
Öhman, L. & Simrén, M. New insights into the pathogenesis and pathophysiology of irritable bowel syndrome. Dig. Liver Dis. 39, 201–215 (2007).
Mazurak, N., Seredyuk, N., Sauer, H., Teufel, M. & Enck, P. Heart rate variability in the irritable bowel syndrome: A review of the literature. Neurogastroenterol. Motil. 24, 206–216 (2012).
Di Rienzo, M. et al. Baroreflex effectiveness index: an additional measure of baroreflex control of heart rate in daily life. Am. J. Physiol. Integr. Comp. Physiol. 280, R744–R751 (2001).
Jarrett, M. E. et al. Anxiety and depression are related to autonomic nervous system function in women with irritable bowel syndrome. Dig. Dis. Sci. 48, 386–394 (2003).
Pinto-Sanchez, M. I. et al. Anxiety and depression increase in a stepwise manner in parallel with multiple FGIDs and symptom severity and frequency. Am. J. Gastroenterol. 110, 1038–1048 (2015).
Melkus, G. D., Weaver, K. R., Henderson, W. A., Sherwin, L. B. & Walitt, B. Neuroimaging the brain-gut axis in patients with irritable bowel syndrome. World J. Gastrointest. Pharmacol. Ther. 7, 320 (2016).
Mayer, E. A. et al. Brain imaging approaches to the study of functional GI disorders: A Rome Working Team Report. Neurogastroenterol. Motil. 21, 579–596 (2009).
Gunterberg, V. et al. Tu1437 Autonomic Nervous Function Assessed by Two Complementary Methods -Baroreceptor Sensitivity and Heart Rate Variability - in Patients With Irritable Bowel Syndrome (IBS). Gastroenterology 142, S–832 (2012).
Thompson, W. G. et al. Functional bowel disorders and functional abdominal pain. Gut 45, ii43–ii47 (1999).
Swenne, C. A. Baroreflex sensitivity: Mechanisms and measurement. Netherlands Hear. J. 21, 58–60 (2013).
Acknowledgements
This study was supported by the Swedish Research Council (grants 13409, 21691, 21692 and 521-2012-1741), AFA Insurance, unrestricted research grants from Ferring Pharmaceuticals and Danone Nutricia Research, and by the Faculty of Medicine, University of Gothenburg. Open access funding provided by University of Gothenburg.
Author information
Authors and Affiliations
Contributions
H.S., P.F., H.T. and M.S. conceived and designed research; M.S. and H.S. performed experiments; I.M. analysed data; I.M. and A.P. interpreted results of experiments; I.M. prepared figures; I.M., M.S. and H.T. drafted manuscript, I.M., A.P., H.S., P.F., H.T. and M.S. edited and revised manuscript, I.M., A.P., H.S., P.F., H.T. and M.S. approved final version of manuscript.
Corresponding author
Ethics declarations
Competing interests
Irina Midenfjord: No competing interest. Annikka Polster: No competing interest. Henrik Sjövall: No competing interest. Peter Friberg: No competing interest. Hans Törnblom has served as Consultant/Advisory Board member for Allergan, Allmiral and Shire. Magnus Simrén has received unrestricted research grants from Danone Nutricia and Ferring Pharmaceuticals, and served as a Consultant/Advisory Board member for AstraZeneca, Danone Nutricia, Nestlé, Almirall, Allergan, Albireo, Menarini, Glycom and Shire, and as a speaker for Tillotts, Takeda, Shire, Menarini, AlfaSigma, Biocodex, Alimentary Health, Allergan and Almirall.
Additional information
Disclosures Irina Midenfjord, Annikka Polster, Peter Friberg: No conflicts of interest, financial or otherwise, to disclose. Henrik Sjövall holds a patent (PC-EP-2016098) regarding principles for motor activity-based correction of PD signal. There are no commercial activities around this patent.
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Midenfjord, I., Polster, A., Sjövall, H. et al. Associations among neurophysiology measures in irritable bowel syndrome (IBS) and their relevance for IBS symptoms. Sci Rep 10, 9794 (2020). https://doi.org/10.1038/s41598-020-66558-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-66558-w
This article is cited by
-
Multi-omics profiles of the intestinal microbiome in irritable bowel syndrome and its bowel habit subtypes
Microbiome (2023)
-
Contribution of sex and gender roles to the incidence of post-infectious irritable bowel syndrome in a prospective study
Scientific Reports (2023)
-
Identifying threshold sizes for enlarged abdominal lymph nodes in different age ranges from about 200,000 individual’s data
Scientific Reports (2021)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.