Abstract
The association between maternal serum total bile acid (TBA) levels and small-for-gestational-age (SGA) infants is unclear. We investigated the association between various degrees of serum TBA levels and the risk of SGA infants in a Chinese population. The current study performed a cohort study among 11811 mothers with singleton pregnancy. Subjects were divided into seven categories according to maternal serum TBA levels. Interestingly, birth sizes were reduced, whereas the rate of SGA infants was increased across increasing categories of serum TBA. Compared to category 1, adjusted ORs (95%CI) for SGA infants were 0.99 (0.82–1.21) in category 2, 1.22 (0.97–1.53) in category 3, 1.99 (1.53–2.58) in category 4, 2.91 (2.16–3.93) in category 5, 4.29 (3.33–5.54) in category 6, and 9.01 (5.99–13.53) in category 7, respectively. Furthermore, adjusted ORs (95%CI) for SGA infants for each 1-SD increase in serum TBA levels were 1.36 (1.29–1.43) among all subjects, 2.40 (1.82–3.45) among subjects without cholestasis, and 1.13 (1.06–1.22) among subjects with cholestasis, respectively. These results suggest that gestational cholestasis increases the risk of SGA infants. Additionally, our results indicate strong, continuous associations of serum TBA levels below those diagnostic of cholestasis with a decreased birth sizes and an increased risk of SGA infants.
Similar content being viewed by others
Introduction
Intrahepatic cholestasis of pregnancy (ICP), also named gestational cholestasis, is defined as the presence of pruritus in combination with elevated serum total bile acid (TBA) levels (≥10 μmol/L). ICP is one of the most prevalent obstetric disease1,2. ICP occurs usually in the second half of pregnancy until delivery. The incidence of ICP ranges from 0.4% to 15% in different countries, ethnic populations and climatic conditions3,4. The majority of studies had demonstrated that ICP was associated with adverse maternal outcomes, including 3-fold increased risks of gestational diabetes mellitus and pre-eclampsia5,6,7. A large cohort study from Sweden showed that women with ICP had increased risks of later liver and biliary tree cancer, later specifically diabetes mellitus, later autoimmune-mediated and cardiovascular diseases after childbirth8. On the other hand, several epidemiological studies reported the association between ICP and the increased risks of adverse fetal outcomes, including spontaneous and iatrogenic preterm delivery, a low (<7) 5-minute Apgar score, respiratory distress syndrome, meconium-stained fluid, stillbirth and intrauterine fetal death3,9,10,11. In addition, a report on human and rodent animal demonstrated that ICP was also associated with sex-specific increased susceptibility to severe obese, diabetic phenotype with hepatosteatosis in adult offspring, indicating a programming effect of the high bile acid exposure in utero12,13.
Small for gestational age (SGA), defined as fetal weight less than the 10th percentile based on gender and gestational age, is one of the leading causes for stillbirth, neonatal death and perinatal morbidity14,15,16. Several epidemiological reports showed that the risks of autism in childhood and cardiovascular and metabolic diseases in adulthood were increased in people born with SGA17,18,19,20. Nevertheless, no report analyzed the association between ICP and an increased risk of SGA infants in a cohort study. It is more obscure whether maternal serum TBA levels less severe than that in cholestasis are associated with an increased risk of SGA infants.
The present study conducted a birth cohort study to investigate the risk of SGA infants associated with various degrees of serum TBA levels. The present study found that ICP elevated the risk of SGA infants. Additionally, our results indicate strong, continuous associations of serum TBA levels below those diagnostic of cholestasis with a decreased birth sizes and an increased risk of SGA infants.
Results
The demographic characteristics and laboratory measurements of study participants
The demographic characteristics of study participants were presented in Table 1. There were significant differences on maternal age, education, and mode of delivery among different groups (Table 1). No significant differences were observed on maternal pre-pregnancy BMI, parity, and gravidity among different groups (Table 1). The incidence of preeclampsia was significantly lower in the TBA <10 μmol/L group than those in the other two groups (Table 1). No significant differences were observed on the incidence of pregnancy-induced hypertension and gestational diabetes mellitus among different groups (Table 1). Maternal serum alanine transaminase concentrations, aspartate transaminase concentrations, serum total bilirubin concentrations, direct bilirubin concentrations, and indirect bilirubin concentrations were measured. Results showed that those were increased across the increasing serum TBA levels categories (Table 2).
Birth sizes among different groups
Subjects were divided into seven categories according to maternal serum TBA levels. Birth weight was compared among seven categories. As shown in Table 3, birth sizes, including birth weight, birth length, head circumference and chest circumference, were decreased across increasing categories of serum TBA levels. Gestational age was also compared among seven categories. Gestational age was reduced across increasing categories of serum TBA levels (Table 3).
Association between serum TBA as a categorical variable and the risk of SGA infants
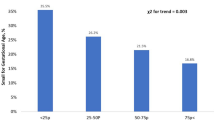
Participants were divided into seven categories according to maternal serum TBA levels. The rate of SGA infants across serum TBA levels categories is shown in Fig. 1. With increasing categories of maternal serum TBA levels, the rate of SGA infants was increased (Fig. 1). Table 4 shows the associations of maternal serum TBA levels as a categorical variable with each primary outcome, including odds ratios (ORs) and 95% confidence intervals (95%CIs) for each category, as compared with the lowest category. After adjustment for confounders, there were strong associations with SGA infants that increased across increasing categories of serum TBA levels. Additionally, there were no obvious thresholds at which risk increased (Table 4).
Rate of SGA infants. Serum TBA categories are as follows: category 1, less than 2.0 μmol/L; category 2, 2.0 to 3.9 μmol/L; category 3, 4.0 to 5.9 μmol/L; category 4, 6.0 to 7.9 μmol/L; category 5, 8.0 to 9.9 μmol/L; category 6, 10.0 to 39.9 μmol/L; category 7, 40 μmol/L or more. SGA, small for gestational age; TBA, total bile acid.
Association between serum TBA as a continuous variable and the risk of SGA infants and birth sizes
Table 5 shows the association between serum TBA as a continuous variable and the risk of SGA infants. Adjusted ORs for SAG infants for each 1-SD increase in serum TBA level were 1.36 (95%CI: 1.29, 1.43) among all subjects, 2.40 (95%CI: 1.82, 3.45) among subjects without cholestasis (TBA <10.0 μmol/L), and 1.13 (95%CI: 1.06, 1.22) among subjects with cholestasis (TBA ≥10.0 μmol/L), respectively (Table 5).
Discussion
The aim of the present study was to clarify the risk of SGA infants associated with various degrees of serum TBA levels, especially less severe than that in overt cholestasis in a birth cohort study. The present study found that birth sizes, including birth weight, birth length, head circumference and chest circumference, were decreased across increasing categories of serum TBA levels. The association between serum TBA and the risk of SGA infants was analyzed. After adjustment for confounders, there were strongly associations with SGA infants that increased across the increasing serum TBA levels categories.
Maternal demographic characteristics, such as maternal age, pre-pregnancy BMI, parity and maternal education, were associated with birth weight and the risk of SGA infants. A number of epidemiological studies demonstrated that advanced maternal age, primiparity and low BMI before pregnancy elevated the risks of SGA and low birth weight infants21,22,23. Several reports indicated that the risk of SGA was higher in low educational subjects compared with high educational subjects24,25. On the other hand, pregnancy complications, such as gestational diabetes mellitus, gestational hypertension and pre-eclampsia, were also associated with birth weight and the risk of SGA. Several reports showed that gestational hypertension and pre-eclampsia elevated the risk of SGA infants26,27. In contrast, gestational diabetes mellitus was significantly associated with higher birth weight and 2-fold increased risk of large for gestational age (LGA) infants and macrosomia28,29. The present study further estimated the adjusted ORs with 95%CI with respect to the incidence of SGA infants using multiple logistic regression models. After adjustment for these confounders, our results still found that the risk of SGA infants was increased across the increasing serum TBA levels categories.
The mechanism by which elevated serum TBA increases the risk of SGA remains obscure. Several case-control studies showed that the levels of proinflammatory cytokines and chemokines in placenta and maternal serum were significantly higher in the cholestasis group as compared to the control group30,31. Reports in vivo and in vitro found that bile acids stimulated the expression of a series of inflammatory cytokines and reactive oxygen species via activating both signal 1 and 2 of the NLRP3 inflammasome and NF-κB pathway32,33,34. These studies indicated that cholestasis was associated with inflammation and oxidative stress. Indeed, many epidemiological studies showed that maternal serum and umbilical cord serum TNF-α, C-reactive protein and IL-8 levels were significantly higher in the SGA group than in the control group35,36. According to a recent nest case-control study, strongly nuclear NF-κB p65 immunoreactivity was observed in placentas from pregnant women with SGA infants37. Animal experiments also found that maternal inflammation and oxidative stress resulted in FGR in rodents38,39. Therefore, we guess that inflammation and oxidative stress may play a vital role in TBA-mediated SGA. On the other hand, recent evidence suggested that the deficiency or downregulation of selective miRNA may be involved in placental-induced diseases, such as pre-eclampsia and fetal growth restriction, through the epigenetic mechanism40,41,42. Indeed, several studies found that bile acid, such as deoxycholic acid, inhibited miRNA expression in cell lines43,44. Consequently, we speculate downregulation of miRNA in placentas may be play a key role in TBA-mediated SGA. Moreover, a recent study reported that maternal serum TBA levels at diagnosis and at delivery were correlated positively with umbilical cord blood TBA levels, which provides evidence that bile acids could transport across the placenta45. Recently, numerous reports found that bile acids induced oncosis, necrotic cell death and apoptosis46,47. Thus, the present study does not exclude that elevated TBA-associated SGA is due to the direct toxic effect of bile acids.
The present study laid emphasis on whether serum TBA levels less severe than that in cholestasis was associated with an increased risk of SGA infants. However, the present study has three faults. Firstly, the nutritional status, drinking and smoking during pregnancy could affect fetal growth, but we did not have data on the variable. Secondly, the present cohort included only Chinese population, so our results should be treated cautiously when branched out to other ethnic populations. Another potential fault is the lack of information on treatment to pregnant women with cholestasis. Although previous reports demonstrated that treatment with ursodeoxycholic acid, a common drug for treating cholestasis during pregnancy, did not reduce adverse perinatal outcomes in pregnant women with ICP, it was associated with the reduction of serum TBA levels in ICP patients48,49.
In summary, the present study investigated the risk of SGA infants associated with various degrees of serum TBA levels in a large birth cohort study. The present study demonstrated that birth sizes were decreased across increasing categories of serum TBA levels. Further analysis found that ICP elevated the risk of SGA infants. Additionally, our results indicate strong, continuous associations of serum TBA levels below those diagnostic of cholestasis with a decreased birth sizes and an increased risk of SGA infants. There were no obvious thresholds at which risk increased. Thus, our study suggests the need to reconsider current criteria for diagnosing and treating ICP.
Subjects and Methods
Cohort study
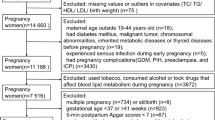
We conducted a retrospective birth cohort in Hefei, a city of central China21. Total 13801 pregnant women who delivered at First Affiliated Hospital of Anhui Medical University between January 2011 and December 2014 were recruited. Maternal demographic characteristics and obstetric records were recorded by midwives on the Birthing Outcomes System and all data included in the study was extracted from this database. Maternal nonfasting blood samples were obtained before labor. The exclusion criteria of the current study included the following: unavailable data of detailed delivery records (n = 897), fetal deaths or stillbirths (n = 270), pregnant women giving birth to multiple births (n = 294), induced-abortions (n = 147) and unavailable serum TBA data (n = 382). Finally, 11811 (85.6%) mothers with singleton pregnancy were eligible for this study. The present study obtained ethics approval from the ethics committee of Anhui Medical University (No. 20160010). All participants signed a written informed consent for this study. All methods were carried out in accordance with the approved guidelines.
Measurement of serum TBA
Serum TBA levels were measured using enzymatic cycling method by an automatic biochemical analyzer (Dirui CS-T300, Ltd, Changchun, China) according to a previous protocol50.
Definition of small-for-gestational age
The cutoff value used for defining the small-for-gestational age (SGA) is birth weight of live-born infants below the 10th percentile for gender and gestational age from a reference population for Chinese51.
Statistical analysis
SPSS 17.0 was used to analysis the data. The mean differences were analyzed using one-way ANOVA and least significant difference (LSD) post hoc test. Categorical variables were analyzed using χ2 tests. The median differences were analyzed using non-parametric statistics (Mann-Whitney U test). The incidence and odds ratio (OR) of SGA infants were calculated in different groups. Multiple logistic regression models were used to estimate the risks of SGA infants in relation to lowest TBA category by crude and adjusted ORs with 95% confidence intervals (95% CI). Linear regression was used to explore the association between serum TBA levels and birth sizes. A p-value of <0.05 (two-tailed) or a 95%CI not including 1 and 0 (for relative risk) was considered statistically significant.
References
Williamson, C. & Geenes, V. Intrahepatic cholestasis of pregnancy. Obstet. Gynecol. 124, 120–133 (2014).
Joshi, D., James, A., Quaglia, A., Westbrook, R. H. & Heneghan, M. A. Liver disease in pregnancy. Lancet 375, 594–605 (2010).
Lammert, F., Marschall, H. U., Glantz, A. & Matern, S. Intrahepatic cholestasis of pregnancy: molecular pathogenesis, diagnosis and management. J. Hepatol. 33, 1012–1021 (2000).
Geenes, V. & Williamson, C. Intrahepatic cholestasis of pregnancy. World. J. Gastroenterol. 15, 2049–2066 (2009).
Wikström-Shemer, E., Marschall, H. U., Ludvigsson, J. F. & Stephansson, O. Intrahepatic cholestasis of pregnancy and associated adverse pregnancy and fetal outcomes: a 12-year population-based cohort study. BJOG. 120, 717–723 (2013).
McIlvride, S., Dixon, P. H. & Williamson, C. Bile acids and gestation. Mol. Aspects. Med. 56, 90–100 (2017).
Rezai, S., Lora, I. & Henderson, C. E. Severe intrahepatic cholestasis of pregnancy is a risk factor for preeclampsia in singleton and twin pregnancies. Am. J. Obstet. Gynecol. 213, 395.e1–8 (2015).
Wikström Shemer, E. A. et al. Intrahepatic cholestasis of pregnancy and cancer, immune-mediated and cardiovascular diseases: A population-based cohort study. J. Hepatol. 63, 456–461 (2015).
Geenes, V. et al. Association of severe intrahepatic cholestasis of pregnancy with adverse pregnancy outcomes: a prospective population-based case-control study. Hepatology 59, 1482–1491 (2014).
Herrera, C. A. et al. Perinatal outcomes associated with intrahepatic cholestasis of pregnancy. J. Matern. Fetal Neonatal Med. 31, 1913–1920 (2018).
Puljic, A. et al. The risk of infant and fetal death by each additional week of expectant management in intrahepatic cholestasis of pregnancy by gestational age. Am. J. Obstet. Gynecol. 212, 667.e1–5 (2015).
Papacleovoulou, G. et al. Maternal cholestasis during pregnancy programs metabolic disease in offspring. J. Clin. Invest. 123, 3172–3181 (2013).
Desai, M. & Ross, M. G. Reproductive endocrinology: maternal cholestasis and offspring metabolic abnormalities. Nat. Rev. Endocrinol. 9, 567–568 (2013).
Blue, N. R. et al. A Comparison of Methods for the Diagnosis of Fetal Growth Restriction Between the Royal College of Obstetricians and Gynaecologists and the American College of Obstetricians and Gynecologists. Obstet. Gynecol. 131, 835–841 (2018).
Ray, J. G., Park, A. L. & Fell, D. B. Mortality in Infants Affected by Preterm Birth and Severe Small-for-Gestational Age Birth Weight. Pediatrics. 140, e20171881 (2017).
Yao, F., Miao, H., Li, B., Wu, Y. & Zhao, Q. New birthweight percentiles by sex and gestational age in Southern China and its comparison with the INTERGROWTH-21st Standard. Sci. Rep. 8, 7567 (2018).
Moore, G. S., Kneitel, A. W., Walker, C. K., Gilbert, W. M. & Xing, G. Autism risk in small- and large-for-gestational-age infants. Am. J. Obstet. Gynecol. 206, 314.e1–9 (2012).
Brøns, C., Saltbæk, P. N., Friedrichsen, M., Chen, Y. & Vaag, A. Endocrine and metabolic diurnal rhythms in young adult men born small vs appropriate for gestational age. Eur. J. Endocrinol. 175, 29–40 (2016).
Crispi, F. et al. Cardiovascular programming in children born small for gestational age and relationship with prenatal signs of severity. Am. J. Obstet. Gynecol. 207, 121.e1–9 (2012).
Glantz, A., Marschall, H. U. & Mattsson, L. A. Intrahepatic cholestasis of pregnancy: Relationships between bile acid levels and fetal complication rates. Hepatology 40, 467–474 (2004).
Chen, Y. H. et al. Pre-pregnancy underweight and obesity are positively associated with small-for-gestational-age infants in a Chinese population. Sci. Rep. 9, 15544 (2019).
Dzakpasu, S. et al. Contribution of prepregnancy body mass index and gestational weight gain to adverse neonatal outcomes: population attributable fractions for Canada. BMC. Pregnancy Childbirth 15, 21 (2015).
Kim, S. S. et al. Obstetric and Neonatal Risks Among Obese Women Without Chronic Disease. Obstet. Gynecol. 128, 104–112 (2016).
Fujiwara, T., Ito, J. & Kawachi, I. Income inequality, parental socioeconomic status, and birth outcomes in Japan. Am. J. Epidemiol. 177, 1042–1052 (2013).
Tamura, N. et al. Different Risk Factors for Very Low Birth Weight, Term-Small-for-Gestational-Age, or Preterm Birth in Japan. Int. J. Environ. Res. Public Health 15, 369 (2018).
Panaitescu, A. M. et al. Chronic hypertension and adverse pregnancy outcome: a cohort study. Ultrasound Obstet. Gynecol. 50, 228–235 (2017).
Hung, T. H., Hsieh, T. T. & Chen, S. F. Risk of abnormal fetal growth in women with early- and late-onset preeclampsia. Pregnancy Hypertens 12, 201–206 (2018).
Martino., J. et al. Maternal Body Weight and Gestational Diabetes Differentially Influence Placental and Pregnancy Outcomes. J. Clin. Endocrinol. Metab. 101, 59–68 (2016).
Lekva, T. et al. Prediction of Gestational Diabetes Mellitus and Pre-diabetes 5 Years Postpartum using 75 g Oral Glucose Tolerance Test at 14-16 Weeks’ Gestation. Sci. Rep. 8, 13392 (2018).
Shao, Y., Chen, J., Zheng, J. & Liu, C. R. Effect of Histone Deacetylase HDAC3 on Cytokines IL-18, IL-12 and TNF-α in Patients with Intrahepatic Cholestasis of Pregnancy. Cell. Physiol. Biochem. 42, 1294–1302 (2017).
Biberoglu, E. et al. Role of inflammation in intrahepatic cholestasis of pregnancy. J. Obstet. Gynaecol. Res. 42, 252–257 (2016).
Hao, H. et al. Farnesoid X Receptor Regulation of the NLRP3 Inflammasome Underlies Cholestasis-Associated Sepsis. Cell Metab. 25, 856–867.e5 (2017).
Li, M., Cai, S. Y. & Boyer, J. L. Mechanisms of bile acid mediated inflammation in the liver. Mol. Aspects Med. 56, 45–53 (2017).
Chen, W. et al. Obeticholic Acid Protects against Gestational Cholestasis-Induced Fetal Intrauterine Growth Restriction in Mice. Oxid. Med. Cell. Longev. 2019, 7419249 (2019).
Tosun, M. et al. Maternal and umbilical serum levels of interleukin-6, interleukin-8, and tumor necrosis factor-alpha in normal pregnancies and in pregnancies complicated by preeclampsia. J. Matern. Fetal Neonatal Med. 23, 880–886 (2010).
Amarilyo, G. et al. Increased cord serum inflammatory markers in small-for-gestational-age neonates. J. Perinatol. 31, 30–32 (2011).
Wang, H. et al. Maternal zinc deficiency during pregnancy elevates the risks of fetal growth restriction: a population-based birth cohort study. Sci. Rep. 5, 11262 (2015).
Chen, Y. H. et al. Obeticholic Acid Protects against Lipopolysaccharide-Induced Fetal Death and Intrauterine Growth Restriction through Its Anti-Inflammatory Activity. J. Immunol. 197, 4762–4770 (2016).
Chen, Y. H. et al. Vitamin D3 inhibits lipopolysaccharide-induced placental inflammation through reinforcing interaction between vitamin D receptor and nuclear factor kappa B p65 subunit. Sci. Rep. 5, 10871 (2015).
Chiofalo, B. et al. Do miRNAs Play a Role in Fetal Growth Restriction? A Fresh Look to a Busy Corner. Biomed. Res. Int. 2017, 6073167 (2017).
Laganà, A. S. et al. miRNA expression for early diagnosis of preeclampsia onset: hope or hype? J. Matern. Fetal Neonatal Med. 6, 817–821 (2018).
Balaguer, N. et al. MicroRNA-30d deficiency during preconception affects endometrial receptivity by decreasing implantation rates and impairing fetal growth. Am. J. Obstet. Gynecol. 221, 46.e1–46.e16 (2019).
Rodrigues, P. M. et al. Inhibition of NF-κB by deoxycholic acid induces miR-21/PDCD4-dependent hepatocellular apoptosis. Sci. Rep. 5, 17528 (2015).
Krattinger, R. et al. Chenodeoxycholic acid significantly impacts the expression of miRNAs and genes involved in lipid, bile acid and drug metabolism in human hepatocytes. Life Sci. 156, 47–56 (2016).
Brouwers, L. et al. Intrahepatic cholestasis of pregnancy: maternal and fetal outcomes associated with elevated bile acid levels. Am. J. Obstet. Gynecol. 212, 100.e1–7 (2015).
Gonzalez-Sanchez, E. et al. Protective role of biliverdin against bile acid-induced oxidative stress in liver cells. Free Radic. Biol. Med. 97, 466–477 (2016).
Hohenester, S. et al. Physiological hypoxia prevents bile salt-induced apoptosis in human and rat hepatocytes. Liver. Int. 34, 1224–1231 (2014).
Chappell, L. C. et al. Ursodeoxycholic acid versus placebo in women with intrahepatic cholestasis of pregnancy (PITCHES): a randomised controlled trial. Lancet. 394, 849–860 (2019).
Grymowicz, M., Czajkowski, K. & Smolarczyk, R. Pregnancy course in patients with intrahepatic cholestasis of pregnancy treated with very low doses of ursodeoxycholic acid. Scand. J. Gastroenterol. 51, 78–85 (2016).
Tian, G. et al. A novel electrochemical biosensor for ultrasensitive detection of serum total bile acids based on enzymatic reaction combined with the double oxidation circular amplification strategy. Biosens. Bioelectron. 118, 31–35 (2018).
Dai, L. et al. Birth weight reference percentiles for Chinese. PLoS. One. 9, e104779 (2014).
Acknowledgements
The authors thank Prof. Guiying Nie (from Hudson Institute of Medical Research, Australia) for assistance in reviewing the data and revising the manuscript. This study was supported by National Natural Science Foundation of China (81471467, 81630084, 81671471, 81801477), National College Students’ Innovation and Entrepreneurship Training Program (201910366007), and Key projects of Anhui provincial natural science research in colleges and universities (KJ2019A0224).
Author information
Authors and Affiliations
Contributions
Y.H.C. designed research; L.L., W.C., L.M., Z.B.L., X.L., X.X.G., Y.L., H.W., M.Z. and Y.H.C. conducted research. L.L., X.L.L. and L.C. provided obstetric expertise. Y.H.C., L.L. and W.C. analyzed data and performed statistical analysis; Y.H.C. wrote paper; Y.H.C. and D.X.X. had primary responsibility for final content. All authors reviewed the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Li, L., Chen, W., Ma, L. et al. Continuous association of total bile acid levels with the risk of small for gestational age infants. Sci Rep 10, 9257 (2020). https://doi.org/10.1038/s41598-020-66138-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-66138-y
This article is cited by
-
Perinatal outcomes associated with ICP in twin pregnancies were worse than singletons: an almost 5-year retrospective cohort study
BMC Pregnancy and Childbirth (2022)
-
The association of serum total bile acid with new-onset hypertension during pregnancy
BMC Pregnancy and Childbirth (2022)
-
Whole-exome sequencing identifies novel mutations in ABC transporter genes associated with intrahepatic cholestasis of pregnancy disease: a case-control study
BMC Pregnancy and Childbirth (2021)
-
Prevalence and risk factors of intrahepatic cholestasis of pregnancy in a Chinese population
Scientific Reports (2020)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.