Abstract
This study was to quantitatively investigate the role of morphological and functional parameters of the left atrium (LA) and left atrial appendage (LAA) with 256-slice spiral computed tomography (CT) in the recurrence of atrial fibrillation (AF) after radiofrequency ablation (RFA). Eighty-three patients with AF who underwent RFA for the first time were divided into the recurrence (n = 27) and non-recurrence (n = 56) groups. All patients underwent a 256-slice spiral CT examination before the operation. The clinical data and quantitative measurement of the morphology and functional parameters of the LA and LAA were analyzed, including the maximal and minimal volume, ejection fraction and volume, and volume strain of LAA and LA (LAAVmax, LAAVmin, LAAEF, LAAEV, and LAA-VS, LAVmax, LAVmin, LAEF, LAEV and LA-VS, respectively). The CHA2DS2-VASc score and the proportion of patients with heart failure were significantly (P < 0.05) higher in the recurrence than non-recurrence group. The LAAVmax, LAAVmin, LAVmax, LAVmin, LAAV and LAV were all significantly greater in the recurrence than non-recurrence group (P < 0.05), and the perimeter, major and minor axes of LAA orifice and LAA depth were also significantly greater in the recurrence than non-recurrence group. The LAAEF, LAEF and LAA-VS were significantly (P < 0.05) lower in the recurrence than non-recurrence group (P < 0.05). Heart failure, CHA2DS2-VASC score, LAEF, LAV, LAAEF and LAA-VS were univariately significant (P < 0.05) risk factors for AF recurrence after ablation. Multivariate analysis revealed LAAEF (HR: 0.790, 95% CI: 0.657–0.950, P = 0.012) and LAAV (HR: 1.160, 95% CI: 1.095–1.229, P <0.001) to be two significant independent predictors of recurrence. ROC curve analysis showed that LAAEF <44.68% had the highest predictive value for recurrence after radiofrequency ablation, with the sensitivity of 90% and specificity of 67.4%, whereas LAA volume >9.25 ml had the highest predictive value for AF recurrence after RFA, with the sensitivity of 85.2% and specificity of 67.9%. In conclusion, the volume of left atrium, volume and morphology of left atrial appendage have all significantly increased while the ejection fraction and volume strain of left atrium and left atrial appendage have both significantly decreased in recurrence than in non-recurrence after radiofrequency ablation. The ejection fraction and volume of left atrial appendage are significant independent predictors of atrial fibrillation recurrence after radiofrequency ablation.
Similar content being viewed by others
Introduction
Atrial fibrillation (AF) is the most common cardiac arrhythmia and affects 1%–2% of the general population, with the incidence increased with age1. AF causes abnormal left atrial hemodynamics, subsequent thrombosis, myocardial infarction and heart failure, resulting in increased risks of stroke and mortality. Radiofrequency ablation aiming for pulmonary vein isolation has become an established option for drug-refractory AF, but with high rates of recurrence following ablation (accounting for 10%–30%)2, with the success rate of pulmonary vein isolation varying between 50% and 80%3. It has been shown that left atrial appendage (LAA) is one of the focal potential sources to spontaneously trigger AF, with the left atrium being another possible source of recurrence4. Left atrial volume enlargement and hypofunction are risk predictors after radiofrequency ablation of AF because AF causes remodeling and fibrosis of the left atrium. Dysfunction is a more sensitive recurrence predictor than size. Patients with a normal size of left atrium but reduced left atrium ejection fraction (LAEF) may experience recurrence after ablation5,6,7. Meanwhile, LAA function is also important in predicting recurrence but is largely neglected. The roles of the left atrium and LAA in AF recurrence have not been clearly stated and may be controversial. Recently, some new methods and markers for left atrium and LAA dysfunction have been investigated including assessment of myocardial strain, which is a relatively novel and promising cardiac imaging technique. Strain has been proven to be a risk factor stratification method for various cardiac disorders such as heart failure and coronary artery disease. It has been measured with ultrasound and magnetic resonance imaging, but no studies have been performed using computed tomography (CT) imaging to evaluate strain. We hypothesized that the volumetric and functional parameters of left atrium and LAA including the volume strain of left atrium and LAA evaluated with CT scan could be used as effective predictors for recurrence of AF after radiofrequency ablation. This study was consequently performed using a 256-slice spiral CT scanner to measure the volumetric and functional parameters of left atrium and LAA for predicting possible recurrence of AF following radiofrequency ablation.
Materials and methods
This study was approved by the ethics committee of the Second Hospital, Hebei Medical University with all patients given signed informed consent. All methods were performed in accordance with the relevant guidelines and regulations. Patients who had undergone catheter radiofrequency ablation for AF for the first time in our hospital between October 2016 and June 2017 were enrolled. The inclusion criteria were patients who had radiofrequency ablation for AF which was clinically confirmed and diagnosed by physical examination and electrocardiogram, with preoperative 256-slice spiral CT examination but no serious procedural complications. The exclusion criteria were poor quality of CT angiography (CTA) images for measuring the volume of the left atrium and LAA, contraindication for CTA examination, contrast agent allergy, pacemaker implantation, valvular and congenital heart disease. The basic data, complications, types and duration of AF were collected. The risk of thromboembolism in patients with AF was assessed with the CHA2DS2-VASc score8.
Examination methods
Philips 256-slice spiral CT scanning was performed in patients with AF. Before scanning, patients were trained in breath holding, and metoprolol was used to decrease the heart rate. Non-ionic contrast agent iohexol (350 mg I/ml, 0.8 ml/kg) was injected intravenously with a two-barrel high-pressure syringe. The scanning range was from 0.5 cm below the tracheal bifurcation to the diaphragm of the heart. Retrospective electrocardiogram (ECG) gating technique was used. The scanning parameters were: tube voltage 80–120 kV, tube current 280–350 mAs/rp, collimation 128*0.625, pitch 0.18, matrix 512*512, rotation time 330 ms, and scanning field 250 mm. The scanning voltage and current were generally adjusted according to the body mass index (BMI) of the patient to reduce scanning dose.
Imaging postprocessing
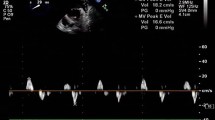
Philips EBW4.5 workstation was used to reconstruct the original image at 5%-95%, with an interval of 10%. The thickness of the reconstructed layer was 0.9 mm and the interval was 0.45 mm. Three-dimensional images of the left atrium and LAA were obtained on the axial images with the post-processing software of cardiac function. The perimeter, major and minor axes of the orifice of LAA were measured putting the coronary positioning line across the conjunction of the left atrium with LAA to obtain the cross section of the orifice of the LAA (Fig. 1). The perimeter and axes of the LAA were measured at the 45% time phase of the cardiac cycle corresponding to the cardiac systolic cycle. In the CT image, the coronary positioning line was put across the conjunction of the left atrium with LAA in the cross section (Fig. 1A&B) to obtain the cross section of the orifice of the LAA (C) for measurement of the major and minor axes of the LAA (Fig. 1C) and the perimeter of the LAA orifice (Fig. 1D). The positioning line was perpendicular to the intersection of the LAA with the left atrium. After multiplane reconstruction and on the coronal location, the positioning line was perpendicular to the conjunction between the LAA and left atrium. The cross-section image of the bottom of the LAA was obtained. The length, short diameter and perimeter of the bottom of the LAA were measured (Fig. 1). The total volume of the left atrium and LAA were automatically calculated. The LAA depth was measured (Fig. 1F, lower part) from the most distal tip of LAA to the center of the cross section of the LAA orifice. The 45% time phase of the cardiac cycle is systolic, and at this period, the LAA has the greatest volume. At 65–85% of the cardiac cycle, the structural parameters of the LAA have minimal changes corresponding to the natural status. The maximal structural parameters of LAA may change with AF. The depth, opening area, diameter lines, and the end diastolic volume of the LAA (i.e. the maximal diameter line of the LAA structure) are significantly greater in patients with than without chronic AF9. Therefore, the choice of the 45% of the cardiac cycle can better reflect the structural changes of LAA. The left atrial volume and LAA volume were measured at every phase, and then the maximal and minimal left atrial volume (LAVmax and LAVmin, respectively), maximal and minimal volume of the LAA (LAAVmax and LAAVmin, respectively) were obtained. The LAA ejection fraction and volume (LAAEF and LAAEV, respectively), left atrial ejection fraction and volume (LAEF and LAEV, respectively), left atrial volume strain (LA-VS) and LAA volume strain (LAA – VS) were calculated as follows: LAAEV = LAAVmax-LAAVmin, LAAEF = (LAAVmax – LAAVmin)/LAAVmax × 100%, LAA – VS = (LAAVmax-LAAVmin)/LAAVmin × 100%, LAEV = LAVmax-LAVmin, LAEF = (LAVmax – LAVmin)/LAVmax × 100%, and LA – VS = (LAVmax – LAVmin)/LAVmin × 100%.
Quantitative measurement of left atrium and left atrial appendage (LAA). (A–C) In computed tomographic imaging, the coronary positioning line was put across the conjunction of the left atrium with LAA in the cross section (A,B) to obtain the cross section of the orifice of the LAA (C). The major and minor axes of the LAA were measured (C). (D) The perimeter of the LAA orifice was measured. (E,F) The left atrium and LAA imaging was obtained using cardiac function software for measuring the volume of the left atrium and LAA. The LAA depth was measured (F, lower part) from the most distal tip of LAA to the center of the cross section of the LAA orifice. The upper part in F is the left atrium and LAA.
Radiofrequency catheter ablation
Radiofrequency catheter ablation was performed according to the unified standard for circumferential pulmonary vein isolation. The coronal sinus electrodes were inserted into the subclavian vein or femoral vein of the patient, and atrial septal puncture was performed to reconstruct the left atrium-pulmonary vein. The pulmonary veins were isolated and ablated. Two-way conduction block between the pulmonary vein and left atrium was confirmed by electrophysiological stimulation after the operation.
Postoperative management and follow-up
Surface ECG or dynamic electrocardiogram (DCG) results were obtained at 3, 6 and 12 months after operation. The DCG was 24-hour dynamic ECG to record the condition of the heart within 24 hours including normal and abnormal activity and status. If palpitation symptoms occurred, ECG examination was performed immediately. The endpoint at follow-up was recurrence of AF which was defined as rapid atrial arrhythmia (atrial tachycardia, atrial flutter, atrial fibrillation) recorded by ECG after 3 months of blank period.
Statistical analysis
SPSS 21.0 statistical software (IBM, Chicago, IL, USA) was used for data analysis. Counting data were expressed as an amount (%) and analyzed with the chi-square test. Mean comparisons between two groups with normal distribution were expressed as mean ± SD (standard deviation) and analyzed by independent sample t-test, and data with non-normal distribution were expressed by Wilcoxon rank-sum test and median (quartile spacing). Univariate and multivariate Cox proportional risk regression models were used to evaluate the risk factors associated with recurrence of AF. Test for collinearity in the variables was included in the model. Strongly correlated variables were excluded. The variance inflation factors were calculated. Independent predictors of recurrence after radiofrequency ablation of AF were analyzed, and adjusted risk ratio (HR) was calculated. The best critical value of predictors of recurrence after AF surgery was calculated by ROC (receiver operating curve) analysis. The statistical significance was set at P < 0.05.
Results
Eighty-three patients with AF who underwent radiofrequency ablation for the first time were enrolled, including 49 male and 34 female patients with a mean age of 60.36 ± 10.11 and a mean BMI of 25.98 ± 4.06 kg/m2. The median follow-up time was 19 (range 4–24) months, and 27 patients (32.5%) relapsed. The patients were divided into two groups: recurrence group (n = 27, mean age 63.26 ± 9.30 year) and the non-recurrence group (n = 56, mean age 58.96 ± 10.26 year).
The clinical data of patients after radiofrequency ablation of AF were compared (Table 1). No significant (P > 0.05) differences existed in the composition of age, sex, BMI, diabetes mellitus, hypertension, coronary heart disease, stroke, transient ischemic attack and duration of AF between the two groups. However, the CHA2DS2-VASc score and heart failure were significantly (P < 0.05) greater in the recurrence than non-recurrence group.
Quantitative measurement of the morphology and functional parameters of the left atrium and LAA was performed. The LAAVmax, LAAVmin, LAVmax, and LAVmin were significantly greater in the recurrence than non-recurrence group (P < 0.05), and the perimeter, major and minor axes of LAA orifice and LAA depth were also significantly greater in the recurrence than non-recurrence group (Table 2). The LAAEF, LAEF and LAA-VS were significantly (P < 0.05) lower in the recurrence than non-recurrence group (P < 0.05) (Table 2). However, no significant (P > 0.05) differences existed in the LAAEV, LAEV, and LA-VS between the two groups. LAEF, LAAEF, and LAA-VS were all calculated from LAAVmax and LAAVmin. The opening and depth of LAA were strongly related to LAAVmax and LAAVmin. Therefore, only LAEF and LAAEF were retained after removing LAVmax, LAVmin, LAAVmax and LAAVmin. Although LAV correlated with LAVmax and LAVmin and LAAV correlated with LAAVmax and LAAVmin, LAV and LAAV represented LA and LAA morphology, respectively. Therefore, LAV and LAAV were also included in the multivariate analysis. Combined with the P value in Table 1, the measurement contents with P value < 0.2 of the group difference were included in the model, namely: age, CHA2DS2-VASC, and heart failure.
Univariate Cox proportional risk regression analysis showed that the P value of age was 0.088, so age was not included in the multivariate analysis. LAEF and LAAEF were significant (P < 0.05) risk factors for AF recurrence after radiofrequency ablation (Table 3). The covariance expansion factors of LAAEF and LAEF were calculated, which were 2.069 and 2.018, respectively. Because these factors were less than 5, the LAAEF and LAEF did not have collinearity. CHA2DS2-VASC, LAV, and LAAV were significant (P < 0.05) risk factors for AF recurrence after radiofrequency ablation.
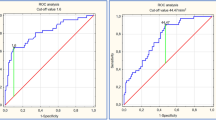
Multivariate analysis revealed LAAEF (HR: 0.79, 95% CI: 0.66–0.95, P = 0.01) and LAAV (HR: 1.160, 95% CI: 1.095–1.229, P < 0.001) to be significant independent predictors of recurrence after radiofrequency ablation of AF (Table 4). For every 1% increase in LAAEF, the AF recurrence rate after radiofrequency ablation is decreased 21%, whereas for every 1 ml increase in the LAA volume, the risk for AF recurrence after radiofrequency ablation increased 1.16 times. ROC curve analysis showed that LAAEF < 44.68% had the highest predictive value for recurrence after radiofrequency ablation (area under curve 0.817), with the sensitivity of 90% and specificity of 67.4%, whereas LAA volume >9.25 ml had the highest predictive value for AF recurrence after radiofrequency ablation (area under curve 0.82), with the sensitivity of 85.2% and specificity of 67.9% (Fig. 2). Among all 27 patients with AF recurrence, only four patients had the LAA volume ≤9.25 ml. Kaplan-Meier curve analysis (Fig. 2) further showed that patients with LAA volume >0.25 ml had a greater recurrence rate after radiofrequency ablation (P < 0.001).
ROC curve analysis of the volume and ejection fraction of the left atrial appendage (LAAV and LAAEF, respectively) and Kaplan-Meier analysis of LAAV. The star indicates the LAAEF or the LAAV with the highest predictive value of recurrence after radiofrequency ablation. The numbers at risk are demonstrated in the Kaplan-Meier analysis of LAAV.
Discussion
Catheter radiofrequency ablation is an effective therapeutic approach for the treatment of AF, especially for refractory patients who have episodes of arrhythmia despite antiarrhythmic medicine therapy. For patients with paroxysmal AF, catheter radiofrequency ablation can be used as a first-line therapy. However, recurrence of AF remains an important issue. Exploring the risk predictors of AF recurrence is critical to identifying high-risk patients following radiofrequency ablation, thus providing a basis for preoperative selection of treatment methods and improving the ablation success rate. The recurrence rate following AF radiofrequency ablation in this study was 32.5%, which was consistent with that reported in previous research10. Our study showed that the LAVmax, LAVmin, LAAVmax, and LAAVmin were all significantly elevated in patients with recurrence compared with those without recurrence, whereas the LAAEF and LAEF significantly decreased in patients with recurrence compared with those of non-recurrence, with the LAAEF and LAAV being two significant independent factors to predict recurrence following catheter radiofrequency ablation. Previous studies have also demonstrated that increased volumes of left atrium and LAA but decreased ejection fraction of the left atrium and LAA are risk predictors of recurrence after radiofrequency ablation of AF5,6.
Left atrial overload may result in structural remodeling, atrial hypertrophy and stretch, and subsequent ionic current alterations and electrical remodeling11. Cardiac endothelin-1 expression correlates with enlarged left atrium size and responds to the wall stress caused by enlarged left atrium, thus promoting hypertrophy of myocytes and fibrosis of myocardial interstitium. Atrial fibrosis in patches can cause slow conduction and change dynamic repolarization in some areas, consequently shifting the initiation focus and AF maintenance to the left atrium from the pulmonary veins12,13. In this case, radiofrequency ablation may be insufficient, resulting in an increased rate of recurrence. Left atrial enlargement is able to independently predict a new AF onset14, and the left atrium diameter has been reported as a predicting factor for AF recurrence following radiofrequency ablation15,16. However, the anterior-posterior diameter of the left atrium is not regarded to reflect the real size of left atrium. Abecasis et al.17 demonstrated that the left atrium volume rather than the anterior-posterior diameter of left atrium was related to AF recurrence following radiofrequency ablation. In a study investigating the relationship of left atrium volume with AF recurrence following ablation18, Helms et al. proved that the volume of the left atrium was significantly increased in recurrence and that only the volume of the left atrium and number of cardiovascular diseases were significantly associated with more recurrences, with patients having left atrial volumes > 135 ml being very likely to experience AF recurrence after radiofrequency ablation. In a meta-analysis11, Nioku et al. proved that the volume rather than the diameter of left atrium is a more accurate parameter in predicting AF recurrence after radiofrequency ablation.
The LAA is a frequent location of thrombosis in AF patients, and significantly larger LAA and left atrium are present in AF patients than those without AF. Expanded LAA may cause poor contraction and elevated risk of thrombosis of both the LAA and the whole system19. Successful radiofrequency ablation to eliminate AF will significantly decrease the orifice, neck and length of the LAA and reverse the LAA neck shape which is less eccentric in AF patients19. Nonetheless, AF recurrence following ablation will lead to progressive dilation of the LAA but no change in the eccentricity of the LAA orifice and neck. The LAA has a blind pouch and a relatively narrow orifice to the main chamber of the left atrium. When the LAA is remodeled in AF, the LAA is stretched and loses its compliance and contractility, and the shape of the LAA neck becomes rounder. Moreover, less cardiomyolysis and less interstitial fibrosis are presented in LAA than in the left atrial main chamber in AF. After radiofrequency ablation, the size of LAA may decrease faster than that of the left atrium20. AF recurrence following catheter ablation will further dilate both the left atrium and LAA because prolonged AF will cause cardiomyocyte hyperplasia, death and fibrosis, resulting in enlargement of cardiac chambers and tachyarrhythmia attack.
For the LAA volume, He et al. demonstrated in a study with transesophageal echocardiography for measuring the LAA volume and function that the LAAVmax and LAAVmin were markedly increased in recurrence while the function parameters including LAAEF, LAA flow emptying velocity and summit filling velocity were significantly decreased, with the multivariate analysis showing the left atrial volume index, LAAEF and LAA flow emptying velocity to be significant factors to predict paroxysmal AF recurrence following radiofrequency ablation21. In a study with multi-detector CT scanning investigating the LAA volume in association with AF recurrence following radiofrequency ablation22, Shiozawa et al. found that both greater LAA volumes and orifice areas were exhibited in recurrent AF patients while the diameter and volume of the left atrium did not have significant differences between patients with and without recurrence. All patients possessing a LAA volume greater than 25 ml experienced AF recurrence. As an embryonic remnant of the left atrium, the LAA plays a very important role in adjusting heart rate and fluid balance via an expandable reservoir function, a capacity to secret atrial natriuretic peptides, and sensitive receptors of stretch22,23,24. The LAA is distensible at a greater degree than the left atrium, and the LAA volume is a dependable parameter to determine the left atrial conditions in both function and structure in early AF. After analyzing the relationship between LAA volume and AF recurrence following catheter ablation25, Pinto et al. pointed out that the volume of the LAA on cardiac CT may be able to independently predict recurrence of paroxysmal and persistent fibrillation after first ablation and that a volume of the LAA more than 8.825 ml may accurately predict recurrent AF.
The left atrium may act as a contractable pump providing up to a third of the volume of the left ventricle, as a reservoir collecting pulmonary venous blood in the right ventricular systolic period, and as a channel to pass stored blood from the left atrium to the left ventricle26. The LAEF reflects left atrial conduit and contracting function while the LAAEF indicates the contracting function only. In our study, the LAAEF and LAEF significantly decreased in patients with recurrence compared with those without recurrence. Impaired emptying fraction of the left atrium (≤20%), decreased emptying velocity (≤20 cm/sec) and fraction (≤20%) of the LAA were significantly correlated with recurrent AF after ablation6. A low LAA peak flow velocity and upward velocity of the LAA apex wall before surgery have been reported to relate to recurrent AF following the initial ablation for persistent AF27,28. Chin et al.29 have reported that the LAEF and LAAEF have significantly decreased in patients with AF recurrence after one year, indicating that AF recurrence may worsen left atrial function. After studying the risk-predicting factors for AF recurrence following revised endoscopic ablation at two years of follow-up, An et al.30 found that the duration of AF, the diameter of left atrium, and LAAEF could significantly independently predict AF recurrence. Decreased LAEF and LAAEF in patients with AF recurrence indicate decreased function in the reservoir and contraction of the left atrium and LAA, which may denote enlarged volume of the left atrium and LAA, and consequently the anatomical parameters of the LAA also increase including the perimeter, major and minor axes of LAA orifice and LAA depth. These parameters were significantly greater in patients with recurrence compared with those without recurrence in our study. Age is also an important factor for AF recurrence31. The older the patient, the more likely the presence of AF recurrence after radiofrequency ablation. In our study, patients with AF recurrence were not significantly different in age from those without recurrence, and that is why multivariable analysis did not show age as a significant factor for recurrence.
AF originating from the LAA is one important index for AF recurrence following radiofrequency ablation. It has been reported that 27% of patients with recurrent arrhythmias after radiofrequency ablation of AF were associated with LAA4. Further investigation has found that LAA isolation can reduce the recurrence rate of arrhythmia4. Therefore, the relationship between LAA function and AF recurrence after radiofrequency ablation is very important. In our study, the LAAEF rather than the LAA volume is a significant factor to predict AF recurrence following radiofrequency ablation, suggesting that LAA function may be more important than LAA volume in predicting recurrence after radiofrequency ablation of AF. Ejection fraction is a better parameter in revealing the rate of volume decrease after ejection of blood and indicating the contractile function of LAA.
AF causes the structure of LAA remodeling like fibrosis, which is related to AF relapse after radiofrequency ablation. The LAA has abundant comb muscles, which have stronger autonomic contraction function than muscles in the left atrium. Changes in the pressure and volume of the left atrium can help regulating its systolic and diastolic function32. In AF patients, the left atrium loses its rhythm, and the ejection function is decreased. To alleviate increased intra-atrial pressure, the myocardia of LAA are structurally remodeled. The degree of LAA remodeling in recurrent patients of AF following radiofrequency ablation is greater than in those without recurrence33. LAA remodeling may lead to electrophysiological changes in LAA. It has been shown that left atrial fibrosis is associated with conduction abnormalities and aggravates recurrence of AF34. Our research showed that, compared to the left atrium, fibrosis of LAA myocardia represented by LAA-VS was more important in recurrence, with significantly greater LAA-VS in the recurrence than non-recurrence group. Displaying myocardial fibrosis of left atrium and LAA is difficult because the fibrosis is too delicate to be measured. Strain imaging of the magnetic resonance imaging can be used to assess fibrosis of myocardia, however, it needs special software, which limits its clinical usage. In our study, the volume strain of left atrium and LAA were calculated with use of the 256-slice CT, which can be easily performed in regular cardiac CT scanning.
Transesophageal echocardiography (TEE) stands for the gold standard in measuring LAA parameters. With high spatial resolution and high repeatability, multi-slice CT (MSCT) is well correlated with TEE in the measurement of the LAA volume and function35. It has been shown that LAAEF measured by TEE can predict the sinus rhythm status in AF patients post treatment21. After examining paroxysmal AF in 80 patients by TEE prior to radiofrequency ablation, He et al.21 found that high LAAEF was a protective factor for preventing AF recurrence. The combined model of left atrial volume index, LAEF and LAA-emptying velocity (LAVI + LAAEF + LAAeV) was effective in predicting paroxysmal AF recurrence21. It has been shown that LAAEF < 30% measured by TEE is an independent index for predicting non-valvular AF recurrence following cardioversion36. However, the relationship between LAA function measured by multi-slice spiral CT and recurrence after radiofrequency ablation has rarely been reported. In our study, the 256-slice spiral CT was used to measure LAA function for the first time to predict AF recurrence after radiofrequency ablation, and our results showed that LAAEF was also an independent factor to predict AF recurrence following radiofrequency ablation, with LAAEF < 44.68% having the highest value for predicting AF recurrence following radiofrequency ablation.
The CHADS2 and the CHA2DS2-VASc systems are affirmative risk stratification models for predicting vascular events and ischemic strokes in non-valvular AF8,37. There are some values in these scores for predicting left atrial ablation outcomes. Larger left atrial volume, diabetes, dyslipidemia, coronary artery disease, class III antiarrhythmic drugs, CHADS2 and CHA2DS2-VASc scores had univariately associated with AF recurrence after left atrial ablation, and both CHADS2 and CHA2DS2-VASc could independently predict AF recurrence8. The CHA2DS2-VASc scores, combined with other clinical parameters of heart failure, advanced age, hypertension, and diabetes, are dependable parameters for predicting AF recurrence after left atrial ablation. In our study, however, the CHA2DS2-VASc score system did not perform better than LAAEF and increased LAA volume in predicting AF recurrence following catheter ablation even though this score was significantly increased in AF recurrence compared with non-recurrence after catheter ablation.
Addition of LAA ligation using the percutaneous endoepicardial closure system to common radiofrequency ablation can improve the ablation success rate but decrease the recurrence rate38,39,40. The AMEZE trial may be a good approach to determine if LAA ligation as an adjunctive treatment approach to pulmonary venous isolation is able to increase the efficacy of sinus rhythm maintenance in persistent AF or long-term persistent AF39. In addition, LAA electrical isolation combined with standard ablation helps achieving freedom from various atrial arrhythmias in persistent AF or long-term persistent AF40. In the study of LAA ligation combined with ablation for persistent AF by Lakkireddy et al.38 enrolling a total of 138 patients with 69 patients in the group with additional LAA ligation (LARIAT), the primary outcome without AF at 1 year off antiarrhythmic treatment following one ablation procedure was better in the LARIAT group (65% vs. 39%, P < 0.01) than in the group applying radiofrequency ablation alone, with significantly more patients in the group using ablation only experiencing repeated ablation due to AF recurrence (33% vs. 16%, P = 0.018). Radiofrequency ablation combined with LAA ligation may exclude the LAA both mechanically and electrically and help improving the prognoses of radiofrequency ablation through eliminating the triggers and changing the substrate of the LAA.
Some limitations may exist in our study including single center study, only Chinese ethnicity enrolled, a small cohort of patients, retrospective nature and non-randomization. Future research will need to overcome these limitations for better outcomes.
In summary, the left atrial volume, the volume and morphology of the left atrial appendage have all significantly increased, whereas the ejection fraction and volume strain of both the left atrium and atrial appendage have both significantly decreased in recurrence than in non-recurrence after radiofrequency ablation. The ejection fraction and volume of the left atrial appendage are significant independent factors to predict recurrence of atrial fibrillation following radiofrequency ablation.
References
Chugh, S. S. et al. Worldwide epidemiology of atrial fibrillation: a Global Burden of Disease 2010 Study. Circulation 129, 837–847, https://doi.org/10.1161/CIRCULATIONAHA.113.005119 (2014).
Aksu, T., Guler, T. E., Bozyel, S. & Yalin, K. 2017 expert consensus statement on catheter and surgical ablation of atrial fibrillation: letter to the Editor. Europace 20, f462, https://doi.org/10.1093/europace/eux363 (2018).
Calkins, H. et al. 2012 HRS/EHRA/ECAS expert consensus statement on catheter and surgical ablation of atrial fibrillation: recommendations for patient selection, procedural techniques, patient management and follow-up, definitions, endpoints, and research trial design. J Interv Card Electrophysiol 33, 171–257, https://doi.org/10.1007/s10840-012-9672-7 (2012).
Di Biase, L. et al. Left atrial appendage: an underrecognized trigger site of atrial fibrillation. Circulation 122, 109–118, https://doi.org/10.1161/CIRCULATIONAHA.109.928903 (2010).
D’Ascenzo, F. et al. Which are the most reliable predictors of recurrence of atrial fibrillation after transcatheter ablation?: a meta-analysis. Int J Cardiol 167, 1984–1989, https://doi.org/10.1016/j.ijcard.2012.05.008 (2013).
Kim, M. N. et al. The difference of predictors for recurrence after catheter ablation of non-paroxysmal atrial fibrillation according to follow-up period. Int Heart J 55, 312–318 (2014).
Taina, M. et al. Morphological and volumetric analysis of left atrial appendage and left atrium: cardiac computed tomography-based reproducibility assessment. PLoS One 9, e101580, https://doi.org/10.1371/journal.pone.0101580 (2014).
Letsas, K. P. et al. CHADS2 and CHA2DS2-VASc scores as predictors of left atrial ablation outcomes for paroxysmal atrial fibrillation. Europace 16, 202–207, https://doi.org/10.1093/europace/eut210 (2014).
Matsumoto, Y. et al. Characteristics of Anatomy and Function of the Left Atrial Appendage and Their Relationships in Patients with Cardioembolic Stroke: A 3-Dimensional Transesophageal Echocardiography Study. J Stroke Cerebrovasc Dis 26, 470–479, https://doi.org/10.1016/j.jstrokecerebrovasdis.2016.12.014 (2017).
Arbelo, E. et al. The atrial fibrillation ablation pilot study: a European Survey on Methodology and results of catheter ablation for atrial fibrillation conducted by the European Heart Rhythm Association. Eur Heart J 35, 1466–1478, https://doi.org/10.1093/eurheartj/ehu001 (2014).
Njoku, A. et al. Left atrial volume predicts atrial fibrillation recurrence after radiofrequency ablation: a meta-analysis. Europace 20, 33–42, https://doi.org/10.1093/europace/eux013 (2018).
Krummen, D. E., Swarup, V. & Narayan, S. M. The role of rotors in atrial fibrillation. J Thorac Dis 7, 142–151, https://doi.org/10.3978/j.issn.2072-1439.2014.11.15 (2015).
Mayyas, F. et al. Association of left atrial endothelin-1 with atrial rhythm, size, and fibrosis in patients with structural heart disease. Circ Arrhythm Electrophysiol 3, 369–379, https://doi.org/10.1161/CIRCEP.109.924985 (2010).
Vaziri, S. M., Larson, M. G., Benjamin, E. J. & Levy, D. Echocardiographic predictors of nonrheumatic atrial fibrillation. The Framingham Heart Study. Circulation 89, 724–730, https://doi.org/10.1161/01.cir.89.2.724 (1994).
Miyazaki, S. et al. Preprocedural predictors of atrial fibrillation recurrence following pulmonary vein antrum isolation in patients with paroxysmal atrial fibrillation: long-term follow-up results. J Cardiovasc Electrophysiol 22, 621–625, https://doi.org/10.1111/j.1540-8167.2010.01984.x (2011).
Patel, D. et al. The impact of statins and renin-angiotensin-aldosterone system blockers on pulmonary vein antrum isolation outcomes in post-menopausal females. Europace 12, 322–330, https://doi.org/10.1093/europace/eup387 (2010).
Abecasis, J. et al. Left atrial volume calculated by multi-detector computed tomography may predict successful pulmonary vein isolation in catheter ablation of atrial fibrillation. Europace 11, 1289–1294, https://doi.org/10.1093/europace/eup198 (2009).
Helms, A. S. et al. Relation of left atrial volume from three-dimensional computed tomography to atrial fibrillation recurrence following ablation. Am J Cardiol 103, 989–993, https://doi.org/10.1016/j.amjcard.2008.12.021 (2009).
Chang, S. H. et al. Morphological changes of the left atrial appendage after catheter ablation of atrial fibrillation. J Cardiovasc Electrophysiol 18, 47–52, https://doi.org/10.1111/j.1540-8167.2006.00655.x (2007).
Corradi, D. et al. Myocyte changes and their left atrial distribution in patients with chronic atrial fibrillation related to mitral valve disease. Hum Pathol 36, 1080–1089, https://doi.org/10.1016/j.humpath.2005.07.018 (2005).
He, Y. et al. Transesophageal echocardiography measures left atrial appendage volume and function and predicts recurrence of paroxysmal atrial fibrillation after radiofrequency catheter ablation. Echocardiography 35, 985–990, https://doi.org/10.1111/echo.13856 (2018).
Shiozawa, T. et al. Left Atrial Appendage Volume and Plasma Docosahexaenoic Acid Levels Are Associated With Atrial Fibrillation Recurrence After Catheter Ablation. Cardiol Res 8, 96–104, https://doi.org/10.14740/cr542w (2017).
Hoit, B. D., Shao, Y. & Gabel, M. Influence of acutely altered loading conditions on left atrial appendage flow velocities. J Am Coll Cardiol 24, 1117–1123, https://doi.org/10.1016/0735-1097(94)90878-8 (1994).
Sherif, H. M. The developing pulmonary veins and left atrium: implications for ablation strategy for atrial fibrillation. Eur J Cardiothorac Surg 44, 792–799, https://doi.org/10.1093/ejcts/ezt098 (2013).
Pinto Teixeira, P. et al. Left atrial appendage volume as a new predictor of atrial fibrillation recurrence after catheter ablation. J Interv Card Electrophysiol 49, 165–171, https://doi.org/10.1007/s10840-017-0256-4 (2017).
Delgado, V. et al. Fate of left atrial function as determined by real-time three-dimensional echocardiography study after radiofrequency catheter ablation for the treatment of atrial fibrillation. Am J Cardiol 101, 1285–1290, https://doi.org/10.1016/j.amjcard.2007.12.028 (2008).
Kanda, T. et al. Low left atrial appendage flow velocity predicts recurrence of atrial fibrillation after catheter ablation of persistent atrial fibrillation. J Cardiol 66, 377–381, https://doi.org/10.1016/j.jjcc.2015.04.009 (2015).
Ariyama, M. et al. Left atrial appendage wall-motion velocity associates with recurrence of nonparoxysmal atrial fibrillation after catheter ablation. Echocardiography 32, 272–280, https://doi.org/10.1111/echo.12647 (2015).
Chin, J. Y. & Youn, H. J. The effect of ablation for paroxysmal atrial fibrillation on left atrial volume and function: a one-year follow-up study. Yonsei Med J 55, 895–903, https://doi.org/10.3349/ymj.2014.55.4.895 (2014).
An, K., Zhu, J., Ma, N., Tang, M. & Mei, J. Predictive risk factors for recurrent atrial fibrillation after modified endoscopic ablation: A 2-year follow-up. Clin Cardiol 41, 372–377, https://doi.org/10.1002/clc.22878 (2018).
Lee, S. H. et al. Predictors of early and late recurrence of atrial fibrillation after catheter ablation of paroxysmal atrial fibrillation. J Interv Card Electrophysiol 10, 221–226, https://doi.org/10.1023/B:JICE.0000026915.02503.92 (2004).
Al-Saady, N. M., Obel, O. A. & Camm, A. J. Left atrial appendage: structure, function, and role in thromboembolism. Heart 82, 547–554, https://doi.org/10.1136/hrt.82.5.547 (1999).
Suksaranjit, P. et al. Relation of Left Atrial Appendage Remodeling by Magnetic Resonance Imaging and Outcome of Ablation for Atrial Fibrillation. Am J Cardiol 122, 83–88, https://doi.org/10.1016/j.amjcard.2018.03.027 (2018).
Krul, S. P. et al. Atrial fibrosis and conduction slowing in the left atrial appendage of patients undergoing thoracoscopic surgical pulmonary vein isolation for atrial fibrillation. Circ Arrhythm Electrophysiol 8, 288–295, https://doi.org/10.1161/CIRCEP.114.001752 (2015).
Korsholm, K., Jensen, J. M. & Nielsen-Kudsk, J. E. Cardiac Computed Tomography for Left Atrial Appendage Occlusion: Acquisition, Analysis, Advantages, and Limitations. Interv. Cardiol Clin 7, 229–242, https://doi.org/10.1016/j.iccl.2017.12.004 (2018).
Okcun, B. et al. Predictors for maintenance of sinus rhythm after cardioversion in patients with nonvalvular atrial fibrillation. Echocardiography 19, 351–357 (2002).
Boriani, G. et al. Improving stroke risk stratification using the CHADS2 and CHA2DS2-VASc risk scores in patients with paroxysmal atrial fibrillation by continuous arrhythmia burden monitoring. Stroke 42, 1768–1770, https://doi.org/10.1161/STROKEAHA.110.609297 (2011).
Lakkireddy, D. et al. Left Atrial Appendage Ligation and Ablation for Persistent Atrial Fibrillation: The LAALA-AF Registry. JACC Clin Electrophysiol 1, 153–160, https://doi.org/10.1016/j.jacep.2015.04.006 (2015).
Lee, R. J. et al. Percutaneous alternative to the Maze procedure for the treatment of persistent or long-standing persistent atrial fibrillation (aMAZE trial): Rationale and design. Am Heart J 170, 1184–1194, https://doi.org/10.1016/j.ahj.2015.09.019 (2015).
Romero, J. et al. Benefit of left atrial appendage electrical isolation for persistent and long-standing persistent atrial fibrillation: a systematic review and meta-analysis. Europace 20, 1268–1278, https://doi.org/10.1093/europace/eux372 (2018).
Author information
Authors and Affiliations
Contributions
Data collection and analysis: Xin Tian, Xue-Jing Zhang, Ying-Fang Yuan, Cai-Ying Li, Study design: Cai-Ying Li, Bu-Lang Gao. Statistics: Xin Tian, Ying-Fang Yuan, Li-Xia Zhou. Supervision: Li-Xia Zhou, Xue-Jing Zhang, Figure preparation: Xin Tian, Ying-Fang Yuan, Bu-Lang Gao, Approval of the paper: all authors, Writing of the draft: Xin Tian, Revision: Bu-Lang Gao.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Tian, X., Zhang, XJ., Yuan, YF. et al. Morphological and functional parameters of left atrial appendage play a greater role in atrial fibrillation relapse after radiofrequency ablation. Sci Rep 10, 8072 (2020). https://doi.org/10.1038/s41598-020-65056-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-65056-3
This article is cited by
-
Left atrial appendage morphofunctional indices could be predictive of arrhythmia recurrence post-atrial fibrillation ablation: a meta-analysis
The Egyptian Heart Journal (2023)
-
An effective prediction model based on XGBoost for the 12-month recurrence of AF patients after RFA
BMC Cardiovascular Disorders (2023)
-
Development and Validation of a Novel Prognostic Model Predicting the Atrial Fibrillation Recurrence Risk for Persistent Atrial Fibrillation Patients Treated with Nifekalant During the First Radiofrequency Catheter Ablation
Cardiovascular Drugs and Therapy (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.