Abstract
This retrospective, cross-sectional study investigated changes in corneal low and high order aberrations (LOAs and HOAs) after lower eyelid epiblepharon repair surgery. In total, 108 eyes from 54 patients were evaluated. Wavefront analyses for calibrated LOAs and HOAs were performed using a Galilei G4 Dual Scheimpflug Analyzer before surgery and during the first and second follow-ups (f/u), adjusting for several risk factors. Flat keratometry (K) and axis values decreased significantly from baseline at the first f/u. At the second f/u, mean K and axis values decreased. Coma and trefoil increased from baseline at the first f/u and normalized by the second f/u. Spherical aberrations (SA) only decreased at the second f/u. After correction for risk factors, cylinder, coma, trefoil, and SA significantly increased at the first f/u; axis and flat K values decreased. At the second f/u, cylinder increased while axis and mean K values significantly decreased. Epiblepharon repair surgery may result in a shift from ‘with-the-rule’ to ‘against-the-rule’ axis change. Flat K, coma, and trefoil may be affected by mechanical force changes immediately post-surgery, while mean K values and SA may also change with corneal state changes including corneal erosion healing after the second f/u during the postoperative period.
Similar content being viewed by others
Introduction
Epiblepharon is a congenital anomaly of eyelids that occurs more frequently among Asian children than among children of other demographic backgrounds1. The prevalence of epiblepharon in the Japanese population was reported to be 9.9% in children aged 3 months to 18 years2. In addition, epiblepharon comprised 9.5% of the oculoplastic surgery clinical cases in a tertiary care hospital setting in Singapore3. Epiblepharon is defined as a horizontal fold in the hypertrophied pretarsal orbicularis muscle and redundant skin below the margin of the eyelid, which cause the eyelashes to project inwards towards the cornea while the eyelids with tarsus remains in normal positions. Epiblepharon is different from congenital entropion, which is an inward rotation of the eyelid margin with the tarsus4,5.
Patients with epiblepharon experience photophobia, foreign body sensation, irritating tearing, and visual disturbances caused by corneal problems6. In addition, astigmatisms are most frequently observed in patients with epiblepharon as compared with the normal population. For instance, Preechawai et al. reported a high prevalence of astigmatism in epiblepharon patients (52.2% had a 1 D or worse astigmatism)7. Furthermore, several studies have reported a greater prevalence of astigmatism in patients with epiblepharon and changes in astigmatism after epiblepharon repair surgery7,8,9,10.
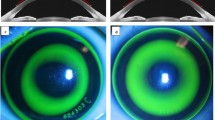
Modern vision research has benefited from wavefront technology, which makes it possible to measure low and high order aberrations (LOA and HOA), including posterior corneal astigmatisms, with total cornea curvature via the Galilei G4 Dual Scheimpflug Analyzer (Ziemer, Port, Switzerland). Ray tracing using Snell’s law and pachymetry data with a reference plane in the posterior corneal surface are used11. Furthermore, HOAs from all refractive errors, such as those that occur with astigmatisms, cannot be corrected by ordinary glasses or contact lenses. Recently, HOAs have been represented mathematically by calculating a Zernike coefficient12,13,14. Moreover, corneal transplantation, intraocular lens (IOL) implantation, pterygium surgery, and scleral buckling result in HOA changes15,16,17. In HOAs, ‘spherical aberration’ changes are known to result in decreased contrast sensitivity, halos, and glare, and ‘coma’ changes are associated with tilt and double vision18,19. These HOAs result in changes that may lead patients to experience a qualitative deterioration in sight18,19,20.
Given that most epiblepharon patients are children, understanding the visual impairments caused by surgery is especially critical. The risk for astigmatism and HOAs due to surgery should be conveyed to patients, and eyeglass prescriptions should be considered. To our knowledge, although changes in anterior LOAs (sphere and cylinder) after surgery have been investigated, no studies on the changes in calibrated anterior and posterior LOAs together with HOAs, including their risk factors, have been conducted. The purpose of the present study was to evaluate the preoperative and postoperative calibration of LOA (anterior and posterior astigmatisms) and HOA changes in the postoperative period, while adjusting for potential risk factors such as age, sex, body mass index (BMI), and corneal keratitis status.
Methods
Approval for the retrospective review (IRB file No.: DSMC 2019-02-005) of our patients’ medical data was obtained from the Keimyoung University Dongsan Hospital Institutional Review Board (IRB), Daegu, Korea. All data and research collection procedures followed the tenets of the Declaration of Helsinki.
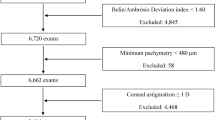
The medical and surgical records of 78 patients (156 eyes) diagnosed with epiblepharon who underwent epiblepharon repair surgery at Keimyoung University Dongsan Hospital from January 2016 to January 2019 were retrospectively reviewed. Due to the retrospective nature of this study, the Institutional Review Board of Keimyoung University Dongsan Hospital waived the requirement for patient consent. A single surgeon (LDC) participated in all surgeries and was involved in all clinical patient assessments. Severe corneal erosions and irritating symptoms such as epiphora, often eye blinking and/or rubbing, and photophobia, were included as surgical indications. Patients with post-surgery f/u of as long as 3 months were included. Patients who had congenital entropion, distichiasis, trichiasis, or a history of ocular or eyelid surgery were excluded. A total of 48 eyes of 24 patients were excluded from this study.
Preoperatively, all patients underwent ophthalmological examinations, including best-corrected visual acuity, slit-lamp examinations, cycloplegic refraction, and indirect fundus examinations. In addition, wavefront analyses for calibrated LOAs (anterior and posterior astigmatisms including keratometry were calibrated in ray-traced mode) and HOAs (root mean square [RMS], coma, three-piece aberrations [Trefoil], secondary astigmatisms [2nd Astig], and spherical aberrations [SA]) were measured via a Galilei G4 Dual Scheimpflug Analyzer. These analyses were performed by a single technician preoperatively, and at the first and second f/u in group 1 (less than 45 days post-surgery), group 2 (from 45 to 75 days post-surgery), and group 3 (more than 75 days post-surgery).
Surgical technique
All surgeries were performed under general anaesthesia due to patient age. A mixture of lidocaine 2% and epinephrine (1:100,000) was injected subcutaneously into the lower eyelid. Excess lower eyelid skin was grasped using forceps to cause mild ectropion, and the lid was marked with a pen. The upper skin incision line was approximately 1–2 mm below the eyelash line, with a delineated ellipse more lateral than proximal to the punctum. The width of the ellipse was extended laterally, until reaching close to the lateral canthus to achieve a good contour.
The infra-eyelash skin incision and excision of the pretarsal orbicularis muscle was performed. Subsequently, the surgeon sutured subcutaneous tissue of the upper skin-muscle flap and exposed tarsal plate using three interrupted 6.0 monosyn sutures (medial, centre, and lateral) to achieve a good eyelash contour21. Moreover, a Bovie monopolar needle cautery instrument (Colorado Biomedical Inc, Evergreen, CO) was used for thermal cauterization of the septum to create adhesions between the preseptal orbicularis oculi muscle and the septum22. These adhesions minimized vertical overriding of the orbicularis oculi muscle at the lower eyelid. If there was excessive skin, such as in the form of a dog-ear at the lateral ends of the incision, the surgeon removed them with a triangular skin excision. If there were small amounts of pretarsal orbicularis oculi muscle and redundant skin overlying the lower eyelid margin, the tissue was also removed. At the end of surgery, the skin was then closed with a continuous 6–0 fast-absorbing plain gut suture. Ocuflox antibiotic ointment was used on the skin wound for 4 weeks postoperatively and was then tapered weekly.
Statistical Methods
R language version 3.3.3 (R Foundation for Statistical Computing, Vienna, Austria)23 and T&F program version 2.9 (YooJin BioSoft, Korea) were used for all statistical analyses. Normally distributed variables are expressed as means ± standard deviations (SD), and non-normally distributed variables are expressed as medians (interquartile range). For categorical variables, data are expressed as sample numbers and percentages (N [%]).
Paired sample t-tests were used to test for differences in outcomes from pre- to post-operation. Patients were divided into two subgroups based on age and a Student t-test was used to determine significant differences between the two subgroups. When variables were not normally distributed, Wilcoxon signed rank tests were performed. Kolmogorov-Smirnov normality tests and Shapiro-Wilk normality tests were used to check the normality of all continuous variables.
Univariable linear regression analyses were performed to analyse the independent effects of risk factors such as age, sex, BMI, and cornea keratitis presence on continuous outcomes after surgery. For multivariable analysis, outcomes measured before and after surgery and risk factors such as age, sex, BMI, and cornea keratitis presence were used as paired dependent variables and independent variables, respectively, in a linear mixed-effect model. Time and all risk factors were used as fixed effect covariates with random intercepts across subjects. Statistical significance was reached when two-tailed p-values were less than 0.05.
Results
A total of 108 eyes of 54 patients were included in the study. Baseline patient characteristics, as well as the average f/u times, are shown in Table 1.
Baseline values for LOA and HOA variables are shown in Table 2. In terms of post-surgical changes for LOA variables, flat K was significantly lower at first f/u (p = 0.023) and G3 (p = 0.034) compared to the baseline (see Supplementary Fig. S1), and mean K values were significantly different only at the second f/u (p = 0.034; see Supplementary Fig. S2). Astigmatism values were significantly higher at second f/u (p = 0.026) and G1 (p = 0.026) compared to the baseline (see Supplementary Fig. S3), while sphere values were significantly lower at G1 (p = 0.041; see Supplementary Fig. S4). Axis values were significantly lower at all post-operative time points compared to baseline (p = < 0.001 and 0.015 at G2; see Supplementary Fig. S5). No significant changes across time points were observed for steep K (see Supplementary Fig. S6), SE (D) (see Supplementary Fig. S7), or cylinder values (see Supplementary Fig. S8, Table 3).
In terms of corneal HOAs, both coma (D) (p = 0.006; see Supplementary Fig. S9) and trefoil (D) (p = 0.037; see Supplementary Fig. S10) values were significantly higher at first f/u compared to baseline while SA was significantly lower at second f/u (p = 0.039) and G3 (p = 0.016) compared to baseline (see Supplementary Fig. S11). No significant differences at any of the post-operative time points, compared to baseline, were observed for total RMS (D) (see Supplementary Fig. S12), total RMS (μm) (see Supplementary Fig. S13), Defocus (see Supplementary Fig. S14), or 2nd Astig values (see Supplementary Fig. S15, Table 3).
In this study, the age distribution of patients was from 3 to 12 years (mean ± SD, 6.51 ± 2.49 years). The median age was 6 years with 5 years in the 1st quartile and 8.5 years in the 3rd quartile. Given the wide age distribution, patients were divided into two subgroups based on the median age (6 years old). Patients in Number 1 (N1) were 6 years of age and older (n = 29; mean ± SD, 8.28 ± 1.94 years old) and those in Number 2 (N2) were less than 6 years old (n = 24; mean ± SD, 4.38 ± 0.82 years old). Mean SE and sphere were statistically different between N1 and N2 at baseline, first f/u, and second f/u in LOA; defocus and SA were statistically different between N1 and N2 at baseline and second f/u in HOA (Table 4).
Univariable linear regression analyses were performed to study the effects of risk factors on postoperative outcomes. At the first and second f/u, sex had an effect on all LOA values except first f/u steep K. Additionally, sex had an effect on all values in G3. Age and BMI affected SE in G1, while sex, age, and BMI affected the first and second f/u times in G2. Sex had an effect on astigmatism values only in G2. The presence of cornea keratitis affected second f/u cylinder values in G3, while sex affected these in G2. Sex, age, and BMI further affected first and second f/u sphere values, while age and BMI affected G1 sphere values, and sex and age affected G2 sphere values. The risk factors assessed did not affect axis values at any time point.
In terms of HOAs, total RMS and RMS values were affected by the presence of cornea keratitis at the second f/u only. Age affected defocus values at the second f/u in G2 and G3. However, 2nd astigmatism was not affected by any risk factors at any time point. Age only affected coma values at the second f/u and in G1, while sex, age, and BMI affected them in G2. Only sex had an effect on trefoil values in G3. Finally, age affected SA values in G2 alone.
Next, we analysed the significance of time as a fixed effect after correcting for the effects of the risk factors discussed above on the two outcomes (change from baseline values and univariable regression analysis) measured before and after surgery. To do this, a multivariable linear mixed-effect model was employed. At the first f/u, cylinder, coma, trefoil, and SA were significantly increased (p = 0.039, 0.008, 0.027, and 0.05, respectively), while axis and flat K decreased (p = < 0.001, 0.022) from baseline. At the second f/u, cylinder was increased (p = 0.05), while axis and mean K were significantly decreased (p = \( < \) 0.001 and 0.045, respectively) from baseline. In G1, sphere, axis, and flat K decreased from baseline (p = 0.041, <0.001, and 0.028, respectively), while astigmatism increased significantly (p = 0.028). In G2, axis decreased from baseline (p = 0.001), while coma increased significantly (p = 0.04). In G3, axis, flat K, and SA all significantly decreased from baseline p = < 0.001, 0.009, and 0.011, respectively).
Discussion
Given the current deficiencies in the understanding of visual impairments caused by surgery in patients with epiblepharon, this study aimed to investigate post-operative changes in corneal LOAs and HOAs after lower eyelid epiblepharon repair in children. This surgical procedure was demonstrated to cause significant changes in axis, flat K, mean K, SA, coma, and trefoil values.
Many kinds of postoperative visual disturbances due to refractive power changes after ocular surgery have been reported previously. Specifically, severe or irregular astigmatism, changes in the astigmatic axis, myopic or hyperopic shifts, changes in axial length, and positional or dioptric errors in the implanted intraocular lenses have been attributed to visual disturbances and refractive changes in the postoperative period24,25,26,27,28,29 ‘With-the-rule’ astigmatism often occurs in epiblepharon patients, as the present paper demonstrates.
The prevalence of ‘with-the-rule’ astigmatism, defined as an axis of astigmatism of 180 ± 15°, has been reported to range from 60.7% to 90.5%7,8,9,30,31. Here, we report changes from ‘with-the-rule’ to ‘against-the-rule’ astigmatism from 138.26° to 86.05° at 1st f/u and 85.93° at 2nd f/u (see Supplementary Fig. S5). Furthermore, flat K and mean K decreased after surgery in the present study. Astigmatisms derived from epiblepharon patients seem to result from corneal changes resulting from the mechanical force caused by abnormal eyelid tension. This tension is caused by redundant horizontal skin folds associated with the hypertrophied pretarsal orbicularis muscle and squeezing or spasms of the eyelids caused by corneal irritation32. In contrast, Shin et al. reported that more severe corneal problems, such as erosion in epiblepharon, were associated with more astigmatism, which persisted after corneal erosions healed9. Khwarg et al. further reported that a higher number of touching cilia and injury of the cornea were correlated with more severe astigmatism. Therefore, long-term corneal epithelial erosion is thought to consist of cellular apoptosis and cytokine release. It may also result in tissue remodelling and keratoconus33,34. According to this model, long-term cornea erosion and the mechanical force of the eyelid cause corneal remodelling and induce astigmatism.
Over the course of the first two post-operative assessments, a trend was observed for the decrease in axis, flat K, and mean K values. This may indicate decreased lower eyelid mechanical force and the presence of cornea keratitis in epiblepharon patients. Vertical pressure by redundant skin folds in the hypertrophied pretarsal orbicularis oculi muscles on the cornea may have resulted in horizontal flattening of the cornea, which could explain the high prevalence of with-the-rule astigmatism in these cases, and flat K change immediately after epiblepharon repair surgery. Conversely, cylinder values were unaffected by epiblepharon surgery. Flat K returned to baseline values in G1 and G2, although a significant drop was observed in G3, and mean K was significantly decreased only at the second f/u. Flat K was more affected by mechanical eyelid forces, while mean K was more affected by corneal erosion.
Correcting for the effects of multiple risk factors (age, sex, BMI, and cornea keratitis presence) on post-surgical outcomes using a multivariable linear mixed-effect model revealed increased cylinder and a significantly decreased flat K at the first f/u. Cylinder and mean K were also significantly different from baseline at the second f/u. This may be because cylinder and keratometry were slightly affected by epiblepharon repair surgery after correcting for LOA risk factors. Given that we used the Galilei G4 Dual Scheimpflug Analyzer to correct for both anterior and posterior astigmatisms, the present study may more accurately reflect pre- to post-epiblepharon surgery topography changes than simulated keratometry approaches that were used previously. Previous studies have reported astigmatic amblyopia in 6–9% of epiblepharon patients7,31. Therefore, in children who have undergone surgical procedures such as epiblepharon repair or strabismus surgery, close monitoring of any refractive changes in the postoperative period is crucial in preventing the development of amblyopia.
HOAs are generally indices of visual quality, including in children35. As problems with the cornea are increasingly numerous during development, visual disturbances including distortion and the appearance of glare and halos may occur. However, correction of HOAs improves contrast sensitivity and visual quality. For instance, previous work has found that total HOAs decrease significantly after epiblepharon repair surgery. Critically, the correlation between reduced corneal staining grade and decreased total HOAs may inform the right time of surgery in children without specific visual disturbance and photopobia32. However, the present study found that coma and trefoil were significantly increased after epiblepharon repair surgery at the first f/u, and normalized by the second f/u rather than being decreased, supporting previous results32. In fact, we found that only SA decreased at the second f/u (especially in G3). Notably, HOAs cannot be corrected by ordinary glasses or contact lenses. Therefore, this indicates that correcting a lens with an astigmatism about 10 days after surgery may not be optimal. About 2 months after epiblepharon surgery may be the optimal time to use correcting lenses.
When accounting for multiple risk factors using a linear mixed-effect model, changes induced by surgery, coma, trefoil, and SA were increased at the first f/u. However, these measures returned to baseline by the second f/u. In G2, only coma increased relative to baseline, while in G3, only SA decreased relative to baseline. This means that coma and trefoil might be affected by the immediate mechanical force changes after surgery, while SA was affected by cornea healing post-operation, especially more than 75 days after surgery.
Recent studies have found that HOAs were significantly more common in patients with dry eye syndrome than in those with healthy eyes36,37, and total ocular HOAs were significantly more common in those with dry eyes and central corneal keratitis than in those with dry eyes alone38. Ocular dryness and eye conditions may have a large effect on the outcomes reported here, as indicated by prior studies on HOAs36,37,38. In this study, we found that HOAs generally increased after epiblepharon repair and then almost immediately returned to baseline values. However, these post-surgical results likely vary depending on eye management with hyaluronic acid and other variables such as eye dryness. We were limited by an inability to assess tear film break up time (TBUT) due to the retrospective nature of the present study. It is suggested that future studies consider controlling for this variable when assessing outcomes following epiblepharon surgery. Non-clinical (e.g., animal) models may be useful for further investigating the factors that lead to a high level of aberrations, such as dry eye syndrome and cornea erosion state.
In the present study, we divided the patients into two subgroups due to their wide age distribution. In LOA, mean SE and sphere were statistically different between patients 6 years of age and older and those patients who were less than 6 years old at baseline. In HOA, defocus and SA were also different between the two subgroups (Table 4). These findings suggest that age might affect the corneal state at baseline. In future studies, it may be advantageous to restrict the age distribution as much as possible in order to reduce bias due to differences in the corneal state at baseline.
A limitation of the present study was the small sample size, which makes it difficult to generalize our results to a broader range of clinical populations. A larger sample size, including patients with or without surgery, would facilitate additional comparisons between control and experimental groups to further assess corneal changes in epiblepharon patients. Future prospective studies with a larger numbers of patients are also needed to gain insight into the postoperative eyelid changes following epiblepharon surgery. Another limitation of our study was the relatively short f/u period. As this was a retrospective study, our analyses were based on the reported f/u periods. The reported f/u results we were able to obtain were preoperative, approximately 1 week after operation, and approximately 3 months postoperatively, which we divided into three groups. Additional observational f/u after surgery is typically not available until one year or more after lower eyelash stinging has abated. Since the patients were between the ages of 3 and 12 years old, it was not easy to examine the HOA after the patient had been transferred to the pediatric ophthalmology department after surgery. Future prospective studies with longer f/u periods (from 1–3 years) after surgery may provide additional insight into the extent of corneal changes achieved by epiblepharon surgery.
In conclusion, epiblepharon repair surgery may result in a shift from ‘with-the-rule’ to ‘against-the-rule’ axis changes. Additionally, flat K, coma, and trefoil were affected by mechanical force changes immediately following surgery. Mean K and SA may also be affected by cornea state changes, including corneal erosion healing after the second f/u in the postoperative period.
References
Jeong, S., Park, H. & Park, Y. G. Surgical correction of congenital epiblepharon: low eyelid crease reforming technique. J. Pediatr. Ophthalmol. Strabismus 38, 356–358 (2001).
Noda, S., Hayasaka, S. & Setogawa, T. Epiblepharon with inverted eyelashes in Japanese children. I. Incidence and symptoms. Br. J. Ophthalmol 73, 126–127 (1989).
Tan, M. C., Young, S., Amrith, S. & Sundar, G. Epidemiology of oculoplastic conditions: the Singapore experience. Orbit 31, 107–113 (2012).
Bartley, G. B., Nerad, J. A., Kersten, R. C. & Maguire, L. J. Congenital entropion with intact lower eyelid retractor insertion. Am. J. Ophthalmol. 112, 437–441 (1991).
Tse, D. T., Anderson, R. L. & Fratkin, J. D. Aponeurosis disinsertion in congenital entropion. Arch. Ophthalmol. 101, 436–440 (1983).
Lemke, B. N. & Stasior, O. G. Epiblepharon. An important and often missed diagnosis. Clin. Pediatr. 20, 661–662 (1981).
Preechawai, P., Amrith, S., Wong, I. & Sundar, G. Refractive changes in epiblepharon. Am. J. Ophthalmol 143, 835–839 (2007).
Park, S. W., Sok, J. Y. & Park, Y. G. The effect of surgical correction of epiblepharon on astigmatism in children. J. Pediatr. Ophthalmol. Strabismus 45, 31–35 (2008).
Shih, M. H. & Huang, F. C. Astigmatism in children with epiblepharon. Cornea 26, 1090–1094 (2007).
Kim, N. M., Jung, J. H. & Choi, H. Y. The effect of epiblepharon surgery on visual acuity and with-the-rule astigmatism in children. Korean J. Ophthalmol. 24, 325–330 (2010).
Siso-Fuertes, I., Dominguez-Vicent, A., del Aguila-Carrasco, A., Ferrer-Blasco, T. & Montés-Micó, R. Corneal changes with accommodation using dual Scheimpflug photography. J. Cataract Refract. Surg. 41, 981–989 (2015).
Lombardo, M. & Lombardo, G. Wave aberration of human eyes and new descriptors of image optical quality and visual performance. J. Cataract Refract. Surg. 36, 313–331 (2010).
Artal, P., Guirao, A., Berrio, E. & Williams, D. R. Compensation of corneal aberrations by the internal optics in the human eye. J. Vis. 1, 1–8 (2001).
Artal, P. & Guirao, A. Contributions of the cornea and the lens to the aberrations of the human eye. Opt. Lett. 23, 1713–1715 (1998).
Marcos., S. P. Aberrations and visual performance following standard laser vision correction. J. Refract. Surg. 17, S596–S601 (2001).
Oshika, T., Klyce, S. D., Applegate, R. A., Howland, H. C. & El Danasoury, M. A. Comparison of corneal wavefront aberrations after photorefractive keratectomy and laser in situ keratomileusis. Am. J. Ophthalmol. 127, 1–7 (1999).
Applegate, R. A., Howland, H. C., Sharp, R. P., Cottingham, A. J. & Yee, R. W. Corneal aberrations and visual performance after radial keratotomy. J. Refract. Surg. 14, 397–407 (1998).
Fujikado, T. et al. Light scattering and optical aberrations as objective parameters to predict visual deterioration in eyes with cataracts. J. Cataract Refract. Surg. 30, 1198–1208 (2004).
Oshika, T., Kawana, K., Hiraoka, T., Kaji, Y. & Kiuchi, T. Ocular higher-order wavefront aberration caused by major tilting of intraocular lens. Am. J. Ophthalmol. 140, 744–746 (2005).
Guirao, A. et al. Corneal optical aberrations and retinal image quality in patients in whom monofocal intraocular lenses were implanted. Arch. Ophthalmol. 120, 1143–1151 (2002).
Woo, K. I., Yi, K. & Kim, Y. D. Surgical correction for lower lid epiblepharon in Asians. Br. J. Ophthalmol 84, 1407–1410 (2000).
Chang, M., Lee, T. S., Yoo, E. & Baek, S. Surgical correction for lower lid epiblepharon using thermal contraction of the tarsus and lower lid retractor without lash rotating sutures. Br. J. Ophthalmol. 95, 1675–1678 (2011).
R Core Team (2017). R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria, http://www.R-project.org/.
Kushner, B. J. The effect of oblique muscle surgery on the axis of astigmatism. J. Pediatr. Ophthalmol. Strabismus 23, 277–280 (1986).
Spierer, A. & Bar-Sela, S. Changes in astigmatism after congenital cataract surgery and foldable intraocular lens implantation. J. Pediatr. Ophthalmol. Strabismus 41, 35–38 (2004).
Bagheri, A., Farahi, A. & Guyton, D. L. Astigmatism induced by simultaneous recession of both horizontal rectus muscles. J. AAPOS. 7, 42–46 (2003).
Godts, D., Tassignon, M. J. & Gobin, L. Binocular vision impairment after refractive surgery. J. Cataract Refract. Surg. 30, 101–109 (2004).
Randleman, J. B., Hewitt, S. M. & Stulting, R. D. Refractive changes after posterior segment surgery. Ophthalmol. Clin. North Am. 17(521-526), v-vi (2004).
Nayak, H., Kersey, J. P., Oystreck, D. T., Cline, R. A. & Lyons, C. J. Diplopia following cataract surgery: a review of 150 patients. Eye 22, 1057–1064 (2007).
Khwarg, S. I. & Lee, Y. J. Epiblepharon of the lower eyelid: classification and association with astigmatism. Korean J. Ophthalmol. 11, 111–117 (1997).
Yang, S. W., Choi, W. C. & Kim, S. Y. Refractive changes of congenital entropion and epiblepharon on surgical correction. Korean J. Ophthalmol. 15, 32–37 (2001).
Lee, H., Jang, S., Park, M., Park, J. & Baek, S. Effects of epiblepharon surgery on higher-order aberrations. J. AAPOS. 20, 226–231 (2016).
Jafri, B., Lichter, H. & Stulting, R. D. Asymmetric keratoconus attributed to eye rubbing. Cornea 23, 560–564 (2004).
Wilson, S. E. et al. Epithelial injury induces keratocyte apoptosis: hypothesized role for the interleukin-1 system in the modulation of corneal tissue organization and wound healing. Exp. Eye Res. 62, 325–327 (1996).
Song, I. S., Kim, M. J., Yoon, S. Y., Kim, J. Y. & Tchah, H. Higher-order aberrations associated with better near visual acuity in eyes with aspheric monofocal IOLs. J. Refract. Surg. 30, 442–446 (2014).
Montes-Mico, R., Caliz, A. & Alio, J. L. Wavefront analysis of higher order aberrations in dry eye patients. J. Refract. Surg. 20, 243–247 (2004).
Montes-Mico, R., Alio, J. L. & Charman, W. N. Dynamic changes in the tear film in dry eyes. Invest. Ophthalmol. Vis. Sci. 46, 1615–1619 (2005).
Koh, S. et al. Serial measurements of higher-order aberrations after blinking in patients with dry eye. Invest. Ophthalmol. Vis. Sci. 49, 133–138 (2008).
Acknowledgements
This work was supported by the Keimyung University Research Grant of 2018. The author would like to thank Editage (www.editage.co.kr) for the English language editing.
Author information
Authors and Affiliations
Contributions
L.D.C. carried out all the work.
Corresponding author
Ethics declarations
Competing interests
The author declares no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lee, D.C. Analysis of corneal real astigmatism and high order aberration changes that cause visual disturbances after lower eyelid epiblepharon repair surgery. Sci Rep 10, 7498 (2020). https://doi.org/10.1038/s41598-020-64386-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-64386-6
This article is cited by
-
Severe corneal involvement secondary to congenital lower eyelid epiblepharon
Graefe's Archive for Clinical and Experimental Ophthalmology (2023)
-
Cylinder power progression associated with axial length in young children: a two-year follow-up study
Graefe's Archive for Clinical and Experimental Ophthalmology (2023)
-
Effect of upper eyelid blepharoplasty on corneal biomechanical, topographic and tomographic parameters 4 weeks after surgery
International Ophthalmology (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.