Abstract
This study aimed to examine the effect of transcutaneous electrical nerve stimulation (TENS) on stair climbing capacity in individuals with pre-radiographic to mild knee osteoarthritis (OA). This is a secondary analysis of data from a single, participant-blinded, randomized controlled trial with a pre-post design. Participants with pre-radiographic to mild knee OA (mean age, 59.1 years; 72.9% women) were randomly assigned into two groups, a TENS (n = 30) and a sham-TENS groups (n = 29). TENS or sham-TENS treatments were applied to all participants by using the prototype TENS device with pre-specified parameters. The primary outcome measures included valid and reliable functional measures for stair climbing (stair-climb test [SCT]), visual analog scale for knee pain during the SCT, and quadriceps muscle strength. TENS improved SCT time by 0.41 s (95% confidence interval [CI]: 0.07, 0.75). The time reduction in the transition phase explains the TENS therapeutic effect. Post-hoc correlation analyses revealed a non-significant but positive relationship between the pain relief effect and improved 11-step SCT time in the TENS group but not in the sham-TENS group. These results indicate that the TENS intervention may be an option for reducing the burden of early-stage knee OA.
Similar content being viewed by others
Introduction
Knee osteoarthritis (OA) is a leading cause of knee pain and chronic disability in the elderly and subsequent mobility limitation1,2. Mobility limitation is typically considered one of the most significant consequences in individuals with knee OA. Weight-bearing activities that involve large knee flexion, such as stair climbing, are biomechanically and physiologically more challenging than level walking3,4 and are thought to be the first mobility limitation observed in individuals with knee OA5. A meta-analysis of 12 articles revealed that longer performance time was an alteration associated with knee OA during stair ambulation6. Although the mechanism of poor stair climbing capacity in knee OA is unclear, severe knee pain and consequent weaker quadriceps muscle power are potential modifiable factors that contribute to poor stair climbing capacity7. Pain-relieving intra-articular knee injection8 and quadriceps strength exercise9 improve stair climbing capacity, which indicates that treatment targeting these factors may alleviate the burden of the earliest stage of knee OA.
Transcutaneous electrical nerve stimulation (TENS) is an effective pain control modality for OA-related knee pain10. TENS treatment is beneficial for increasing isometric quadriceps muscle activation, possibly through reduced knee pain and increased quadriceps motor neuron pool excitability11, in patients with knee OA12,13. These evidences indicate that TENS may improve stair climbing capacity by reducing knee pain and increasing quadriceps muscle strength. Cherian et al. showed that 12 weeks of TENS treatment for individuals with severe knee OA did not significantly improve their stair climbing capacity14, which was possibly due to severe radiographic disease. Given that patients with less severe radiographic disease respond better to therapeutic interventions than those with severe disease15,16, TENS intervention targeting patients with less severe knee OA would be more effective in improving stair climbing function.
From a biomechanical perspective, stair descending involves higher knee extension moment, a leading cause of knee pain, than stair ascending3,17. The stair-climb test (SCT) is a validated and typical functional assessment for stair ambulation18 and can identify functional limitation better than other objectively measured functional assessments (e.g., timed up and go test and 6-minute walk test) in patients with knee OA19. However, the SCT incorporates stair ascending and descending, and their transition, which may represent distinct functional constructs. The total timed score of SCT limits our interpretation of the proportional contribution of these subtasks and therapeutic efficacy of the TENS treatment. As more severe pain and pain-related inhibition of muscle contraction were expected in stair descending, it was plausible that TENS treatment had a greater impact on stair descending than stair ascending. Thus, this study aimed to test the following hypotheses: (1) TENS has a greater impact on stair climbing capacity, the time to perform stair ascending, descending, and their transition, than sham TENS; (2) TENS is more effective for improving stair descending than ascending; (3) the beneficial effects of TENS on stair climbing capacity are driven through reduced knee pain; and (4) the beneficial effects of TENS on stair climbing capacity are driven through increased quadriceps muscle strength/activation in individuals with pre-radiographic to mild knee OA.
Results
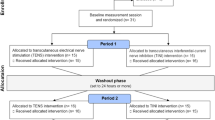
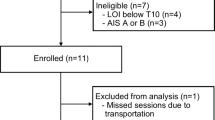
Fifty-nine participants (mean age, 59.1 years; mean body mass index [BMI]: 22.7 kg/m2; 72.9% were women) were included and randomized into the sham-TENS (n = 29) and TENS groups (n = 30). All the participants completed the post-treatment outcome measurements without any adverse events. Data from the results of the insole-based 11-step SCT (11-SCT) in the baseline period from one patient were imputed. Table 1 shows the comparison of participant characteristics between the sham-TENS and TENS groups.
Table 2 shows a comparison of changes in outcome measures between the sham-TENS and TENS groups after multiple imputation. The between-group differences in change in knee pain and quadriceps muscle strength were not significantly different. The proportion of treatment responders (i.e., visual analog scale [VAS] pain score improved by ≥30% from baseline to post-treatment) did not differ between the sham-TENS and TENS groups (relative risk to responder in the TENS group: 1.03; 95% confidence interval [CI]: 0.65, 1.62). Although the between-group difference in the change in stopwatch-based 11-SCT time was not significant, that in the insole-based 11-SCT time was 0.41 s (95% CI: − 0.75, −0.07 s), which showed better improvement in the patients in the TENS group than in those in the sham-TENS group. When insole-based 11-SCT time was further divided into three phases (ascending, descending, and transition), the between-group difference in the transition phase time was 0.32 s, which was more improved in patients in the TENS group than in those in the sham-TENS group. The case completed data, excluding one patient in the sham-TENS group, showed similar results (data not shown).
A graphic illustration of these relationships is provided in Fig. 1 to further address the relationship between the pain-relief and therapeutic effect of TENS on the stopwatch- (Fig. 1A) and insole-based 11 SCT times (Fig. 1B). The post-hoc correlation analyses revealed a positive relationship between the change in VAS pain score during SCT and the change in stopwatch- (r = 0.22; 95% CI: −0.15, 0.54) and insole-based 11-SCT times (r = 0.39; 95% CI: 0.04, 0.66) in the TENS group, which were higher than those in the sham-TENS group (stopwatch-based 11-SCT, r = 0.01; 95% CI: −0.35, 0.38; insole-based 11-SCT, r = −0.02; 95% CI: −0.39, 0.36). The interaction effect of group × change in VAS pain score on the insole-based 11-SCT time was marginally significant (p = 0.080).
Illustration of the relationship between pain relief and therapeutic effect on stair climbing capacity. (A) Change in VAS pain score during SCT and change in stopwatch-based 11-SCT time. (B) Change in VAS pain score during 11-SCT and change in insole-based 11-SCT time. Linear regression lines and Pearson correlation coefficients (95% confidence intervals) are provided. p-values for group-change in VAS pain score interaction effect are also provided.
Discussion
The objective of this study was to examine the therapeutic effects of TENS on stair climbing capacity in individuals with pre-radiographic to mild knee OA. Supporting the first hypothesis, TENS improved the 11-SCT time better than sham-TENS. However, contrary to the second hypothesis, the therapeutic effect of TENS was similar between stair descending and ascending during the 11-SCT. Furthermore, TENS was not superior to sham-TENS in improving knee pain during stair climbing and quadriceps strength, which does not support the third and fourth hypotheses. The improved stair climbing ability by TENS was not due to the reduced knee pain and increased quadriceps muscle strength, although the post-hoc correlation analyses revealed a non-significant but positive relationship between the pain relief effect and improved 11-SCT time in the TENS group. The main finding of this study is that TENS improved stair climbing capacity, determined using a sensor-mounted insole, better than sham-TENS in the patients with earlier radiographic OA stage. The time reduction in the transition phase during TENS treatment mostly explained the therapeutic effects (see graphic abstract, Fig. 2). As poor stair climbing capacity is thought to be the first mobility limitation observed in individuals with knee OA5, these findings indicate that TENS may be an option for reducing early-stage knee OA-related burden.
Graphic abstract. TENS improved insole-based 11-SCT time (ES: −0.80; 95% CI: −1.33, −0.26) better than sham-TENS in people with pre-radiographic to mild knee OA, which was through reducing transition time (ES: −0.79; 95% CI: −0.1.32, −0.26) rather than ascending (ES: 0.01; −0.50, 0.52) and descending stair time (ES: −0.39; −0.90, 0.13). ES, effect size; 95% CI, 95% confidence interval.
Interpretation of the Effects of TENS on Stair Climbing Capacity
In this study, we found that TENS improved insole-based SCT time by 0.41 s, which is beyond the 95% CI of measurement error. This therapeutic effect on SCT time is not consistent with the findings of a previous study that showed that 12 weeks of TENS treatment in individuals with severe knee OA did not significantly improve SCT time14. This discordance may be attributed to the difference in radiographic disease severity. Approximately 85% of the study participants had pre-radiographic knee OA (K&L grade ≤1), who may respond better to therapeutic interventions than those with severe disease15,16. Furthermore, insole-based SCT may be more sensitive than stopwatch-based SCT in detecting the efficacy of therapeutic treatment, although the stopwatch-based SCT has high reliability and validity18. It should be acknowledged that this study is a secondary analysis from randomized controlled trial (RCT) data without calculation of the required sample size to detect the therapeutic effect of TENS on 11-SCT time. Thus, a type II error may exist, and the non-significant TENS treatment effects on the stopwatch-based 11-SCT time may be attributed to the low statistical power, given that the upper limit of the 95% CI in the stopwatch-based 11-SCT improvement was almost zero.
Contrary to the hypothesis, TENS did not significantly improve the time during stair descending that requires higher internal knee extension moment3,17. It is Interesting that the time reduction in the transition phase during TENS treatment mostly explained its therapeutic effects. Although the exact mechanism is unclear, the transition phase involves a quick turn that increases the external knee rotational moment20, which may cause knee pain and a subsequent impairment of smooth transition from stair descending to ascending. This preliminary finding warrants validation of the association between knee pain and impaired transition motion, and whether the transition motion responds well to pain-relief treatment.
Theoretically, the TENS treatment reduces pain through selective stimulation for large-diameter, low-threshold non-noxious afferents in dermatomes related to pain21 and increases quadriceps motor neuron pool excitability11. Nevertheless, this study could not detect significant between-group improvements in knee pain during 11-SCT and quadriceps muscle strength immediately after TENS, although the same TENS protocol improved knee pain and walk distance during 6-minute walk test22. Further studies would be needed to determine what factors mediate the therapeutic effect of TENS. As improved knee pain was associated with improved 11-SCT time only in the TENS group, the underlying mechanism associated with change in 11-SCT may be different between the sham-TENS and TENS groups.
Significance and Clinical Impact of the Study
TENS was effective in improving mobility during insole-based 11-SCT, including people with pre-radiographic OA, the earliest clinical manifestation associated with knee OA5. This finding may help clinicians and physical therapists provide effective therapy for patients with early-knee OA who have difficulty performing weight-bearing activities that involve large knee flexion. TENS may be an option for reducing early-stage knee OA-related burden, which should be validated in future clinical trials.
The type of measurement metrics is important for identifying the therapeutic effects of TENS, and this study used both the stopwatch- and insole-based 11-step SCT. The stopwatch-based 11-SCT may not adequately identify the therapeutic effects of TENS, although non-significant results may come from the low sample size. Thus, biomechanically and physiologically more challenging tasks (e.g., 15-step SCT) might be suitable in adequately determining the therapeutic effect by using a stopwatch in the clinical setting. Further studies are warranted to address this question.
Study limitations
First, this study examined the immediate effects of TENS without follow-up. This study cannot specify optimal TENS treatment protocol. Second, the knee pain intensity on the testing day was quite mild in both groups, although all the participants experienced pain at a mean score of >4 but <9 on a numeric rating scale. As severe knee pain at baseline could influence the pain relief effects of the TENS treatment, the relatively mild pain profile of the included participants may underestimate the pain relief effects of the TENS treatment. Third, the 11-SCT in this study was performed while wearing standard shoes, which may not be used in clinical practice. Data should be interpreted with caution because most clinicians would perform stopwatch-based 11-SCT while the participants wear their own footwear, which might influence the SCT time. Fourth, this study did not calculate the required sample size, as this study is a secondary analysis of RCT data22. Finally, the lack of muscle activity data such as electromyography data limited our analysis. As patients are required to use their quadriceps submaximally, the muscle activity during the 11-SCT for quadriceps motor neuron activation may be a better option for identifying the therapeutic effect of TENS.
In conclusion, TENS immediately improved the 11-SCT time better than sham-TENS. However, the therapeutic effect of TENS was similar between stair descending and ascending during the 11-SCT, and the time reduction in the transition phase during the TENS treatment mostly explained its therapeutic effects. The improved stair climbing ability by TENS was not due to the reduced knee pain and increased quadriceps muscle strength, although post-hoc correlation analyses revealed a non-significant positive relationship between the pain relief effect and the improved 11-SCT time in the TENS group. Given that stair climbing is suggested to be the first task that is affected in people with knee OA, TENS intervention may be an option for reducing early-stage knee OA-related burden, which should be validated in future clinical trials.
Methods
Study design and participants
This study was a secondary analysis of data from a RCT that examined the effects of TENS on knee pain and physical function in individuals with painful knee OA22. The institutional ethics committee of Kyoto University Graduate School and Faculty of Medicine approved the study (approval No. C1349). The study was conducted in compliance with Good Clinical Practice, the ethical standards of the responsible committee on human experimentation (institutional and national) and the Declaration of Helsinki 1975. Written informed consent was obtained from all participants before their enrollment. The required sample size in the RCT was calculated on the basis of the data from a previous clinical trial to detect the therapeutic effects of TENS. Details for sample size calculation were provided in the original RCT study22. Community-dwelling adults who reported knee pain within the last month were identified through a website. Subjects interested in this study answered a questionnaire concerning their physical condition, and those who met the inclusion criteria were invited to the university in February 2018 to participate in the study. The eligibility criteria included (1) age of ≥50 years; (2) Kellgren and Lawrence (K&L) grade of ≤2 in one or both knees as evaluated using weight-bearing anteroposterior radiographs, and (3) mean pain score of ≥4 but ≤9 on a numeric rating scale (0–10 total points) in the last month. The participants were excluded if they (1) had a history of knee surgery or intra-articular corticosteroid or hyaluronic acid injection within the last 6 months, (2) had a history of knee joint replacement or tibial osteotomy, (3) were receiving physical therapy, (4) had pain in any other major joints (e.g. back, hip, or ankle) with a greater effect than their knee pain on the current ability limits, (5) had severe medical conditions (e.g., chronic obstructive pulmonary disease, cardiovascular disease, arteriosclerosis obliterans, cerebrovascular accident, lumbar disk herniation, and rheumatoid arthritis), (6) did not usually use stairs in daily living, and (7) did not have the ability to walk and climb stairs without an ambulatory assistive device and handrail. Although the original RCT excluded patients with K&L grade 2 after data assessment22, this secondary study included these patients to increase its statistical power.
Randomization
The participants were randomly allocated to one of the two groups, the TENS or sham-TENS group, by using stratified and block randomization22. Studies have shown that female patients have a lower sensory threshold and respond to electrical stimulation differently from male patients;7,8 thus, blocks were stratified by sex. Details for randomization were provided in the original RCT study22.
TENS Intervention
The TENS and sham-TENS treatments were applied to index knee of all participants using the prototype TENS device (HV-F710, Omron Healthcare Co., Ltd., Kyoto, Japan) with pre-specified parameters (sweep mode from 1 to 250 Hz, symmetrical biphasic pulse, and a 60-μs pulse width). Sweep mode was chosen because low and high frequency TENS demonstrate analgesic effects in different mechanism, and the combination of these frequencies is supposed to be more effective in reducing pain than alone23. The index knee was defined as the more painful knee at inclusion. The intensity in the TENS group was gradually increased and limited by the participant’s perception of a “strong but comfortable, non-painful tingle” immediately below the visible motor threshold. The participants in the sham-TENS group received sham stimulation at the same sites. TENS and sham-TENS were applied just before functional assessments explained in original RCT study22. Treatment time was not strictly set because previous Cochrane review showed similar therapeutic effects on knee pain and functional outcomes regardless of treatment time of ≤20 min, 30 to 40 min, and 60 ≥ min24. The TENS units were turned off when all the functional assessments were completed, for a total application time of around 60 minutes. Trained physical therapists with clinical experience in the musculoskeletal field performed the procedures. More information on the treatment procedure was provided in the original RCT22.
Outcome measurement
The participants were assessed by the same assessor at baseline and during the treatment period. The primary outcome measures included valid and reliable functional measures for stair climbing, VAS for knee pain during SCT, and quadriceps muscle strength.
Instrumentation
Footwear influences balance performance25,26 and walking speed26; thus, all the participants wore standard shoes (LD AROUND M, Mizuno, Tokyo, Japan) with a pressure sensor (Force register sensors Model 402, Interlink Electronics Inc., CA, USA) to avoid any potential bias from the participants’ wearing of their own footwear27. Fifteen sensors were attached in the shoe insole to enable detection of the precise initial contact and foot off time point during the SCT. During stair climbing, forefoot contact without heel contact was expected, and a pilot study for healthy adults indeed confirmed the forefoot initial contact during stair descending (data not shown). In-shoe foot pressure sensors can more precisely detect foot contact than single foot sensor. Furthermore, this method allows examination of the stair climbing capacity using actual stairs outside the motion laboratory. The sensors were connected to a flexible circuit board containing a microcontroller and micro-SD card placed on the participants’ lower legs27. Although the footwear was novel for each participant, all the subjects reported that the shoes were comfortable and caused no pain. Data were sampled at 100 Hz.
Procedure for the 11-Step Stair-Climb Test
Each participant underwent the SCT in accordance with the OARSI recommended method28, while wearing pressure sensor-mounted standard shoes. To exclude the influence of the participants’ clothes on the stopwatch operability, the participants’ pants were rolled up to the knee level. The 11-SCT with a regular stairwell was selected because it represents the type and size of stairs that subjects likely need to manage during daily activities, and some previous studies that examined reliability also used 11-SCT29,30. The participants descended and ascended a flight of stairs, which consisted of 11 steps with step height, width, and tread of 17, 135, and 29 cm, respectively. Although the standard SCT starts from the ascending stairs, the 11-SCT in this study started from descending stairs because of environmental constraints. The pilot study confirmed that the 11-SCT time in the 6 healthy adults (mean age: 24.3 years) did not significantly differ between starting ascending and descending (data not shown). A trained physical therapist (KS) measured the time required to perform 11-SCT in all the participants’ test and retest sessions by using a stopwatch (TD-392, Tanita Corp., Tokyo, Japan). On the trained physical therapist’s “start” command, each participant was instructed to walk as quickly and safely as possible without running31 and was subsequently retested to ensure that their physical condition was stable over the testing period. The use of any walking aid or handrail was prohibited. The participants performed one practice trial for familiarization and to verify their safety. Stopwatch-based 11-SCT time was defined as the time from the therapist’s command to “start” to the subject reaching the point where both feet were on the top platform. The stopwatch and insole measurements were performed simultaneously.
To determine insole-based 11-SCT time, vertical ground reaction force (GRF) was calculated from the sensor-mounted shoe data as previously described27. Subsequently, initial contact and foot off were defined as the time point where the vertical GRF exceeded and was <1% of the threshold of the estimated maximum GRF using MATLAB version R2017a (MathWorks Inc., Natick, MA, USA). The insole-based 11-SCT time was defined as the time from the initial foot off on the top platform to the point of foot contact in both feet on the top platform. By using the initial contact and foot off data, the insole-based 11-SCT time was further divided into three phases, namely descending, ascending, and transition. The transition phase was defined as the time between initial contact to staircase landing after descending and initial contact to the first step during ascending. The test–retest reliability was excellent for the stopwatch-based (intraclass correlation coefficient [ICC1,1], 0.952 s; 95% CI, 0.560, 0.985 s) and insole-based 11-SCT times (ICC1,1, 0.929 s; 95% CI, 0.883, 0.957 s). The minimal detectable changes (MDC95) for stopwatch- and insole-based 11-SCT times were 0.102 s and 0.089 s, respectively.
Knee Pain Intensity during Stair-Climb Test
Knee pain during SCT was evaluated after the 11-SCT by using the VAS (0–100 mm). Each participant was asked the following “Please mark on where you think the level of pain you experienced during stair climbing.” The participants recorded their level of knee pain by drawing a vertical mark between the ends of a 100-mm horizontal line. The 0- and the 100-mm end represented no pain and most extreme pain, respectively. The distance from the 0-mm end to the drawn mark was recorded to the first decimal place.
Quadriceps muscle strength
The maximum isometric quadriceps (Nm/kg) in both legs were measured using a hand-held dynamometer (HHD; μTas F-1, Anima Corp., Tokyo, Japan) in accordance with a method previously validated for use on community-dwelling elderly fallers32. The participants were instructed to remain seated in an upright position. The knee was placed in 90° flexion, with the HHD attached 10 cm proximal to the lateral malleolus and held in place with an inelastic strap that was looped around the therapy bed and fastened. The length of the straps allowed for an isometric contraction to be performed, with the knee at 90° flexion during testing. The participants were instructed to extend their leg for 5 s. Strong verbal encouragement was provided to ensure maximum effort. To provide moment value (Nm), the lever arm (length of tibia) between the knee joint and the HHD was manually measured and subsequently normalized to their mass (Nm/kg). The means of the values from the two exercises were used for statistical analysis.
The MDC95 was calculated using 100 randomly selected participants (i.e., 200 knees) to determine the smallest degree of change outside the muscle strength testing error range. The MDC95 was 0.227 Nm/kg. The intra-rater reliability was excellent for quadriceps strength (ICC1,1: 0.939; 95% CI: 0.921, 0.954).
Patient Characteristics
Data on age, sex, and height were self-reported by the patients. Body mass was measured on a stadiometer with the participants clothed without shoes. BMI was calculated by dividing the weight in kilometers by the height in meters squared. The knee OA-related health domain measure, the Japanese Knee Osteoarthritis Measure (JKOM), was evaluated33. The concurrent and construct validities of the JKOM were established by comparing the Western Ontario and McMaster Universities Arthritis Index and the Medical Outcomes Study 36-item Short-Form Health Survey score33. Radiographic OA severity in both knees was assessed in the anteroposterior short view in the weight-bearing position, similarly to a previous study34.
Statistical analyses
Statistical analysis was performed on an intention-to-treat basis and included all patients who were randomized into two groups. To account for missing data, primary analyses included multiple imputation technique. Imputation of insole-based 11-SCT for one patient data was conducted. Imputed data set was formed using the multiple imputation procedure of SPSS Statistics for Windows, Version 23.0 (IBM Corp., NY, USA). Sensitivity analysis was performed using all available data without imputation (complete cases).
Multiple regression analysis was performed with TENS intervention (0: no, 1: yes) as independent variable and with each outcome measure (continuous) as dependent variable after adjusting for the baseline value of each outcome. The change in VAS pain score during SCT was dichotomized as “responder” (the VAS pain score improved by ≥30% from baseline to post-treatment35) and “non-responder.” Between-group comparisons were performed using log binomial regression and presented as relative risks.
Post-hoc correlation analysis was performed to address the relationship between the pain relief and therapeutic effects of TENS on SCT time stratified by group (sham-TENS and TENS). In this analysis, the Pearson correlation coefficients between the change in VAS pain score and 11-SCT time were evaluated in each group. The interaction effect of group × change in VAS pain score on change in 11-SCT time was also evaluated. Data analyses were performed using JMP Pro 13.0 (SAS Institute, Cary, NC, USA). Statistical significance was determined with p < 0.05.
Data availability
The datasets generated and/or analyzed in the present study are available from the corresponding author on reasonable request.
References
Guccione, A. A. et al. The effects of specific medical conditions on the functional limitations of elders in the Framingham Study. Am. J. public. health 84, 351–358 (1994).
Peat, G., McCarney, R. & Croft, P. Knee pain and osteoarthritis in older adults: a review of community burden and current use of primary health care. Ann. Rheum. Dis. 60, 91–97 (2001).
Andriacchi, T. P., Andersson, G. B., Fermier, R. W., Stern, D. & Galante, J. O. A study of lower-limb mechanics during stair-climbing. J. bone Jt. surgery. Am. volume 62, 749–757 (1980).
Nadeau, S., McFadyen, B. J. & Malouin, F. Frontal and sagittal plane analyses of the stair climbing task in healthy adults aged over 40 years: what are the challenges compared to level walking? Clin. Biomech. 18, 950–959 (2003).
Hensor, E. M., Dube, B., Kingsbury, S. R., Tennant, A. & Conaghan, P. G. Toward a clinical definition of early osteoarthritis: onset of patient-reported knee pain begins on stairs. Data from the osteoarthritis initiative. Arthritis care Res. 67, 40–47, https://doi.org/10.1002/acr.22418 (2015).
Iijima, H., Shimoura, K., Aoyama, T. & Takahashi, M. Biomechanical characteristics of stair ambulation in patients with knee OA: A systematic review with meta-analysis toward a better definition of clinical hallmarks. Gait posture 62, 191–201, https://doi.org/10.1016/j.gaitpost.2018.03.002 (2018).
Valtonen, A. M., Poyhonen, T., Manninen, M., Heinonen, A. & Sipila, S. Knee extensor and flexor muscle power explains stair ascension time in patients with unilateral late-stage knee osteoarthritis: a cross-sectional study. Arch. Phys. Med. Rehabil. 96, 253–259, https://doi.org/10.1016/j.apmr.2014.09.011 (2015).
Shrader, M. W., Draganich, L. F., Pottenger, L. A. & Piotrowski, G. A. Effects of knee pain relief in osteoarthritis on gait and stair-stepping. Clinical orthopaedics and related research, 188–193 (2004).
Bruce-Brand, R. A. et al. Effects of home-based resistance training and neuromuscular electrical stimulation in knee osteoarthritis: a randomized controlled trial. BMC Musculoskelet. Disord. 13, 118, https://doi.org/10.1186/1471-2474-13-118 (2012).
Chen, L. X. et al. Transcutaneous Electrical Nerve Stimulation in Patients With Knee Osteoarthritis: Evidence From Randomized-controlled Trials. Clin. J. Pain. 32, 146–154, https://doi.org/10.1097/AJP.0000000000000233 (2016).
Hopkins, J., Ingersoll, C. D., Edwards, J. & Klootwyk, T. E. Cryotherapy and Transcutaneous Electric Neuromuscular Stimulation Decrease Arthrogenic Muscle Inhibition of the Vastus Medialis After Knee Joint Effusion. J. Athl. Train. 37, 25–31 (2002).
Cheing, G. L. & Hui-Chan, C. W. Would the addition of TENS to exercise training produce better physical performance outcomes in people with knee osteoarthritis than either intervention alone? Clin. rehabilitation 18, 487–497, https://doi.org/10.1191/0269215504cr760oa (2004).
Pietrosimone, B. G., Hart, J. M., Saliba, S. A., Hertel, J. & Ingersoll, C. D. Immediate effects of transcutaneous electrical nerve stimulation and focal knee joint cooling on quadriceps activation. Med. Sci. Sports Exerc. 41, 1175–1181, https://doi.org/10.1249/MSS.0b013e3181982557 (2009).
Cherian, J. J. et al. Knee Osteoarthritis: Does Transcutaneous Electrical Nerve Stimulation Work? Orthopedics 39, e180–186, https://doi.org/10.3928/01477447-20151222-02 (2016).
Bruyere, O. et al. Can we identify patients with high risk of osteoarthritis progression who will respond to treatment? A focus on epidemiology and phenotype of osteoarthritis. Drugs Aging 32, 179–187, https://doi.org/10.1007/s40266-015-0243-3 (2015).
Qi, L. et al. Comparing the Effectiveness of Electroacupuncture with Different Grades of Knee Osteoarthritis: A Prospective Study. Cell Physiol. Biochem. 39, 2331–2340, https://doi.org/10.1159/000447925 (2016).
Riener, R., Rabuffetti, M. & Frigo, C. Stair ascent and descent at different inclinations. Gait Posture 15, 32–44, https://doi.org/10.1016/s0966-6362(01)00162-x (2002).
Iijima, H., Shimoura, K., Eguchi, R., Aoyama, T. & Takahashi, M. Concurrent validity and measurement error of stair climb test in people with pre-radiographic to mild knee osteoarthritis. Gait Posture 68, 335–339, https://doi.org/10.1016/j.gaitpost.2018.12.014 (2019).
Varbakken, K., Loras, H., Nilsson, K. G., Engdal, M. & Stensdotter, A. K. Relative difference among 27 functional measures in patients with knee osteoarthritis: an exploratory cross-sectional case-control study. BMC Musculoskelet. Disord. 20, 462, https://doi.org/10.1186/s12891-019-2845-0 (2019).
Taylor, M. J., Dabnichki, P. & Strike, S. C. A three-dimensional biomechanical comparison between turning strategies during the stance phase of walking. Hum. Mov. Sci. 24, 558–573, https://doi.org/10.1016/j.humov.2005.07.005 (2005).
Johnson, M. Transcutaneous Electrical Nerve Stimulation: Mechanisms, Clinical Application and Evidence. Rev. Pain. 1, 7–11, https://doi.org/10.1177/204946370700100103 (2007).
Shimoura, K., Iijima, H., Suzuki, Y. & Aoyama, T. Immediate Effects of Transcutaneous Electrical Nerve Stimulation on Pain and Physical Performance in Individuals With Preradiographic Knee Osteoarthritis: A Randomized Controlled Trial. Arch. Phys. Med. rehabilitation 100(300-306), e301, https://doi.org/10.1016/j.apmr.2018.08.189 (2019).
Han, J. & Wang, Q. Mobilization of specific neuropeptides by peripheral stimulation of identified frequencies. Physiology 7, 176–180 (1992).
Rutjes, A. W. et al. Transcutaneous electrostimulation for osteoarthritis of the knee. Cochrane Database Syst Rev, Cd002823, https://doi.org/10.1002/14651858.CD002823.pub2 (2009).
Robbins, S. & Waked, E. Balance and vertical impact in sports: role of shoe sole materials. Arch. Phys. Med. Rehabil. 78, 463–467 (1997).
Arnadottir, S. A. & Mercer, V. S. Effects of footwear on measurements of balance and gait in women between the ages of 65 and 93 years. Phys. Ther. 80, 17–27 (2000).
Eguchi, R., Yorozu, A. & Takahashi, M. in Control Conference (ASCC), 2017 11th Asian. 2861-2865 (IEEE).
International, O. R. S. Physical Performance Measures. OARSI recommended set of physical performance measures for knee and hip osteoarthritis, https://www.oarsi.org/research/physical-performance-measures (2014, October 3).
Dobson, F. et al. Reliability and measurement error of the Osteoarthritis Research Society International (OARSI) recommended performance-based tests of physical function in people with hip and knee osteoarthritis. Osteoarthr. Cartil. 25, 1792–1796, https://doi.org/10.1016/j.joca.2017.06.006 (2017).
Almeida, G. J., Schroeder, C. A., Gil, A. B., Fitzgerald, G. K. & Piva, S. R. Interrater reliability and validity of the stair ascend/descend test in subjects with total knee arthroplasty. Arch. Phys. Med. Rehabil. 91, 932–938, https://doi.org/10.1016/j.apmr.2010.02.003 (2010).
Dobson, F. et al. OARSI recommended performance-based tests to assess physical function in people diagnosed with hip or knee osteoarthritis. Osteoarthr. Cartil. 21, 1042–1052, https://doi.org/10.1016/j.joca.2013.05.002 (2013).
Wang, C. Y., Olson, S. L. & Protas, E. J. Test-retest strength reliability: hand-held dynamometry in community-dwelling elderly fallers. Arch. Phys. Med. Rehabil. 83, 811–815 (2002).
Akai, M. et al. An outcome measure for Japanese people with knee osteoarthritis. J. Rheumatol. 32, 1524–1532 (2005).
Iijima, H. et al. Coexisting lateral tibiofemoral osteoarthritis is associated with worse knee pain in patients with mild medial osteoarthritis. Osteoarthr. Cartil. 25, 1274–1281, https://doi.org/10.1016/j.joca.2017.02.801 (2017).
Dworkin, R. H. et al. Interpreting the clinical importance of treatment outcomes in chronic pain clinical trials: IMMPACT recommendations. J. pain: Off. J. Am. Pain. Soc. 9, 105–121, https://doi.org/10.1016/j.jpain.2007.09.005 (2008).
Acknowledgements
The authors thank the members of Aoyama Laboratory (Kyoto University, Kyoto) for their assistance with the data collection. The authors thank Editage (www.editage.jp) for the English language editing. This study was supported in part by (1) a funding from Omron Healthcare Co., Ltd., and (2) a grant-in-aid from the Japan Society for the Promotion of Science (https://www.jsps.go.jp/) for Research Fellows to HI.
Author information
Authors and Affiliations
Contributions
All authors made substantial contributions to (1) the study conception and design, data acquisition, or data analysis and interpretation; (2) drafting the article or revising it critically for important intellectual content; and (3) providing final approval of the manuscript for submission. All authors agreed both to be personally accountable for their own contributions and to ensure that questions related to the accuracy or integrity of any part of the work, even those in which they were not personally involved, are appropriately investigated and resolved, with the resolution documented in the literature. The specific contributions of the authors were as follows: (1) Study conception and design: H.I., K.S. and K.Y.; (2) Data analysis and interpretation: H.I., R.E., K.S., T.A. and M.T.; (3) Article drafting: H.I., R.E., K.S., T.A. and M.T.; (4) Critical revision of the article for important intellectual content: H.I., K.S., K.Y. and T.A.; (5) Final approval of the article: H.I., R.E., K.S., K.Y., T.A. and M.T.; (6) Statistical expertise: H.I.; (7) Obtaining funding: H.I.; and (8) Data collection and assembly: H.I., R.E., K.S., K.Y., T.A. and M.T.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Iijima, H., Eguchi, R., Shimoura, K. et al. Transcutaneous Electrical Nerve Stimulation Improves Stair Climbing Capacity in People with Knee Osteoarthritis. Sci Rep 10, 7294 (2020). https://doi.org/10.1038/s41598-020-64176-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-64176-0
This article is cited by
-
A comparison of different physical stimulation combined with platelet-rich plasma for the treatment of knee osteoarthritis: study protocol for a randomized controlled trial
Trials (2023)
-
The effects of low-level laser therapy on muscle strength and functional outcomes in individuals with knee osteoarthritis: a double-blinded randomized controlled trial
Scientific Reports (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.