Abstract
To determine the causality of micro-nutrients concentrations and risk of ovarian cancer using the Mendelian randomization approach. Analyses were conducted using summary statistics data for SNPs robustly associated with concentrations of thirteen micro-nutrients (iron, copper, zinc, calcium, magnesium, phosphorus, selenium, vitamin A, β-carotene, vitamin B6, vitamin B12, vitamin E, folate). The corresponding data for ovarian cancer were obtained from the Ovarian Cancer Association Consortium (25,509 cases and 40,941 controls). In standard Mendelian randomization analysis, the odds ratios (OR) of invasive epithelial ovarian cancer were 0.14 (95% CI, 0.03–0.70; P = 0.02) per 0.1 mmol/L (about one standard deviation, SD) increase in genetically predicted magnesium concentration, 1.04 (95% CI, 1.00–1.09; P = 0.03) per 0.3 μmol/liter (about one SD) increase in genetically predicted β-carotene concentration. The OR of low malignant potential tumours were 0.82 (95% CI, 0.76–0.90; P = 1.01 × 10−5) per 0.3 μmol/liter (about one SD) increase in β-carotene concentration, 1.42 (95% CI, 1.21–1.68; P = 3 × 10−5) per 153 pmol/L (about one SD) increase in vitamin B12 concentration, 0.21 (95% CI, 0.06–0.76; P = 0.02) per 6 mg/L (about one SD) increase in vitamin E concentration. No significant associations of other micro-nutrients and ovarian cancer were observed. This study found that an increased risk of invasive epithelial ovarian cancer was observed with a genetically higher concentration of β-carotene, whereas a decreased risk of invasive epithelial ovarian cancer was found with a higher concentration of magnesium. As for low malignant potential tumours, increased concentration of vitamin B12 could increase the risk of low malignant potential tumours, while increased concentrations of β-carotene and vitamin E could lower the risk of low malignant potential tumours.
Similar content being viewed by others
Introduction
Globally, around 300,000 new cases and 185,000 deaths occur each year, making ovarian cancer the eighth most common cause of death in female cancer, and the second most common cause of death in gynecological cancer (after cervical cancer)1. The prognosis of ovarian cancer is generally poor, with a 5-year survival rate of only 48% after diagnosis. In contrast, the 5-year survival rate of breast cancer is 90%2. Despite advances in modern medicine, the survival rate of ovarian cancer has changed little over the decades, even in the resource-rich countries such as the United States and Canada2,3. These frustrating figures are in part due to the lack of effective screening tests for early detection of ovarian cancer and the lack of early, specific symptoms that result in diagnostic delays2. Given the limited success of secondary prevention strategies and high cure rate of early-stage disease, at present, the best opportunity for disease control and even cure might be at primary prevention. Stratified analyses across clinically distinct histotypes are necessary for prevention and treatment of ovarian cancer. Ovarian epithelial tumours can be classified according to the following histological subtypes: serous, mucinous, endometrioid, clear cell, transitional cell, Brenner, small cell, mixed mesodermal and undifferentiated. Usually each subtype can be classified as benign, borderline (low malignant potential, LMP) and malignant (invasive), in which the prognosis of invasive epithelial ovarian cancer is generally poorer4.
Micronutrients include vitamins and minerals required in very small quantities in our bodies. They’re critical for a number of important functions, including growth, development and disease prevention5. However, the role of nutrients in the development of ovarian cancer remains unclear. Firstly because the literature on the circulating concentrations of minerals and vitamins with risk of ovarian cancer is generally limited, except vitamin D6,7. Previous research of the cellular mechanism of vitamin D in ovarian cancer suggested that vitamin D played a critical role in antitumorigenic activities by regulating cellular proliferation and metabolism through genomic and nongenomic signal transduction pathways6. However, the role of other micronutrients in ovarian cancer and underlying mechanisms need to be unraveled. Besides, there has been little agreement in the published literature on the role of micro-nutrients in ovarian cancer. For instance, the California Teachers Study prospective cohort study showed that higher intake of β-carotene was associated with a 41% higher risk for ovarian cancer8, but another population-based case-control retrospective study suggested that the serum concentration of β-carotene was inversely correlated with the risk of ovarian cancer9. Furthermore, given the observational design of most available studies on micro-nutrients and ovarian cancer risk, it is uncertain whether the observed associations are causal and independent of other confounding factors.
Mendelian randomization (MR) is a genetic epidemiological approach that exploits germline genetic variants as unbiased proxies for exposure of interest to infer causality10,11,12. Since germline genetic variants are randomly assorted at meiosis, MR analyses should be less likely to be confounded by environmental factors than conventional observational studies. Additionally, since at the time of conception, germline genetic variants are set and cannot be changed by subsequent processes of disease, MR analyzes are not influenced by reverse causality bias. Another benefit of MR is that it can be applied using summary genetic association data from two independent samples (known as the 2-sample MR approach) representing (1) associations of genetic variant-risk factor and (2) associations of genetic variant-outcome. This approach provides an effective and statistically robust method for assessing the causal relationships between risk factors and outcomes. However, to our knowledge, the effects of micronutrient in ovarian cancer have not been evaluated on a large scale with the use of MR.
The aim of our study is to investigate whether micro-nutrients concentrations are causally associated with epithelial ovarian cancer as a whole or any of its histotypes by applying the 2-sample MR approach.
Results
For each risk factor, the number of SNPs included in the genetic instruments was provided in Table 1. Complete Mendelian randomization analyses were presented in Tables S1 and S2 for invasive epithelial ovarian cancer histotypes and low malignant potential tumours. Scatter plots for findings showing strong or suggestive evidence of association in standard IVW analyses were presented in S1 Plots. Leave-one-out plots were presented in S2 Plots.
Causality between minerals and epithelial ovarian cancer
In analyses examining invasive epithelial ovarian cancer and low malignant potential tumours, magnesium was the only mineral that was negatively correlated with invasive epithelial ovarian cancer in the standard IVW analysis, with an OR of 0.14 (95%CI, 0.03–0.70; P = 0.02) (Fig. 1). The correlation was in line with complementary analyses using weighted median method (OR, 0.19; 95% CI, 0.02–1.67) and MR-RAPS (OR, 0.12; 95% CI, 0.02–0.73) (Table S1). No outlier was detected using MR-PRESSO. No indication of directional pleiotropy was found in the MR-Egger analysis (P for MR-Egger intercept = 0.26).
In analyses examining ovarian cancer histotypes, calcium and phosphorus were positively correlated with mucinous borderline tumours and high grade serous carcinoma, respectively. The standard IVW estimate showed that the OR of mucinous borderline tumours per SD (0.5 mg/dL) increase in calcium concentration was 3.29 (95% CI, 1.14–9.53; P = 0.03). Similar trends were shown when employing weighted median estimators (OR, 2.71; 95% CI, 0.58–12.71) and MR-RAPS (OR, 3.20; 95% CI, 0.80–12.79), though without significance. No outlier and directional pleiotropy were detected (P for MR-Egger intercept = 0.96) (Table S1). The IVW estimate showed that the OR of high grade serous carcinoma per SD (0.5 mg/dL) increase in phosphorus concentration was 1.40 (95% CI, 1.05–1.85; P = 0.02). The corresponding OR was 1.40 (95% CI, 0.81–2.41) in the analysis based on the weighted median method. No outlier and directional pleiotropy were found (P for MR-Egger intercept = 0.99) (Table S1).
Causality between vitamins and epithelial ovarian cancer
Among six vitamins, β-carotene was significantly associated with risk of invasive epithelial ovarian cancer (including histotypes) and low malignant potential tumours. Genetically predicted serum β-carotene levels were positively associated with invasive epithelial ovarian cancer (OR, 1.04; 95% CI, 1.00–1.09; P = 0.03) (Fig. 1), mucinous carcinoma (OR, 1.21; 95% CI, 1.07–1.37; P = 0.003), and endometrioid carcinoma (OR, 1.10; 95% CI, 1.05–1.15; P = 4.02 × 10−5) in standard IVW analysis. In contrast, β-carotene was negatively correlated with low grade serous carcinoma (OR, 0.76; 95% CI, 0.67–0.86; P = 1.85 × 10−5), low malignant potential tumours (OR, 0.82; 95% CI, 0.76–0.90; P = 1.01 × 10−5)(Fig. 1) and mucinous borderline tumours (OR, 0.57; 95% CI, 0.53–0.61; P = 3.89 × 10−53). No outlier and directional pleiotropy were detected (Table S2).
In analyses performed for invasive epithelial ovarian cancer and low malignant potential tumours, genetically predicted vitamin E levels were inversely associated with low malignant potential tumours in the standard IVW analysis, with an OR of 0.21 (95% CI, 0.06–0.76; P = 0.02) per 1 SD (6.0 mg/L) increase of serum vitamin E levels (Fig. 1). Genetically predicted vitamin B12 concentration was not significantly associated with low malignant potential tumours in the IVW method (OR, 1.16; 95% CI, 0.96–1.41; P = 0.12) until the MR-PRESSO test detected one outlier (rs12272669). After adjustment for the outlier, there was a suggestive positive association between vitamin B12 and low malignant potential tumours by using the IVW analysis (OR, 1.42; 95% CI, 1.21–1.68; P = 3 × 10−5), the weighted median analysis (OR, 1.33; 95% CI, 1.05–1.69; P = 0.02), the MR-Egger regression (OR, 1.57; 95% CI, 1.08–2.28; P = 0.04), and MR-RAPS (OR, 1.41; 95% CI, 1.17–1.70; P = 3 × 10−4) (Fig. 1, Table S2). There was no indication of directional pleiotropy (P for MR-Egger intercept = 0.57).
In analyses performed for ovarian cancer histotypes, a negative association was observed between genetically determined vitamin B6 concentrations and clear cell carcinoma based on the MR-RAPS approach (OR, 0.91; 95% CI, 0.85–0.97; P = 0.005). Genetically predicted vitamin E levels were inversely associated with serous borderline tumours in the standard IVW analysis (OR, 0.12; 95% CI, 0.02–0.56; P = 0.01), and in the weighted median analysis (OR, 0.12; 95% CI, 0.01–1.06). There was no evidence of directional pleiotropy (P for MR-Egger intercept = 0.45) (Table S2).
Discussion
In this comprehensive Mendelian randomization analysis of thirteen nutrients concentrations with risk of epithelial ovarian cancer, an increased risk of invasive epithelial ovarian cancer was related to a higher concentration of β-carotene, while a decreased risk of invasive epithelial ovarian cancer was related to a higher concentration of magnesium. As for the risk of low malignant potential tumours, it had a positive correlation with the concentration of vitamin B12, and negative correlations with β-carotene and vitamin E. When stratified on histotypes, most risk factors (calcium, phosphorus and vitamin B6) were associated with one or more subtypes, underscoring the heterogeneous nature of this disease.
There is a paucity of literature on the association of circulating magnesium and the risk of epithelial ovarian cancer. Only one case-control study in Taiwan13, involving 933 ovarian cancer deaths and 933 deaths from other causes, from 1986 to 2000, reported on the possible association between the risk of ovarian cancer and the levels of magnesium and calcium in drinking water. This study reported that there was a significant protective effect of magnesium intake from water on the risk of ovarian cancer, supporting our findings. A randomized intervention trial showed that the average serum magnesium concentration increased from 0.84 mmol/L to 0.87 mmol/L after 12 weeks supplementation with 350 mg magnesium daily14, and the increase of serum magnesium corresponds to about 0.3 SD in our MR study. Low magnesium promoted inflammation which induced genetic instability and might cause mutation in synergy with low magnesium, thus allowing the generation of highly aggressive cells15. Inflammation was very intense, and Tumour Necrosis Factor α (TNFα) was increased in the serum of magnesium-deficient mice15. TNFα, the target of NF-κB and prototypical pro-inflammatory cytokine, could enhance tumour invasion by facilitating the epithelial to mesenchymal transition, then augment the capacity of cancer cells to metastatize16. Further, magnesium was an absolute requirement for the function of NM23-H1, a metastasis-suppressor gene. Metastasis was accelerated in NM23-H1 knockout mice17. Therefore, low magnesium availability impaired the anti-metastatic activity of NM23-H1 in mice. Additionally, senescence of endothelial and fibroblast cells was promoted by low magnesium18, and senescent cells could change the tissue environment in a way that synergistically potentiated tumour growth and development with carcinogenic mutations19.
The role of β-carotene in ovarian cancer development is unclear. Our result showed that higher concentration of β-carotene could reduce the risk of low malignant potential tumours, which was in line with a population-based study of 549 cases of ovarian cancer and 516 controls, demonstrating that intakes of carotene from food and supplements were significantly and inversely correlated with risk of ovarian cancer, predominantly among postmenopausal women9. This result can readily be understood for the supportive function of β-carotene, such as antioxidation, inhibition of tumour initiation and promotion, and enhancement of immunity and cellular maturation20. Data from a randomized controlled trial indicated that the average serum concentration of β-carotene increased from 0.47 μmol/liter to 1.14 μmol/liter with 3 mg daily oral supplement of β-carotene for one month21, and the increase of serum β-carotene corresponds to about 2 SD in our MR study. However, an increased risk of invasive epithelial ovarian cancer was also observed for genetically higher concentrations of β-carotene in our study. In accordance with this result, the California Teachers’ Study has demonstrated that higher intake of β-carotene was associated with a 41% higher risk for ovarian cancer8. Abhishek Goyal22 et al. evaluated all-cause, cancer and cardiovascular mortality risks associated with quintiles (Q1-Q5) of serum antioxidants, including β-carotene, in 16,008 adult NHANES III (The Third National Health and Nutrition Examination Survey, 1988–1994) participants. The results of this study indicated that cancer mortality risks decreased from Q1-Q2 of β-carotene and did not change significantly with higher levels of β-carotene. Clinical trials of vitamin supplementation with cancer incidence and mortality as outcomes suggested that 12 years of supplementation with β-carotene produced neither benefit nor harm to the incidence of malignant tumours23. These results (i.e., the different roles of β-carotene in different histotypes of ovarian cancer) may appear confusing. First, the reliability of results needs to be checked. The reliability of MR results relies on the MR assumptions and pleiotropy occurs when a genetic variant is associated with more than one phenotype. As β-carotene needs to be consumed (i.e., they are not synthesised endogenously), it is possible that genetic variants may influence β-carotene levels indirectly through altered dietary preferences, like vegetables and fruit consumption. In order to minimize the confounding effect of any dietary preferences, we examined the associated phenotype of each genetic instruments, and no correlation between dietary preferences and genetic variants was found24,25. Second, the tissue and cell specific effects of circulating β-carotene cannot be ruled out, as well as the unknown difference in genetic or epigenetic alterations between these two histotypes. Therefore, As the first to explore the correlation of β-carotene and risk of ovarian cancer histotypes, our study indicated that further studies, taking cancer histotypes into account, will need to be undertaken.
In analyses examining the correlation between the concentration of vitamin B12 and risk of low malignant potential tumours, one outlier (rs12272669) was detected by MR-PRESSO and leave-one-out analyses (S2 plots). A strong positive correlation between vitamin B12 and low malignant potential tumours was observed after the exclusion of rs12272669 (OR, 1.42; 95% CI, 1.21–1.68; P = 2 × 10−5). Rs12272669, located in the MMACHC gene, was involved in binding and intracellular trafficking of vitamin B1226. The effect allele frequency of rs12272669 was 0.22%, which might give rise to the unstable effects on analysis. To date, epidemiological studies have largely failed to provide evidence to support the association of vitamin B12 with risk of ovarian cancer27. However, our finding reported here shed new light on the positive correlation of vitamin B12 and risk of low malignant potential tumours. The precise mechanism of vitamin B12 in ovarian cancer remains to be elucidated.
A randomized intervention study showed that the supplementation of 200 mg/d vitamin E for one month increased the serum vitamin E level from 25.6 μmol/L to 49 μmol/L, which corresponds to about 1.7 SD in our MR study28. In our study, a higher concentration of vitamin E was observed to reduce risk of low malignant potential tumours. However, the observed correlation between vitamin E and invasive epithelial ovarian cancer in this study was not significant. Prior studies that have noted the importance of vitamin E in preventing cancer: various cancer-promoting pathways such as COX and 5-LOX-catalyzed eicosanoids could be blocked, key transcription factors such as NF-κB and STAT3 could be inhibited, and cancer cell death could be induced by vitamin E via modulating various signaling pathways, including sphingolipid metabolism29. Moreover, those natural forms of vitamin E that were easy to metabolize had stronger anti-inflammatory effects than some unmetabolized vitamers30,31,32. A previous study revealed that vitamin E could reduce cancer cell growth by suppressing telomerase activity in ovarian cancer cells33. This result also accorded with another study showing that the intake of vitamin E was inversely associated with ovarian cancer (OR = 0.6; 95%CI, 0.5–0.8)34. Future more preclinical studies are therefore recommended to validate the efficacy of vitamin E for ovarian cancer prevention.
Strengths of this analysis include the use of a comprehensive collection of micro-nutrients GWASs, the large number of cases of ovarian cancer, the appraisal of the role of these micro-nutrients in various ovarian cancer subtypes, the unlikely weak instrument bias (i.e., F-statistics for respective genetic instruments across the 13 micronutrients ranged from 18 to 344), the employment of Mendelian randomization approach to minimize confounding and avoid reverse causation bias, and the usage of complementary analyses to provide additional evidence regarding the causal relationship.
There are several limitations to our analyses. First, the statistical power was not high enough in the analysis of some kinds of micro-nutrients; specifically, the SNPs of folate only explained a small portion of the variance (1%) in serum folate levels. Hence, we cannot rule out the possibility of overlooking weak associations between genetically predicted serum folate concentrations and ovarian cancer subtypes, and the same is true for other nutrients. In this case, larger GWASs of micro-nutrients are required for the construction of better genetic instruments. Second, we performed several statistical tests to explore the potential violation of MR assumptions. Despite the lack of indication of directional pleiotropy in the results with significance, we cannot robustly exclude the associations from being mediated through other causal pathways due to some underpowered statistical tests when a small number of genetic instruments were used (for example, MR-Egger). Third, due to the genetic studies largely limited in European ancestry, it might restrict the finding’s generalisability in other ancestral groups. Fourth, we should draw conclusions based on effect estimates and their CIs, rather than only based on statistical tests using a P value cut-off35,36. Given some point estimates with wider CIs, the effects of some micro-nutrients were not so precisely estimated, for example, the effect of magnesium on invasive epithelial ovarian (95% CI, 0.03–0.70) and the effect of vitamin E on low malignant potential tumours (95% CI, 0.06–0.76). Also, the point estimate of effect of β-carotene on invasive epithelial ovarian with the CI including the null (95% CI, 1.00–1.09) should be treated with more caution as well. Fifth, all models employed assumed linear relationships between micro-nutrients and ovarian cancer. Future studies focusing on nonlinear relationships of the concentration of micro-nutrients and the risk of epithelial ovarian cancer are warranted to elucidate potential underlying pathways. In spite of its limitations, our study certainly offers some insights into the correlation between micro-nutrients and ovarian cancer.
Conclusion
In conclusion, we conducted the first comprehensive two-sample MR study to investigate whether the concentrations of thirteen micro-nutrients were related to the risk of epithelial ovarian cancer. An increased risk of invasive epithelial ovarian cancer was observed with a genetically higher concentration of β-carotene, whereas a decreased risk of invasive epithelial ovarian cancer was found with a higher concentration of magnesium. As for low malignant potential tumours, increased concentration of vitamin B12 could increase the risk of low malignant potential tumours, while increased concentrations of β-carotene and vitamin E could lower the risk of low malignant potential tumours.
Methods
Study design
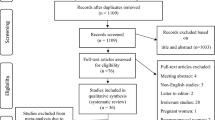
A Mendelian randomization study that examined whether single nucleotide polymorphisms (SNPs) associated with concentrations of micro-nutrients are causally linked to the risk of ovarian cancer. The unbiased causal relationship between exposures and disease outcomes can be estimated by using genetic instruments for exposures if the following assumptions are fulfilled: (1) the genetic instruments (one or more independent SNPs) are robustly related to the exposures concerned; (2) the genetic instruments are not associated with any possible confounding variables; (3) the genetic instruments influence outcomes only through the exposures (Fig. 2).
Ovarian cancer population
Genotype data were obtained from the Illumina Custom Infinium array (OncoArray) project, a part of the Ovarian Cancer Association Consortium (OCAC) genome-wide association study (GWAS). There were 25,509 epithelial ovarian cancer (EOC) cases and 40,941 controls of European ancestry included in the summary genetic association data37. The OCAC OncoArray data comprised 63 genotyping project/case-control sets. From seven genotyping projects, 66,450 samples passed quality control. Analyses were performed for 40,941 controls, 22,406 invasive epithelial ovarian cancer cases, and 3,103 low malignant potential tumours cases. The invasive cases (n = 22,406) involved the following histotypes: high grade serous carcinoma (n = 13,037), low grade serous carcinoma (n = 1,012), mucinous carcinoma (n = 1,417), endometrioid carcinoma (n = 2,810), clear cell carcinoma (n = 1,366), and others (n = 2,764). The low malignant potential tumours (n = 3,103) included serous borderline tumours (n = 1,954) and mucinous borderline tumours (n = 1,149).
Micro-nutrients GWAS sources
Published GWAS on micro-nutrients, including minerals and vitamins, were searched by using Genome-Wide Association Studies (GWAS) catalog (https://www.ebi.ac.uk/gwas) and Pubmed (https://www.ncbi.nlm.nih.gov/pubmed). Vitamin D was excluded because the role of vitamin D in ovarian cancer has been investigated by MR studies38,39. Vitamins B1, B2, B3, B5, B7, C, sulfur, iodine, chloride and fluoride were excluded because no genome-wide association studies have been conducted. Vitamin K, potassium, sodium, cobalt, chromium and molybdenum were also excluded for no genome-wide significant results40,41,42. In total, thirteen micro-nutrients with suitable genetic instruments were included in the analysis: calcium, magnesium, iron, copper, zinc, phosphorus, selenium, β-carotene, vitamin A, B6, B12, E and folate26,40,43,44,45,46,47,48,49,50,51.
Genetic instrument selection
After obtaining effect estimates from relevant GWASs, SNPs were pruned for linkage disequilibrium at r2 < 0.1 from the lead SNP at a genome-wide significance level (P < 5 × 10−8). Then, the corresponding effect estimates and standard errors of the remaining independent SNPs were obtained from the ovarian cancer dataset. When an SNP was not available in the ovarian cancer dataset, the presence of a “proxy” SNP in linkage disequilibrium with this SNP at r2 > 0.8 was assessed using the Phase 3 (Version 5) of the 1000 Genomes Project sample data (identified using online tool SNiPa, available at http://snipa.helmholtz-muenchen.de/snipa3/). If such “proxy” SNP was not available in the ovarian cancer dataset, this SNP was excluded from the analysis.
Statistical analyses
Estimates of the proportion of variance in each micro-nutrient explained by the genetic instruments (R2) and the strength of the association between the genetic instruments and micro-nutrients (F-statistics) were generated using methods previously described52. Inverse-variance-weighted (IVW) fixed effects models were used to generate effect estimates for micro-nutrients with 2 or 3 SNPs as instruments. IVW multiplicative random effects models were used if the number of SNPs was greater than 353. Complementary analyses using the weighted median, MR-Egger regression, MR-robust adjusted profile score (MR-RAPS, an MR method for correcting for horizontal pleiotropy using robust adjusted profile scores54) and MR-Pleiotropy Residual Sum and Outlier (MR-PRESSO, an MR method for correcting pleiotropy residual sum and outlier)55. Directional pleiotropy statistics were conducted using MR-Egger, and the intercept term can provide a formal statistical test for pleiotropy. Additionally, whether the results were driven by individual influential SNPs was examined by using leave-one-out permutation analyses. MR analyses were conducted using the TwoSampleMR R packages56. A two-sided p-value of <0.05 was set as the threshold for significance. To avoid inference based simply on P-value thresholds, the direction and strength of effect for each association, together with the corresponding P-value, were presented35,36. All analyses were conducted in R version 3.6.1.
Ethics approval and informed consent
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional committee and with the 1964 Helsinki declaration. The protocol of OCAC was approved by each of the Ethics Committees of the participating institutions. The specific study reported here was approved by the Zhejiang University Ethics Committee. Written informed consent was obtained from all individual participants included in the study. All the methods were carried out in accordance with the approved guidelines.
Data availability
The datasets analyzed in this study are publicly available summary statistics.
References
Bray, F. et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 68, 394–424, https://doi.org/10.3322/caac.21492 (2018).
Noone, A. et al. SEER cancer statistics review, 1975–2015. Bethesda, MD: National Cancer Institute (2018).
Committee, C. C. S. A. Canadian Cancer Statistics 2019, <cancer.ca/Canadian-Cancer-Statistics-2019-EN> (2019).
Lee-Jones, L. Ovary: epithelial tumors. Atlas of Genetics and Cytogenetics in Oncology and Haematology (2004).
Shenkin, A. The key role of micronutrients. Clinical Nutrition 25, 1–13, https://doi.org/10.1016/j.clnu.2005.11.006 (2006).
Guo, H., Guo, J., Xie, W., Yuan, L. & Sheng, X. The role of vitamin D in ovarian cancer: epidemiology, molecular mechanism and prevention. J Ovarian Res 11, 71, https://doi.org/10.1186/s13048-018-0443-7 (2018).
Granato, T. et al. Low 25-OH vitamin D levels at time of diagnosis and recurrence of ovarian cancer. Tumour Biol 37, 2177–2181, https://doi.org/10.1007/s13277-015-4055-1 (2016).
Chang, E. T. et al. Diet and risk of ovarian cancer in the California Teachers Study cohort. Am J Epidemiol 165, 802–813, https://doi.org/10.1093/aje/kwk065 (2007).
Cramer, D. W., Kuper, H., Harlow, B. L. & Titus-Ernstoff, L. Carotenoids, antioxidants and ovarian cancer risk in pre- and postmenopausal women. Int J Cancer 94, 128–134, https://doi.org/10.1002/ijc.1435 (2001).
Smith, G. D. & Ebrahim, S. ‘Mendelian randomization’: can genetic epidemiology contribute to understanding environmental determinants of disease? Int J Epidemiol 32, 1–22, https://doi.org/10.1093/ije/dyg070 (2003).
Lawlor, D. A., Harbord, R. M., Sterne, J. A. C., Timpson, N. & Davey Smith, G. Mendelian randomization: using genes as instruments for making causal inferences in epidemiology. Statistics in medicine 27, 1133–1163, https://doi.org/10.1002/sim.3034 (2008).
Burgess, S. & Thompson, S. G. Mendelian randomization: methods for using genetic variants in causal estimation. (Chapman and Hall/CRC, 2015).
Chiu, H. F., Chang, C. C. & Yang, C. Y. Magnesium and calcium in drinking water and risk of death from ovarian cancer. Magnes Res 17, 28–34 (2004).
Joris, P. J., Plat, J., Bakker, S. J. & Mensink, R. P. Long-term magnesium supplementation improves arterial stiffness in overweight and obese adults: results of a randomized, double-blind, placebo-controlled intervention trial. The American journal of clinical nutrition 103, 1260–1266, https://doi.org/10.3945/ajcn.116.131466 (2016).
Mazur, A. et al. Magnesium and the inflammatory response: potential physiopathological implications. Arch Biochem Biophys 458, 48–56, https://doi.org/10.1016/j.abb.2006.03.031 (2007).
Drutskaya, M. S., Efimov, G. A., Kruglov, A. A., Kuprash, D. V. & Nedospasov, S. A. Tumor necrosis factor, lymphotoxin and cancer. IUBMB Life 62, 283–289, https://doi.org/10.1002/iub.309 (2010).
Boissan, M. et al. Increased lung metastasis in transgenic NM23-Null/SV40 mice with hepatocellular carcinoma. J Natl Cancer Inst 97, 836–845, https://doi.org/10.1093/jnci/dji143 (2005).
Killilea, D. W. & Maier, J. A. A connection between magnesium deficiency and aging: new insights from cellular studies. Magnes Res 21, 77–82 (2008).
Campisi, J. Cancer and ageing: rival demons? Nat Rev Cancer 3, 339–349, https://doi.org/10.1038/nrc1073 (2003).
Albanes, D. β-Carotene and lung cancer: a case study. The American Journal of Clinical Nutrition 69, 1345S–1350S, https://doi.org/10.1093/ajcn/69.6.1345S (1999).
Sasaki, S. et al. Effects of three-month oral supplementation of beta-carotene and vitamin C on serum concentrations of carotenoids and vitamins in middle-aged subjects: a pilot study for a randomized controlled trial to prevent gastric cancer in high-risk Japanese population. Jpn J Cancer Res 91, 464–470, https://doi.org/10.1111/j.1349-7006.2000.tb00968.x (2000).
Goyal, A., Terry, M. B. & Siegel, A. B. Serum antioxidant nutrients, vitamin A, and mortality in USAdults. Cancer Epidemiol Biomarkers Prev 22, 2202–2211, https://doi.org/10.1158/1055-9965.Epi-13-0381 (2013).
Hennekens, C. H. et al. Lack of effect of long-term supplementation with beta carotene on the incidence of malignant neoplasms and cardiovascular disease. N Engl J Med 334, 1145–1149, https://doi.org/10.1056/nejm199605023341801 (1996).
Staley, J. R. et al. PhenoScanner: a database of human genotype-phenotype associations. Bioinformatics 32, 3207–3209, https://doi.org/10.1093/bioinformatics/btw373 (2016).
Kamat, M. A. et al. PhenoScanner V2: an expanded tool for searching human genotype-phenotype associations. Bioinformatics 35, 4851–4853, https://doi.org/10.1093/bioinformatics/btz469 (2019).
Grarup, N. et al. Genetic architecture of vitamin B12 and folate levels uncovered applying deeply sequenced large datasets. PLoS Genet 9, e1003530, https://doi.org/10.1371/journal.pgen.1003530 (2013).
Harris, H. R., Cramer, D. W., Vitonis, A. F., DePari, M. & Terry, K. L. Folate, vitamin B(6), vitamin B(12), methionine and alcohol intake in relation to ovarian cancer risk. Int J Cancer 131, E518–529, https://doi.org/10.1002/ijc.26455 (2012).
Meydani, S. N. et al. Vitamin E supplementation and in vivo immune response in healthy elderly subjects. A randomized controlled trial. JAMA 277, 1380–1386, https://doi.org/10.1001/jama.1997.03540410058031 (1997).
Jiang, Q. Natural forms of vitamin E: metabolism, antioxidant, and anti-inflammatory activities and their role in disease prevention and therapy. Free Radic Biol Med 72, 76–90, https://doi.org/10.1016/j.freeradbiomed.2014.03.035 (2014).
Jiang, Q. et al. Long-chain carboxychromanols, metabolites of vitamin E, are potent inhibitors of cyclooxygenases. Proc Natl Acad Sci USA 105, 20464–20469, https://doi.org/10.1073/pnas.0810962106 (2008).
Jiang, Z., Yin, X. & Jiang, Q. Natural forms of vitamin E and 13′-carboxychromanol, a long-chain vitamin E metabolite, inhibit leukotriene generation from stimulated neutrophils by blocking calcium influx and suppressing 5-lipoxygenase activity, respectively. J Immunol 186, 1173–1179, https://doi.org/10.4049/jimmunol.1002342 (2011).
Jang, Y., Park, N. Y., Rostgaard-Hansen, A. L., Huang, J. & Jiang, Q. Vitamin E metabolite 13′-carboxychromanols inhibit pro-inflammatory enzymes, induce apoptosis and autophagy in human cancer cells by modulating sphingolipids and suppress colon tumor development in mice. Free Radic Biol Med 95, 190–199, https://doi.org/10.1016/j.freeradbiomed.2016.03.018 (2016).
Bermudez, Y., Ahmadi, S., Lowell, N. E. & Kruk, P. A. Vitamin E suppresses telomerase activity in ovarian cancer cells. Cancer Detect Prev 31, 119–128, https://doi.org/10.1016/j.cdp.2006.12.002 (2007).
Bidoli, E. et al. Micronutrients and ovarian cancer: a case-control study in Italy. Ann Oncol 12, 1589–1593, https://doi.org/10.1023/a:1013124112542 (2001).
Sterne, J. A. & Davey Smith, G. Sifting the evidence-what’s wrong with significance tests? BMJ 322, 226–231, https://doi.org/10.1136/bmj.322.7280.226 (2001).
Wasserstein, R. L. & Lazar, N. A. The ASA statement on p-values: context, process, and purpose. The American Statistician 70 (2016).
Phelan, C. M. et al. Identification of 12 new susceptibility loci for different histotypes of epithelial ovarian cancer. Nat Genet 49, 680–691, https://doi.org/10.1038/ng.3826 (2017).
Ong, J. S. et al. Association of vitamin D levels and risk of ovarian cancer: a Mendelian randomization study. Int J Epidemiol 45, 1619–1630, https://doi.org/10.1093/ije/dyw207 (2016).
Ong, J. S. et al. Vitamin D and overall cancer risk and cancer mortality: a Mendelian randomization study. Hum Mol Genet 27, 4315–4322, https://doi.org/10.1093/hmg/ddy307 (2018).
Meyer, T. E. et al. Genome-wide association studies of serum magnesium, potassium, and sodium concentrations identify six Loci influencing serum magnesium levels. PLoS Genet 6, https://doi.org/10.1371/journal.pgen.1001045 (2010).
Dashti, H. S. et al. Meta-analysis of genome-wide association studies for circulating phylloquinone concentrations. Am J Clin Nutr 100, 1462–1469, https://doi.org/10.3945/ajcn.114.093146 (2014).
Ng, E. et al. Genome-wide association study of toxic metals and trace elements reveals novel associations. Hum Mol Genet 24, 4739–4745, https://doi.org/10.1093/hmg/ddv190 (2015).
Benyamin, B. et al. Novel loci affecting iron homeostasis and their effects in individuals at risk for hemochromatosis. Nat Commun 5, 4926, https://doi.org/10.1038/ncomms5926 (2014).
Evans, D. M. et al. Genome-wide association study identifies loci affecting blood copper, selenium and zinc. Hum Mol Genet 22, 3998–4006, https://doi.org/10.1093/hmg/ddt239 (2013).
O’Seaghdha, C. M. et al. Meta-analysis of genome-wide association studies identifies six new Loci for serum calcium concentrations. PLoS Genet 9, e1003796, https://doi.org/10.1371/journal.pgen.1003796 (2013).
Kestenbaum, B. et al. Common genetic variants associate with serum phosphorus concentration. J Am Soc Nephrol 21, 1223–1232, https://doi.org/10.1681/asn.2009111104 (2010).
Mondul, A. M. et al. Genome-wide association study of circulating retinol levels. Human molecular genetics 20, 4724–4731, https://doi.org/10.1093/hmg/ddr387 (2011).
Ferrucci, L. et al. Common variation in the beta-carotene 15,15′-monooxygenase 1 gene affects circulating levels of carotenoids: a genome-wide association study. Am J Hum Genet 84, 123–133, https://doi.org/10.1016/j.ajhg.2008.12.019 (2009).
Tanaka, T. et al. Genome-wide association study of vitamin B6, vitamin B12, folate, and homocysteine blood concentrations. Am J Hum Genet 84, 477–482, https://doi.org/10.1016/j.ajhg.2009.02.011 (2009).
Major, J. M. et al. Genome-wide association study identifies common variants associated with circulating vitamin E levels. Hum Mol Genet 20, 3876–3883, https://doi.org/10.1093/hmg/ddr296 (2011).
van Meurs, J. B. et al. Common genetic loci influencing plasma homocysteine concentrations and their effect on risk of coronary artery disease. Am J Clin Nutr 98, 668–676, https://doi.org/10.3945/ajcn.112.044545 (2013).
Burgess, S., Thompson, S. G. & Collaboration, C. C. G. Avoiding bias from weak instruments in Mendelian randomization studies. International journal of epidemiology 40, 755–764, https://doi.org/10.1093/ije/dyr036 (2011).
Burgess, S., Dudbridge, F. & Thompson, S. G. Combining information on multiple instrumental variables in Mendelian randomization: comparison of allele score and summarized data methods. Stat Med 35, 1880–1906, https://doi.org/10.1002/sim.6835 (2016).
Zhao, Q., Wang, J., Hemani, G., Bowden, J. & Small, D. S. Statistical inference in two-sample summary-data Mendelian randomization using robust adjusted profile score. arXiv preprint arXiv:1801.09652 (2018).
Verbanck, M., Chen, C. Y., Neale, B. & Do, R. Detection of widespread horizontal pleiotropy in causal relationships inferred from Mendelian randomization between complex traits and diseases. Nat Genet 50, 693–698, https://doi.org/10.1038/s41588-018-0099-7 (2018).
Hemani, G. et al. The MR-Base platform supports systematic causal inference across the human phenome. Elife 7, https://doi.org/10.7554/eLife.34408 (2018).
Author information
Authors and Affiliations
Contributions
Yan Guo designed the study, conducted the analysis and drafted the first draft. Yunlong Lu and Hongchuan Jin reviewed the design and analysis, commented on the text and provided subject matter expertise. All authors reviewed the final version for intellectual content.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Guo, Y., Lu, Y. & Jin, H. Appraising the role of circulating concentrations of micro-nutrients in epithelial ovarian cancer risk: A Mendelian randomization analysis. Sci Rep 10, 7356 (2020). https://doi.org/10.1038/s41598-020-63909-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-63909-5
This article is cited by
-
An atlas of associations between 14 micronutrients and 22 cancer outcomes: Mendelian randomization analyses
BMC Medicine (2023)
-
Systematic review of Mendelian randomization studies on risk of cancer
BMC Medicine (2022)
-
Pre-diagnostic dietary consumption of calcium and magnesium and calcium-to-magnesium intake ratio and ovarian cancer mortality: results from the ovarian cancer follow-up study (OOPS)
European Journal of Nutrition (2022)
-
Causal Effect of Genetically Determined Blood Copper Concentrations on Multiple Diseases: A Mendelian Randomization and Phenome-Wide Association Study
Phenomics (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.