Abstract
There are still lot of controversies whether aberrant left hepatic artery (ALHA) originating from left gastric artery should be ligated or preserved during gastric cancer (GC) surgery. We aimed to investigate this issue. We reviewed ALHA cases who had laparoscopic gastrectomy for gastric cancer at Seoul National University Hospital (SNUH) from 2012 to 2016. Type of ALHA variants using Michel’s classification of hepatic arterial anatomy and diameter of each vessel were evaluated by 2 radiologists. Postoperative hepatic function and surgical outcome were collected until 6 months after surgery. Results showed that if the diameter of ALHA was larger than 1.5 mm, a transient elevation of SGOT and SGPT on postoperative day 2 was observed in the ligated cases. No differences were observed in operation time, amount of blood loss, overall complication rate, hospital stay, and number of lymph nodes retrieved between the ligated and preserved replaced left hepatic artery (RLHA) and accessory left hepatic artery (acLHA) group. In this study, we conclude that ligation of ALHA seems to be safe as none of the patients suffered adverse outcome. A transient rise in postoperative SGOT and SGPT levels were seen after ligating ALHA >1.5 mm in diameter regardless of subtype.
Similar content being viewed by others
Introduction
About 25–75% of the population have variation in hepatic artery anatomy1. Twenty five percent of these are aberrant left hepatic artery (ALHA) originating from left gastric artery2 of which 55% and 45% are replaced (RLHA) and accessory (acLHA) type3. Recent data showed that the worldwide incidence of ALHA is 13.52% and for replaced and accessory type, 8.26% and 5.55% respectively4. These hepatic artery variants are occasionally seen during gastric cancer surgery and preservation of these arteries with complete removal of surrounding lymph nodes especially in laparoscopic surgery is challenging. Ligation or preservation of these arteries is of great concern to surgeons regarding patient’s postoperative liver function, safety and oncologic outcome.
Oncologic gastric surgery requires complete station 7 lymph node dissection5. In order to achieve this, left gastric artery should be ligated at the base to ensure en bloc lymph node dissection which means that when ALHA is present it should be ligated. Many literatures recommend preservation of ALHA during surgery especially in patients with pre-existing liver disease to prevent liver dysfunction and ischemia6,7. Although there were no difference in oncologic outcome between patients whose aberrant left hepatic artery were preserved or ligated during gastric cancer surgery as reported by Shinohara et al.8, many surgeons believed that preserving ALHA during surgery increases the operation time and blood loss especially during laparoscopic procedures. Mays et al.9 and Lee et al.10 have demonstrated in their studies that revascularization thru collateral flow takes place after ligation of hepatic arterial inflow8 and there were case reports of ligation of ALHA11, hepatic artery proper12 for ruptured aneurysm and accidental ligation of hepatic artery13 which showed no morbidity and mortality. The objective of this study is to determine if ligation of ALHA during laparoscopic gastrectomy for gastric cancer is safe with regards to patient’s postoperative short-term outcome and oncologic safety.
Methods
Patients
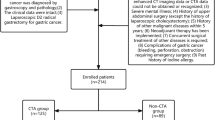
Medical records of 2,487 patients who had laparoscopic gastrectomy for gastric cancer at Seoul National University Hospital from January 2012 and December 2016 were reviewed. The presence of ALHA were initially noted on multidetector computed tomography (MDCT) reports. To confirm presence of ALHA and to check whether it was preserved or ligated, full-version video of each operation was reviewed.
Two radiologists independently reviewed each patient’s CT scan and categorized ALHA into either RLHA (Type II or IV) or acLHA (Type V, VII or VIII) based on Michel’s classification of hepatic arterial anatomy. The diameter of ALHA were also measured. Patients were then categorized into four groups: RLHA-ligated and preserved group and acLHA-ligated and preserved group. Staging of the gastric cancer was based on the International Union Against Cancer [UICC] TNM Classification, 7th edition. Patients who had palliative gastric surgery, history of previous gastric or liver surgery and combined gastric and liver operations were excluded from the study. This study was approved by the SNUH Institutional Review Board (IRB) with IRB no. H-1705-018-851. All procedures done were in accordance with the ethical standards. Because the risk is minimal for the patient, informed consent was waived by the Institutional Review Board.
Imaging
MDCT scanners with 16–256 detector rows (Definition, Siemens medical system; Brilliance 16, Philips Healthcare; Discovery HD750, GE healthcare) were used in the preoperative imaging. Stomach protocol CT consists of two phases for early gastric cancer (EGC) and three phases for advanced gastric cancer (AGC). For EGC, arterial and portal phase CT scan were obtained in right anterior oblique position. A delayed phase obtained in right down decubitus position was added for AGC. The following are CT acquisition parameters for MDCT: tube voltage of 100–120 kVp; tube current of 150–250 mAs; slice thickness of 1.3–3 mm; reconstruction interval of 0.7–3 mm; pitch of 0.9–1; rotation time of 0.5–1 sec. For contrast administration, an automatic power injector was used with iodinated contrast agent (350 or 370 mg·I/ml) at a rate of 3–5 ml/sec and at a dose of 1.5–1.6 ml/kg for 30 seconds. Saline chase was performed at the same rate for 10 seconds. By using the bolus tracking method, arterial phase scan was started 18–23 sec after the enhancement threshold (100 Hounsfield Unit HU) was reached in the descending thoracic aorta. For portal venous phase scan, a fixed delay of 65–75 sec was used.
Surgical procedure
The type of gastric resection (i.e. distal gastrectomy, proximal gastrectomy, pylorus-preserving gastrectomy or total gastrectomy) and the extent of lymphadenectomy (D1, D1 + or D2) were based on the TNM stage and location of the tumor as stated in the Japanese Gastric Cancer Association treatment guidelines 2014 (ver. 4)14. During surgery, tissues and lymph nodes located in the vicinity of the common hepatic (station 8), celiac axis (station 9) and proximal splenic artery (station 11p) were dissected to expose the origin of the left gastric artery. If an ALHA was encountered during dissection of the gastrohepatic ligament, if it were to be preserved, fat and lymphoid tissues around the entire course of the vessel were skeletonized during dissection and then ligated distal to the branching from the LGA. If ALHA were to be sacrificed, LGA was ligated at root of the vessel.
Postoperative evaluation
Postoperative short term outcome such as operation time, amount of blood loss, length of hospital stay after surgery and number of harvested lymph nodes were compared between each groups. Amount of blood loss was calculated based on the operative records. Liver function tests such as SGOT, SGPT, alkaline phosphatase and total bilirubin and surgical morbidity were reviewed at postoperative day 2, day 5, 2 weeks, 3 and 6 months using Clavien-Dindo classification of surgical complications15.
Statistical analysis
Data were analyzed using SPSS 20.0 (SPSS Inc, Chicago, IL, USA) and GraphPad Prism 7 (San Diego, CA) software. Chi-square test was used to compare patient characteristics and surgical complications. Liver function test results, operation outcome and number of harvested lymph nodes in each station on the lesser curvature side of the 4 groups were compared using Student t test. Pearson correlation and linear regression were used to correlate liver function parameter (SGOT, SGPT) with diameter of ALHA in ligated patients. Less than 0.05 p-value was considered statistically significant.
Results
Of the 2,487 laparoscopic gastrectomy cases screened, ALHA was seen in 442 (17.7%) patients of which 204 (8.2%) patients with complete data including operation video were included in the study. In the 204 patients, 131 (64.2%) were classified as replaced and 73 (35.8%) as accessory left hepatic artery and these arteries were preserved in the 135 (66.2%) cases and ligated in 69 (33.8%) cases.
Patient’s demographics
Patient characteristics are presented in Table 1. There are 204 patients included in the study, 140 are men and 64 are women. No significant differences were seen among the 4 groups in terms of age, gender, body mass index (BMI), surgery type and T and N stage (P > 0.05). There were 21 patients with pre-existing hepatic disease which includes drug induced liver injury (DILI), hepatitis infection and liver cirrhosis, 14 of these patients are in the RLHA-preserved group, 1 in acLHA-preserved, 3 in RLHA-ligated and 3 in acLHA-ligated group.
Changes in liver function
We reviewed the liver function tests done within 6 months postoperatively. Liver enzyme values are presented in Table 2. Significant higher levels of SGOT was seen on POD 2 in ligated RLHA group (p < 0.001) and significant higher levels of SGPT was seen on POD 2 and POD 5 in ligated RLHA group (p < 0.001, p 0.046). All values recovered completely two weeks after surgery without any medication or intervention. Mean total bilirubin level was slightly elevated at postoperative 6 months for the ligated RLHA group but we noted that there was no elevation of total bilirubin levels in the patient group except for one with Child’s B liver cirrhosis who had elevated baseline TB level preoperatively and on day 2,5, 2 weeks, 3 and 6 months postoperatively. We attributed this elevated TB level as a result of progression of the disease process. Differences in mean serum alkaline phosphatase were not significant between the 4 groups. The correlation of SGOT and SGPT levels with the diameter of the aberrant LHA in ligated patients were analyzed. There was no significant trend towards SGOT and SGPT elevation in either RLHA or acLHA (p = 0.853, 0.914, 0.523, 0.356 respectively) using the diameter of the vessel as continuous variable (Fig. 1) but when combining all ALHA ligated cases and divided into >1.5 mm and <1.5 mm diameter group, a significant higher level of SGOT and SGPT were seen on POD2 in the >1.5 mm group as shown in Fig. 2.
In this study, we had 21 patients with pre-existing liver disease. In 15 cases, ALHA was preserved and in 6 cases (3 replaced, 3 accessory), it was ligated. There was only transient increased in SGPT level on postoperative day 2 in RLHA ligated patients (Fig. 3).
Operative outcome
The operation data and complications are presented in Table 3. The median operation time, blood loss, hospital stay after operation and postoperative complications were not statistically different between the groups. There was no reported liver failure and mortality. Differences on the number of harvested lymph nodes in each station on the lesser curvature side (stations 1, 3, 5, 7, 8a, 9 and 11p) were also not statistically significant as presented in Table 4.
Discussion
Laparoscopic gastrectomy with oncologic lymph node dissection has been recommended for treatment of early gastric cancer in Japan and Korea16,17,18. Evidence have shown that laparoscopic gastrectomy had similar or even better outcome compared to open gastrectomy19,20,21 and is safe even in patients with chronic liver disease22. During laparoscopic gastrectomy for gastric cancer, aberrant left hepatic artery is occasionally seen. It is either a replaced artery or an accessory artery. Recent advancement of CT protocol makes preoperative detection and classification of ALHA possible10.
Today, there are still lots of debates on whether it is safe to ligate aberrant left hepatic artery during abdominal surgeries. In a study by Okano et al.23, ligation of aberrant left hepatic artery is safe as it only resulted in transient liver dysfunction. In contrast, other studies have reported severe complications such as abscess formation, cholangitis, liver failure, liver necrosis and even deaths after ligation of ALHA7,8,9. In our institution, we usually preserve the ALHA in early gastric cancer and sacrifice it in advanced cases.
In this study, we classified the ALHA into replaced or accessory type and reviewed each case retrospectively to see if ligation of these arteries during laparoscopic gastrectomy is safe or not in terms of postoperative liver function, surgical and oncologic outcome. Results showed that sacrificing RLHA or acLHA only resulted in transient elevation in SGOT and SGPT levels which spontaneously returned to normal two weeks after surgery. There were no reports of hepatic necrosis even after ligation of ALHA in patients with preexisting liver disease. This phenomenon showed that collateral arterial flow developed after ligation of hepatic artery, which have been demonstrated in the studies of Koehler et al.24 and Reimann et al.25
Oki et al.26 introduced a surgical technique to preserve ALHA but many surgeons believed that preserving the ALHA during laparoscopic gastrectomy will increase the surgical time and amount of blood loss. In our study, there were no significant differences in surgical time, amount of blood loss, number of lymph nodes retrieved in the lesser curvature side, length of hospital stay after surgery and complications among the four groups. These findings shows that ligated ALHA has same postoperative and oncologic outcome as preserving the ALHA.
According to previous reports, elevation of liver enzymes are usually encountered after ligation of large ALHA. We also found the same result in our study. Elevation of serum SGOT and SGPT were seen on postoperative day 2 in the ALHA-ligated group >1.5 mm diameter. Based on the analysis we performed, we recommend that after ligating ALHA >1.5 mm in diameter, liver enzymes should be monitored postoperatively.
A similar study was done by Kim et al.27 in 2016 but in our study we further categorized ALHA into replaced and accessory type to determine which type of ALHA is safer to preserve or ligate. We also measured the diameter of ALHA instead of LGA as this accurately measures the amount of blood flow to the portion of the liver supplied by the ALHA. This study had several limitations. First, there were only small number of ALHA cases and secondly, it is a single center experience so the total volume of patients enrolled are smaller. Despite of these limitations, we still had sufficient number of patients in each of the four groups that we compared and it showed that ligation of ALHA appeared to be safe as none of the patients suffered adverse outcome. A transient rise in postoperative SGOT and SGPT levels were seen after ligating ALHA >1.5 mm in diameter regardless of subtype. We recommend monitoring liver enzymes postoperatively in these type of patients especially for the RLHA subtype. Our suggestion may also applicable to any upper abdominal surgeries, such as fundoplication, myotomy, hiatal hernia and bariatric surgeries. Since this is a retrospective study, a prospective study involving larger number of patients is recommended for confirmation.
Data availability
All data generated or analyzed during this study are included in this published article (and its Supplementary Information files).
References
Hiatt, J. R., Gabbay, J. & Busuttil, R. W. Surgical anatomy of the hepatic arteries in 1000 cases. Ann. Surg. 220(1), 50–2, https://doi.org/10.1097/00000658-199407000-00008 (1994).
Tiwari, S., Roopashree, R., Padmavathi, G., Varalakshmi, K. L. & Sangeeta, M. Study of aberrant left hepatic artery from left gastric artery and its clinical importance. IJCRR. 6(17), 25–28 (2014).
Michel, N. A. Newer anatomy of the liver and its variant blood supply and collateral circulation. Am. J. Surg. 112(3), 337–47, https://doi.org/10.1016/0002-9610(66)90201-7 (1966).
Cirocchi, R et al. Aberrant left hepatic arteries arising from left gastric arteries and their clinical importance. The Surgeon. (19)30077-0, S1479-666X. https://doi.org/10.1016/j.surge.2019.06.002 (2019).
Japanese Gastric Cancer Association. Japanese classification of gastric carcinoma: 3rd English edition. Gastric Cancer. 14, 101–112 (2011).
Hendrickson, R. J. et al. Preservation of an aberrant left hepatic artery during laparoscopic nissen fundoplication. JSLS. 10(2), 180–3 (2006).
Huang, C. M. et al. Short-term clinical implications of the accessory left hepatic artery in patients undergoing radical gastrectomy for gastric cancer. PLoS One. 8(5), e64300, https://doi.org/10.1371/journal.pone.0064300 (2013).
Shinohara, T., Ohyama, S., Muto, T., Yanaga, K. & Yamaguchi, T. The significance of the aberrant left hepatic artery arising from the left gastric artery at curative gastrectomy for gastric cancer. Eur. J. Surg. Oncol. 33, 967–971, https://doi.org/10.1016/j.ejso.2007.02.030 (2007).
Mays, E. T. & Wheeler, C. S. Demonstration of collateral arterial flow after interruption of hepatic arteries in man. N. Engl. J. Med. 290, 993–996 (1974).
Lee, S. W. et al. Preoperative simulation of vascular anatomy by three-dimensional computed tomography imaging in laparoscopic gastric cancer surgery. J. Am. Coll. Surg. 197, 927–36 (2003).
Chirica, M. et al. Hepatic artery ligation: a simple and safe technique to treat extrahepatic aneurysms of the hepatic artery. Am. J. Surg. 196(3), 333–8, https://doi.org/10.1016/j.amjsurg.2007.08.074. (2008). Epub 2008 Jun 30.
Brittain, R. S., Marchioro, T. L., Hermann, G., Waddell, W. R. & Starzl, T. E. Accidental hepatic artery ligation in humans. Am. J. Surg. 107, 822–832 (1964).
Egorov, V. et al. Celiaco-mesenterial arterial aberrations in patients undergoing extended pancreatic resections: correlation of CT angiography with findings at surgery. JOP. 11(4), 348–357 (2010).
Japanese Gastric Cancer Association. Japanese gastric cancer treatment guidelines 2014 (ver. 4). Gastric Cancer. 20, 1–19, https://doi.org/10.1007/s10120-016-0622-4 (2017).
Dindo, D., Demartines, N. & Clavien, P. A. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann. Surg. 240(2), 205–213, https://doi.org/10.1097/01.sla.0000133083.54934.ae (2004).
Kitano, S. et al. A randomized controlled trial comparing open vs laparoscopy-assisted distal gastrectomy for the treatment of early gastric cancer: an interim report. Surgery. 131, S306–S311 (2002).
Kitano, S. & Shiraishi, N. Current status of laparoscopic gastrectomy for cancer in Japan. Surg. Endosc. 18, 182–185 (2004).
Kim, H. H. et al. Long-term results of laparoscopic gastrectomy for gastric cancer: a large-scale case-control and case-matched korean multicenter study. J. Clin. Oncol. 32(7), 627–33, https://doi.org/10.1200/JCO.2013.48.8551 (2014).
Kim, W. et al. Decreased morbidity of laparoscopic distal gastrectomy compared with open distal gastrectomy for stage I gastric cancer: short-term outcomes from a multicenter randomized controlled trial (KLASS-01). Ann. Surg. 263(1), 28–35, https://doi.org/10.1097/SLA.0000000000001346 (2016).
Oh, S. Y. et al. Outcomes of minimally invasive surgery for early gastric cancer are comparable with those for open surgery: analysis of 1,013 minimally invasive surgeries at a single institution. Surg. Endosc. 28(3), 789–95, https://doi.org/10.1007/s00464-013-3256-1 (2014).
Lee, H. J. & Yang, H. K. Laparoscopic gastrectomy for gastric cancer. Dig. Surg. 30(2), 132–41, https://doi.org/10.1159/000350884 (2013).
Yoon, H. M. et al. Comparison of liver function after laparoscopically assisted and open distal gastrectomies for patients with liver disease. Surg. Endosc. 25(6), 1761–5, https://doi.org/10.1007/s00464-010-1449-4 (2011).
Okano, S., Sawai, K., Taniguchi, H. & Takahashi, T. Aberrant left hepatic artery arising from the left gastric artery and liver function after radical gastrectomy for gastric cancer. World J. Surg. 17, 70–4 (1993).
Koehler, R. E., Korobkin, M. & Lewis, F. Arteriographic demonstration of collateral arterial supply to the liver after hepatic artery ligation. Radiology. 117, 49–54 (1975).
Reimann, B., Lierse, W. & Schreiber, H. W. Anastomoses between the segmental arteries of the liver and phrenicohepatic arterio-arterial anastomoses. Langenbecks Arch. Chir. 359, 81–92 (1983).
Oki, E. et al. Preservation of an aberrant hepatic artery arising from the left gastric artery during laparoscopic gastrectomy for gastric cancer. J. Am. Coll. Surg. 212, e25–e27, https://doi.org/10.1016/j.jamcollsurg.2011.01.009 (2011).
Kim, J. et al. Should an aberrant left hepatic artery arising from the left gastric artery be preserved during laparoscopic gastrectomy for early gastric cancer treatment? J. Gastric Cancer. 16(2), 72–77, https://doi.org/10.5230/jgc.2016.16.2.72 (2016).
Author information
Authors and Affiliations
Contributions
These are the contributions of each author: R.R.A., T.H.K. and S.H.P. collected the data, C.C.Z., J.S.B. and S.H.K. analyzed the data, R.R.A., F.B. and H.J.L. wrote the abstract, R.R.A., H.J.L., Y.S.S., S.H.K. and H.K.Y. wrote the manuscript, R.R.A. and C.C.Z prepared the tables and figures.
Corresponding author
Ethics declarations
Competing interests
Rene Ronson G. Ang, Hyuk-Joon Lee, Jae Seok Bae, Chun-Chao Zhu, Felix Berlth, Tae Han Kim, Shin-Hoo Park, Yun-Suhk Suh, Seong-Ho Kong, Se Hyung Kim, and Han-Kwang Yang declares that they have no financial and non-financial conflicts of interest to disclose.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ang, R.R.G., Lee, HJ., Bae, J.S. et al. Safety of Ligation of Aberrant Left Hepatic Artery Originating from Left Gastric Artery in Laparoscopic Gastrectomy for Gastric Cancer. Sci Rep 10, 5856 (2020). https://doi.org/10.1038/s41598-020-62587-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-62587-7
This article is cited by
-
Duplicate left gastric artery identified during robot-assisted distal gastrectomy: a case report
Surgical Case Reports (2023)
-
A rare case with multiple arterial variations of the liver complicated laparoscopic pancreaticoduodenectomy
BMC Gastroenterology (2022)
-
Real-time identification of aberrant left hepatic arterial territories using near-infrared fluorescence with indocyanine green during gastrectomy for gastric cancer
Surgical Endoscopy (2021)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.