Abstract
Batrachochytrium salamandrivorans (Bsal) is an emerging invasive pathogen that is highly pathogenic to salamander species. Modeling infection dynamics in this system can facilitate proactive efforts to mitigate this pathogen's impact on North American species. Given its widespread distribution and high abundance, the eastern newt (Notophthalmus viridescens) has the potential to significantly influence Bsal epidemiology. We designed experiments to 1) estimate contact rates given different host densities and habitat structure and 2) estimate the probability of transmission from infected to susceptible individuals. Using parameter estimates from data generated during these experiments, we modeled infection and disease outcomes for a population of newts using a system of differential equations. We found that host contact rates were density-dependent, and that adding habitat structure reduced contacts. The probability of Bsal transmission given contact between newts was very high (>90%) even at early stages of infection. Our simulations show rapid transmission of Bsal among individuals following pathogen introduction, with infection prevalence exceeding 90% within one month and >80% mortality of newts in three months. Estimates of basic reproductive rate (R0) of Bsal for eastern newts were 1.9 and 3.2 for complex and simple habitats, respectively. Although reducing host density and increasing habitat complexity might decrease transmission, these management strategies may be ineffective at stopping Bsal invasion in eastern newt populations due to this species’ hyper-susceptibility.
Similar content being viewed by others
Introduction
Across a variety of taxa, disease has been implicated as a major contributor to population- and species-level declines1,2,3,4,5,6. Epidemiological modeling can facilitate disease response and management by elucidating host-pathogen interactions and identifying strategies that could reduce the severity of outbreaks in wild populations7,8,9. Ideally, evaluating disease management strategies and modeling possible outcomes should occur prior to pathogen invasion, because the likelihood for disease control is greater and the cost of response is less8,10,11,12. Conversely, reactive or delayed responses to disease outbreaks can result in significant biodiversity loss and economic impact, as demonstrated by the unexpected emergence of Batrachochytrium dendrobatids (Bd)6,13,14 and Pseudogymnoascus destructans (the causative agent of White Nose syndrome)13,15.
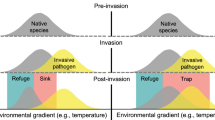
The newly emergent fungal pathogen Batrachochytrium salamandrivorans (Bsal) provides a unique opportunity to evaluate possible management strategies, especially in areas where it has yet to emerge. Bsal is rapidly spreading in Europe, where it is believed to have been introduced from Asia via the pet trade16,17. In areas where Bsal has emerged, populations of fire salamanders (Salamandra salamandra) have declined substantially18. Preventing and mitigating Bsal outbreaks is described as one of the greatest current priorities for wildlife conservation19. Bsal appears to have a high invasion probability and has already been detected in wild populations of salamanders in several European countries16,20,21, within captive populations in western Europe22,23, and in the pet trade24,25. Currently, Bsal has not yet been detected in North America, though several risk assessment models predict Bsal invasion probability is high due to suitable environmental conditions, high salamander diversity, and its high likelihood of entry through trade26,27,28.
Initial model simulations using European fire salamanders predict Bsal outbreaks at low host densities and rapid spread of the pathogen across a landscape, suggesting that mitigation efforts should focus on preventing pathogen introduction and transmission within populations29. Although these simulations are useful for informing disease response options for the fire salamander, they may not be translatable to North American ecosystems, where susceptible species have different life history strategies30,31,32. North America is home to the greatest biodiversity of salamanders in the world28. In eastern North America, one of the most widely distributed and common salamander species is the eastern newt (Notophthalmus viridescens31,32). The eastern newt is as susceptible to Bsal infection as the fire salamander16,33; hence, this species could play a major role in the epidemiology of Bsal if the pathogen is introduced to North America.
In this study, we develop an epidemiological model to understand Bsal transmission and mortality within a population of eastern newts. We parameterize this model using host contact rates and Bsal transmission probabilities estimated during two laboratory experiments. In the first experiment, we estimated contact rates of newts among different host densities and levels of habitat complexity, as prior work has demonstrated that both of these factors can influence host contacts and within-system pathogen transmission34,35,36,37,38,39,40. We hypothesized that contact rates would increase linearly with host density (i.e., mass-action density dependence), as seen in many wildlife disease systems36,41. Theory predicts that mass-action density dependence can lead to a stable equilibrium, with hosts persisting at low densities42. We also hypothesized that increasing habitat complexity would reduce host contacts by providing greater opportunity for spatial separation40. In the second experiment, we evaluated whether the probability of Bsal transmission from an infected to susceptible host via contact changed among different durations of disease progression (i.e., disease states) and among different rates of direct contact between susceptible and infected hosts. We hypothesized that hosts infected with Bsal for a greater amount of time would cause greater rates of transmission, because pathogen loads should be greater as disease progresses18,43,44,45. We also hypothesized that as host contact rate increased, pathogen transmission would increase46. Using contact and transmission estimates from these experiments, we simulated infection prevalence and mortality in an eastern newt population over three months, and estimated the basic reproductive rate (R0) for Bsal in simple and complex habitats42.
Results
Number of contacts per hour between newts was density dependent regardless of whether plants were absent (F2,81 = 199.3, P < 0.001) or present (F2,81 = 59.8, P < 0.001) in the mesocosms (Fig. 1). Per capita contact rates at 8 newts per m2 were 5–15X greater than 2 newts per m2. At 8 newts per m2, the presence of plants significantly reduced newt contacts by 3X(F1,58 = 80.3, P < 0.001), and at 4 newts per m2, plants reduced newt contacts by 35% (F1,52 = 4.89, P = 0.03; Fig. 1). Head, tail and leg contacts between newts were more common than ventrum and dorsum contacts (Fig. 2).
Estimated number of contacts per hour among three eastern newt densities per m2 when plants are absent (shaded bars) or present (9 plants/m2; white bars). Asterisks denote significant differences in host contact rates between habitat complexity treatments. Figure was produced from raw data with standard error bars based on back-transformed data used to construct linear models.
All susceptible newts (100%) became infected with Bsal following one or more contacts with an infected newt; the median duration to detectable infection was 7.5 days. Mortality of susceptible hosts began 22 days after contact with an infected host and increased rapidly thereafter (Figs. 3 and 4). Median duration to mortality was 32 days post-contact with an infected individual, with 89% cumulative mortality among contact treatments. Of the surviving newts (11%), all appeared to clear Bsal infection by the end of the 90-day experiment. Survival was similar among disease-state treatments (X22 = 0.2, P = 0.92; Fig. 3), despite that infected hosts had greater Bsal loads on their skin at 24 days compared to 12 days of disease progression (F2,7.8 = 7.3, P = 0.02; Fig. 5). Survival of susceptible hosts also was similar among contact-rate treatments (X22 = 1.4, P = 0.49; Fig. 4) – one contact for <1 second was sufficient to result in Bsal transmission from an infected to susceptible host.
Survival curves for susceptible hosts following contact with an infected host among different infected host disease states (12, 18, or 24 days post-exposure to Bsal); dashed lines represent 50% mortality. Survival probabilities did not differ significantly (P = 0.90) among disease states using Kaplan-Meier analysis.
Survival curves of susceptible hosts following contact with an infected host among different contact rates (one-second forced contact, 10-min cohabitation, or 30-min cohabitation); dashed lines represent 50% mortality. Survival probabilities did not differ significantly (P = 0.48) among host contact treatments by Kaplan-Meier analysis.
Infection loads of Bsal (copies/ uL) on the skin of infected newts that were exposed to susceptible newts at three states of disease progression (12, 18, or 24 days post-exposure to Bsal). Bsal loads in the infected hosts increased significantly with disease progression. Unlike letters above each disease state indicate significant differences detected in loads.
Using data from the these experiments, the functional form (Holling’s Type II) of the density dependent contact rate (per hour) was found and used with a system of differential equations to model infection and disease dynamics in a population of eastern newts. In an aquatic habitat with simple complexity (i.e., no plants), our simulations suggest that >95% of newts could become infected after one month following introduction of one infected newt, with >80% mortality in three months (Fig. 6). In more complex aquatic habitat (i.e., 9 plants per m2), infection prevalence was <80% and cumulative mortality was <70% over the same duration (Fig. 6). Using the cumulative proportion of infected individuals in Fig. 6 (Isimple = 0.95, Icomplex = 0.77), we estimated Ro as 1.9 and 3.2 for complex and simple habitats, respectively.
Cumulative proportion of infected and dead newts in a population simulated for 96 days following introduction of one infected adult eastern newt with Bsal transmission only occurring due to host-host contact. (A) Predicted dynamics in simple habitats (i.e., no plant treatment), and (B) complex habitats (i.e., 9 plants per m2) when contact is made with an infected host 12 days after initial exposure to Bsal. Open circles represent actual deaths recorded during experiments used to estimate model parameters (Supplementary Table S1).
Discussion
Our epidemiological model confirms that the eastern newt will likely play a major role in the epidemiology of Bsal if the pathogen emerges in North America33. Moreover, this abundant and widely distributed species could experience precipitous declines. The simulations show rapid transmission of Bsal among individuals, such that >90% of a population could become infected in less than one month, and mortality could exceed 80% in three months. Our results are similar to infection prevalence and mortality rates observed in wild fire salamander populations in Belgium18; however, the role of eastern newts in the epidemiology of Bsal in North America could be even more extreme. Our estimates of R0 exceeded one for eastern newts in all cases, which is similar to that estimated by Islam et al.47. The R0 is an estimate of secondary infections resulting from one infected salamander, hence R0 > 1 indicates infection will spread and an outbreak will occur42. As discussed below, the high contact rates and high probability of infection given contact certainly facilitate the likelihood of Bsal invasion in an eastern newt population. However, other aspects of eastern newt life history, might contribute to their role in Bsal epidemiology if the pathogen is introduced to North America. Eastern newts have a unique 3-stage life history where gregarious congregations of adults breed aquatically (hence facilitating density independent transmission), they lay eggs that develop into aquatic larvae, and larvae metamorphose to a juvenile eft stage that is terrestrial for up to eight years48,49. Eastern newt efts have high dispersal ability49,50, and they are susceptible to Bsal (MJG, unpubl. data), hence could play a role in the overland movement of Bsal among aquatic breeding sites and contamination of the terrestrial environment. Adult eastern newts can remain in the aquatic system or return to the terrestrial environment49, providing additional opportunities for maintenance and amplification of Bsal in both ecosystems. In comparison, fire salamanders are terrestrial species that interact with the aquatic environment only when viviparous larvae are born30,51, hence spillover and maintenance in the aquatic ecosystem is less likely than eastern newts. Despite potentially fewer transmission pathways than eastern newts, Bsal is devastating fire salamanders in Europe, which is not surprising because the estimated R0 = 945. The difference in R0 between these species may be related to their susceptibility to Bsal infection. Although both species are very susceptible to Bsal, the infectious dose (ID)-50 for eastern newts is approximately 3000 zoospores (MJG, unpubl. data); whereas, fire salamanders can be infected with as few as 100 zoospores18. Given the clear and present threat of Bsal to eastern newts, we recommend that future planning for Bsal invasion and intervention in North America take into consideration the possible epidemiological role of this species in both aquatic and terrestrial ecosystems33.
We found that contact rates of adult eastern newts in an aquatic environment were density dependent, and that relationship was stronger when habitat structure was less complex. In fact, the addition of plants to the aquatic environment reduced newt contact rates by 3X at the highest newt density (8 individuals/m2) tested. Our simulations also suggest that complex habitats might reduce Bsal infection prevalence and prevent population extirpation. Greer et al. (2008) hypothesized that pathogen transmission in wetlands grazed by cattle was higher due to reduced habitat structure and increased contact rates40. Similarly, Becker and Zamudio (2010) found that Bd spread more slowly in fragmented landscapes where host contacts between patches occurred less frequently52. Indeed, complex habitats might provide barriers to movement and additional sites for refugia, resulting in decreased host contact rates. Contrary to our original hypothesis, eastern newt contacts followed a Holling’s Type II functional form, where contacts increased linearly at typical eastern newt densities (e.g., 2–8 individuals/m2) but became saturated at simulated high densities (e.g., >50 newts/m2). Thus, density-independent transmission might be expected at high newt densities, which could occur during breeding, and is a common attribute of sexually transmitted diseases53,54,55. At lower newt densities, density reduction should reduce Bsal transmission. Reducing density from 8 to 2 newts per m2 reduced per capita contact rates by 5–15X. Thus, decreasing host density or increasing habitat complexity might be viable disease management options for reducing Bsal transmission, although population impacts might depend on host tolerance to Bsal infection. We hypothesize that these management strategies will be most effective for amphibian species that have moderate to high tolerance to Bsal infection, or if eastern newts are exposed to environmental conditions that negatively impact Bsal growth or persistence. It is likely that a combination of disease management strategies will be most effective at controlling Bsal invasions in eastern newt populations56.
Our study provides evidence that probability of Bsal transmission given contact is very high at 14 °C. One contact of one-second duration was sufficient to result in 100% transmission from an infected host at 12–24 days disease progression to a susceptible host. Other contact scenarios (10 and 30-min cohabitation) that we tested and modeled showed nearly identical infection and disease dynamics. Across all treatments, the estimated mortality of susceptible eastern newt hosts due to contact with an infected host was 89%. Hence, high contact rates of eastern newts and efficient transmission of Bsal due to direct contact will likely complicate possible disease intervention strategies for this hyper-susceptible host species, as suggested by previous work with fire salamanders29,57. Indeed, one caveat that should be considered is that reducing host density or increasing habitat complexity could prolong a Bsal outbreak in eastern newt populations44. Canessa et al. (2018, 2019)45,57, suggested that reduction in fire salamander density would need to exceed at least 80% to stop Bsal invasion (i.e., reduce R0 < 1).
The contact rates that we estimated for eastern newts at densities found in the wild were high. Even at the lowest density tested (2 newts per m2), there were on average 93 contacts per day and 1792 contacts per day in the highest newt density, both of which provide ample opportunity for Bsal transmission. Although plant structure was provided in the complex habitat treatment, it is possible that natural aquatic systems afford other conditions that facilitate host separation and reduce contact rates. Future research should estimate newt contact rates under more natural conditions. Additionally, our newts were captured during summer when some breeding activity occurs and maintained at 20–22 °C, which is typical of summer water temperatures in Tennessee58. Hence, contacts may be lower during seasons or in geographic locations with colder temperatures. That said, only 3% of our contacts lasted longer than 20 seconds (i.e., there were few cases of amplexus behavior). Also, ongoing research suggests that eastern newts are more susceptible to Bsal at colder temperatures (EDC and MJG, unpubl. data), hence even if contact rates are lower than what we estimated, the probability of Bsal transmission given contact may remain high at colder temperatures. We expect that invasion probability of Bsal in eastern newt populations will change among seasons59, which is the focus of ongoing research.
Our study did not model environmental transmission60. Bsal transmission can occur via mobile and encysted spores through water and soil18. We suspect that addition of these additional transmission pathways will create even faster infection and disease outcomes. Moreover, as infected newt density increases, we anticipate the environmental population of zoospores will grow, and contribute more to epidemiological dynamics47,61. Fortunately, it appears that the environmental persistence of Bsal zoospores in water with microbes or on soil is probably <1 week18. Hence, the contribution of environmental transmission to Bsal epidemiology might be a tradeoff between zoospore production by hosts and zoospore degradation in the environment61.
Loads of Bsal on eastern newt skin increased with disease progression, which was expected, as the infection became systemic and more zoospores and zoosporangia were present. However, interestingly, Bsal transmission to susceptible individuals and subsequent development of disease were similar regardless of the infected host disease state, further providing evidence of very efficient transmission between hosts. We suspect eastern newts have few immunological barriers to Bsal infection. If skin microbes (e.g., Pseudomonas) are proved to provide inhibitory effects on Bsal62, bioaugmentation of hosts or the environment that can increase the abundance of Bsal-inhibiting microbes on the skin might be a viable disease management strategy63.
Eleven percent of susceptible hosts (5/45) became infected with Bsal yet did not experience disease-induced mortality at 90 days post-exposure and they appeared to clear the infection. These results differ from European fire salamanders, where 100% mortality is observed following exposure to Bsal18,45. The individuals that survived were across all disease-state and contact-rate treatments, so no relationship between infection intensity and contact was identified. It is possible these individuals had different microbiome attributes that afforded protection62, or may have been genetically predisposed to be more immunologically resistant to severe infection. It also is possible that these individuals by chance did not have sufficient host contact to result in a large number of zoospores encysting during transmission. Our results suggest that location of host contact could play a role in Bsal transmission. The majority of contacts that we observed were on the head, tail and legs, which also corresponds to the frequent location of Bsal lesions64,65; (MJG and DLM, unpubl. data). Thus, perhaps contacts for these individuals occurred in locations with lower Bsal infection intensity.
Considering the eastern newt’s widespread distribution, high dispersal ability, and high susceptibility, we believe this species will significantly impact Bsal epidemiology should the pathogen reach North America. In addition, eastern newts could play a major role in transmitting Bsal to other species. The distribution of eastern newts overlaps with some of the highest salamander species richness in North America, and encompasses a global hotspot for Plethodontidae (lungless salamander) diversity. There is growing evidence that several species of lungless salamanders are susceptible to Bsal infection and chytridiomycosis66. Future research needs to include multiple species interactions and estimate community-level R0 under different management scenarios57.
Our results suggest a grim outcome for eastern newts and other highly susceptible species if Bsal is introduced to North America; thus, actions that reduce the likelihood of introduction are key57. The U.S. Fish and Wildlife Service implemented a ban on trade of 201 salamander species due to the risk of Bsal invasion67. Although this action likely reduced number of Bsal-infected salamanders entering the United States via international trade, it did not eliminate the threat. In fact, we now know that frogs can be infected with Bsal18,25, and anurans dominate (ca. 94%) international amphibian trade in the United States68. We recommend that future management actions for Bsal include clean trade, where animal health certificates accompany shipments that verify animals are pathogen-free. Currently, no regulations exist in North America requiring clean trade of amphibians, despite three amphibian pathogens (including Bsal) listed as notifiable by the World Organization for Animal Health23,69. If regulations are enacted, government resources should be allocated to verify compliance and subsidize amphibian trade industries.
Methods
Model organism
Adult eastern newts were collected from two wild populations in eastern Tennessee, USA, in Carter County (36.177N, -82.113W) and Knox County (35.847N, -83.872W) in May 2017 and August 2018 under Tennessee Wildlife Resources Agency Science Collection Permit #1504. Following capture, newts were transported by vehicle in <3 hrs to the Johnson Animal Research and Teaching Unit facility at the University of Tennessee and held in large mesocosm tanks at room temperature prior to the experiments. All experiments described herein were approved by the University of Tennessee approved Institutional Animal Care and Use Committee under protocol #2395. All procedures described followed the Association for Assessment and Accreditation of Laboratory Animal Care International Standards.
Experiment 1: Estimating contact rates among newt densities and habitat complexity
Newts were randomly assigned to one of six circular 1-m2 aquatic mesocosms (i.e., experimental units) containing approximately 7 cm of aged, dechlorinated water and maintained at room temperature (20–22 °C). Due to space limitations in the laboratory, we tested one host-density treatment (2, 4, or 8 newts) per week. These densities represent a natural range of eastern newt densities in the wild and have been used in other density-focused studies70,71,72. After each week, mesocosms were drained and refilled with aged, dechlorinated water in order to maintain favorable water quality, and we re-randomized newts into mesocosms at a new density to randomly distribute any biases associated with captive duration among experimental effects. For the complex habitat treatment, we repeated the experiment following the same weekly randomization with artificial plants present in the mesocosms. We placed nine artificial plants (ca. 9 cm in height) in a 3 × 3 grid in each mesocosm, with each plant equidistant from each other (ca. 15 cm apart). Newts were fed ad libitum by equally dispersing thawed brine shrimp daily throughout each mesocosm. The laboratory was set to 12 hours of light and dark per diel cycle, which is typical daylight duration in Tennessee during summer.
To ensure observers did not influence movements, number of newt contacts per hour was estimated using a surveillance camera (Night Owl, Model: DVR-BBHDA10PB-82-RS; Naples, FL, USA) suspended ca. 170 cm above each mesocosm. Video was recorded for one hour during each of four diel periods (0–0600, 0600–1200, 1200–1800, 1800–2400 hrs), resulting in four hours of video observed per mesocosm per day. We averaged number of newt contacts among the diel periods and days for each mesocosm to obtain a robust estimate of contacts per hour for each host density and plant treatment. One contact was defined as a noticeable contact between two newts, such that one newt responded to contact from the other.
Experiment 2: Estimating the probability of Bsal transmission among disease states and contact frequencies
A separate group of newts were collected from the wild for Experiment 2. Newts were housed individually in 2000-cm3 circular containers (diameter = 16.5 cm) with ca. 300 mL of aged, dechlorinated water and a PVC cover object. Because co-infection with B. dendrobatidis (Bd) could influence Bsal infection dynamics33, we heat-treated eastern newts upon arrival to the laboratory in an environmental chamber held at 30 °C for 9 days73. We did not test the newts for Bd infection prior to heat treatment, because prior exposure to Bd does not seem to connote acquired immunity to Bsal33. After heat treatment, we decreased temperature over four days to 14 °C and held them at that temperature for four additional days before starting the experiment. We verified that all newts were Bd-negative using quantitative PCR (protocol discussed below) prior to beginning the experiment. Every three days, we changed housing containers, cover objects and water, and fed newts frozen bloodworms at 2% of their initial body mass.
After the heat treatment, newts were randomly assigned to two groups of either infected or susceptible hosts. Infected hosts (n = 15) were exposed to a standardized quantity of Bsal zoospores (5 × 106 zoospores/mL) in a 10-mL water bath for 24 hours. We cultured Bsal on TgHL plates and harvested them by flooding each plate with a total of 6 mL of autoclaved dechlorinated water and filtering the suspended zoospores through a 20-um filter. Zoospores were enumerated by hemocytometry and verified by flow cytometry. After 12, 18 and 24 days post-exposure (i.e., referred to as disease states in this study), one infected newt was exposed to a susceptible newt through one of three contact frequency treatments: one-second forced contact, 10-min cohabitation, and 30-min cohabitation (n = 5 susceptible newts per treatment combination). The one-second contact involved ventrum (infected) to ventrum (susceptible) touching for <1 second then animal separation. For cohabitation, susceptible and infected individuals were co-housed in a 2000-cm3 circular container with ca. 300 mL of aged, dechlorinated water for the specified duration. To relate cohabitation treatments to contacts, we recorded and enumerated contacts in each container. The average number of contacts in the 10- and 30-min cohabitation treatments were 19 + 2 and 41 + 6 (s.e.m.), respectively. Location of newt contacts also was recorded for five major body regions: head, tail, legs, dorsum and ventrum.
Following the contact-exposure treatments, susceptible newts were housed in individual containers (same size as above) in environmental chambers at 14 °C, newts were inspected daily for signs of Bsal chytridiomycosis, and animals euthanized using benzocaine hydrochloride (100 mg/L) at humane endpoints of disease progression. To test for Bsal infection, we swabbed infected and susceptible newts every six days following the standardized protocol for Bd74. Genomic DNA was extracted from each swab using Qiagen DNeasy Blood and Tissue kits (Qiagen, Hilden, Germany), and Bsal presence and load on each swab estimated using qPCR methods similar to those described in Blooi et al. 75. All qPCR reactions were amplified using an Applied Biosystems Quantstudio 6 Flex qPCR instrument. Each swab sample was run in duplicate and considered positive if both replicates amplified within 50 cycles. We confirmed Bsal infection on a subset of animals representing each experiment by performing histological examinations of epidermal tissues. The experiment ended at 90 days post-exposure to an infected newt, which is sufficient duration for Bsal chytridiomycosis to develop in eastern newts16.
Statistical analyses
For experiment one, we used two-way analysis-of-variance76 and Tukey-Kramer post-hoc tests77 to test for differences in contact rates among density and habitat complexity treatments. For experiment two, we used Kaplan-Meier survival analyses to compare median survival duration among disease-state and contact-frequency treatments78. Because the same infected individuals were used for each subsequent disease-state treatment, we used a linear mixed-effects model79 to compare Bsal loads in these newts among disease-state treatments (12, 18 and 24-days post-exposure). Post-hoc comparisons of Bsal loads among disease states were performed using Tukey contrasts80.
We used a hierarchical Bayesian model to estimate the proportion of contacts between newts to be expected across five body regions (head, tail, ventrum, dorsum, and legs) during cohabitation in the second experiment81. This approach allowed us to model the contact proportions by body area as a multinomial distribution with parameter values unique to each cohabitation replicate. We modeled each replicate as a multinomial distribution, and parameters were drawn from a Dirichlet distribution using a 100,000 step Markov-Chain-Monte-Carlo following a burn-in of 500 steps. The estimated posterior distributions were interpreted as an estimate of the probability of host contact to each body location for the overall population.
Epidemiological model
Because our data suggested density dependent contact rates that increased linearly at low densities and reached an asymptotic maximum at higher densities, we modeled host transmission given contact using the following Holling’s type II functional form82:
here, f(N) represents the per capita newt contacts per hour for a given newt density N; c is the value of the asymptote as N approaches infinity, and K is the half-saturation constant (f(K) = c/2). The parameters c and K were estimated by fitting f to contact and transmission data from Experiments 1 and 2 using multistart with constrained optimization in the MATLAB global optimization toolbox where \(0\le c\le 100\) and \(0\le K\le 18\times {10}^{4}\). Supplementary Table S1 provides estimates for c and K.
We modeled Bsal transmission, as it occurred in Experiment 2, using a system of ordinary differential equations with three compartments: Susceptible S, Exposed E, and Infected I individuals.
Susceptible individuals (S) transitioned to the exposed compartment (E) if they remained qPCR negative following cohabitation with an infected newt. Exposed individuals were deemed infected (I) and capable of Bsal transmission after two qPCR positive swabs. We defined the latency period as the estimated number of days between cohabitation and two qPCR positive results (note: swabbing frequency was every six days).
This model includes the transmission rate (i.e., product of the transmission probability given a contact, β, with the frequency interaction term S(I/N) and the density dependent contact rate function \(f(N)=\frac{cN}{K+N}\)), latency rate γ (from exposed to infected), and a disease-induced death rate d. The characteristic function χ[0,10] denotes the number of minutes that the susceptible newts were in contact with infected newts, which in this case was the 10-min cohabitation experiment. For additional details on how parameters were estimated, please see the Supplemental Information file.
Using this system of differential equations, we simulated not only infection prevalence, but also the cumulative proportion of mortality in a population of eastern newts over 90 days due solely to contact transmission. Because model simulations for the 10- and 30-min cohabitation treatments were nearly identical, we present the modeling results in Fig. 6 for the 10-min cohabitation data with and without plants present. We estimated the basic reproductive rate (R0) of Bsal by using equation 6.21 in Anderson and May (1991:127)42 and the cumulative proportion of infected newts for each simulation interpolated from Fig. 6 as the asymptotic level. We decided to not model the one-second contact data, because the treatment represented forced human-induced contact. Also, we performed simulations for all infected host disease states (12–18- and 24 days post-exposure), but simulations are presented for the 12-day infected hosts only because outcomes were similar among disease states. The data sets and code for all statistical analyses and modelling are available in Supplementary File 2.
References
Wilcove, D. S., Rothstein, D., Dubow, J., Phillips, A. & Losos, E. Quantifying Threats to Imperiled Species in the United States. Bioscience 48, 607–615 (1998).
Stuart, S. N. et al. Status and trends of amphibian declines and extinctions worldwide. Science (80−). 306, 1783–1786 (2004).
Griffiths, R. A. & Pavajeau, L. Captive breeding, reintroduction, and the conservation of amphibians. Conservation Biology 22, 852–861 (2008).
Daszak, P., Cunningham, A. A. & Hyatt, A. D. Infectious disease and amphibian population declines. Diversity and Distributions 9, 141–150 (2003).
Daszak, P. et al. Emerging infectious diseases and amphibian population declines. Emerg. Infect. Dis. 5, 735–748 (1999).
Scheele, B. C. et al. Amphibian fungal panzootic causes catastrophic and ongoing loss of biodiversity. Science (80−). 363, 1459–1463 (2019).
Fenichel, E. P., Horan, R. D. & Hickling, G. J. Management of infectious wildlife diseases: Bridging conventional and bioeconomic approaches. Ecol. Appl. 20, 903–914 (2010).
Grant, E. H. C. et al. Using decision analysis to support proactive management of emerging infectious wildlife diseases. Front. Ecol. Environ. 15, 214–221 (2017).
Gray, M. J. et al. Pathogen Surveillance in Herpetofaunal Populations: Guidance on Study Design, Sample Collection, Biosecurity, and Intervention Strategies. Herpetol. Rev. 48, 334–351 (2017).
Langwig, K. E. et al. Context-dependent conservation responses to emerging wildlife diseases. Frontiers in Ecology and the Environment 13, 195–202 (2015).
Fraser, C., Riley, S., Anderson, R. M. & Ferguson, N. M. Factors that make an infectious disease outbreak controllable. Proc. Natl. Acad. Sci. USA 101, 6146–6151 (2004).
World Bank. PEOPLE, PATHOGENS AND OUR PLANET Volume 2 - The Economics of One Health. The World Bank 2, (2012).
Voyles, J. et al. Moving Beyond Too Little, Too Late: Managing Emerging Infectious Diseases in Wild Populations Requires International Policy and Partnerships. Ecohealth 12, 404–407 (2014).
Berger, L. et al. Chytridiomycosis causes amphibian mortality associated with population declines in the rain forests of Australia and Central America. Proc. Natl. Acad. Sci. USA 95, 9031–9036 (1998).
Lorch, J. M. et al. Experimental infection of bats with Geomyces destructans causes white-nose syndrome. Nature 480, 376–378 (2011).
Martel, A. et al. Recent introduction of a chytrid fungus endangers Western Palearctic salamanders. Science (80−). 346, 630–631 (2014).
Yap, T. A., Nguyen, N. T., Serr, M., Shepack, A. & Vredenburg, V. T. Batrachochytrium salamandrivorans and the Risk of a Second Amphibian Pandemic. EcoHealth 14, 851–864 (2017).
Stegen, G. et al. Drivers of salamander extirpation mediated by Batrachochytrium salamandrivorans. Nature 544, 353–356 (2017).
Berger, L. et al. History and recent progress on chytridiomycosis in amphibians. Fungal Ecol. 19, 89–99 (2016).
Feldmeier, S. et al. Exploring the distribution of the spreading lethal salamander chytrid fungus in its invasive range in Europe - A macroecological approach. Plos One 11 (2016).
Spitzen-van der Sluijs, A. et al. Expanding distribution of lethal amphibian fungus Batrachochytrium salamandrivorans in Europe. Emerg. Infect. Dis. 22, 1286–1288 (2016).
Sabino-Pinto, J. et al. First detection of the emerging fungal pathogen Batrachochytrium salamandrivorans in Germany. Amphib. Reptil. 36, 411–416 (2015).
Fitzpatrick, L. D., Pasmans, F., Martel, A. & Cunningham, A. A. Epidemiological tracing of Batrachochytrium salamandrivorans identifies widespread infection and associated mortalities in private amphibian collections. Sci. Rep. 8 (2018).
Cunningham, A. A. et al. Surveillance: Emerging disease in UK amphibians. Vet. Rec. 176, 468 (2015).
Nguyen, T. T., Nguyen, T. V., Ziegler, T., Pasmans, F. & Martel, A. Trade in wild anurans vectors the urodelan pathogen Batrachochytrium salamandrivorans into. Europe. Amphib. Reptil. 38, 554–556 (2017).
Grant, E. H. C. et al. Salamander chytrid fungus (Batrachochytrium salamandrivorans) in the United States—Developing research, monitoring, and management strategies. Open-File Rep., https://doi.org/10.3133/ofr20151233 (2016).
Richgels, K. L. D., Russell, R. E., Adams, M. J., White, C. L. & Grant, E. H. C. Spatial variation in risk and consequence of Batrachochytrium introduction in the USA Subject Areas: R. Soc. open sci. (2016).
Yap, T. A., Koo, M. S., Ambrose, R. F., Wake, D. B. & Vredenburg, V. T. Averting a North American biodiversity crisis: A newly described pathogen poses a major threat to salamanders via trade. Science (80−). 349, 481–482 (2015).
Schmidt, B. R., Bozzuto, C., Lötters, S. & Steinfartz, S. Dynamics of host populations affected by the emerging fungal pathogen Batrachochytrium salamandrivorans. R. Soc. Open Sci. 4 (2017).
Alcobendas, M., Dopazo, H. & Alberch, P. Geographic variation in allozymes of populations of Salamandra salamandra (Amphibia: Urodela) exhibiting distinct reproductive modes. J. Evol. Biol. 9, 83–102 (1996).
Scott, D. E. & Petranka, J. W. Salamanders of the United States and Canada. Copeia 1999, 845 (1999).
Niemiller, M. & Reynolds, R. The Amphibians of Tennessee. Choice Rev. Online 49, 49-5058–49–5058 (2012).
Longo, A. V., Fleischer, R. C. & Lips, K. R. Double trouble: co-infections of chytrid fungi will severely impact widely distributed newts. Biol. Invasions 21, 2233–2245 (2019).
Penczykowski, R. M., Hall, S. R., Civitello, D. J. & Duffy, M. A. Habitat structure and ecological drivers of disease. Limnol. Oceanogr. 59, 340–348 (2014).
Briggs, C. J., Knapp, R. A. & Vredenburg, V. T. Enzootic and epizootic dynamics of the chytrid fungal pathogen of amphibians. Proc. Natl. Acad. Sci. USA 107, 9695–9700 (2010).
Greer, A. L., Briggs, C. J. & Collins, J. P. Testing a key assumption of host-pathogen theory: Density and disease transmission. Oikos 117, 1667–1673 (2008).
Echaubard, P., Little, K., Pauli, B. & Lesbarréres, D. Context-dependent effects of ranaviral infection on northern leopard frog life history traits. Plos One 5 (2010).
Rachowicz, L. J. & Briggs, C. J. Quantifying the disease transmission function: Effects of density on Batrachochytrium dendrobatidis transmission in the mountain yellow-legged frog Rana muscosa. J. Anim. Ecol. 76, 711–721 (2007).
Kjær, L. J., Schauber, E. M. & Nielsen, C. K. Spatial and Temporal Analysis of Contact Rates in Female White-Tailed Deer. J. Wildl. Manage. 72, 1819–1825 (2008).
Greer, A. L. & Collins, J. P. Habitat fragmentation as a result of biotic and abiotic factors controls pathogen transmission throughout a host population. J. Anim. Ecol. 77, 364–369 (2008).
Habib, T. J., Merrill, E. H., Pybus, M. J. & Coltman, D. W. Modelling landscape effects on density-contact rate relationships of deer in eastern Alberta: Implications for chronic wasting disease. Ecol. Modell. 222, 2722–2732 (2011).
Anderson, R. M. & May, R. M. (Robert M. Infectious diseases of humans: dynamics and control. (Oxford University Press, 1991).
Brunner, J. L., Schock, D. M. & Collins, J. P. Transmission dynamics of the amphibian ranavirus Ambystoma tigrinum virus. Dis. Aquat. Organ. 77, 87–95 (2007).
Quinn, T. C. et al. Viral load and heterosexual transmission of human immunodeficiency virus type 1. N. Engl. J. Med. 342, 921–929 (2000).
Canessa, S. et al. Decision-making for mitigating wildlife diseases: From theory to practice for an emerging fungal pathogen of amphibians. J. Appl. Ecol. 55, 1987–1996 (2018).
Klous, G., Huss, A., Heederik, D. J. J. & Coutinho, R. A. Human-livestock contacts and their relationship to transmission of zoonotic pathogens, a systematic review of literature. One Health 2, 65–76 (2016).
Islam, R. Gray, M. J. & Peace, A. Identifying the Dominant transmission pathway in a multi-stage infection model of the Emerging Fungal Pathogen Batrachochytrium salamandrivorans on the Eastern Newt. Math. Planet Earth (Infectious Dis. Our Planet), Springer, New York (2020, in press).
Healy, W. R. Population Consequences of Alternative Life Histories in Notophthalmus v. viridescens. Copeia 1974, 221 (1974).
Gill, D. E. The Metapopulation Ecology of the Red-Spotted Newt, Notophthalmus viridescens (Rafinesque). Ecol. Monogr. 48, 145–166 (1978).
Roe, A. W. & Grayson, K. L. Terrestrial Movements and Habitat Use of Juvenile and Emigrating Adult Eastern Red-Spotted Newts, Notophthalmus Viridescens. J. Herpetol. 42, 22–30 (2008).
Wells, K. D. The Ecology and Behavior of Amphibians. The Ecology and Behavior of Amphibians, https://doi.org/10.7208/chicago/9780226893334.001.0001 (2013).
Becker, C. G. & Zamudio, K. R. Tropical amphibian populations experience higher disease risk in natural habitats. Proc. Natl. Acad. Sci. USA 108, 9893–9898 (2011).
Thrall, P. H., Antonovics, J. & Hall, D. W. Host and pathogen coexistence in sexually transmitted and vector- borne diseases characterized by frequency-dependent disease transmission. Am. Nat. 142, 543–552 (1993).
Getz, W. M. & Pickering, J. Epidemic Models: Thresholds and Population Regulation. Am. Nat. 121, 892–898 (1983).
Antonovics, J., Iwasa, Y. & Hassell, M. P. A generalized model of parasitoid, venereal, and vector-based transmission processes. Am. Nat. 145, 661–675 (1995).
Thomas, V. et al. Mitigating Batrachochytrium salamandrivorans in Europe. Amphibia Reptilia 40, 265–290 (2019).
Canessa, S., Bozzuto, C., Pasmans, F. & Martel, A. Quantifying the burden of managing wildlife diseases in multiple host species. Conserv. Biol., cobi.13313, https://doi.org/10.1111/cobi.13313 (2019).
Schmutzer, A. Influences of Cattle on Community Structure and Pathogen Prevalence in Larval Amphibians on the Cumberland Plateau, Tennessee. Masters Theses (2007).
Bozzuto, C. & Canessa, S. Impact of seasonal cycles on host-pathogen dynamics and disease mitigation for Batrachochytrium salamandrivorans. Glob. Ecol. Conserv. 17 (2019).
Fisher, M. C. Ecology: In peril from a perfect pathogen. Nature 544, 300–301 (2017).
Wilber, M. Q., Knapp, R. A., Toothman, M. & Briggs, C. J. Resistance, tolerance and environmental transmission dynamics determine host extinction risk in a load-dependent amphibian disease. Ecology Letters 20, 1169–1181 (2017).
Bletz, M. C. et al. Disruption of skin microbiota contributes to salamander disease. Proceedings. Biol. Sci. 285 (2018).
Woodhams, D. C., Bletz, M., Kueneman, J. & McKenzie, V. Managing Amphibian Disease with Skin Microbiota. Trends in Microbiology 24, 161–164 (2016).
Martel, A. et al. Batrachochytrium salamandrivorans sp. nov. causes lethal chytridiomycosis in amphibians. Proc. Natl. Acad. Sci. USA 110, 15325–15329 (2013).
Van Rooij, P., Martel, A., Haesebrouck, F. & Pasmans, F. Amphibian chytridiomycosis: A review with focus on fungus-host interactions. Veterinary Research 46 (2015).
Carter, E. D. et al. Conservation risk of Batrachochytrium salamandrivorans to endemic lungless salamanders. Conserv. Lett., https://doi.org/10.1111/conl.12675 (2019).
Klocke, B. et al. Batrachochytrium salamandrivorans not detected in U.S. survey of pet salamanders. Scientific Reports 7 (2017).
Gray, M. J. et al. Batrachochytrium salamandrivorans: The North American Response and a Call for Action. PLoS Pathogens 11 (2015).
Schloegel, L. M., Daszak, P., Cunningham, A. A., Speare, R. & Hill, B. Two amphibian diseases, chytridiomycosis and ranaviral disease, are now globally notifiable to the World Organization for Animal Health (OIE): An assessment. Dis. Aquat. Organ. 92, 101–108 (2010).
Harris, R., Alford, R. & Wilbur, H. Are there jobs for all in the shipping industry? Herpetologica 44, 8 (1988).
Morin, P. J. Competitive and Predatory Interactions in Natural and Experimental Populations of Notophthalmus viridescens dorsalis and Ambystoma tigrinum. Copeia 1983, 628 (1983).
Morin, P. J., Wilbur, H. M. & Harris, R. N. Salamander predation and the structure of experimental communities: responses of Notophthalmus and microcrustacea. Ecology 64, 1430–1436 (1983).
Bletz, M. Probiotic bioaugmentation of an anti-Bd bacteria, Janthinobacterium lividum, on the amphibian, Notophthalmus viridescens: Transmission efficacy and persistence of the probiotic on the host and non-target effects of probiotic addition on ecosystem componen. Masters Theses (2013).
Boyle, D. G., Boyle, D. B., Olsen, V., Morgan, J. A. T. & Hyatt, A. D. Rapid quantitative detection of chytridiomycosis (Batrachochytrium dendrobatidis) in amphibian samples using real-time Taqman PCR assay. Dis. Aquat. Organ. 60, 141–148 (2004).
Blooi, M. et al. Duplex real-Time PCR for rapid simultaneous detection of Batrachochytrium dendrobatidis and Batrachochytrium salamandrivorans in amphibian samples. J. Clin. Microbiol. 51, 4173–4177 (2013).
Girden, E. R. ANOVA: repeated measures. (Sage Publications, 1992).
Hayter, A. J. A Proof of the Conjecture that the Tukey-Kramer Multiple Comparisons Procedure is Conservative. Ann. Stat. 12, 61–75 (1984).
Jager, K. J., Van Dijk, P. C., Zoccali, C. & Dekker, F. W. The analysis of survival data: The Kaplan-Meier method. Kidney Int. 74, 560–565 (2008).
Bates, D., Mächler, M., Bolker, B. M. & Walker, S. C. Fitting linear mixed-effects models using lme4. J. Stat. Softw. 67 (2015).
Hothorn, T., Bretz, F. & Westfall, P. Simultaneous inference in general parametric models. Biometrical Journal 50, 346–363 (2008).
Fordyce, J. A., Gompert, Z., Forister, M. L. & Nice, C. C. A hierarchical bayesian approach to ecological count data: A flexible tool for ecologists. Plos One 6 (2011).
Kot, M. Elements of mathematical ecology. Choice Reviews Online 39, (Cambridge University Press, 2002).
Acknowledgements
We thank The University of Tennessee (UT) College Scholars Program and the Institute of Agriculture for supporting this research. The following UT personnel made this work possible: Bobby Simpson, Alex Anderson, Brittany Bajo, Rajeev Kumar, Brian Gleaves, Ciara Sheets and Bailee Augustino. Partial support (LAM, OFP, SL) was provided by the National Institute for Mathematical and Biological Synthesis, an Institute supported by the National Science Foundation through NSF Award #DBI-1300426. National Science Foundation Division of Environmental Biology (DEB-#1814520) also provided partial support for DAM, EDC, MJG and DLM. This work was completed under Hatch Project 1012932 of the USDA National Institute of Food and Agriculture. We thank Susan Kalisz, Jeffrey Kovac, and Cheryl Kojima for co-mentoring DAM and for helpful comments on earlier versions of this manuscript. We thank Frank Pasmans and An Martel of Ghent University for providing the Bsal used in this study.
Author information
Authors and Affiliations
Contributions
D.A.M. and M.J.G. designed the experiment. D.A.M. and E.D.C. carried out the experiment and collected the data. D.A.M. conducted the statistical analysis with guidance from E.D.C., J.A.F. and M.J.G. L.A.M., O.F.P., S.L., M.J.G., and D.A.M. designed the epidemiological model and performed the simulations. All authors (including A.C.P. and D.L.M.) contributed to manuscript writing.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Malagon, D.A., Melara, L.A., Prosper, O.F. et al. Host density and habitat structure influence host contact rates and Batrachochytrium salamandrivorans transmission. Sci Rep 10, 5584 (2020). https://doi.org/10.1038/s41598-020-62351-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-62351-x
This article is cited by
-
Pathways linking nutrient enrichment, habitat structure, and parasitism to host–resource interactions
Oecologia (2024)
-
Broad host susceptibility of North American amphibian species to Batrachochytrium salamandrivorans suggests high invasion potential and biodiversity risk
Nature Communications (2023)
-
Host–multiparasite interactions in amphibians: a review
Parasites & Vectors (2021)
-
Plethodontid salamanders show variable disease dynamics in response to Batrachochytrium salamandrivorans chytridiomycosis
Biological Invasions (2021)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.