Abstract
Systemic lupus erythematosus (SLE) might increase deep neck infection (DNI) risk, but evidence supporting this hypothesis is limited. In this retrospective follow-up study, the SLE–DNI association was investigated using data from the Registry for Catastrophic Illness Patients, which is a subset of the Taiwan National Health Insurance Research Database. All patients newly diagnosed as having SLE in 1997–2011 were identified, and every SLE patient was individually matched to four patients without SLE according to sex, age, and socioeconomic status. The study outcome was DNI occurrence. DNI treatment modalities and prognoses in SLE and non-SLE patients, along with the association of steroid dose with DNI risk, were also studied. In total, 17,426 SLE and 69,704 non-SLE patients were enrolled. Cumulative DNI incidence was significantly higher in the SLE cohort than in the non-SLE cohort (p < 0.001). The Cox regression model demonstrated that SLE significantly increased DNI risk (hazard ratio: 4.70; 95% confidence interval: 3.50–6.32, p < 0.001). Moreover, in the sensitivity and subgroup analyses, the effect of SLE on DNI was stable. Relatively few SLE–DNI patients received surgical interventions (15.6% vs. 28.6%, p = 0.033). The between-group differences in tracheostomy use and hospitalisation duration were nonsignificant. In SLE patients, high steroid doses significantly increased DNI incidence (≥3 vs. <3 mg/day = 2.21% vs. 0.52%, p < 0.001). This is the first study demonstrating that SLE increases DNI risk by approximately five times and that high steroid dose increases DNI incidence in SLE patients.
Similar content being viewed by others
Introduction
The prevalent infectious disease deep neck infection (DNI) is typically encountered in emergency departments. Patients with DNI typically require intensive care and aggressive treatment. DNI has the likelihood to be life threatening, notably in systemic disease patients and elderly individuals1,2,3. Immunocompromised patients do not show usual symptoms of DNI, making its early diagnosis difficult, possibly increasing complications and mortality1,3,4,5. Therefore, investigating the influence of immunosuppressing diseases on DNI is important.
Systemic lupus erythematosus (SLE) renders its affected patients vulnerable to infection; in addition, in such patients undergoing dialysis, infection is a notable cause of mortality6,7,8,9. SLE activity itself and long-term usage of immunosuppressants are considered the two main causes for infection susceptibility6,10. In their case series of 130 patients with DNI, Yang et al.11 reported two cases of DNI in patients with SLE under steroid therapy. However, the influence of SLE on DNI was not investigated in depth. In addition, the association between the duration of SLE, steroid dosage, and DNI risk remains unknown. We therefore conducted this real-world study with the primary purpose of probing the influence exerted by SLE on DNI incidence, treatment, and prognosis.
Methods
Data source
As of 2018, Taiwan’s well-known National Health Insurance covered approximately 99.6% of the country’s residents12,13. The National Health Insurance Research Database (NHIRD) contains the entirety of NHI beneficiaries’ medical claims data; these data include information related to disease diagnoses made at the time of clinical visits and hospitalisation, examinations received, drugs and doses prescribed, payments made, procedures and surgeries received, locations of residence, and income levels—all generated during insurance reimbursement in electronic format13,14. Diagnoses recorded in the NHIRD were made on the basis of International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes14,15.
Before release, the data are anonymised. This therefore obviated the necessity of obtaining participants’ informed consent for this study. Because of the anonymity of the beneficiaries’ information, our executed study neither violated the participants’ privacy nor negatively influenced their welfare13,15. Chang Gung Memorial Hospital’s Institutional Review Board ratified our study (IRB No.: 201601249B1), with the executed study methods conforming to approved guidelines as well as regulations.
Study cohort
NHIRD lists SLE under the “catastrophic illness” category. The Taiwanese government certifies SLE patients through a process that entails closely assessing medical records in addition to pathological and serological reports supplied by medical professionals1,3. Subsequently, the patients are included in the Registry for Catastrophic Illness Patients (RFCIP) and are entitled to substantial discounts on medical expenses. This confirms the reliability and accuracy of SLE diagnosis received by the enrolled patients.
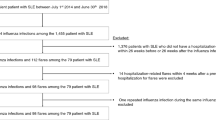
From the Taiwan RFCIP, we retrieved data of patients newly diagnosed as having SLE for the period from January 1997 to December 2011 (Fig. 1). To make sure that we had a 2-year follow-up period at minimum, we disregarded patients receiving an SLE diagnoses after 2011. We employed ICD-9-CM code 710 associated with SLE, as defined in RFCIP16. We also disregarded in this study patients receiving a DNI diagnosis prior to receiving their SLE diagnosis.
Study and comparison cohort enrolment process. Abbreviations: SLE, systemic lupus erythematosus; RFCIP, Registry for Catastrophic Illness Patients; LHID2000, Longitudinal Health Insurance Database 2000; DM, diabetes mellitus; DNI, deep neck infection; ICD-9, International Classification of Diseases, Ninth Revision.
Comparison cohort
From the Longitudinal Health Insurance Database 2000 (LHID2000), which is an NHIRD subset consisting of data of 1,000,000 insurance beneficiaries randomly selected from all beneficiaries in 2000, we collected data to establish our comparison cohort15,17. The National Health Research Institutes has published reports1,3,15 revealing no significant disparity in healthcare costs or sex or age distribution between the sample group derived from LHID2000 and all beneficiaries in the NHIRD. Several population-based studies have employed LHID20001,3,12,13,14,15. Here, our established comparison cohort contained patients without SLE or other systemic autoimmune diseases [based on these ICD-9-CM codes: 443.1 (Buerger disease), 446.0 (polyarteritis nodosa), 446.2 (hypersensitivity angiitis), 446.5 (giant cell arteritis), 446.7 (Takayasu disease), 696.0 (psoriatic arthropathy), 696.1 (psoriasis), 710.4 (polymyositis), and 714.0–714.4 (rheumatoid arthritis)].
Matching process
With four randomly selected non-SLE patients from LHID2000, we matched each patient with SLE according to diabetes mellitus (DM), income level, age, urbanisation level, and sex. For our included SLE patients, we considered the index date to be the date on which they were registered in the RFCIP, and for the matched non-SLE patients, we considered it to be the same date as that of their matched SLE patient.
Main outcome: DNI incidence
Here, DNI incidence was the main outcome. We defined such incidence to be any hospitalisation for the infections outlined as follows: parapharyngeal abscess (ICD-9-CM code: 478.22), cellulitis and abscess of oral soft tissues (Ludwig angina; ICD-9-CM code: 528.3), cellulitis and abscess of neck (ICD-9-CM code: 682.1), and retropharyngeal abscess (ICD-9-CM code: 478.24)1,3,5. We defined the follow-up period as that spanning from the index date to the DNI diagnosis date or date of death or 31 December 2013.
Comorbidities
Several diseases that can lead to an immunocompromised status can be DNI risk factors; these include chronic kidney disease (CKD), DM, and liver cirrhosis (LC)1,3,4,18. In addition, tonsillectomy is confirmed a DNI risk factor19. Therefore, both our cohorts were evaluated for these comorbidities. The comorbidities were included if their ICD-9-CM codes were noted in the claims data at least once for inpatients or at least thrice for outpatients; thus, following ICD-9-CM codes were included: DM (250), hypertension (HTN; 401–405), CKD (403, 404, 585, and 586), cerebrovascular accident (CVA; 430–438), LC (571.2 and 571.5–571.6), and coronary artery disease (CAD; 410–414)1,3,13,14,15,17,20.
Therapeutic modalities
We subcategorized our included patients into the following groups according to the therapeutic modalities applied to them: “surgical” group, comprising patients undergoing surgical intervention; and “nonsurgical” group, comprising patients receiving antibiotic or abscess aspiration without surgery1,3.
Prognosis evaluation
We analysed prognosis using the hospitalisation duration, intensive care unit (ICU) admission, tracheostomy performance, and mediastinal complications—all defined in accordance with ICD-9-CM codes for mediastinitis (510, 513, and 519.2) or on the basis of whether patients received mediastinal surgery during hospitalisation1,3. For both cohorts, we investigated mortality (death in the course of DNI treatment) and mortality related to mediastinitis (death in the course of DNI treatment along with a mediastinitis diagnosis)1,3.
Association of DNI occurrence with steroid dose for SLE therapy
SLE is typically treated using steroids with and without immunomodulators6. During the acute or unstable phase of SLE, high doses of steroids are administered, whereas in its chronic or stable stage, low doses of steroids are prescribed to control disease activities and prevent related complications. Chang et al.6 reported an average dose of 3 mg/day of prednisolone or equivalent to be the threshold for defining high or low doses of steroids in SLE patients. Therefore, we divided our SLE patients into two groups based on their average daily dose of prednisolone or equivalent during the period spanning between the index date and the conclusion of their follow-up.
Statistical analysis
To compare the SLE and non-SLE cohorts’ demographic characteristics and comorbidities, we executed the unpaired Student t and Pearson chi-square tests for continuous and categorical variables, respectively. In the univariate analysis executed in this study, control variables constituted the covariates, namely urbanisation level, sex, comorbidities (CAD, LC, HTN, DM, CVA, and CKD), age, and income level. In the multivariate analysis implemented in the study, we included only variables whose p values were determined to be <0.1. Through the execution of Kaplan–Meier analysis, we could assess the cumulative incidence in the two cohorts; determined differences through the use of a two-tailed log-rank test. Next, we measured the hazard ratios (HRs) along with the corresponding 95% confidence intervals (CIs) of the incidence of DNI in the SLE and non-SLE cohorts by using multivariable Cox proportional hazard regression models. Moreover, we executed subgroup analysis and sensitivity testing to assess the stability of the SLE effect on DNI. We executed the entirety of the analysis procedures on SAS (version 9.4; SAS Institute, Cary, NC, USA), with statistical significance level being set to p < 0.05.
Results
The sociodemographic characteristics, DNI incidence, and comorbidities in the SLE and non-SLE cohorts are presented in Table 1. In total, 17,426 SLE cases and 69,704 comparison cases were included. We observed the non-SLE cohort to exhibit a significantly lower CAD, LC, HTN, CVA, and CKD prevalence than did the SLE cohort (Table 1). Of all SLE and non-SLE patients, DNI was noted in 96 (incidence rate, 60 per 100,000 person-years; mean follow-up period, 9.18 ± 4.69 years) and 91 (incidence rate, 13.1 per 100,000 person-years; mean follow-up period, 10.0 ± 4.37 years), respectively. Thus, DNI incidence was determined to be significantly higher in the SLE cohort (p < 0.001). The mean duration from SLE diagnosis to DNI occurrence was 5.4 ± 4.2 years. Table 2 presents overall DNI incidence and that during <1, 1–5, and >5 years of follow-up in the two cohorts. The overall individual incidence rate ratio (IRR) of SLE patients compared with non-SLE patients was 4.59 (95% CI: 3.45–6.12); moreover, at <1, 1–5, and >5 years of follow-up, IRRs (95% CIs) were 7.66 (3.25–18.07), 6.06 (3.74–9.82), and 3.35 (2.24–5.02), respectively (all p < 0.001).
The results obtained from the Kaplan–Meier analysis executed in this study revealed the cumulative DNI incidence over the observation period (1997–2013) in the two cohorts. Moreover, log-rank analysis results indicated the SLE cohort to exhibit a significantly higher DNI incidence (p < 0.001; Fig. 2). According to the results of the Cox proportional hazard regression executed in this study, the crude HRs and HRs adjusted for urbanisation level, sex, DM, income level, and age were obtained for both groups. DNI risk was 4.7-fold (95% CI: 3.50–6.32) greater in the SLE patients cohort when compared with the non-SLE cohort (p < 0.001; Table 3). The results obtained from the sensitivity analysis, in which a selected covariate was added to the main model, revealed that the effect of SLE on DNI was considerable and stable, and its significance was sustained in all subgroups, except for the LC, CKD, and CVA subgroups, according to the subgroup analysis results. Moreover, in the tonsillectomy subgroup, which was extremely small (n = 4 in study cohort and 22 in comparison cohort), DNI risk could not be calculated because no DNI occurrence was noted.
The therapeutic modalities for DNI employed in the two cohorts were antibiotics only or antibiotics plus abscess aspiration (nonsurgical group) or surgical drainage (surgical group); these modalities, along with other factors, including tracheostomy performance, hospitalisation duration, ICU admission, mediastinal complications, and mortality, are presented in Table 4. Regarding the proportion of treatment, SLE–DNI patients received less surgical intervention (SLE vs. non-SLE = 15.6% vs. 28.6%, p = 0.033). The between-group differences in tracheostomy performance (SLE vs. non-SLE = 3.1% vs. 3.3%, p = 0.947), hospitalisation duration (SLE vs. non-SLE = 12.86 ± 18.26 vs. 10.12 ± 22.17 days, p = 0.356), and ICU admission (SLE vs. non-SLE = 5.2% vs. 9.9%, p = 0.224) were all nonsignificant. The only two cases of mortality among all of the patients considered herein occurred in the non-SLE–DNI patients.
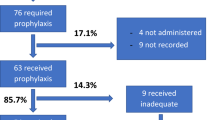
By using the data presented in Fig. 3, we analysed incidence of DNI in SLE patients administered high (≥3 mg/day) or low (<3 mg/day) doses of steroids. Of the 183 patients administered high steroid doses, 6 developed DNIs (2.21%)—significantly higher than that in patients administered low steroid doses (90 in 17,243 patients, 0.52%; p < 0.001).
Discussion
Our executed nationwide population-based study entailed the use of data from a real-world database. This is the first study to be executed on the influence exerted on DNI occurrence and prognosis by SLE. The derived results confirm SLE to be a definite DNI risk factor and DNI risk to be approximately five times higher in SLE patients than in non-SLE patients.
Studies have reported that SLE can increase infection and mortality risks, particularly in patients on a high steroid or immunosuppressant dose, with the respiratory tract being the most commonly involved, followed by the bloodstream, and bacteria being the most common causative agent, followed by viruses and fungi21,22,23. Moreover, infection rate is highest in the initial stages after SLE diagnosis, particularly the initial 5 years22. An SLE project and a large-scale case series revealed that infection accounted for the first cause of mortality within the initial 5 years after disease onset24,25. In the current study, DNI developing after SLE had a mean duration of 5.4 years. In addition, the IRRs for SLE–DNI compared with the comparison cohort over <1, 1–5 and >5 years of follow-up are presented in Table 2. IRR was highest for DNI diagnosis at <1 year of follow-up (7.66), followed by that at 1–5 (6.06) and >5 (3.35) years of follow-up.
Acquired deficiency of regulatory T cells for self-immunologic intolerance is thought to be an aspect of SLE pathogenesis26,27. Sjögren syndrome concomitant with SLE is common, and the immune defences of the oral cavity can be attenuated by xerostomia28. Therefore, oral infections, including periodontitis and tooth decay, are typically latent in SLE patients. In addition, steroids are the main medications administered in SLE therapy29, and they may cause immunosuppression, thus making patients susceptible to infection7,8,9, particularly patients administered high doses6,9. Based on the preceding evidence, the aforementioned factors could constitute the etiologies for the higher incidence of DNI in SLE patients.
Surgical debridement accounts for 20–80% of all therapies for DNI1,3,4,30,31,32,33,34. In our study, 15.6% of SLE–DNI patients and 28.6% of non-SLE–DNI patients received surgical treatment. The ratio of DNI patients who underwent surgical drainage is lower in this real-world study than the ratios in previous studies in which patients from tertiary medical centres were enrolled4,11,32,34. This study was based on a nationwide population-based database that includes data from primary to tertiary hospitals as well as those of patients with low DNI severity. This result may provide a complete spectrum of DNI treatment and prognosis and is consistent with the results of previous DNI-relevant population-based studies1,3. There were between-group differences in tracheostomy performance, hospitalisation duration, and ICU admission between the two cohorts, implying that DNI severity and prognosis in patients with SLE do not differ significantly from those in non-SLE–DNI patients.
In clinical applications, steroids may be administered to patients with acute or unstable SLE ether alone at high doses or in combination with immunosuppressants6,9. High doses of steroids, concomitant immunosuppressants, and high lupus activity would attenuate immune defences and engender more severe infection. We used the threshold given by Chang et al.6 (i.e. average daily dose = 3 mg of prednisolone or equivalent) to evaluate the incidence of DNI in SLE patients. The results indicate that high average daily doses of steroids (≥3 mg of prednisolone or equivalent) increased infection and mortality rates compared with low average daily doses of steroids. Danza et al.9 found that SLE patients treated with a daily dose of more than 7.5 mg of methylprednisolone were at an increased infection risk. In our study, SLE patients who were administered high doses of steroids exhibited significantly higher rates of DNI incidence (high dose: ≥3 mg/day vs. low dose: <3 mg/day = 2.21% vs. 0.52%, p < 0.001), thus corroborating previous findings9.
The strengths our study include the large sample size (17,426 patients with SLE, representing a nationwide spectrum) and long follow-up period (9.84 ± 4.43 years). However, the following are the few limitations of our population-based study: First, medical images such as computed tomography and magnetic resonance imaging were not available; hence, we could not confirm the extent of DNI and the size of the abscess. Second, blood- and pus-culture data could not be obtained from the NHIRD; we thus could not discern the definite bacterial spectra or drug sensitivities of our patients with DNI. Third, the definite causes of death could not be obtained from the NHIRD; therefore, as an alternative to DNI-specific mortality, we investigated 3-month mortality. Finally, because this retrospective study used claims data, several factors, including patients’ clinical presentation and treatment course, physical examination findings, and laboratory study results, could not be evaluated in detail. Additional studies elucidating the causal relationship of SLE with DNI as well as the related treatment outcomes are warranted.
Conclusions
This real-world study is the first to investigate SLE and the incidence, treatment, and prognosis of DNI. Our findings strongly support the assertion that SLE is a DNI risk factor. Patients with SLE under high-dose steroid treatment demonstrated higher DNI incidence rates than did those under low-dose steroid treatment. Fewer SLE–DNI patients were subjected to surgical treatment compared with the non-SLE–DNI patients. Finally, the differences in mortality, tracheostomy performance, ICU admission, and hospitalisation duration between SLE–DNI and non-SLE–DNI patients were nonsignificant.
Data availability
The datasets generated or analysed in the current study can be accessed from the Taiwan National Health Insurance Research Database repository (https://nhird.nhri.org.tw/en/How_to_cite_us.html).
References
Chang, G.-H. et al. High Risk of Deep Neck Infection in Patients with Type 1 Diabetes Mellitus: A Nationwide Population-Based Cohort Study. Journal of Clinical Medicine 7, 385 (2018).
Santos Gorjon, P. et al. Deep neck infection. Review of 286 cases. Acta Otorrinolaringologica Espanola 63, 31–41 (2012).
Chang, G. H. et al. End-stage renal disease: a risk factor of deep neck infection - a nationwide follow-up study in Taiwan. BMC Infectious Diseases 17, 424 (2017).
Huang, T. T. et al. Deep neck infection: analysis of 185 cases. Head & Neck 26, 854–860 (2004).
Liu, C. F. et al. Increased risk of deep neck infection among HIV-infected patients in the era of highly active antiretroviral therapy–a population-based follow-up study. BMC Infectious Diseases 13, 183 (2013).
Chang, Y. S. et al. Survival analysis in systemic lupus erythematosus patients on maintenance dialysis: a nationwide population-based study in Taiwan. Rheumatology (Oxford, England) 52, 166–172 (2013).
Wang, L. C., Yang, Y. H., Lu, M. Y. & Chiang, B. L. Retrospective analysis of mortality and morbidity of pediatric systemic lupus erythematosus in the past two decades. J. Microbiol. Immunol. Infect. 36, 203–208 (2003).
Chan, P. C., Yu, C. H., Yeh, K. W., Horng, J. T. & Huang, J. L. Comorbidities of pediatric systemic lupus erythematosus: A 6-year nationwide population-based study. J Microbiol Immunol Infect 49, 257–263 (2016).
Danza, A. & Ruiz-Irastorza, G. Infection risk in systemic lupus erythematosus patients: susceptibility factors and preventive strategies. Lupus 22, 1286–1294 (2013).
Stahn, C. & Buttgereit, F. Genomic and nongenomic effects of glucocorticoids. Nat Clin Pract Rheumatol 4, 525–533 (2008).
Yang, W. et al. Deep Neck Infection: A Review of 130 Cases in Southern China. Medicine 94, e994 (2015).
Tsai, Y. T. et al. Risk of acute epiglottitis in patients with preexisting diabetes mellitus: A population-based case-control study. PLoS One. 13, e0199036. doi:10.0191371/journal.pone.0199036. eCollection 0192018 (2018).
Chang, G.-H. et al. Real-World Database Examining the Association between Sjögren’s Syndrome and Chronic Rhinosinusitis. Journal of Clinical Medicine 8, 155 (2019).
Tsai, M. S. et al. Unilateral Vocal Fold Paralysis and Risk of Pneumonia: A Nationwide Population-Based Cohort Study. Otolaryngology–Head and Neck Surgery: Official Journal of American Academy of Otolaryngology-Head and Neck Surgery, 194599818756285 (2018).
Tsai, M. S. et al. Sleep apnea and risk of vertigo: A nationwide population-based cohort study. The Laryngoscope 128, 763–768 (2018).
Yen, Y. F. et al. Incidence of autoimmune diseases in a nationwide HIV/AIDS patient cohort in Taiwan, 2000–2012. Annals of the Rheumatic Diseases 76, 661–665 (2016).
Tsai, M. S. et al. Chang Gung Research Database: A multi-institutional database consisting of original medical records. Biomed J 40, 263–269 (2017).
Tsai, M. S. et al. The Association Between Decompensated Liver Cirrhosis and Deep Neck Infection: Real-World Evidence. Int J Environ Res Public Health 16 (2019).
Wang, Y. P., Wang, M. C., Lin, H. C., Lee, K. S. & Chou, P. Tonsillectomy and the risk for deep neck infection-a nationwide cohort study. PloS one 10, e0117535 (2015).
Chung, W. S. et al. Rheumatoid arthritis and risk of acute myocardial infarction–a nationwide retrospective cohort study. Int J Cardiol 168, 4750–4754 (2013).
Shi, L. H. et al. Risk of systemic lupus erythematosus in patients with human papillomavirus infection: a population-based retrospective cohort study. Lupus 27, 2279–2283 (2018).
Zhan, Z. et al. Hospital-acquired infection in patients with systemic lupus erythematosus: a case-control study in a southern Chinese population. Clin Rheumatol 37, 709–717 (2018).
Tsai, W. P. et al. Cytomegalovirus infection causes morbidity and mortality in patients with autoimmune diseases, particularly systemic lupus: in a Chinese population in Taiwan. Rheumatology International 32, 2901–2908 (2012).
Cervera, R. et al. Systemic lupus erythematosus in Europe at the change of the millennium: lessons from the “Euro-Lupus Project”. Autoimmun Rev 5, 180–186 (2006).
Fei, Y. et al. Death causes and pathogens analysis of systemic lupus erythematosus during the past 26 years. Clin Rheumatol 33, 57–63 (2014).
Humrich, J. Y. & Riemekasten, G. Restoring regulation - IL-2 therapy in systemic lupus erythematosus. Expert Review of Clinical Immunology 12, 1153–1160 (2016).
Ohl, K. & Tenbrock, K. Regulatory T-cells in systemic lupus erythematosus. IL-2 is decisive for loss of tolerance. Zeitschrift fur Rheumatologie 75, 253–264 (2016).
Christensen, L. B., Petersen, P. E., Thorn, J. J. & Schiodt, M. Dental caries and dental health behavior of patients with primary Sjogren syndrome. Acta odontologica Scandinavica 59, 116–120 (2001).
Chang, C. M. et al. Integrative therapy decreases the risk of lupus nephritis in patients with systemic lupus erythematosus: A population-based retrospective cohort study. Journal of Ethnopharmacology 196, 201–212 (2017).
Bakir, S. et al. Deep neck space infections: a retrospective review of 173 cases. American Journal of Otolaryngology 33, 56–63 (2012).
Boscolo-Rizzo, P., Marchiori, C., Montolli, F., Vaglia, A. & Da Mosto, M. C. Deep neck infections: a constant challenge. ORL; Journal for Oto-Rhino-Laryngology and its Related Specialties 68, 259–265 (2006).
Bottin, R. et al. Deep neck infection: a present-day complication. A retrospective review of 83 cases (1998–2001). European Archives of Oto-Rhino-Laryngology: Official Journal of the European Federation of Oto-Rhino-Laryngological Societies (EUFOS): Affiliated With the German Society for Oto-Rhino-Laryngology - Head and Neck Surgery 260, 576–579 (2003).
Dolezalova, H., Zemek, J. & Tucek, L. Deep Neck infections of Odontogenic Origin and Their Clinical Significance. A Retrospective Study from Hradec Kralove, Czech Republic. Acta Medica (Hradec Kralove) 58, 86–91 (2015).
Eftekharian, A., Roozbahany, N. A., Vaezeafshar, R. & Narimani, N. Deep neck infections: a retrospective review of 112 cases. European Archives of Oto-Rhino-Laryngology: Official Journal of the European Federation of Oto-Rhino-Laryngological Societies (EUFOS): Affiliated With the German Society for Oto-Rhino-Laryngology - Head and Neck Surgery 266, 273–277 (2009).
Acknowledgements
The research was supported by Chang Gung Memorial Hospital, Taiwan, grants CMRPG6J0331, CFRPG6J0061, CGRPG6G0021, and CGRPG6J0031. The authors thank the Health Information and Epidemiology Laboratory of Chiayi Chang Gung Memorial Hospital (CLRPG6G0041) for their comments and assistance with data analysis. This study was based on the National Health Insurance Research Database provided by the Central Bureau of National Health Insurance, the Department of Health, and managed by the National Health Research Institutes. This manuscript was edited by Wallace Academic Editing.
Author information
Authors and Affiliations
Contributions
Geng-He Chang, Yi-Cheng Su, and Ko-Ming Lin wrote the main manuscript text. Chia-Yen Liu, Yao-Hsu Yang, and Pey-Jium Chang designed the study. Meng-Hung Lin, Chuan-Pin Lee, and Cheng-Ming Hsu analysed data and prepared tables. Yao-Te Tsai and Ching-Yuan Wu prepared figures. Ming-Shao Tsai supervised the study. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Chang, GH., Su, YC., Lin, KM. et al. Deep Neck Infection in Systemic Lupus Erythematosus Patients: Real-World Evidence. Sci Rep 10, 4133 (2020). https://doi.org/10.1038/s41598-020-61049-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-61049-4
This article is cited by
-
Periodontitis and the subsequent risk of glaucoma: results from the real-world practice
Scientific Reports (2020)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.