Abstract
Cortical lesions (CLs) have a low prevalence and are associated with physical disabilities in Japanese patients with multiple sclerosis (MS). However, the contribution of CLs to cognitive impairment remains unclear in Asian MS. Sixty-one prospectively enrolled MS patients underwent three-dimensional double inversion recovery MR imaging, the Brief Repeatable Battery of Neuropsychological Tests (BRB-N), the Apathy Scale (AS), the Fatigue Questionnaire (FQ), and the Hospital Anxiety and Depression Scale (HADS) within a 1-week period. The cognitive impairment index (CII) score was calculated to measure patients’ overall cognitive impairment. MS patients with CLs had poorer scores than those without CLs in most BRB-N tests, but scored comparably in the FQ, AS, and HADS. The number of CLs correlated negatively with all BRB-N test scores and positively with total CII scores. Leukocortical lesions were more extensively associated with cognitive dysfunction in various domains than intracortical lesions. Stepwise multiple regression analysis revealed that potential confounding factors for the highest quartile of CII score were the number of CLs (odds ratio 2.38, p = 0.0070) and the Expanded Disability Severity Scale score (odds ratio 2.13, p = 0.0003). Our results demonstrate that the presence and number of CLs are robustly associated with cognitive dysfunction in Asian MS patients.
Similar content being viewed by others
Introduction
Multiple sclerosis (MS) is an autoimmune demyelinating disease of the central nervous system that affects not only motor, but also cognitive and psychiatric functions. Cognitive impairment has been reported in 43–70% of MS patients1,2,3 and increases the risk of loss of employment or reduction in vocational duties4. In MS, information processing speed, visual memory, visuospatial perception, and working memory are particularly impaired from the early phase of the disease1. No large-scale epidemiological studies have investigated the prevalence of cognitive impairment among Japanese patients with MS. However, in a small case series, attention deficits characterized by slow automatic information processing, a very early sign of cognitive impairment in MS, were found in 14 of 22 (66.7%) patients5. Several studies have also reported significantly lower scores in the cognition test batteries, including the Brief Repeatable Battery of Neuropsychological Tests (BRB-N) used in the present study, among Japanese MS patients compared with healthy controls6,7,8,9.
The advent of new magnetic resonance imaging (MR) sequences, such as double inversion recovery (DIR) and phase-sensitive inversion recovery, have facilitated the identification of cortical lesions (CLs) in patients with MS, even in the early phase of the disease10. In Caucasians, there are several lines of evidence demonstrating that CLs contribute to cognitive dysfunction in patients with MS11,12,13,14,15. Cognitively impaired relapsing-remitting MS (RRMS) patients have higher numbers and greater volumes of intracortical lesions (ICLs) compared with cognitively normal MS patients11. Prospective studies have shown that CLs accumulate over time in association with cognitive decline12,13. One study reported that leukocortical lesions (LCLs) affecting both grey matter (GM) and white matter (WM) make a greater contribution to cognitive impairment than ICLs in MS13. Recent 7-tesla MRI studies have reported that LCLs are more extensively associated with various domains of cognitive impairment than ICLs14,15.
Despite the serious impact of cognitive decline on the quality of life of patients with MS, only a few studies have investigated cognitive impairment and CLs in Asian patients with MS16,17, who present features distinct from those of European patients with MS18,19. We recently reported that CLs were found at a relatively low frequency (29.7%) on DIR imaging of 3-tesla MRI among Japanese patients with RRMS16 compared with that among Caucasian patients with RRMS (≥ 60%)20,21,22,23. Moreover, the number of CLs was significantly associated with motor disability in Japanese patients16. Furthermore, because two human leukocyte antigen (HLA) risk alleles, HLA–DRB1*15:01 and HLA–DRB1*04:05, are prevalent in Japanese MS patients24, we also studied the influence of these HLA alleles on CLs and found that HLA–DRB1*15:01 increases CLs, whereas HLA–DRB1*04:05 decreases CLs16. This finding is consistent with the result from a previous pathological study, which found that HLA–DRB1*15:01 was associated with greater cortical inflammation in autopsied MS materials25, suggesting an involvement of HLA class II molecules in CL development26,27. Another small-scale study of Japanese MS patients that assessed cognitive function reported that the attention of 13 CL-positive patients was significantly worse than that of six CL-negative patients; however, the study did not classify CLs into ICLs and LCLs and did not evaluate the relationship between CL quantity and cognitive function17.
Therefore, it is possible that despite the lower quantity of CLs in Japanese MS patients compared with Caucasian MS patients, CLs may have similar effects on cognitive function in Japanese and Caucasian MS patients. The effects of different CL subtypes, particularly ICLs and LCLs, on cognitive dysfunction remains to be elucidated in Asian patients, including Japanese patients. Therefore, we aimed to elucidate the effects of CLs on cognitive functions by using a comprehensive, prospective assessment of these functions, combined with DIR neuroimaging. In particular, our focus was the differential effects of ICLs and LCLs on cognition and the association between the HLA–DRB1 genotype and cognitive impairment in Japanese patients with MS.
Results
Demographics
The participants consisted of 61 MS patients in the remission phase (42 RRMS and 19 secondary progressive MS [SPMS]) (Table 1). Mean disease duration was 13.5 ± 10.5 years. CLs, ICLs, and LCLs were observed in 27 (44.3%), 13 (21.3%), and 25 patients (41.0%), respectively. Among the 27 MS patients with CLs, 11 (40.7%) had both LCLs and ICLs, 14 (51.9%) had only LCLs, and two (7.4%) had only ICLs. The numbers of CLs, ICLs, and LCLs (mean ± SD) were 1.31 ± 2.54, 0.31 ± 0.65, and 1.01 ± 2.11, respectively (Table 1).
Neuropsychological assessment of MS patients with and without CLs
We first compared our MS patients with age- and sex-matched healthy controls previously subjected to BRB-N who were included in our previous study6. Overall, MS patients showed significantly lower scores than controls in the following tests (Supplementary Table 1): SRT-LTS (p = 0.0367), SPART (p < 0.0001), SPART-D (p = 0.0169), SDMT (p < 0.0001), PASAT-3 (p < 0.0001), PASAT-2 (p < 0.0001), and the WLG test (p < 0.0001).
Japanese MS patients with CLs had significantly lower scores than those without CLs in the following tests (Table 2): SRT-LTS (p = 0.0201), SPART (p = 0.0335), SPART-D (p = 0.0082), SDMT (p = 0.0080), PASAT-3 (p = 0.0033), and PASAT-2 (p = 0.0042). Similarly, CII scores were significantly poorer in MS patients with CLs than in those without CLs (p = 0.0019). However, there were no significant differences in AS, FQ, HADS-A, or HADS-D scores between MS patients with and without CLs.
MS patients with ICLs had significantly lower scores on the SPART (p = 0.0043), SPART-D (p = 0.0325), PASAT-3 (p = 0.0117), PASAT-2 (p = 0.0075), and WLG test (p = 0.0126) and higher CII scores (p = 0.0065) than those without ICLs (Table 2). MS patients with LCLs had significantly lower scores on the SRT-LTS (p = 0.0262), SPART (p = 0.0179), SPART-D (p = 0.0072), SDMT (p = 0.0077), PASAT-3 (p = 0.0020), and PASAT-2 (p = 0.0084) and higher CII scores (p = 0.0033) than those without LCLs (Table 2). Subsequently, among MS patients with CLs, we compared patients who had ICLs with those who did not have ICLs. MS patients with ICLs had significantly lower SPART scores (mean ± SD: 15.7 ± 5.1 vs. 20.4 ± 3.7; p = 0.0315) and WLG scores (18.5 ± 7.4 vs. 23.9 ± 6.3; p = 0.0462) than those with LCLs but lacking ICLs (Supplementary Fig. 1).
Correlations between neuropsychological findings and clinical parameters
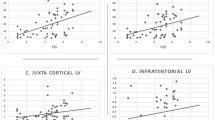
We next examined the correlations between the results of neuropsychological examinations and the following variables: age at examination, disease duration, EDSS score, the number of CLs, the number of ICLs, and the number of LCLs. All tests of BRB-N were negatively correlated with age at examination, disease duration, EDSS score, and the number of CLs, except for the WLG score with age at examination (Fig. 1A). CII scores were positively correlated with age at examination, disease duration, EDSS score, number of CLs, number of ICLs, and number of LCLs. AS scores were positively correlated only with the EDSS score (ρ = 0.27, p = 0.0329), whereas FQ scores were correlated with age at examination and with the EDSS score (ρ = 0.43, p = 0.0006 and ρ = 0.35, p = 0.0061, respectively). HADS-A and HADS-D scores were weakly associated with age at examination (ρ = 0.25, p = 0.0482 and ρ = 0.26, p = 0.0418, respectively). The associations of CII scores with EDSS scores and with the number of CLs were the most robust among all the comparisons (ρ = 0.58, p < 0.0001 and ρ = 0.48, p < 0.0001, respectively) (Fig. 1B,C).
Correlation between neuropsychological test results and clinical parameters in MS patients. (A) Heatmap displays Spearman correlation coefficients between neuropsychological test results and clinical parameters. * p < 0.05, ** p < 0.01, *** p < 0.001. (B) Correlation between CII and EDSS scores. (C) Correlation between CII scores and the number of CLs. AS, Apathy Scale; CII, Cognitive Impairment Index; CLs, cortical lesions; EDSS, Expanded Disability Status Scale; FQ, Fatigue Questionnaire; HADS, Hospital Anxiety and Depression Scale; HADS-A, anxiety score of the HADS; HADS-D, depression score of the HADS; ICLs, intracortical lesions; LCLs, leukocortical lesions; MS, multiple sclerosis; NS, not significant; PASAT, Paced Auditory Serial Addition Test; PASAT-2, 2-s version of the PASAT; PASAT-3, 3-s version of the PASAT; SDMT, Symbol Digit Modalities Test; SPART, 10/36-Spatial Recall Test; SPART-D, delayed recall of the SPART; SRT, Selective Reminding Test; SRT-LTS, long-term storage of the SRT; SRT-CLTR, consistent long-term retrieval of the SRT; WLG, word list generation test.
Comparison of neuropsychological assessment scores between carriers and non-carriers of HLA–DRB1*15:01 and HLA–DRB1*04:05
Neuropsychological status was compared between patients with and without the HLA–DRB1*15:01 or HLA–DRB1*04:05 alleles (Supplementary Table 2). There were no significant differences in the neuropsychological assessment scores between the carriers and the non-carriers of each of these alleles.
Logistic regression analysis for potential confounders of effects on cognitive dysfunction
Univariate and multivariate regression analyses were performed to elucidate the factors contributing to poor cognitive function in Japanese MS patients (Table 3). Univariate regression analysis showed that age at examination, disease duration, clinical subtype of the disease (RRMS versus SPMS), EDSS score, and number of CLs, but not HLA–DRB1*15:01 or HLA–DRB1*04:05, were significantly associated with the highest quartile of CII score. With forward stepwise selection, the EDSS score and the number of CLs were included in the multivariate regression analysis, which demonstrated that both EDSS score and number of CLs were independent predictors of the highest quartile of CII scores in Japanese patients with MS (EDSS score: odds ratio 2.13, p = 0.0003; number of CLs: odds ratio 2.38, p = 0.0070).
Discussion
In the present study, SDMT, PASAT-2, and PASAT-3 scores were significantly lower in our MS patients compared with controls, indicating impairments of attention, information processing, and working memory. Additionally, lower SPART and SPART-D scores indicated visual memory impairment in Japanese MS patients, an aspect of cognition that is also commonly affected even during the early phase of the disease in Caucasian MS patients1. The lower SRT-LTS and WLG scores suggest impairment of verbal memory and verbal fluency in our MS patients, which is observed in around half of Caucasian MS patients1. In the present study, WLG score did not correlate with age. We believe this lack of correlation in part resulted from the age distribution of this cohort, which included patients from 16 to 72 years of age and lacked very elderly participants. Similarly, Niino et al. reported that WLG scores did not correlate with age in either 184 MS patients or in 163 healthy controls with a similar age distribution6. However, WLG negatively correlated with disease duration, EDSS score, and the number of CLs, ICLs, and LCLs, suggesting that verbal fluency was affected more profoundly by the disease course and disability progression of MS as well as the presence of CLs than by aging. These observations suggest the patterns of cognitive impairment in Japanese patients with MS are largely similar to those in Caucasian patients.
Although the prevalence and the number of CLs, ICLs, and LCLs were relatively low in our subjects compared with Caucasian MS patients, we found that the number of CLs in Japanese MS patients was significantly associated with all of the BRB-N tests. This result is in accord with previous studies of Caucasian MS patients9,12,13 and with an earlier study of Japanese MS patients, which reported an association between the presence of CLs and cognitive dysfunction17. The presence and number of CLs were strongly associated with the overall CII score in our study, which is also consistent with a previous study in Caucasian MS patients21. The results of multivariate regression analysis also indicate that both the number of CLs and the EDSS score are independent predictors of the most severe cognitive decline in Japanese MS patients. The presence and the number of CLs could therefore be relevant risk factors for cognitive impairment in Japanese patients with MS, even though Japanese patients have CLs less frequently than Caucasian patients.
As for the cognitive subdomains assessed, our study revealed that in Japanese MS patients, the presence and number of CLs were more significantly associated with scores in the SDMT, PASAT-3, and SPART-D than with SRT-LTS scores. This finding suggests that CLs contribute more to impairments of attention, information processing, and working and visual memory than verbal memory. A study of Caucasian MS patients also reported a more robust association of CL numbers with PASAT and SDMT scores than with SRT-LTS scores21. Therefore, CLs are more strongly related to the cognitive subdomains that are preferentially affected in the early phase of the disease1, which further suggests that CLs are an important risk factor for early cognitive impairment in MS.
Concerning the subtype of CLs, pathologically classified type I lesions correspond to LCLs, while type II–IV lesions correspond to ICLs28. However, type III subpial lesions are only detectable by 7-tesla high-resolution MRI, not conventional 3-tesla MRI14. LCLs were reported to affect total cognitive function more severely than ICLs, based on 3-tesla MRI of Caucasian MS patients13. A recent study using 7-tesla MRI demonstrated that type I CLs (LCLs) were most frequently associated with impairments in various domains of cognitive function, such as visuospatial, learning/memory, processing speed, and semantic language domains, while type III and IV CLs (ICLs) were associated with poor performance in learning/memory and semantic language domains14. In the present study, we found that LCLs in patients were more extensively associated with various domains of neuropsychological assessments than ICLs, although the effects on overall CII scores were comparable. However, ICLs, including in patients who had both ICLs and LCLs, were more significantly associated with lower scores in the SPART and WLG test than LCLs. This finding suggests that the presence of ICLs may relate to impairments of verbal and visual memory. Given the association of type III and IV CLs, which are included in the ICL category, with impairment of learning/memory and semantic language tests in Caucasian MS patients14, it is possible that ICLs may relate to impairments in somewhat distinct domains of cognitive functions from LCLs. This point should be clarified in future large-scale studies. Overall, although we could not assess type III subpial lesions by 3-tesla MRI, these results are roughly consistent with results from studies of Caucasian MS patients13,14.
In this study, we did not find any significant differences in the neuropsychological status of carriers and non-carriers of the HLA–DRB1*1501 and HLA–DRB1*04:05 alleles. Although we previously reported that HLA–DRB1*15:01 increased CLs, whereas HLA–DRB1*04:05 decreased CLs16, the MS-susceptible HLA–DRB1 genotypes did not influence the neuropsychological outcome in the present study. CLs contribute to cognitive impairment, but such an impairment could be influenced by much broader damage to brain structures. For example, cognitive dysfunction is also associated with losses of volume in subcortical structures, such as the caudate29 and the thalamus30. Therefore, although the HLA alleles for MS susceptibility can facilitate CL development, they are not so influential as to modulate cognitive decline.
There are several limitations to the present study. First, the sample size was relatively small, mainly because of the low prevalence of MS in Japan31 and the difficulties in enrolling patients prospectively to undergo both MRI and neuropsychological studies within a 1-week period in a single institution. Second, because 3-tesla MRI was used, subpial lesions could not be assessed and evaluating which CLs extended into the subcortical WM was occasionally difficult, even though two examiners independently assessed the CLs. Third, the relationship between the location of CLs and cognitive functions was not assessed because of the small number of enrolled patients; this should be investigated in future studies. Fourth, volumetric measurement of WM, GM, and T2 lesions were lacking, because the present study was initially designed to determine whether CLs imaged with 3-tesla 3D-DIR MRI might be an indicator of cognitive impairment in real-world settings in the Japanese population. Thus, such volumetric analysis should be performed in future studies to further evaluate factors contributing to cognitive dysfunction.
Nonetheless, in this study we demonstrated the contribution of CLs to overall cognitive impairment in Japanese MS patients. LCLs were more significantly associated with the impairment of cognitive domains preferentially affected by MS, including attention, information processing, and working and visual memory, while ICLs may contribute more to verbal and visual memory impairments. The presence and number of CLs could be relevant risk factors for cognitive decline in Japanese MS patients.
Materials and Methods
Participants
Sixty-one patients with MS who gave written informed consent prior to their inclusion in this study were prospectively and consecutively enrolled in the period from February 1, 2016, to May 31, 2017 (Table 1). The diagnosis of MS was based on the established criteria at that time32. All patients were carefully followed-up at a single MS centre in the district, the Department of Neurology at Kyushu University Hospital. Patients were clinically stable with no relapse at least for 1 month prior to MRI (including 3D-DIR imaging) and neuropsychological assessment, which were both performed within a 1-week period. This study was approved by the Ethics Committee of Kyushu University and was conducted according to the World Medical Association Declaration of Helsinki.
MR imaging and identification of CLs
All MRI images were obtained with a 3-tesla scanner (Achieva; Philips, Best, The Netherlands) with the following sequence parameters, as previously described16: repetition time (TR)/echo time (TE) = 5500/255–284 ms, inversion time (TI) = 450/2550 ms, echo train length (ETL) = 173, matrix size = 208 × 208, and field of view (FOV) = 250 mm × 250 mm. Lesions were identified based on consensus between two examiners, an experienced neuroradiologist (A.H.) and a neurologist (K.S.), with special attention to the recommendations made by Geurts et al.33. CLs were classified into ICLs localized in the cortical GM and LCLs encompassing both GM and WM (Fig. 2).
Examples of cortical lesions on 3-dimensional double inversion recovery (DIR) images from two patients with MS. (A–C) Arrowheads indicate an intracortical lesion that does not appear to extend into the subcortical white matter. (D–F) Arrows indicate a leukocortical lesion that involves both the grey and white matter.
Neuropsychological assessments
Participants underwent the Japanese version of BRB-N6, which comprises the following tests: the Selective Reminding Test (SRT) of verbal learning memory; the 10/36-Spatial Recall Test (SPART) of visuospatial memory and learning; the Paced Auditory Serial Addition Test (PASAT) and Symbol Digit Modalities Test (SDMT) of attention, information processing, and working memory; and the word list generation (WLG) test of verbal fluency. The battery of tests was performed in the following order: SRT, SPART, SDMT, PASAT, delayed recall of SRT (SRT-D), delayed recall of SPART (SPART-D), and WLG. These tests included the following variants: for the SRT, the long-term storage (SRT-LTS), consistent long-term retrieval (SRT-CLTR), and delayed recall (SRT-D) tests; for the SPART, the immediate recall (SPART) and delayed recall (SPART-D) tests; and for the PASAT, both the 2-s and 3-s versions (PASAT-2 and PASAT-3). Cognitive impairment index (CII) scores were computed by calculating the mean and the SD of the control data6, as previously described34. The results obtained from the controls in our previous study6 were used for comparison with the total MS patient group in this study. Apathy was assessed with the Apathy Scale (AS)35, using a translated version of the scale that has been previously validated in Japanese36. Fatigue was evaluated with the Japanese version of the Fatigue Questionnaire (FQ)37. Depression and anxiety were assessed with the Japanese version of the Hospital Anxiety and Depression Scale (HADS-A and HADS-D)38.
HLA genotyping
The genotypes of the HLA–DRB1 alleles were analysed in all patients by using hybridization between the polymerase chain reaction amplification products of the genes and the sequence-specific oligonucleotide probes, as previously described39.
Statistics
Statistical analysis was performed with JMP Pro 12.2.0 (SAS Institute, Cary, NC, USA) or GraphPad Prism 7.0d (GraphPad Software, San Diego, CA, USA). Fisher’s exact test was used to compare categorical variables, and the Wilcoxon rank-sum test was used to analyse continuous scales. Correlations among continuous scales were calculated by using Spearman’s rank correlation coefficient. To perform the regression analysis, we divided the CII scores of patients into quartiles defined by the following ranges: 0–1, 2–4, 5–9, and ≥10. Univariate and multivariate logistic regression analysis was performed to assess possible factors associated with the lowest quartile of the CII score, including sex, age at examination, disease duration, Kurtzke Expanded Disability Severity Scale (EDSS) score, number of CLs, presence of the HLA–DRB1*15:01 allele, and presence of the HLA–DRB1*04:05 allele. Given the small sample size, forward stepwise selection was performed to reduce the number of predictors incorporated into the multivariate analysis40. A p-value < 0.05 was considered statistically significant.
References
Chiaravalloti, N. D. & DeLuca, J. Cognitive impairment in multiple sclerosis. Lancet Neurol. 7, 1139–1151, https://doi.org/10.1016/S1474-4422(08)70259-X (2008).
Rao, S. M., Leo, G. J., Bernardin, L. & Unverzagt, F. Cognitive dysfunction in multiple sclerosis. I. Frequency, patterns, and prediction. Neurol. 41, 685–691 (1991).
Benedict, R. H. et al. Validity of the minimal assessment of cognitive function in multiple sclerosis (MACFIMS). J. Int. Neuropsychol. Soc. 12, 549–558 (2006).
Ruet, A. et al. Cognitive impairment, health-related quality of life and vocational status at early stages of multiple sclerosis: a 7-year longitudinal study. J. Neurol. 260, 776–784, https://doi.org/10.1007/s00415-012-6705-1 (2013).
Takeda, A. et al. Attention deficits in Japanese multiple sclerosis patients with minor brain lesion loads. Neuropsychiatr. Dis. Treat. 7, 745–751, https://doi.org/10.2147/NDT.S27447 (2011).
Niino, M. et al. Apathy/depression, but not subjective fatigue, is related with cognitive dysfunction in patients with multiple sclerosis. BMC Neurol. 14, 3, https://doi.org/10.1186/1471-2377-14-3 (2014).
Yoshii, F. et al. Cognitive impairment of Japanese multiple sclerosis patients: Follow-up study using BRB-N assessment tool. J. Neurol. Sci. 359, 323–327, https://doi.org/10.1016/j.jns.2015.11.002 (2015).
Kimura, Y. et al. A structural MRI study of cholinergic pathways and cognition in multiple sclerosis. eNeurologicalSci 8, 11–16, https://doi.org/10.1016/j.ensci.2017.06.008 (2017).
Niino, M. et al. Validation of the Brief International Cognitive Assessment for Multiple Sclerosis in Japan. Mult. Scler. J. Exp. Transl. Clin. 3, 2055217317748972, https://doi.org/10.1177/2055217317748972 (2017).
Geurts, J. J., Calabrese, M., Fisher, E. & Rudick, R. A. Measurement and clinical effect of grey matter pathology in multiple sclerosis. Lancet Neurol. 11, 1082–1092, https://doi.org/10.1016/S1474-4422(12)70230-2 (2012).
Calabrese, M. et al. Cortical lesions and atrophy associated with cognitive impairment in relapsing-remitting multiple sclerosis. Arch. Neurol. 66, 1144–1150, https://doi.org/10.1001/archneurol.2009.174 (2009).
Roosendaal, S. D. et al. Accumulation of cortical lesions in MS: relation with cognitive impairment. Multiple Scler. 15, 708–714, https://doi.org/10.1177/1352458509102907 (2009).
Nelson, F. et al. Intracortical lesions by 3T magnetic resonance imaging and correlation with cognitive impairment in multiple sclerosis. Multiple Scler. 17, 1122–1129, https://doi.org/10.1177/1352458511405561 (2011).
Nielsen, A. S. et al. Contribution of cortical lesion subtypes at 7T MRI to physical and cognitive performance in MS. Neurol. 81, 641–649, https://doi.org/10.1212/WNL.0b013e3182a08ce8 (2013).
Harrison, D. M. et al. Association of Cortical Lesion Burden on 7-T Magnetic Resonance Imaging With Cognition and Disability in Multiple Sclerosis. JAMA Neurol. 72, 1004–1012, https://doi.org/10.1001/jamaneurol.2015.1241 (2015).
Shinoda, K. et al. HLA-DRB1*04:05 allele is associated with intracortical lesions on three-dimensional double inversion recovery images in Japanese patients with multiple sclerosis. Multiple sclerosis, 1352458517707067, https://doi.org/10.1177/1352458517707067 (2017).
Matsushita, F. et al. Clinical significance of cortical lesions in patients with multiple sclerosis: A neuropsychological and neuroimaging study. Brain Behav. 8, e00934, https://doi.org/10.1002/brb3.934 (2018).
Kira, J. Multiple sclerosis in the Japanese population. Lancet Neurol. 2, 117–127 (2003).
Nakamura, Y. et al. A comparison of brain magnetic resonance imaging lesions in multiple sclerosis by race with reference to disability progression. J. neuroinflammation 15, 255, https://doi.org/10.1186/s12974-018-1295-1 (2018).
Calabrese, M. et al. Detection of cortical inflammatory lesions by double inversion recovery magnetic resonance imaging in patients with multiple sclerosis. Arch. Neurol. 64, 1416–1422, https://doi.org/10.1001/archneur.64.10.1416 (2007).
Calabrese, M. et al. Evidence for relative cortical sparing in benign multiple sclerosis: a longitudinal magnetic resonance imaging study. Multiple Scler. 15, 36–41, https://doi.org/10.1177/1352458508096686 (2009).
Calabrese, M. et al. Imaging distribution and frequency of cortical lesions in patients with multiple sclerosis. Neurol. 75, 1234–1240, https://doi.org/10.1212/WNL.0b013e3181f5d4da (2010).
Filippi, M. et al. Intracortical lesions: relevance for new MRI diagnostic criteria for multiple sclerosis. Neurol. 75, 1988–1994, https://doi.org/10.1212/WNL.0b013e3181ff96f6 (2010).
Nakamura, Y. et al. Latitude and HLA-DRB1*04:05 independently influence disease severity in Japanese multiple sclerosis: a cross-sectional study. J. neuroinflammation 13, 239, https://doi.org/10.1186/s12974-016-0695-3 (2016).
Yates, R. L., Esiri, M. M., Palace, J., Mittal, A. & DeLuca, G. C. The influence of HLA-DRB1*15 on motor cortical pathology in multiple sclerosis. Neuropathol. Appl. Neurobiol. 41, 371–384, https://doi.org/10.1111/nan.12165 (2015).
Spencer, J. I., Yates, R. L., Bell, J. S. & DeLuca, G. C. Cortical lesions and HLA genotype: Still a grey area? Multiple sclerosis, 1352458517734071, https://doi.org/10.1177/1352458517734071 (2017).
Shinoda, K. et al. HLA genotype and cortical lesions: Response to the letter from Spencer et al. Multiple sclerosis, 1352458517734072, https://doi.org/10.1177/1352458517734072 (2017).
Bo, L., Vedeler, C. A., Nyland, H. I., Trapp, B. D. & Mork, S. J. Subpial demyelination in the cerebral cortex of multiple sclerosis patients. J. neuropathology Exp. Neurol. 62, 723–732 (2003).
Matias-Guiu, J. A. et al. Identification of Cortical and Subcortical Correlates of Cognitive Performance in Multiple Sclerosis Using Voxel-Based Morphometry. Front. Neurol. 9, 920, https://doi.org/10.3389/fneur.2018.00920 (2018).
Gouveia, A. et al. Cognitive impairment and magnetic resonance imaging correlates in primary progressive multiple sclerosis. Acta Neurol. Scand. 136, 109–115, https://doi.org/10.1111/ane.12702 (2017).
Osoegawa, M. et al. Temporal changes and geographical differences in multiple sclerosis phenotypes in Japanese: nationwide survey results over 30 years. Multiple Scler. 15, 159–173, https://doi.org/10.1177/1352458508098372 (2009).
Polman, C. H. et al. Diagnostic criteria for multiple sclerosis: 2010 revisions to the McDonald criteria. Ann. Neurol. 69, 292–302, https://doi.org/10.1002/ana.22366 (2011).
Geurts, J. J. et al. Consensus recommendations for MS cortical lesion scoring using double inversion recovery MRI. Neurol. 76, 418–424, https://doi.org/10.1212/WNL.0b013e31820a0cc4 (2011).
Camp, S. J. et al. Cognitive function in primary progressive and transitional progressive multiple sclerosis: a controlled study with MRI correlates. Brain 122(Pt 7), 1341–1348 (1999).
Starkstein, S. E. et al. Reliability, validity, and clinical correlates of apathy in Parkinson’s disease. J. Neuropsychiatry Clin. Neurosci. 4, 134–139, https://doi.org/10.1176/jnp.4.2.134 (1992).
Okada, K., Kobayashi, S., Yamagata, S., Takahashi, K. & Yamaguchi, S. Poststroke apathy and regional cerebral blood flow. Stroke 28, 2437–2441 (1997).
Abe, K., Takanashi, M. & Yanagihara, T. Fatigue in patients with Parkinson’s disease. Behav. Neurol. 12, 103–106 (2000).
Zigmond, A. S. & Snaith, R. P. The hospital anxiety and depression scale. Acta Psychiatr. Scand. 67, 361–370 (1983).
Matsuoka, T. et al. Association of the HLA-DRB1 alleles with characteristic MRI features of Asian multiple sclerosis. Multiple Scler. 14, 1181–1190, https://doi.org/10.1177/1352458508097818 (2008).
Peduzzi, P., Concato, J., Feinstein, A. R. & Holford, T. R. Importance of events per independent variable in proportional hazards regression analysis. II. Accuracy and precision of regression estimates. J. Clin. Epidemiol. 48, 1503–1510 (1995).
Acknowledgements
This study was supported in part by the following grants: a research grant from the Japan Intractable Disease Research Foundation; a Health and Labour Sciences Research Grant on Intractable Diseases (H26-Nanchitou (Nan)-Ippan-043) from the Ministry of Health, Labour and Welfare, Japan; a Grant-in-Aid for Scientific Research A (MEXT KAKENHI Grant No. 16H02657) and C (15K09341); and a Grant-in-Aid for Young Scientists B (17K16125) from the Japan Society for the Promotion of Science, Japan. We thank Doran Amos, PhD, and Rebecca Tollefson, DVM, from Edanz Group (https://en-author-services.edanzgroup.com/) for editing drafts of this manuscript.
Author information
Authors and Affiliations
Contributions
K.S. and J.K. conceived and designed the present study, analysed the data, and wrote the paper. K.S., K.M., Y.N., N.I., T.M., O.T., and J.K. collected clinical and neuroradiological data. S.S. and H.N. were speech-language-hearing therapists and conducted all neuropsychological examinations. M.N. contributed to the design of the study. K.S. and A.H. identified lesions on MRI images. All authors reviewed, amended, and agreed on the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
K.S. received speaker honoraria from Biogen Idec Japan and Takeda Pharmaceutical Company. T.M. received a grant and payment from Bayer Schering Pharma and Takeda Pharmaceutical Company for manuscript preparation and development of educational presentations and also received speaker honoraria payments from Mitsubishi Tanabe Pharma, Bayer Schering Pharma, and Biogen Idec Japan. Y.N. received grant support from Mitsubishi Tanabe Pharma, Bayer Yakuhin, Ltd., and Japan Blood Products Organization and also received speaker honoraria from Novartis Pharma. M.N. has received speaker honoraria from Biogen Idec Japan, Novartis Pharma, Mitsubishi Tanabe Pharma, Takeda Pharmaceutical Company, and Alexion Pharma Godo Kaisha. N.I. received grant support from Mitsubishi Tanabe Pharma, Osoegawa Neurology Clinic, Bayer Yakuhin, Ltd., and Japan Blood Products Organization. J.K. received grants from the Ministry of Health, Labour, and Welfare, Japan; the Ministry of Education, Culture, Sports, Science and Technology of Japan; the Japan Society for the Promotion of Science; and the Japan Agency for Medical Research and Development (AMED), Japan. J.K. further received grants and personal fees from Biogen Idec Japan, Novartis Pharma, Philips and Mitsubishi Tanabe Pharma, Eisai, Otsuka Pharmaceutical, Chugai Pharmaceutical Company, Nihon Pharmaceutical Company, and Fukuda Denshi. K.M., S.S., H.N., O.T., and A.H. have nothing to declare.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Shinoda, K., Matsushita, T., Nakamura, Y. et al. Contribution of cortical lesions to cognitive impairment in Japanese patients with multiple sclerosis. Sci Rep 10, 5228 (2020). https://doi.org/10.1038/s41598-020-61012-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-61012-3
This article is cited by
-
An angel or a devil? Current view on the role of CD8+ T cells in the pathogenesis of myasthenia gravis
Journal of Translational Medicine (2024)
-
Symptom Interconnectivity in Multiple Sclerosis: A Narrative Review of Potential Underlying Biological Disease Processes
Neurology and Therapy (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.