Abstract
Forecasting healthcare utilization has the potential to anticipate care needs, either accelerating needed care or redirecting patients toward care most appropriate to their needs. While prior research has utilized clinical information to forecast readmissions, analyzing digital footprints from social media can inform our understanding of individuals’ behaviors, thoughts, and motivations preceding a healthcare visit. We evaluate how language patterns on social media change prior to emergency department (ED) visits and inpatient hospital admissions in this case-crossover study of adult patients visiting a large urban academic hospital system who consented to share access to their history of Facebook statuses and electronic medical records. An ensemble machine learning model forecasted ED visits and inpatient admissions with out-of-sample cross-validated AUCs of 0.64 and 0.70 respectively. Prior to an ED visit, there was a significant increase in depressed language (Cohen’s d = 0.238), and a decrease in informal language (d = 0.345). Facebook posts prior to an inpatient admission showed significant increase in expressions of somatic pain (d = 0.267) and decrease in extraverted/social language (d = 0.357). These results are a first step in developing methods to utilize user-generated content to characterize patient care-seeking context which could ultimately enable better allocation of resources and potentially early interventions to reduce unplanned visits.
Similar content being viewed by others
Introduction
There are approximately 137 million emergency department (ED) visits and 36 million inpatient admissions annually in the United States (US). Forecasting healthcare utilization has the potential to anticipate care needs, either accelerating needed care or redirecting patients toward care most appropriate to their needs. The behavioral traces people leave in their social media and digital activities embed clues about health and health care behaviors, creating an opportunity for such forecasting.
Indeed, many Internet users spend nearly 10% of waking time each day using social media platforms like Facebook, Twitter, Instagram, and Snapchat, generating or consuming content1. Approximately 15–25% of this content is health-related2. As a result, social media now provides a view into an enormous sector of patients’ health that was previously unobservable. Statistical and machine learning language processing techniques have been used to relate social media language use to a wide variety of health-related outcomes including mood3 and mental health attributes such as depression4, suicidal ideation5,6, loneliness7, and post-traumatic stress disorder8.
Social media sources provide an opportunity to evaluate data at the individual level, and their accessibility supports studies to test their predictive power and to generate insights about what underlies observed associations between people’s communications and their health. For example, depressed individuals use more first-person singular pronouns suggesting higher self-focus9,10. Natural language processing and machine learning automate the analysis of posts that would have been too numerous to evaluate manually. These tools have revealed their value, with studies showing that Facebook and Twitter posts can be used to predict mental health diagnoses and outcomes. To date, only a few studies have evaluated the potential contribution of digital data in studying healthcare utilization at the individual level11.
We sought to develop a machine learning framework to evaluate if posts on social media change before an ED visit or inpatient hospitalization. We aimed to answer two questions: 1) Can social media language forecast healthcare utilization? 2) Which specific linguistic characteristics in social media posts change before a hospital visit?
Results
Participants
Of the 5,401 patients seeking care at an urban academic hospital who consented to share their Facebook posts along with their electronic medical record (EMR) data, 2915 individuals had posts that we obtained. We used the case-crossover design12 to distinguish change in users’ social media language features before a hospital visit compared to the change prior to any random time point (Fig. 1). 419 patients with an emergency visit without inpatient admission and 167 with inpatient admissions met the eligibility criteria. Of 419 included in the analysis for emergency visits, 84% were African American, 89% were women, and the median age was 28. Of 167 included in the analysis for inpatient visits, 86% were African American and 91% were women, with a median age of 30 (Table 1). Of 167 patients who were admitted to inpatient services, 117 initially received care in the ED. The primary ED visits were for unspecified abdominal pain, chest pain, and headache; and the primary inpatient admissions were pregnancy-related, sickle cell disease with crisis, and shortness of breath. We compared the age, gender, and race of the participants who were included in this analysis to those who were not and found no significant difference.
Defining time periods prior true (hospital visits) and null (random time point) events. Figure shows the time periods before a hospital visit and random time points from which changes in linguistic features were calculated. Dark blue points are hospital visits (true event). Red point is a random time point (null event). Grey and Orange windows are 30 day periods, separated by a 15 day window, prior to true and null events.
Predicting hospital visits using changes in language prior to the visit
Using the linear ensembling of machine learning models, language change prior to ED visits was predicted with an AUC of 0.64 (F1 score = 0.61) and those prior to inpatient visits with an AUC of 0.70 (F1 score = 0.65). Figure 2 shows the Area Under the Receiver Operating Curves with True Positive Rates (sensitivity) vs. False Positive Rates (1-specificity). While the ensemble model obtained the best performance, we also performed an active control analysis using a simple modeling technique (logistic regression with ridge penalization) and obtained AUC of 0.69 (F1 score = 0.62) and 0.63 (F1 score = 0.60) for predicting inpatient and emergency visits respectively. We ran the same ensemble model on another control set (for the same patients) independently and obtained similar results (ED: AUC of 0.63, F1 score = 0.60; inpatient: AUC of 0.69 and F1 score = 0.62). The methods we implemented achieved predictive power comparable to methods that relied on direct clinical information such as prior hospitalizations and primary outcomes for patients hospitalized for at least 24 hours13,14,15.
Area Under the Receiver Operating Curves of linear ensemble models forecasting emergency (ED) and inpatient visits. Black dots indicate sensitivity at specific false positive rates (10%, 50% and 90%). Black dashed line represents AUC of 0.5. Blue line indicates Inpatient visits and red line indicates emergency visits.
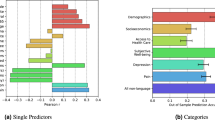
Identifying differentially expressed language features prior to a hospital visit
Tables 2 and 3 show the differentially expressed language features prior to ED and inpatient visits respectively. Table 4 shows several representative examples of posts. All represented posts were de-identified and paraphrased for anonymity.
Dictionary-based: Prior to ED visits, patients less more likely to post about leisure (d = −0.225), associated words such as ‘family’, ‘fun’, ‘play’, ‘nap’, internet slang (netspeak) (d = −0.374) words such as ‘:)’, ‘fb’, ‘ya’, ‘ur’, and informal language (d = −0.345) with words such as ‘u’, ‘lol’, ‘smh’, ‘da’. Patients also use personal pronouns less (d = −0.345) prior to ED visits compared to random time windows. In addition to these, prior to inpatient visits, patients increasingly post about family (d = 0.306) using words such as ‘baby’, ‘ma’, ‘son’; health (d = 0.255) using words such as ‘tired’, ‘pain’, ‘sick’, ‘ill’; and post less about their drives (d = -0.354) with words such as ‘up’, ‘get’, ‘love’, ‘good’, use less swear words (d = -0.209), less non fluences (d = -0.335) such as ‘ugg’, ‘oh’, ‘er’ and less positive emotion (d = -0.228) words such as ‘love’, ‘good’, ‘better, and affiliations (d = -0.361) with words such as ‘we’, ‘our’, ‘friends’.
Open-vocabulary: Posts prior to ED visits had an increased usage of topics related to family (d = 0.165, ‘kids’, ‘child’, ‘their’, ‘mother’) and words indicative of hospital visits (d = 0.230, ‘hospital’, ‘paid’, ‘blood’, ‘doctor’), and gratitude (d = 0.142, ‘thankful’, ‘amazing’, ‘blessed’). In addition to these, prior to inpatient visits, patients increasingly post about doctor appointments (d = 0.504, ‘check’, ‘yes’, ‘doctor’, ‘office’, ‘waiting’) and somatic issues (d = 0.267, ‘hurt’, ‘head’, ‘bad’, ‘body’, ‘stomach’).
Mental well-being: Anxious and depressed language increased significantly (d = 0.241 and 0.238, respectively) prior to an ED visit. Increases were found in positive valence (d = 0.168) and arousal (d = 0.160) as revealed by users’ language. Also, the frequency of posts between 9am-3pm increased prior to an ED visit. Language changes prior to inpatient visits had higher effect sizes on several of these categories. Depressed and anxious language increased significantly (effect size, d = 0.306 and 0.286 respectively), and increase in extroverted language was more prominent (d= −0.357) during random time windows compared to that prior an inpatient visit.
Posts in context: The examples in Table 4 demonstrate that the words used in posts may also provide insights about patients’ health related behaviors, symptoms, and intentions to present to the hospital. Health related behaviors could be risk factors - one patient reported eating a “cheeseburger and fries” 25 days prior to an admission for angina in the setting of heart failure – or steps leading to procedure - another patient posted confirming that they were fasting in the 24-hour lead up to a scheduled surgery. Symptoms were sometimes specific, like a patient complaining of being unable to sleep when lying flat, consistent with orthopnea, one day prior to an admission for a heart failure exacerbation. At other times, they were more vague, like a patient describing a “heavy heart” in the setting of the passing of a grandparent 3 days prior to an ED visit for “breast pain”, or a post describing feeling “sick” and “so bored” 2 days before an ED visit for nausea of unclear etiology. Patients often gave warning prior to presenting to the hospital: one patient wrote, “I’m so sick…I’m ready to go to the emergency room…it took me an hour to get up and pee” one day before an inpatient admission for pelvic inflammatory disease.
Discussion
This study has three main findings. First, people use different language in their Facebook posts prior to an ED visit or inpatient admission compared to other times. Second, a machine learning model based on these language differences distinguished ED and inpatient visit months from non-visit month with AUCs of 0.64 and 0.70 respectively. Third, a machine learning model identified linguistic markers that are differentially expressed prior to hospital visits. One of the salient themes that emerged the month prior to ED and inpatient visits was that anxious and depressed language increased significantly. Similar associations have been found with psychological stress16,17, quality of life and physical health in general18. A manual review of posts showed that posts often describe specific risk factors and symptoms that align with an eventual diagnoses. Collectively, these results suggest that analyzing non-clinical data from social media posts has the potential to forecast hospital utilization for certain conditions.
Prior efforts to predict healthcare visits have relied on clinical information such as prior hospitalizations and primary outcomes for patients hospitalized for at least 24 hours. Such features were found to predict 30-day readmission risk using deep learning models with an AUC of 0.7513. Also, prediction of readmission risk post hospitalizations for heart failure did not seem to be improved by using self-reported socioeconomic, health status, and psychosocial characteristics (to an AUC of 0.65)14. While prediction of health care utilization has been examined in terms of readmission for specific diseases15, researchers are investigating non-traditional sources to supplement clinical and sociodemographic information that give insight into everyday aspects of one’s life in their natural environment19. These ecological factors could potentially complement information directly obtained in a clinic or laboratory. Other work using web search behavior suggests that it is possible to predict future patient visits from geotagged mobile search logs20, though they provide little insight on the context of healthcare utilization. The findings in this study show promise to use social media in not only forecasting hospital visits at the patient level but also gaining insight into patients’ behavior.
One-fifth of the world’s population uses Facebook and Twitter21, and people are increasingly sharing information about their health on social media sites22. Social media has been used to study a wide variety of health-related outcomes including depression4, stress17, and schizophrenia23. The benefits of studying patterns of language use as opposed to other sources of “big data” is that words are more easily interpretable, enabling studies to not only test the predictive power of social media but also to generate insights.
Utilizing nontraditional digital sources may allow clinicians to intervene earlier and design interventions to target patients at higher risk of readmission or excessive hospital utilization. In future studies, machine learning models could target specific patient populations to alert clinicians when there are patients at higher risk of readmission before the event occurs. The clinician could then intervene by addressing the patient’s medical needs with the goal of preventing the hospital visit. For instance, a patient complaining online of persistent fever despite antibiotic therapy could be flagged for more immediate follow-up, or a patient reporting doubts about what, if anything, could be eaten during bowel preparation prior to a surgery could be contacted proactively with an automated message outlining basic instructions.
This study has several limitations. First, although the demographics of our sample are similar to the overall population served by ED of our health system, our sample is not representative of the general population. Our sample represents both a historically underserved and non-representative sample. This was a convenience sample of patients receiving care at an academic, urban health system who indicated they used social media and were willing to share access to their EMR and social media data. Second, the EMR data about visits is obtained from a single health system whereas patients might have received care from other systems which are not captured in our analysis. Third, language use is highly regional and so the particular terms, or even the patterns of use, modeled in one region may not well predict events in another.
The potential to glean such personal information about individuals when they might visit the hospital from social media reveal challenges associated with addressing several ethical and privacy concerns. Research has found that a large proportion of patients are willing to securely share their personal data sources24 and are open to linking it to their electronic health record22 for research purposes. In this type of work, privacy is of central importance. When consenting patients, we stress that their clinicians are not surveilling their Facebook posts directly; rather, the de-identified data are automatically processed in aggregate and knowledge is drawn from the data to help us learn how to better address patient needs. Transparency about how, why and by whom these health indicators are used is critical. A multi-disciplinary approach of involving clinicians, computer scientists, policy makers, ethicists can inform how to analyze and integrate predictive models based on digital traces into systems of care25.
Methods
This study was approved by the University of Pennsylvania Institutional Review Board. De-identified data necessary to reproduce the results contained in the document are available upon request. We will not, however, share individual-level Facebook data as it contains potentially identifying information about patients enrolled in the study. We will not share any EMR data. Data from participants was obtained from all participants with informed consent. All methods were performed and results presented in accordance with HIPAA guidelines.
Participants
The social mediome study26 is an ongoing study of consenting patients who share access to their social media and EMR data. Using a convenience sample framework, patients receiving care in an urban academic hospital system are approached for study participation. Patients who consent to share their Facebook posts and access to their EMR are enrolled. We do not access data from study participants’ friends or from posts on the study participants’ pages made by anyone other than the participant. Additional details about the study design are described elsewhere26. For each participant we collect data from the EMR regarding demographics (age, race, gender), date and primary reason for every ED visit and inpatient admission.
Study design
We used the case-crossover design to distinguish change in a user’s social media language features before a hospital visit compared to the change prior to any random time point (Fig. 1). In case-crossover studies, the existence of triggers before an event are compared to the existence of triggers at prior time periods from the same participant, allowing a more precise estimate of the association of triggers with events because each patient serves as his or her own control. We first describe how different time periods were defined for comparison and then describe the approaches we used to quantify features from language.
Time periods before a hospital visit and random time points: defining true and null events
Using the EMR, we identified emergency and inpatient visits for all participants who consented to share their social media data. Using the case-control design, two periods were defined per person: one 2.5 month period before a hospital visit (true event–the “case”), and one 2.5 month period before a random date (null event–the “control”). For the case, we selected the most recent visit date for each participant with more than 20 posts in each month. The users meeting this inclusion criteria were used for subsequent analysis. The day of the hospital visit was removed, and only the messages prior to that date were used in the analysis.
To control for time-invariant differences between individuals (e.g. the use of hashtags was constantly increasing in time) we made predictions based on change in language rather than direct language use. Within each 2.5 month period, change was defined as the difference between two 30 day periods, separated by 15 days (see Fig. 1). We compared age, gender, and race of those who met the inclusion criteria versus others and found similar distribution. Based on prior research27, we chose 20 posts as the threshold within each window, and consequently we used 30 days as the window length and the gap between both windows was set to 15 days for emergency and inpatient settings.
In this longitudinal analysis, every patient is his or her own control–i.e. language prior to the null event is considered as control and language prior to the true event is considered part of the case group.
Defining language features
We use three sets of linguistic features for measuring change in language: a) open-vocabulary topics28, b) dictionary-based psycholinguistic features29, c) style features such as valence (positive or negative affectivity), arousal (how calming or exciting the post is)30, and extent of anxious, extraverted, and depressed language31 by applying previously developed statistical models, and meta features such as posting statistics (average number of 1-grams) and time of posts. These have been shown to be predictive of several health outcomes such as depression4, schizophrenia32, attention deficit hyperactivity disorder (ADHD)33, and general well-being34. As researchers have used various types of biomarkers for diseases35,36, our aim was to identify the language markers37 among these features that are predictive and are differentially expressed prior to hospital visits.
From each post, we extracted the relative frequency of single words and phrases (consisting of two or three consecutive words). The distribution of two hundred latent dirichlet allocation (LDA) open vocabulary topics generated from a different cohort (consisting of N = 999 further patients)38, was then extracted from each post. The distribution of Linguistic Inquiry Word Count (LIWC) dictionary features39 was also extracted for each post. We extracted the relative frequency of each attribute (i.e., the total number of times a word written by the user matches a word in a given attribute, divided by the user’s total number of words). After aggregating these features for every user in each time window, the difference was then calculated to measure language change prior to hospital visit and prior to a random time point.
Finally, in order to understand language trends by diagnosis, two coders, DCS and SCG, identified presumed primary diagnoses for inpatient and ED encounters based on the combination of provider-reported ICD codes. DCS and SCG then reviewed Facebook posts prior to these encounters to identify representative examples. Examples were agreed upon by both coders and paraphrased in order to preserve sentiment while maintaining anonymity.
Statistical analysis
Predicting hospital visits using changes in language prior to the visit
The aim of our prediction analysis was to assess whether a machine learning algorithm can automatically predict changes in linguistic markers prior to a hospital visit compared to a null event. For each patient, every hospital visit was paired with a null event.
Cross-Validation: The predictive model was tested using 5-fold cross-validation40, where the users in the training and test folds were mutually exclusive. Thus, the predictive model was created 5 times without any outcome information outside of the training data. A dimensionality reduction step (using Principal component analysis) was employed on all the language features to remove correlated features before input to the predictive model. We used linear ensembling (averaging) of several classifiers (Random Forest, Support Vector Machine, Gradient Boosting Machine and Logistic Regression) from the scikit-learn41 module in Python 3.4 language to fit all our models on the training folds. This is similar to the autoML paradigm of model selection which not only tends to give better predictive performance but also prevents any user bias from being introduced into the resulting model, such as a preference for one algorithm over another or prior knowledge about the dataset that can be exploited42. The ensemble trained on each training set was then applied on the corresponding held-out test set. This was repeated 5 times; the overall predictive performance is reported in terms of the Area Under the ROC Curve (AUC) and F1-score.
Identifying differentially expressed language features prior to a hospital visit
Within each participant, we then compared all the features from the windows prior to true and null events using a two-tailed paired t-test (alpha = 0.05). We used Benjamini-Hochberg p-correction to control the False Discovery Rate and a threshold of p < 0.05. We measured the effect sizes using Cohen’s d.
Change history
07 July 2020
An amendment to this paper has been published and can be accessed via a link at the top of the paper.
References
Alhabash, S. & Ma, M. A Tale of Four Platforms: Motivations and Uses of Facebook, Twitter, Instagram, and Snapchat Among College Students? Soc. Media + Soc. 3 (2017).
Bravo, C. A. & Hoffman-Goetz, L. Social Media and Men’s Health: A Content Analysis of Twitter Conversations During the 2013 Movember Campaigns in the United States, Canada, and the United Kingdom. Am. J. men’s Health 11, 1627–1641 (2017).
Roshanaei, M., Han, R. & Mishra, S. Features for mood prediction in social media. In Proceedings of the 2015 IEEE/ACM International Conference on Advances in Social Networks Analysis and Mining 2015 - ASONAM ’15 1580–1581 (ACM Press, 2013), https://doi.org/10.1145/2808797.2809342
Guntuku, S. C., Yaden, D. B., Kern, M. L., Ungar, L. H. & Eichstaedt, J. C. Detecting depression and mental illness on social media: an integrative review. Current Opinion in Behavioral Sciences 18, 43–49 (2017).
Burnap, P., Colombo, W. & Scourfield, J. Machine Classification and Analysis of Suicide-Related Communication on Twitter. In Proceedings of the 26th ACM Conference on Hypertext & Social Media - HT ’15 75–84 (ACM Press, 2013), https://doi.org/10.1145/2700171.2791023
Shing, H.-C. et al. Expert, crowdsourced, and machine assessment of suicide risk via online postings. In Proceedings of the Fifth Workshop on Computational Linguistics and Clinical Psychology: From Keyboard to Clinic 25–36 (1985).
Guntuku, S. C. et al. Studying expressions of loneliness in individuals using twitter: an observational study. BMJ Open 9(11), e030355 (2019).
Coppersmith, G., Harman, C. & Dredze, M. Measuring post traumatic stress disorder in Twitter. In Eighth international AAAI conference on weblogs and social media (2014, May).
De Choudhury, M., Gamon, M., Counts, S. & Horvitz, E. Predicting depression via social media. In Seventh international AAAI conference on weblogs and social media (2013, June).
Chung, C. K. & Pennebaker, J. W. The psychological functions of function words. Soc. Commun. Front. Soc. Psychol. 343–359 (2005).
Asch, J. M. et al. Google search histories of patients presenting to an emergency department: an observational study. BMJ open 9, e024791 (2019).
Maclure, M. The Case-Crossover Design: A Method for Studying Transient Effects on the Risk of Acute Events. American Journal of Epidemiology 133(2), 144–153 (1991).
Frizzell, J. D. et al. Prediction of 30-Day All-Cause Readmissions in Patients Hospitalized for Heart Failure: Comparison of Machine Learning and Other Statistical Approaches. JAMA Cardiol. 2, 204–209 (2017).
Krumholz, H. M. et al. Do Non-Clinical Factors Improve Prediction of Readmission Risk?: Results From the Tele-HF Study. JACC. Heart Fail. 4, 12–20 (2016).
Krumholz, H. M. Big data and new knowledge in medicine: the thinking, training, and tools needed for a learning health system. Health Aff. 33, 1163–1170 (2014).
Lin, H. et al. User-level psychological stress detection from social media using deep neural network. In Proceedings of the ACM International Conference on Multimedia - MM ’14 507–516 (ACM Press, 2012), https://doi.org/10.1145/2647868.2654945
Guntuku, S. C. et al. Understanding and measuring psychological stress using social media. Proceedings of the International AAAI Conference on Web and Social Media 13, 1 (2019).
Engin, B. et al. The levels of depression, anxiety and quality of life in patients with chronic idiopathic urticaria. Journal of the European Academy of Dermatology and Venereology 22.1, 36-40 (2008).
Luxton, D. D., McCann, R. A., Bush, N. E., Mishkind, M. C. & Reger, G. M. mHealth for mental health: Integrating smartphone technology in behavioral healthcare. Prof. Psychol. Res. Pract. 42, 505–512 (2010).
Agarwal, V. et al. Impact of Predicting Health Care Utilization Via Web Search Behavior: A Data-Driven Analysis. J. Med. Internet Res. 18, e251 (2016).
Errasti, J., Amigo, I. & Villadangos, M. Emotional Uses of Facebook and Twitter. Psychol. reports 33294117713496, https://doi.org/10.1177/0033294117713496 (2017).
Asch, D. A., Rader, D. J. & Merchant, R. M. Mining the social mediome. Trends Mol. Med. 21 (2015).
Birnbaum, M. L., Ernala, S. K., Rizvi, A. F., De Choudhury, M. & Kane, J. M. A Collaborative Approach to Identifying Social Media Markers of Schizophrenia by Employing Machine Learning and Clinical Appraisals. J. Med. Internet Res. 19, e289 (2017).
Seltzer, E. et al. Patients’ willingness to share digital health and non-health data for research: a cross-sectional study. BMC Medical Informatics and Decision Making 19(1) (2019).
Inkster, B., Stillwell, D., Kosinski, M. & Jones, P. A decade into Facebook: where is psychiatry in the digital age? lancet. Psychiatry 3, 1087–1090 (2016).
Padrez, K. A. et al. Linking social media and medical record data: a study of adults presenting to an academic, urban emergency department. BMJ Qual. & Saf. 25, 414–423 (2016).
Jaidka, K., Guntuku, S. C. & Ungar, L. H. Facebook versus Twitter: Differences in Self-Disclosure and Trait Prediction. In Twelfth International AAAI Conference on Web and Social Media. (2018, June).
Schwartz, H. A. et al. Personality, gender, and age in the language of social media: the open-vocabulary approach. PloS one 8, e73791 (2013).
Tausczik, Y. R. & Pennebaker, J. W. The Psychological Meaning of Words: LIWC and Computerized Text Analysis Methods. J. Lang. Soc. Psychol. 29, 24–54 (2009).
Preoţiuc-Pietro, D. et al. Modelling Valence and Arousal in Facebook posts. In Proceedings of the 7th Workshop on Computational Approaches to Subjectivity, Sentiment and Social Media Analysis 9–15 (Association for Computational Linguistics), https://doi.org/10.18653/v1/W16-0404
Schwartz, H. A. et al. Towards Assessing Changes in Degree of Depression through Facebook. In Proceedings of the Workshop on Computational Linguistics and Clinical Psychology: From Linguistic Signal to Clinical Reality 118–125 (Association for Computational Linguistics, 2012), https://doi.org/10.3115/v1/W14-3214
Ernala, S. K., Rizvi, A. F., Birnbaum, M. L., Kane, J. M. & De Choudhury, M. Linguistic Markers Indicating Therapeutic Outcomes of Social Media Disclosures of Schizophrenia. Proc. ACM Human-Computer Interact. 1 (2017).
Guntuku, S. C., Ramsay, J. R., Merchant, R. M. & Ungar, L. H. Language of ADHD in Adults on Social Media. J. Atten. Disord. 1087054717738083, https://doi.org/10.1177/1087054717738083 (2017).
Schwartz, H. A. et al. Predicting individual well-being through the language of social media. Pac. Symp. Biocomput. Pac. Symp. Biocomput. 21, 516–527 (2014).
Breteler, M. M. B. Mapping out biomarkers for Alzheimer disease. JAMA 305, 304–305 (2011).
Shah, S. H. & de Lemos, J. A. Biomarkers and cardiovascular disease: determining causality and quantifying contribution to risk assessment. JAMA 302, 92–93 (2009).
Rosenstein, M., Foltz, P. W., DeLisi, L. E. & Elvevåg, B. Language as a biomarker in those at high-risk for psychosis. Schizophr. Res. 165, 249–250 (2015).
Merchant, R. M. et al. Evaluating the predictability of medical conditions from social media posts. PloS one 14.6, e0215476 (2019).
Pennebaker, J. W., Boyd, R. L., Jordan, K. & Blackburn, K. The development and psychometric properties of LIWC2015 (2015).
Shao, J. Linear model selection by cross-validation. Journal of the American statistical Association 88(422), 486–494 (1993).
Pedregosa, F. et al. Scikit-learn: Machine Learning in Python. J. Mach. Learn. Res. 12, 2825–2830 (2009).
Guyon, I. et al. A Brief Review of the ChaLearn AutoML Challenge: Any-time Any-dataset Learning Without Human Intervention. In Workshop on Automatic Machine Learning 21–30 (2014).
Acknowledgements
We thank Justine Marks, Molly Casey, Janice Lau for helping with data collection. This work was funded by Robert Wood Johnson Foundation Pioneer Award (Merchant). No sponsor of funding source played a role in study design and the collection, analysis, and interpretation of data and the writing of the article and the decision to submit it for publication. All researchers are independent from funders.
Author information
Authors and Affiliations
Contributions
S.C. Guntuku, H.A. Schwartz and R.M. Merchant originated the study. S.C. Guntuku, H.A. Schwartz, A. Kashyap, L.H. Ungar, R.M. Merchant developed methods, interpreted analysis, and contributed to the writing of the article. J. Gaulton, D.C. Stokes, and D.A. Asch assisted with the interpretation of the findings and contributed to the writing of the article.
Corresponding author
Ethics declarations
Competing interests
DAA is a US Government Employee.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Guntuku, S.C., Schwartz, H.A., Kashyap, A. et al. Variability in Language used on Social Media prior to Hospital Visits. Sci Rep 10, 4346 (2020). https://doi.org/10.1038/s41598-020-60750-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-60750-8
This article is cited by
-
Discovering Clusters of Support Utilization in the Canadian Community Health Survey–Mental Health
International Journal of Mental Health and Addiction (2024)
-
Social media language of healthcare super-utilizers
npj Digital Medicine (2021)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.